Abstract
Objective
To estimate weather contraceptive failure rates among combined oral contraceptive pill, patch, and vaginal ring users was associated with increasing body mass index (BMI).
Methods
Females enrolled in a large contraceptive study offering the reversible method of their choice at no cost, were followed for 2 to 3 years. We compared the failure rates (pregnancy) among users of the oral contraceptive pill (OCP), transdermal patch, and contraceptive vaginal ring stratified by BMI.
Results
Among the 7,486 participants available for this analysis, 1,523 chose OCPs, patch, or ring at enrollment. Of the 334 unintended pregnancies, 128 were found to be a result of pill, patch, or ring failure. Three-year failure rates were not different across BMI categories (BMI <25: 8.44% (95% CI 6.1, 11.5), BMI 25–30: 11.03% (95% CI 7.5, 16.0), BMI >30: 8.92% (95% CI 7.6, 11.5). Increasing parity (HR: 3.06, CI 1.31–7.18), and history of a previous unintended pregnancy (HR: 2.82, CI: 1.63–4.87), but not BMI, were significant risk factors for unintended pregnancy.
Conclusion
Overweight and obese females do not appear to be at increased risk for contraceptive failure when using the contraceptive pill, patch, or vaginal ring.
Introduction
The epidemic of obesity worldwide is continuing to grow. Current statistics estimate that 61.3% of adult females in the United States are classified as overweight, with 34.3% classified as obese. (1) The remarkable growth can be best illustrated when we compare these rates to just ten years ago when only 20.8% of the US female population was classified as obese. (1)The increase in obesity has led to the development of sub-classifications within the larger obese group; class I: BMI 30–34.9, class II BMI 35–39.9 and class III BMI ≥ 40. (2) In 2007–2008, 10.5% of reproductive age females age 20–39 were class II obese and 7.5% were class III. (1)
Equally discouraging is the prevalence of unintended pregnancy which despite widespread use of contraception is still estimated to be 49%. (3) Preventing unplanned pregnancy in obese females is especially important given the associated comorbidities and pregnancy complications. Still understudied is the role that obesity plays in contraceptive effectiveness. Most contraceptive research has been limited to females who are within 130% of ideal body weight. To date, there has been conflicting data regarding contraceptive failure rates among overweight and obese females using combined hormonal contraception (oral contraceptive pill (OCP) and the contraceptive patch and ring). (4–7) Holt and colleges performed a case-control study evaluating pregnancy failures in oral contraceptive users and suggest that being overweight may be associated with an increased risk of pregnancy while using OCPs. (8) The methodology of this study has been challenged however citing recall bias, as well as flaws in the design and data collection. (9) Among the proposed mechanisms for increased failure rates are incomplete ovarian suppression leading to more frequent ovulation and altered bioavailability of the active drugs perhaps because of variable rates of metabolism and clearance or differences in steroid distribution and absorption. (10–12) Thus, accurate contraceptive counseling regarding failure rates in obese females is difficult.
The objective of our study was to estimate whether contraceptive failure rates were associated with increasing body mass index (BMI). Our null hypothesis was that there would be no difference in failure rates with increasing BMI.
Materials and Methods
The methodologic details of the Contraceptive CHOICE Project have been previously published (13) and enrolled participants from August 2007 through September 2011. A brief description of the project and this specific analysis are described below. The CHOICE protocol was approved by the Institutional Review Board at Washington University in St. Louis.
The CHOICE Project is a prospective cohort study of 9256 reproductive-age females in the St Louis area that was designed to promote long-acting reversible contraceptive (LARC) methods by reducing cost, knowledge, and access barriers. Each potential participant received standardized contraceptive counseling on all available reversible methods. This counseling included information regarding effectiveness, common side-effects, as well as risks and benefits for each method. (14) Each participant was then provided with the reversible contraceptive method of her choice at no cost for three years (first 5090 participants) or two years (remainder of the cohort). Participants choosing oral contraceptive pills could choose from various types based on their own preference or provider recommendation. Ethinyl estradiol dose in the combined hormonal methods ranged from 20mcg to 35mcg. Participants were allowed to change methods as many times as desired during the follow-up period.
Inclusion criteria for the CHOICE project included 1) age 14–45 years; 2) not currently using contraception or willing to change reversible contraceptive methods; 3) not desiring pregnancy in the next 12 months; 4) sexually active or intending sexual activity with a male partner in the next six months; 5) reside in or seeking health care in the St Louis area; and 6) able to consent in English or Spanish. Females were excluded if they had a history of a previous sterilization procedure. This analysis includes the first 7,486 participants enrolled in the CHOICE Project, of which 1,523 chose the contraceptive pill, patch, or vaginal ring at enrollment. All participants who used the OCP, patch or vaginal ring at any point during their study enrollment and had their body mass index (BMI) calculated at the time of enrollment using objectively measured weight and height were included.
