Abstract
Acute appendicitis is one of the most common emergencies handled by a surgeon. Various aetiologies of acute appendicitis have been proposed but none have been proved. Trauma too has been proposed as a cause of acute appendicitis. Here we present a case of blunt trauma abdomen which was explored to rule out a perforation of hollow viscous organ and haemoperitoneum, but at the time of exploration a perforated appendicitis was found. The chronological order of events points towards blunt trauma as the probable cause of this appendicitis. This case also highlights the fact that even if trauma was not the cause of acute appendicitis, acute appendicitis should still be kept in the differential diagnosis of a patient presenting with pain in the right lower abdomen and a history of trauma.
Background
In young adults the most common cause of acute abdomen is acute appendicitis.1 Various aetiologies of acute appendicitis have been proposed but none have been proved. Trauma has also been proposed as one of the aetiologies.2 We present a case of appendicitis following trauma which was diagnosed preoperatively by senior surgeons as a case of post-traumatic pneumohaemoperitoneum. The chronological events of this case point towards trauma as the most probable cause of this acute appendicitis.
Case presentation
A 12-year-old boy presented with painful abdomen following a blunt trauma to his right lower abdomen from a desk's corner. The trauma occurred 2 days previously while playing in school. Mild pain started in the periumbilical region 1 day after the trauma which soon became profound and diffuse in nature. There was a history of mild fever from the first post-traumatic day. There was no history of vomiting.
At the time of presentation, the patient was toxic. His pulse was 114/min. The blood pressure was 90/56 mm Hg. Mild pallor was present. Abdominal examination was carried out. The abdomen was flat with no distension. Movement with respiration was minimal in all the four quadrants. A small 3×4 cm bluish-coloured bruise over the right lower abdomen region was observed. On palpation, the whole abdomen was tender. Guarding and rigidity were present all over the abdomen. The patient had passed urine and stool in the morning.
Investigations
His routine blood examination showed haemoglobin=10.5 g/dL; total leucocyte count was 17 000/mm3. His ultrasonography (figure 1) carried out outside the hospital and in the hospital showed fluid in the pelvis suggestive of haemoperitoneum. Straight X-ray abdomen erect posture showed gas under the diaphragm (figure 2).
Figure 1.
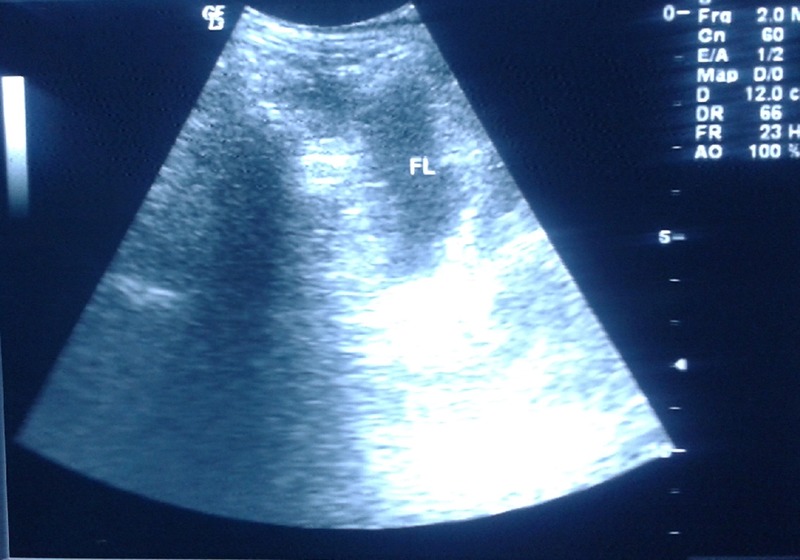
Ultrasonoghraphic picture showing free fluid in the abdomen with internal granular echoes suggestive of haemoperitoneum.
Figure 2.

Straight X-ray abdomen in erect posture showing pneumoperitoneum under the right diaphragm.
Differential diagnosis
The differential diagnoses that were considered were hollow visceral perforation with or without solid organ injury and mesenteric tear.
