Abstract
We describe the case of a 65-year-old patient who was admitted to our tertiary centre with cardiac sounding chest pain and inferior ST elevation. Coronary angiography revealed mild plaque disease in the left anterior descending artery. The right coronary artery was smooth with no plaques with the exception of an occluded distal branch with no flow. The left ventriculogram revealed a ballooned and akinetic apex typical of Takotsubo syndrome (TS). We suspected a coronary embolus secondary to TS. A serial rise and fall in biomarkers of myocardial necrosis was noted. The patient was treated for acute coronary syndrome and discharged home 72 h from admission. Distal thromboembolism has been described in the literature before. On a search of PubMed there are no examples of coronary artery embolus in the context of TS.
Background
Broken heart syndrome more commonly known as Takotsubo syndrome (TS) or stress-induced cardiomyopathy is described as transient depression in left ventricular systolic function frequently related to emotional stress.1 Typical TS describes apical and mid-left ventricular wall depression creating a ballooning of the ventricular apex with systole. In atypical TS ventricular impairment is restricted to the mid-left ventricular wall with sparing of the apex. Up to one-third of patients may have both ventricles affected.2 3 The prevalence of TS is currently unknown although may account for up to 2.5% of all patients presenting with clinically suspected ST elevation myocardial infarction (STEMI).4
Emotional stressors are thought to be responsible for promoting microvascular dysfunction or spasm involved with the pathogenesis of TS. Evidence for catelcholamine-induced cardiomyopathy comes from a case series where plasma catecholamine concentrations were measured at presentation.5 The presentation of TS can mimic that of STEMI.4 5 Indeed Ksuge et al6 report a vast range of ECG abnormalities and attempt to quantify criteria to differentiate acute anterior MI and TS. However, conclusions drawn from this report suggest that ECG is unreliable in the diagnosis of TS.
Complications include cardiogenic shock, tachy/bradyarrythmias, heart failure and left ventricular thrombus.
Case presentation
A 65-year-old woman with hypertension and hypercholesterolaemia presented with cardiac sounding chest pain. She had recently stopped taking simvastatin due to myalgia but was on other appropriate primary prevention treatment. She was also an ex-smoker having stopped 35 years previously.
The ambulatory ECG revealed ST elevation of more than 2 mm in the inferior leads. As per local policy, she was thrombolysed with tenecteplase at the scene and transferred to the local hospital. On arrival her chest pain persisted and was associated with persistent ST elevation in inferior leads (figure 1). Following further medical therapy with vasodilators, she was transferred for rescue angioplasty to our tertiary centre.
Figure 1.
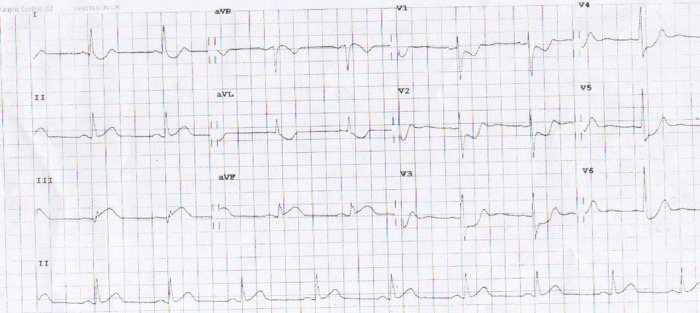
Initial ECG.
Coronary angiography revealed mild plaque disease in the left anterior descending coronary artery and a normal left circumflex coronary artery (figure 2). The right coronary artery (RCA) was smooth with no plaques with the exception of an occluded distal branch with no flow (figure 3 and video 1). A left ventriculogram revealed a ballooned and akinetic apex typical of TS (TS; video 2).
Figure 2.