Participants were followed with telephone interviews at 3 and 6 months, and every 6 months thereafter and received a $10 gift card for each completed follow-up survey. The possibility of contraceptive failure was assessed at each follow-up survey with questions about missed menses and the participant’s perception of the possibility of pregnancy. Any participant concerned about pregnancy was offered a clinic appointment for urine pregnancy testing. All pregnancies were documented in a pregnancy log. Each participant with a documented pregnancy was then asked if the pregnancy was planned, and what contraceptive method they were using at the time. A true contraceptive failure was defined as pregnancy that occurred during a period of OCP, patch, or vaginal ring use. Intended or planned pregnancies and pregnancies occurring with other contraceptive method use (or no method) were excluded.
The primary outcome of this analysis was contraceptive failure in females using the contraceptive pill, patch, or vaginal ring by BMI class. Participants were classified in one of 4 weight categories according to their BMI as defined by the World Health Organization. (15) Normal weight woman are defined as those with BMI less than 25, overweight females with BMI 25.0–29.9, obese females with BMI 30.0–39.9, and morbidly obese with BMI ≥ 40.
All statistical analyses were performed using STATA 11(StataCorp). Significance levels were set at 0.05. Demographic characteristics of all participants identified for this analysis are presented as frequencies, percentages, means, and standard deviations. Baseline characteristics of females in each method group (contraceptive pill, patch, and ring) were compared using chi-square and Fisher’s exact tests for categorical variables and Student’s t-test for normally distributed continuous variables. Normality was evaluated by checking on the distribution of the variable via histogram charts. Demographic characteristics of females were also compared across four BMI categories. Contraceptive failures across methods (OCPs, ring, and patch) were combined for the remainder of analyses. Kaplan-Meier failure curves were used to estimate the contraceptive failure rates by BMI group. The Log-rank test was performed to test the equivalence of contraceptive failure rates among BMI groups. Cox proportional hazard models were used to estimate the hazard ratios for unintended pregnancy between different BMI categories. Because we measured distinct segments of contraceptive method use by each participant, there are correlations among different periods of contraceptive use from the same participant. To account for this correlation effect, we used robust variance-covariance estimation methods. (16) Univariable analyses were conducted to evaluate crude associations between each baseline covariate and unintended pregnancy. Confounding was defined as a greater than 10% relative change in the association between unintended pregnancy and BMI category with or without the covariate of interest in the model. Confounders were included in the final multivariable model.
To confirm we had an adequate sample size to detect a two-fold difference in failure rates across BMI groups a post-hoc sample size using nQuery software was calculated. Using the observed failure rate at three years of 8% in the normal weight group as the reference, we determined that 274 distinct periods of pill, patch, or ring use per BMI group would be required to achieve 80% power with an alpha error of 0.05. We combined our obese and morbidly obese groups to maintain 80% power for our analyses.
Results
From August 2007 through May 2011, we identified 334 unintended pregnancies, of which 128 were attributed to pill, patch, or vaginal ring failure. Table 1 describes the demographic characteristics of females choosing the contraceptive pill, patch, or vaginal ring at enrollment by method type. The demographic characteristics of pill and ring users were similar. Pill and ring users were more likely to be white, educated, have private insurance, and nulliparous than were patch users. Patch users were more likely to be black, have less education, report low socioeconomic status, no insurance, higher parity, and a history of unintended pregnancy and abortion. Despite demographic differences, one-year contraceptive failure rates among the three methods were similar (pill: 5.6%, patch: 4.6%, vaginal ring: 3.4% p=0.22). In addition, no statistically significant interactions were found between contraceptive method and BMI; thus, the three methods were combined for analysis across BMI categories.
Table 1.