Treatment
Since the patient had features of early shock, he was resuscitated first. Owing to features of early shock, haemoperitoneum and peritonitis, an emergency exploratory laparotomy was carried out at midnight. Median laparotomy was carried out in the emergency operation theatre. On exploration, about 50 mL of pus was found in the pelvis. After wash, the vermiform appendix was found to be adhered to the caecum and the ascending colon. The tip was found to be perforated (figures 3 and 4). The surrounding area was found to have sloughed. Slough was removed and appendectomy carried out (figure 5). No other abnormality was found. The histopathological diagnosis was acute appendicitis.
Figure 3.
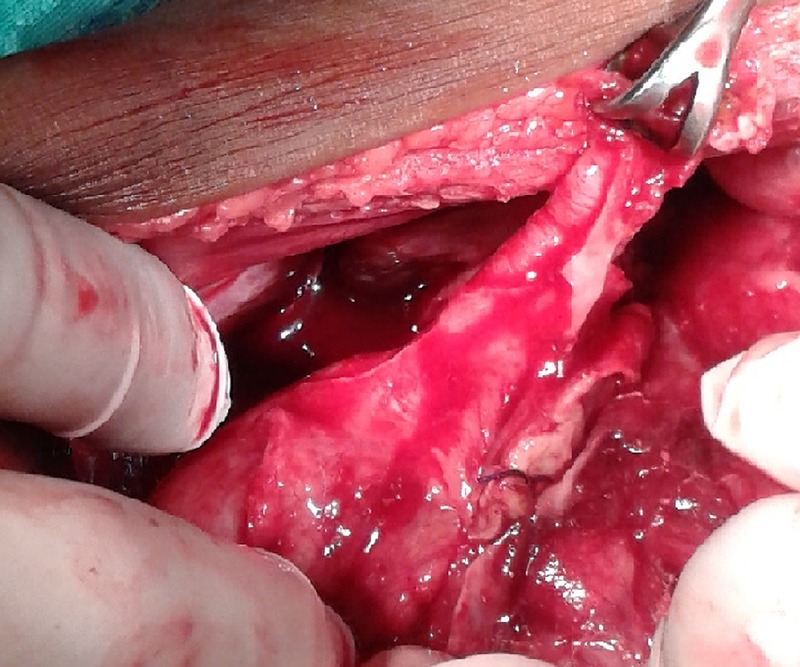
Exploratory laparotomy finding showing the perforated vermiform appendix.
Figure 4.
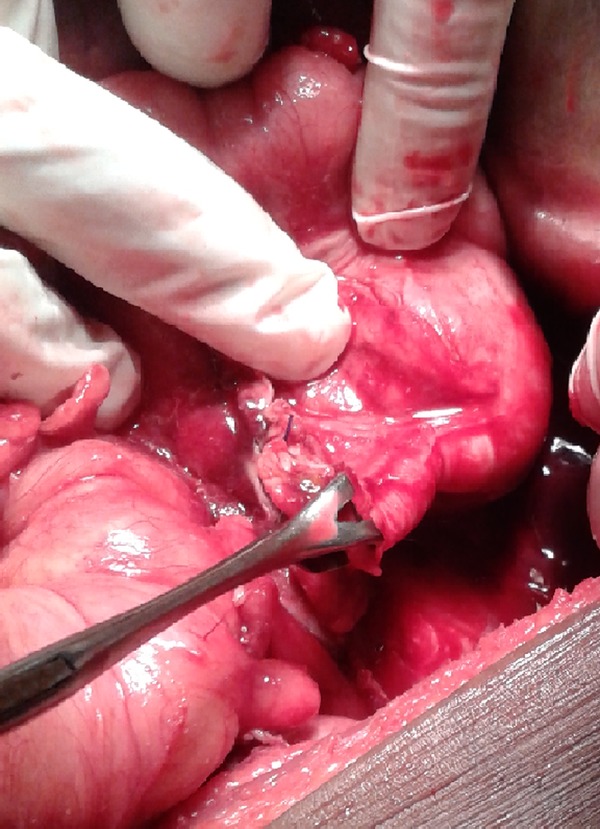
Perforation found at the tip of the vermiform appendix.
Figure 5.