Demographic Characteristics of Pill, Patch, and Ring Users
| Pills (n=779) | Patch (n=143) | Ring (n=601) | P | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Age* | 23.7 (5.0) | 24.1 (4.4) | 24.3 (4.5) | 4.5 | 0.042 | ||
| Race | <0.001 | ||||||
| Black or African American | 327 | 42.1 | 85 | 59.4 | 227 | 38.2 | |
| White | 385 | 49.5 | 47 | 32.9 | 317 | 53.3 | |
| Other or multiracial | 65 | 8.4 | 11 | 7.7 | 51 | 8.6 | |
| Education | <0.001 | ||||||
| High school or less | 201 | 25.8 | 46 | 32.2 | 116 | 19.3 | |
| Some college | 350 | 44.9 | 66 | 46.2 | 266 | 44.3 | |
| College or graduate school | 228 | 29.3 | 31 | 21.7 | 219 | 36.4 | |
| Low socio-economic status | 0.024 | ||||||
| No | 427 | 54.8 | 64 | 44.8 | 345 | 57.4 | |
| Yes | 352 | 45.2 | 79 | 55.2 | 256 | 42.6 | |
| Monthly income (US dollars) | 0.002 | ||||||
| None | 135 | 18.1 | 23 | 16.2 | 74 | 12.8 | |
| 1–800 | 267 | 35.9 | 60 | 42.3 | 191 | 33.1 | |
| 801–1600 | 216 | 29.0 | 33 | 23.2 | 167 | 28.9 | |
| 1601 or higher | 126 | 16.9 | 26 | 18.3 | 145 | 25.1 | |
| Insurance | <0.001 | ||||||
| None | 332 | 43.1 | 76 | 53.5 | 222 | 37.6 | |
| Private/student/parent/military | 396 | 51.4 | 51 | 35.9 | 346 | 58.5 | |
| Medicare/Medicaid/disability | 42 | 5.5 | 15 | 10.6 | 23 | 3.9 | |
| Parity | 0.002 | ||||||
| 0 | 584 | 75.0 | 81 | 56.6 | 420 | 69.9 | |
| 1 | 124 | 15.9 | 38 | 26.6 | 116 | 19.3 | |
| 2 | 53 | 6.8 | 17 | 11.9 | 45 | 7.5 | |
| 3 or more | 18 | 2.3 | 7 | 4.9 | 20 | 3.3 | |
| History of unintended pregnancy | <0.001 | ||||||
| 0 | 445 | 57.5 | 52 | 36.4 | 330 | 54.9 | |
| 1 | 191 | 24.7 | 48 | 33.6 | 152 | 25.3 | |
| 2 | 82 | 10.6 | 17 | 11.9 | 60 | 10.0 | |
| 3 more | 56 | 7.2 | 26 | 18.2 | 59 | 9.8 | |
| History of abortion | <0.001 | ||||||
| 0 | 559 | 71.8 | 79 | 55.2 | 430 | 71.5 | |
| 1 | 164 | 21.1 | 46 | 32.2 | 121 | 20.1 | |
| 2 | 41 | 5.3 | 9 | 6.3 | 37 | 6.2 | |
| 3 or more | 15 | 1.9 | 9 | 6.3 | 13 | 2.2 | |
| History of sexually transmitted infection | <0.001 | ||||||
| No | 551 | 70.7 | 82 | 57.3 | 373 | 62.1 | |
| Yes | 228 | 29.3 | 61 | 42.7 | 228 | 37.9 | |
| Parity | <0.001 | ||||||
| 0 | 584 | 75.0 | 81 | 56.6 | 420 | 69.9 | |
| 1–2 | 177 | 22.7 | 55 | 38.5 | 161 | 26.8 | |
| 3 or more | 18 | 2.3 | 7 | 4.9 | 20 | 3.3 | |
| History of unintended pregnancy | <0.001 | ||||||
| No | 445 | 57.1 | 52 | 36.4 | 330 | 54.9 | |
| Yes | 334 | 42.9 | 91 | 63.6 | 271 | 45.1 | |
| History of abortion | <0.001 | ||||||
| No | 559 | 71.8 | 79 | 55.2 | 430 | 71.5 | |
| Yes | 220 | 28.2 | 64 | 44.8 | 171 | 28.5 | |
Data are mean (standard deviation).
Table 2 describes demographic and reproductive characteristics of participants by BMI category. Normal weight females (n=1476) contributed 1,473 woman-years of pill, patch, or vaginal ring use. Overweight females, BMI 25–30 (n=817), contributed 694 women-years of pill, patch, or vaginal ring use. Obese females, BMI 30–40 (n=702), contributed 572 women-years of pill, patch, or vaginal ring use. And finally, morbidly obese females, BMI ≥ 40 (n=171), contributed 124 women-years of pill, patch, or vaginal ring use. As BMI category increased, so did the mean age. Overweight, obese, and morbidly obese females were more likely to be black, have less education, lower socioeconomic status, higher parity, and a history of unintended pregnancy and abortion.
Table 2.
Demographic Characteristics by Body Mass Index Class
| BMI Lower Than 25 (n=1476) | BMI 25–30 (n=817) | BMI 30–40 (n=702) | BMI 40 or Higher (n=171) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | P | |
| Age* | 23.4 (4.6) | 24.7 (5.2) | 25.5 (5.8) | 27.0 (5.5) | <0.001 | ||||
| Race | <0.001 | ||||||||
| Black or African American | 458 | 31.2 | 437 | 53.7 | 455 | 65.0 | 131 | 76.6 | |
| White | 864 | 58.9 | 314 | 38.6 | 211 | 30.1 | 34 | 19.9 | |
| Other or multiracial | 146 | 9.9 | 63 | 7.7 | 34 | 4.9 | 6 | 3.5 | |
| Education | <0.001 | ||||||||
| High school or less | 386 | 26.2 | 224 | 27.4 | 233 | 33.2 | 50 | 29.2 | |
| Some college | 611 | 41.4 | 388 | 47.5 | 324 | 46.2 | 90 | 52.6 | |
| College or graduate school | 479 | 32.5 | 205 | 25.1 | 144 | 20.5 | 31 | 18.1 | |
| Low socio-economic status | <0.001 | ||||||||
| No | 861 | 58.4 | 369 | 45.2 | 233 | 33.2 | 55 | 32.2 | |
| Yes | 614 | 41.6 | 448 | 54.8 | 469 | 66.8 | 116 | 67.8 | |
| Monthly income (US dollar) | |||||||||
| None | 273 | 19.2 | 122 | 15.2 | 125 | 18.2 | 26 | 15.3 | |
| 1–800 | 514 | 36.1 | 274 | 34.1 | 181 | 26.3 | 52 | 30.6 | |
| 801–1600 | 365 | 25.7 | 246 | 30.6 | 236 | 34.3 | 59 | 34.7 | |
| 1601 or higher | 271 | 19.0 | 162 | 20.1 | 146 | 21.2 | 33 | 19.4 | |
| Insurance | <0.001 | ||||||||
| None | 529 | 36.2 | 359 | 44.4 | 320 | 45.8 | 96 | 56.1 | |
| Private/student/parent/military | 814 | 55.8 | 364 | 45.0 | 279 | 39.9 | 59 | 34.5 | |
| Medicare/Medicaid/disability | 117 | 8.0 | 86 | 10.6 | 100 | 14.3 | 16 | 9.4 | |
| Parity | <0.001 | ||||||||
| 0 | 1070 | 72.5 | 435 | 53.2 | 297 | 42.3 | 78 | 45.6 | |
| 1 | 248 | 16.8 | 212 | 25.9 | 200 | 28.5 | 50 | 29.2 | |
| 2 | 116 | 7.9 | 110 | 13.5 | 132 | 18.8 | 28 | 16.4 | |
| 3 or more | 42 | 2.8 | 60 | 7.3 | 73 | 10.4 | 15 | 8.8 | |
| History of unintended pregnancy | <0.001 | ||||||||
| 0 | 812 | 55.1 | 323 | 39.7 | 232 | 33.1 | 61 | 35.7 | |
| 1 | 347 | 23.6 | 219 | 26.9 | 200 | 28.6 | 50 | 29.2 | |
| 2 | 171 | 11.6 | 131 | 16.1 | 119 | 17.0 | 29 | 17.0 | |
| 3 or more | 143 | 9.7 | 141 | 17.3 | 149 | 21.3 | 31 | 18.1 | |
| History of abortion | <0.001 | ||||||||
| 0 | 1038 | 70.3 | 501 | 61.3 | 429 | 61.1 | 120 | 70.2 | |
| 1 | 298 | 20.2 | 204 | 25.0 | 170 | 24.2 | 27 | 15.8 | |
| 2 | 106 | 7.2 | 71 | 8.7 | 66 | 9.4 | 16 | 9.4 | |
| 3 or more | 34 | 2.3 | 41 | 5.0 | 37 | 5.3 | 8 | 4.7 | |
| History of sexually transmitted infections | <0.001 | ||||||||
| No | 991 | 67.1 | 473 | 57.9 | 364 | 51.9 | 85 | 49.7 | |
| Yes | 485 | 32.9 | 344 | 42.1 | 338 | 48.1 | 86 | 50.3 | |
| Parity | <0.001 | ||||||||
| 0 | 1070 | 72.5 | 435 | 53.2 | 297 | 42.3 | 78 | 45.6 | |
| 1–2 | 364 | 24.7 | 322 | 39.4 | 332 | 47.3 | 78 | 45.6 | |
| 3 or more | 42 | 2.8 | 60 | 7.3 | 73 | 10.4 | 15 | 8.8 | |
| History of unintended pregnancy | <0.001 | ||||||||
| No | 812 | 55.0 | 323 | 39.5 | 232 | 33.0 | 61 | 35.7 | |
| Yes | 664 | 45.0 | 494 | 60.5 | 470 | 67.0 | 110 | 64.3 | |
| History of abortion | <0.001 | ||||||||
| No | 1038 | 70.3 | 501 | 61.3 | 429 | 61.1 | 120 | 70.2 | |
| Yes | 438 | 29.7 | 316 | 38.7 | 273 | 38.9 | 51 | 29.8 | |
Data are mean (standard deviation).
BMI, body mass index.