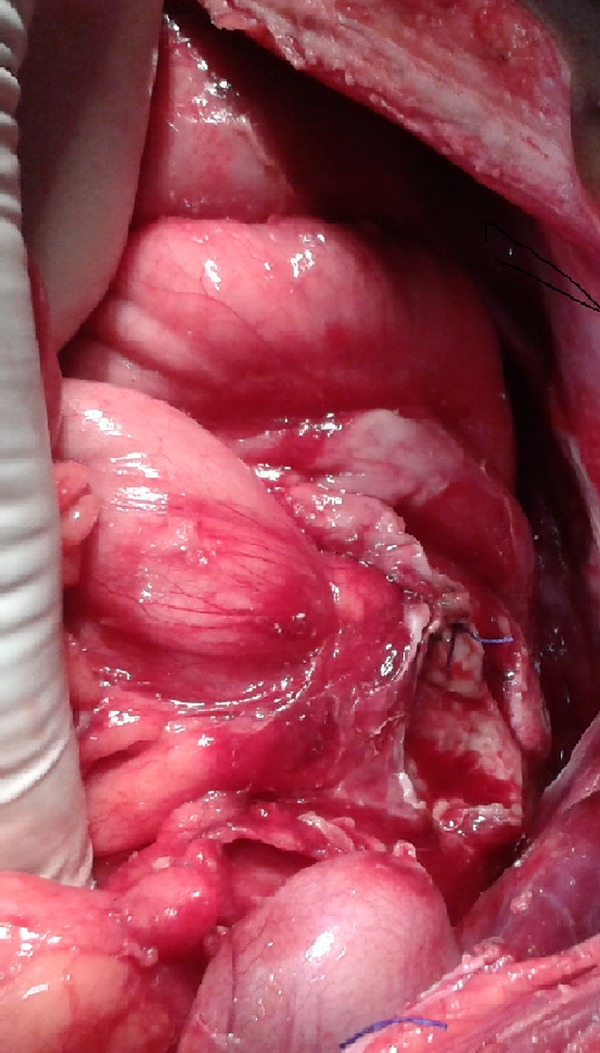
Necrosed base of the vermiform appendix and the caecum after appendectomy.
Outcome and follow-up
On the fourth postoperative day, the patient developed fever and skin erythema in the right lower quadrant. On examination, the surgical site was found to be indurated and tender. A diagnosis of superficial incisional surgical site infection was made. The patient was managed with immediate stitch removal and devitalised tissue debridement. It was followed by regular local dressing with povidone iodine and the patient was kept under antibiotic coverage. The patient recovered uneventfully. Three months postoperatively the patient was doing well.
Discussion
Acute appendicitis is one of the most common surgical emergencies encountered. The diagnosis of appendicitis is dependent on clinical parameters.1 Diagnosis may be difficult in cases of traumatic appendicitis. With the recent trend of conservative management of most of the non-severe traumas, delay in diagnosis of acute traumatic appendicitis is usual.
The pathogenesis of appendicitis is mainly twofold: obstructive and ischaemic. Trauma may cause inflammation of the vermiform appendix either by directly injuring the vermiform appendix or indirectly by compression of the vermiform appendix causing increase in intraluminal pressure leading to burst, by intramural haematoma causing narrowing and obstruction of the narrow lumen of the vermiform appendix, by oedema and obstruction of the appendiceal lumen due to fluid resuscitation, obstruction due to impacted stool and by microvascular tear causing ischaemia.3 4
The diagnostic criteria of traumatic appendicitis were enumerated by Shutkin and Wetzler as follows:
There must be absolute freedom from abdominal discomfort associated with pain, nausea, vomiting and tenderness before the trauma.
Direct trauma must be severe and forcible, involving the abdominal wall in the right half especially.
Indirect trauma must be violent, acute and unexpected.
Symptoms must appear immediately after the trauma.
Symptoms must be persistent and progressive, assuming the symptoms and signs of acute appendicitis.
The pathological findings must indicate a suppurative, destructive or necrotic process.5
Although Serour et al6 believed that trauma was very unlikely as a cause of acute appendicitis because of the small size and high mobility of the vermiform appendix, this case fulfils most of the above-mentioned criteria.