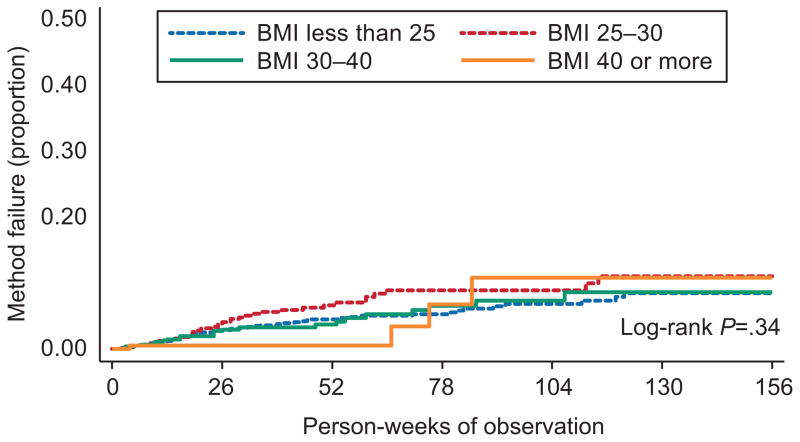
The total number of failures and cumulative failure rates per year for 3 years by BMI class are presented in Table 3. As expected, the cumulative failure rates increase with each year, but do not appear to differ across BMI categories (3-year contraceptive failure range: 8.4–11.0% 95% CI 6.1, 16.0%). The probability of contraceptive failure using log-rank testing was not different (p=0.34) when BMI classes are compared (Figure 1).
Table 3.
Failure Rates by Body Mass Index Class
| Year 1 | Year 2 | Year 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| BMI | n | Rate % | 95% CI | n | Rate % | 95% CI | n | Rate % | 95% CI |
| Lower than 25 | 48 | 4.51 | (3.4–6.0) | 9 | 6.85 | (5.1–9.2) | 3 | 8.44 | (6.1, 11.5) |
| 25–30 | 33 | 6.63 | (4.7–9.4) | 5 | 8.87 | (6.3,12.4) | 2 | 11.03 | (7.5, 16.0) |
| 30 or higher | 18 | 4.80 | (4.0,5.9) | 9 | 7.90 | (6.4,9.4) | 1 | 8.92 | (7.6, 11.5) |
| 30–40 | 17 | 3.69 | (2.3, 6.0) | 6 | 7.36 | (4.6, 11.6) | 1 | 8.61 | (5.3, 13.9) |
| 40 or higher | 1 | 0.53 | (0.08, 3.7) | 3 | 10.84 | (3.8, 29.1) | 0 | 10.84 | (3.8, 29.1) |
BMI, body mass index; n, number of failures per BMI class per year; CI, confidence interval.
Figure 1.
Kaplan-Meier failure curve. Contraceptive failure rate of pill, patch, and vaginal ring users. Log rank P=.34 represents comparison of failure rates across body mass index (BMI) classes over time.
Table 4 shows the crude and adjusted risk of contraceptive failure associated with BMI and participant characteristics. For the final model, obese and morbidly obese classes were combined. We found no difference in the risk of unintended pregnancy by BMI class. While older age was negatively associated with unintended pregnancy (HR=0.9, CI: 0.85–0.95), increasing parity (HR: 3.06, CI: 1.31–7.18) and history of unintended pregnancy (HR= 2.82, CI: 1.63–4.87) remained significant risk factors for contraceptive failure.
Table 4.
Risk of Unintended Pregnancy
| Crude Model | Adjusted Model | |||
|---|---|---|---|---|
| Hazard Ratio | [95% CI] | Hazard Ratio | [95% CI] | |
| Normal weight | Ref | Ref | ||
| Overweight | 1.38 | (0.91, 2.10) | 1.16 | (0.76, 1.78) |
| Obese | 0.97 | (0.61, 1.53) | 0.71 | (0.45, 1.12) |
| Age | 0.95 | (0.91, 0.99) | 0.91 | (0.87, 0.96) |
| Race | ||||
| 1 Black or African American | 1.84 | (1.27, 2.67) | 1.15 | (0.75, 1.75) |
| White | Ref | Ref | ||
| Other or multiracial | 1.26 | (0.64, 2.48) | 1.18 | (0.61, 2.27) |
| Education | ||||
| High school or less | Ref | Ref | ||
| Some college | 0.57 | (0.39, 0.83) | 0.77 | (0.53, 1.13) |
| College or Graduate school | 0.22 | (0.12, 0.39) | 0.61 | (0.32, 1.15) |
| Low socio-economic status | ||||
| No | Ref | Ref | ||
| Yes | 1.75 | (1.22, 2.51) | 0.77 | (0.48, 1.26) |
| Monthly income (US dollars) | ||||
| None | Ref | Ref | ||
| 1–800 | 0.87 | (0.53, 1.42) | - | - |
| 801–1600 | 0.69 | (0.40, 1.16) | - | - |
| 1601 or higher | 0.64 | (0.36, 1.16) | - | - |
| Insurance | ||||
| None | Ref | Ref | ||
| Private/student/parent/military | 0.47 | (0.32, 0.69) | 0.63 | (0.40, 1.00) |
| Medicare/Medicaid/disability | 1.51 | (0.86, 2.66) | 0.96 | (0.54, 1.70) |
| Parity | ||||
| 0 | Ref | Ref | ||
| 1–2 | 2.68 | (1.86, 3.87) | 2.00 | (1.2, 3.25) |
| 3 or more | 3.13 | (1.53, 6.42) | 3.06 | (1.3, 7.18) |
| History of unintended pregnancy | ||||
| No | Ref | Ref | ||
| Yes | 4.07 | (2.64, 6.28) | 2.82 | (1.6, 4.87) |
| History of abortion | ||||
| No | Ref | Ref | ||
| Yes | 1.76 | (1.24, 2.50) | - | - |
| History of sexually transmitted infections | ||||
| No | Ref | Ref | ||
| Yes | 1.44 | (1.02, 2.05) | 1.02 | (0.68, 1.51) |
CI, confidence interval.
Discussion
We found no difference in contraceptive failure rates among females using the pill, patch, or vaginal ring across BMI categories. Contraceptive failure is influenced by many factors including compliance, frequency of intercourse, ovulatory function, and the inherent efficacy of the contraceptive method. The potential risk of combined hormonal contraceptive failure with increasing BMI is not well understood, but is extremely important as the epidemic of obesity continues to grow, and pregnancy in this population is associated with significant maternal and neonatal morbidity. (17–22) Although there may be sound biologic plausibility for theories of increased failure rates among obese females, (10, 23) we did not find clinically important differences in contraceptive failure rates with increasing BMI.
Our findings support previous studies that have been limited by self-reported BMI and contraceptive use, as well as small numbers of obese subjects. (24–26) One possible explanation for the similar effectiveness of combined hormonal contraceptives is that fertility is reduced with increasing BMI. (22, 27–29) The contraceptive efficacy of the pill, patch, or vaginal ring in overweight and obese females, even if reduced compared to normal weight females, results in similar levels of pregnancy protection to that of a normal weight woman with intact fertility. Although understanding the mechanism by which reversible contraceptives work in obese females may be important, it is more critical to be able to assure females that their risk of pregnancy when using these methods is not increased because of their BMI.
Strengths of our study include the large sample size of overweight and obese females, prospective design, objective assessment of weight and BMI, and prospective assessment of contraceptive failures. There are few reports assessing clinical outcomes in females greater that 130% of ideal body weight and this study begins to fill that knowledge gap. The prospective design of the Contraceptive CHOICE Project incorporates assessment of contraceptive use through different sources (frequent subjective follow-up surveys, and objective pharmacy data). Coupling this with low rates of loss to follow-up (18% at 3 years) allowed for accurate classification of typical (real world) method-failure pregnancies.
Our study is not without limitations. As an observational study, the possibility of residual confounding still exists. The number of patch users in our cohort is limited, and these females have different demographic characteristics than pill or vaginal ring users. In addition, the demographic characteristics of CHOICE participants may differ from other populations, in turn limiting the generalizability of our findings. However, our adjusted analysis demonstrated no effect of BMI on contraceptive effectiveness even after controlling for baseline differences. The sample size of our BMI groups exceeded the calculated sample size required to detect a clinically significant two-fold difference, with the exception of the morbidly obese group (BMI ≥ 40). This group contributed 124 female years of pill, patch, or ring use, translating into a power of 68% to detect a twofold difference in contraceptive failures in this group. It is important to note that there were only four contraceptive failures in the morbidly obese group using combined hormonal contraception over the three years. As is true with many contraceptive studies, we have relied on self-reported correct use of the method. Females experiencing pregnancy in the CHOICE Project were asked if the pregnancy was planned and if unplanned, what method of contraception they were using at the time. Those reporting no method use were excluded from the analysis. Additionally, we do not have information of specific oral contraceptive dosing. It is reasonable to think that pills with lower ethinyl estradiol could be less effective in females as BMI increases. Lastly, pregnancy risk is affected by many things including frequency of sexual activity. We did not present data on the frequency of intercourse among all females in the CHOICE Project by BMI; however, previous research has shown no differences in sexual behaviors between BMI categories. (30)
In conclusion, our findings are encouraging in that we found there is no difference in failure rates among overweight, obese, and morbidly obese contraceptive pill, patch, or vaginal ring users. Based on this data, there is no evidence to support a change in contraceptive counseling for females based on BMI alone. However, we have previously shown that failure rates for these methods are far greater than long-acting reversible contraceptive (LARC) methods such as the implant and intrauterine device; (31) thus, LARC methods should be first-line contraceptive options for all females. The contraceptive pill, patch, and ring remain excellent second-tier methods. Overweight and obese females do not appear to be at increased risk of contraceptive failure when using combined oral contraceptive pills, patch, or vaginal ring.
Acknowledgments
The Contraceptive CHOICE Project is funded by the Susan Thompson Buffett Foundation. This research is also supported in part by the Washington University Institute of Clinical and Translational Sciences National Center for Research Resources (NCRR) grant UL1 RR024992 from the National Center for Advancing Translational Sciences, and the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number T32HD055172.