Blunt trauma abdomen is a surgical emergency. Patients with blunt trauma who have features of peritonitis or whose focused assessment with sonography for trauma (FAST) shows free intraperitoneal fluid and are haemodynamically unstable (like our patient) require urgent laparotomy. If FAST is not available then diagnostic peritoneal lavage should be carried out. Other patients of blunt trauma abdomen should be evaluated with contrast-enhanced CT scan of the abdomen. Abdominal CT scan is the mainstay in the management of stable blunt trauma abdomen, but its use in the evaluation of hollow visceral perforation is doubtful. Hollow visceral perforation is suggested on the CT scan by bowel wall thickening, inflammation in the surrounding adipose tissue seen as stranding or presence of free intraperitoneal fluid. A CT scan of the abdomen showing free fluid in the abdomen with no solid organ injury also creates a doubt in the minds of the surgeon. It is suggestive of mesenteric tear and may require emergency laparotomy.7 The role of laparoscopy in blunt trauma is not well established. Although earlier reports questioned its efficacy, some recent reports have supported its use.8 Diagnostic laparoscopy can be used in patients with blunt trauma who are haemodynamically stable with equivocal findings on CT scan of the abdomen, patients with penetrating trauma of the abdomen and patients with suspected diaphragmatic injury. Such patients need to be observed cautiously in the postoperative period for any missed injuries. The main limitations of diagnostic laparoscopy are that it cannot be used in patients with haemodynamic instability and in patients with late peritonitis, and a high level of laparoscopic expertise is needed.9–11
The present case was a rare case of traumatic appendicitis which was misdiagnosed as traumatic pneumohaemoperitoneum. CT scan and diagnostic laparoscopy were not used as the patient had features of haemodynamic instability. Any further delay in laparotomy would have been catastrophic for the patient. Even if trauma is not the causative factor, we would like to bring to the notice of surgical community the fact that appendicitis and trauma may coexist and surgeons should not rule out appendicitis as a cause of acute abdomen in a patient with a history of blunt trauma.
Learning points.
Trauma can cause appendicitis by direct or indirect methods.
Acute appendicitis can coexist with a history of trauma.
Urgent exploration is the treatment of choice for traumatic appendicitis.
Patients with blunt trauma abdomen with late peritonitis or haemodynamic instability require urgent exploratory laparotomy.
Footnotes
Contributors: All the four authors were actively involved in acquisition of the data, conception and design of the article and the final version was approved by all the four authors.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.O'Connell P R. The vermiform appendix. In: Williams NS, Bulstrode CJK, O'Connell PR, eds Bailey and Love's short practice of surgery. 25th edn New York: Arnold, 2008:1205 [Google Scholar]
- 2.Sumer A, Caglayan K, Altinli E, et al. Posttraumatic perforated appendicitis: a case report. Israeli J Emerg Med 2008;8:23–6 [Google Scholar]
- 3.Husham A, Sheikha AL T, Sebastian M, et al. Traumatic appendicitis: a case report. Panam J Trauma Crit Care Emerg Surg 2012;1:48–9 [Google Scholar]
- 4.Hennington MH, Tinsley EA, Jr, Proctor HJ, et al. Acute appendicitis following blunt abdominal trauma. Incidence or coincidence? Ann Surg 1999;214:61–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Torres-Grau J, Monkhouse SJW. Trauma induced appendicitis…a real entity. Am Med J 2012;3:124–5 [Google Scholar]
- 6.Serour F, Efrati Y, Klin B, et al. Acute appendicitis following abdominal trauma. Arch Surg 1996;131:785–6 [DOI] [PubMed] [Google Scholar]
- 7.Hoyt DB, Coimbra R, Acosta J. Management of acute trauma. In: Townsend CM, Jr, Beauchamp RD, Evers BM, Mattox KL. eds. Sabiston Textbook of Surgery. 18th edn. The Saunders; 2008:837–42 [Google Scholar]
- 8.Teamma MS. Evaluation of laparoscopy in the management of abdominal emergencies. J Arab Soc Med Res 2013;8:19–25 [Google Scholar]
- 9.Feliz A, Shultz B, McKenna C, et al. Diagnostic and therapeutic laparoscopy in pediatric abdominal trauma. J Pediatr Surg 2006;41:72–7 [DOI] [PubMed] [Google Scholar]
- 10.Fabiani P, Iannelli A, Mazza D, et al. Diagnostic and therapeutic laparoscopy for stab wounds of the anterior abdomen. J Laparoendosc Adv Surg Tech A 2003;13:309–12 [DOI] [PubMed] [Google Scholar]
- 11.Chol YB, Lim KS. Therapeutic laparoscopy for abdominal trauma. Surg Endosc 2003;17:421–7 [DOI] [PubMed] [Google Scholar]