Footnotes
Financial Disclosure: Dr. Madden is a former speaker for Bayer HealthCare Pharmaceuticals. The other authors did not report any potential conflicts of interest.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. Jama. 2010;303(3):235–41. doi: 10.1001/jama.2009.2014. Epub 2010/01/15. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Report of a WHO Consultation of Obesity. Geneva -J; Obesity: Preventing and Managing the Global Epidemic. [PubMed] [Google Scholar]
- 3.Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84(5):478–85. Epub 2011/10/25. [Google Scholar]
- 4.Dinger JC, Cronin M, Mohner S, Schellschmidt I, Minh TD, Westhoff C. Oral contraceptive effectiveness according to body mass index, weight, age, and other factors. American journal of obstetrics and gynecology. 2009;201(3):263, e1–9. doi: 10.1016/j.ajog.2009.03.017. Epub 2009/06/02. [DOI] [PubMed] [Google Scholar]
- 5.Trussell J, Schwarz EB, Guthrie K. Obesity and oral contraceptive pill failure. Contraception. 2009;79(5):334–8. doi: 10.1016/j.contraception.2008.11.017. Epub 2009/04/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Westhoff CL, Hait HI, Reape KZ. Body weight does not impact pregnancy rates during use of a low-dose extended-regimen 91-day oral contraceptive. Contraception. 2012;85(3):235–9. doi: 10.1016/j.contraception.2011.08.001. Epub 2011/11/10. [DOI] [PubMed] [Google Scholar]
- 7.Lopez LM, Grimes DA, Chen-Mok M, Westhoff C, Edelman A, Helmerhorst FM. Hormonal contraceptives for contraception in overweight or obese women. Cochrane Database Syst Rev. 2010;(7):CD008452. doi: 10.1002/14651858.CD008452.pub2. Epub 2010/07/09. [DOI] [PubMed] [Google Scholar]
- 8.Holt VL, Scholes D, Wicklund KG, Cushing-Haugen KL, Daling JR. Body mass index, weight, and oral contraceptive failure risk. Obstet Gynecol. 2005;105(1):46–52. doi: 10.1097/01.AOG.0000149155.11912.52. Epub 2004/12/31. [DOI] [PubMed] [Google Scholar]
- 9.Creinin MD, Roberts E. Body mass index, weight, and oral contraceptive failure risk. Obstet Gynecol. 2005;105(6):1492. doi: 10.1097/01.AOG.0000162541.05836.45. author reply-3. Epub 2005/06/04. [DOI] [PubMed] [Google Scholar]
- 10.Cheymol G. Effects of obesity on pharmacokinetics implications for drug therapy. Clinical pharmacokinetics. 2000;39(3):215–31. doi: 10.2165/00003088-200039030-00004. Epub 2000/10/06. [DOI] [PubMed] [Google Scholar]
- 11.Westhoff CL, Torgal AH, Mayeda ER, Pike MC, Stanczyk FZ. Pharmacokinetics of a combined oral contraceptive in obese and normal-weight women. Contraception. 2010;81(6):474–80. doi: 10.1016/j.contraception.2010.01.016. Epub 2010/05/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Westhoff CL, Torgal AH, Mayeda ER, Stanczyk FZ, Lerner JP, Benn EK, et al. Ovarian suppression in normal-weight and obese women during oral contraceptive use: a randomized controlled trial. Obstet Gynecol. 2010;116(2 Pt 1):275–83. doi: 10.1097/AOG.0b013e3181e79440. Epub 2010/07/29. [DOI] [PubMed] [Google Scholar]
- 13.Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. American journal of obstetrics and gynecology. 2010;203(2):115, e1–7. doi: 10.1016/j.ajog.2010.04.017. Epub 2010/06/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Madden T, Mullersman JL, Omvig KJ, Secura GM, Peipert JF. Structured contraceptive counseling provided by the Contraceptive CHOICE Project. Contraception. 2012 doi: 10.1016/j.contraception.2012.07.015. Epub 2012/09/11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. The international classification of adult underweight oaoatB. 2004 [cited 2012 June 12]; Available from: http://apps.who.int/bmi/index.jsp?introPage=intro_3.html.
- 16.Lin DY, Wei LJ. The robust inference for the Cox proportional hazards model. Journal of the American Statistical Association. 1989;84:1074–8. [Google Scholar]
- 17.Djelantik AA, Kunst AE, van der Wal MF, Smit HA, Vrijkotte TG. Contribution of overweight and obesity to the occurrence of adverse pregnancy outcomes in a multi-ethnic cohort: population attributive fractions for Amsterdam. BJOG: an international journal of obstetrics and gynaecology. 2012;119(3):283–90. doi: 10.1111/j.1471-0528.2011.03205.x. Epub 2011/12/16. [DOI] [PubMed] [Google Scholar]
- 18.Zander-Fox DL, Henshaw R, Hamilton H, Lane M. Does obesity really matter? The impact of BMI on embryo quality and pregnancy outcomes after IVF in women aged </=38 years. The Australian & New Zealand journal of obstetrics & gynaecology. 2012;52(3):270–6. doi: 10.1111/j.1479-828X.2012.01453.x. Epub 2012/06/15. [DOI] [PubMed] [Google Scholar]
- 19.Van Lieshout RJ, Taylor VH, Boyle MH. Pre-pregnancy and pregnancy obesity and neurodevelopmental outcomes in offspring: a systematic review. Obesity reviews: an official journal of the International Association for the Study of Obesity. 2011;12(5):e548–59. doi: 10.1111/j.1467-789X.2010.00850.x. Epub 2011/03/19. [DOI] [PubMed] [Google Scholar]
- 20.Narchi H, Skinner A. Overweight and obesity in pregnancy do not adversely affect neonatal outcomes: new evidence. Journal of obstetrics and gynaecology: the journal of the Institute of Obstetrics and Gynaecology. 2010;30(7):679–86. doi: 10.3109/01443615.2010.509824. Epub 2010/10/12. [DOI] [PubMed] [Google Scholar]
- 21.Joy S, Istwan N, Rhea D, Desch C, Stanziano G. The impact of maternal obesity on the incidence of adverse pregnancy outcomes in high-risk term pregnancies. American journal of perinatology. 2009;26(5):345–9. doi: 10.1055/s-0028-1110084. Epub 2008/12/11. [DOI] [PubMed] [Google Scholar]
- 22.Reece EA. Perspectives on obesity, pregnancy and birth outcomes in the United States: the scope of the problem. American journal of obstetrics and gynecology. 2008;198(1):23–7. doi: 10.1016/j.ajog.2007.06.076. Epub 2008/01/02. [DOI] [PubMed] [Google Scholar]
- 23.Cheymol G. Drug pharmacokinetics in the obese. Fundamental & clinical pharmacology. 1988;2(3):239–56. doi: 10.1111/j.1472-8206.1988.tb00635.x. Epub 1988/01/01. [DOI] [PubMed] [Google Scholar]
- 24.Brunner Huber LR, Toth JL. Obesity and oral contraceptive failure: findings from the 2002 National Survey of Family Growth. Am J Epidemiol. 2007;166(11):1306–11. doi: 10.1093/aje/kwm221. Epub 2007/09/06. [DOI] [PubMed] [Google Scholar]
- 25.Brunner LR, Hogue CJ. The role of body weight in oral contraceptive failure: results from the 1995 national survey of family growth. Annals of epidemiology. 2005;15(7):492–9. doi: 10.1016/j.annepidem.2004.10.009. Epub 2005/07/21. [DOI] [PubMed] [Google Scholar]
- 26.Kaneshiro B, Edelman A, Carlson N, Nichols M, Jensen J. The relationship between body mass index and unintended pregnancy: results from the 2002 National Survey of Family Growth. Contraception. 2008;77(4):234–8. doi: 10.1016/j.contraception.2007.10.012. Epub 2008/03/18. [DOI] [PubMed] [Google Scholar]
- 27.Chavarro JE, Ehrlich S, Colaci DS, Wright DL, Toth TL, Petrozza JC, et al. Body mass index and short-term weight change in relation to treatment outcomes in women undergoing assisted reproduction. Fertility and sterility. 2012 doi: 10.1016/j.fertnstert.2012.04.012. Epub 2012/05/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rich-Edwards JW, Spiegelman D, Garland M, Hertzmark E, Hunter DJ, Colditz GA, et al. Physical activity, body mass index, and ovulatory disorder infertility. Epidemiology. 2002;13(2):184–90. doi: 10.1097/00001648-200203000-00013. Epub 2002/03/07. [DOI] [PubMed] [Google Scholar]
- 29.Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC. Diet and lifestyle in the prevention of ovulatory disorder infertility. Obstet Gynecol. 2007;110(5):1050–8. doi: 10.1097/01.AOG.0000287293.25465.e1. Epub 2007/11/06. [DOI] [PubMed] [Google Scholar]
- 30.Kaneshiro B, Jensen JT, Carlson NE, Harvey SM, Nichols MD, Edelman AB. Body mass index and sexual behavior. Obstet Gynecol. 2008;112(3):586–92. doi: 10.1097/AOG.0b013e31818425ec. Epub 2008/09/02. [DOI] [PubMed] [Google Scholar]
- 31.Winner B, Peipert JF, Zhao Q, Buckel C, Madden T, Allsworth JE, et al. Effectiveness of long-acting reversible contraception. The New England journal of medicine. 2012;366(21):1998–2007. doi: 10.1056/NEJMoa1110855. Epub 2012/05/25. [DOI] [PubMed] [Google Scholar]