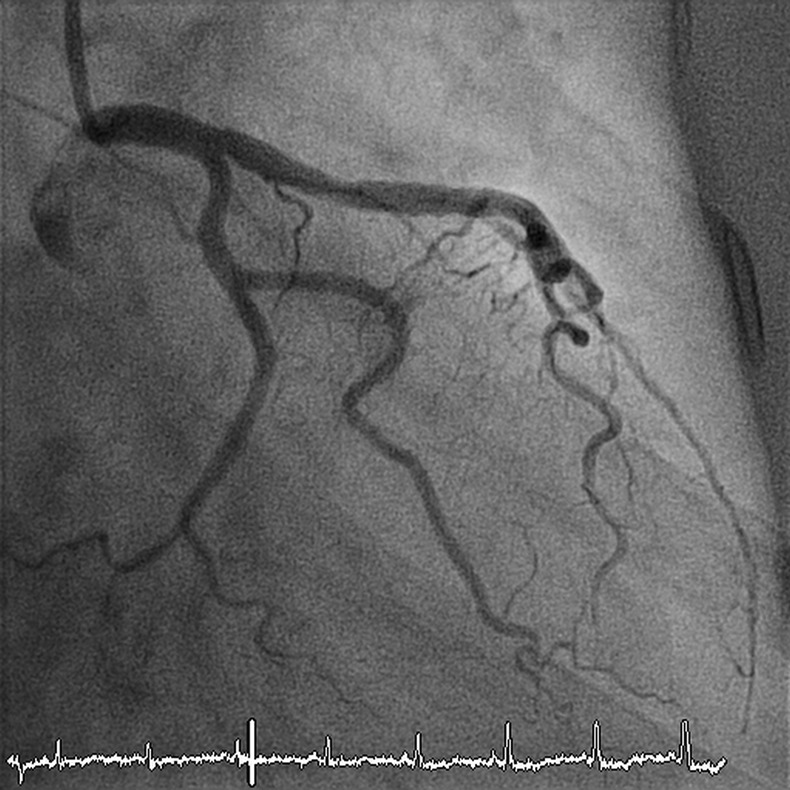
The left coronary circulation.
Figure 3.
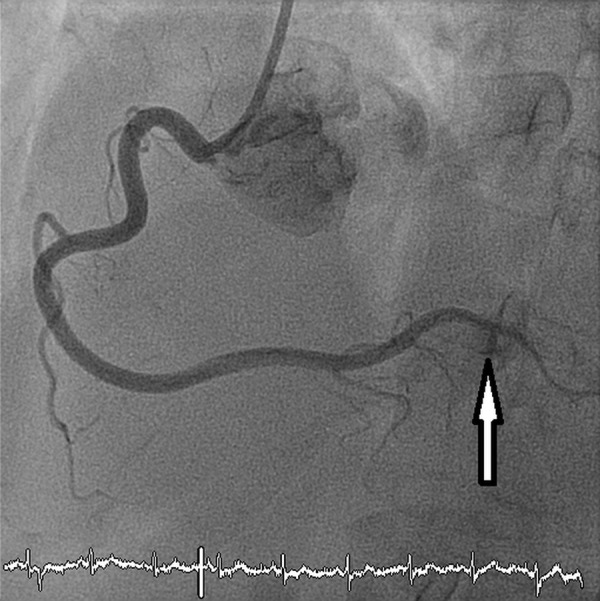
The right coronary circulation with occluded distal branch.
Right coronary circulation with occluded distal branch.
Left ventriculogram showing classic appearance of TS.
A coronary embolus secondary to TS was suspected. A serial rise and fall in biomarkers of myocardial necrosis was noted, with initial creatine kinase (CKMB) 28 µg/L rising to 110 µg/L approximately 8 h later and falling to 36 µg/L 24 h later. Echocardiography performed 48 h after admission showed resolution of the regional wall motion abnormalities seen on the left ventriculogram. Subsequent ECGs showed a resolution of inferior ST elevation.
The patient was treated for acute coronary syndrome with standard medical therapy. Formal anticoagulation was not deemed necessary due to resolution of the regional wall motion abnormalities. The patient was discharged home after 72 h with follow-up echocardiography arranged for 6 weeks postdischarge.
Discussion
Distal thromboembolism in patients with TS is rare but has been described in the literature before.7 8 The transient regional wall abnormality with subsequent improvement in apical hypokinesia would encourage distal embolisation of intraventricular thrombus. In this case the combination of inferior ST elevation and the timing of elevated cardiac enzymes illustrates that the occluded distal RCA branch was the responsible lesion. The left ventricular angiogram showed classical apical ballooning associated with Takotsubo. From the angiographic findings and elevated cardiac marker we can deduce that the acute coronary event was a probable consequence of left ventricular thrombus formation and subsequent embolisation.
The evidence for incidence of thromboembolism in the context of TS is variable. Mistuma et al9 describe a series of 21 patients with TS in whom thromboembolism was detected in three patients (14%). In their systematic review De Gregorio et al10 report 15 patients in whom ventricular thrombus was detected (2.5% of patients with TS). Five went on to develop cardioembolic complications (representing 0.8% of known population).
On a search of PubMed there are 839 case reports of TS but none describing coronary artery embolus in the context of apical ballooning syndrome.
Unfortunately TS mimics acute coronary syndromes in clinical features and ECG changes. Early echocardiography could be used to assess for the characteristic apical ballooning but should not prevent or be used as an alternative to immediate angiography. In the setting of typical clinical features and ST elevation on ECG emergency coronary angiography should remain the investigation of choice. Thankfully thrombus formation and embolisation remains an extremely rare complication of TS.
Learning points.
Takotsubo syndrome (TS) can be associated with left ventricular thrombus formation and subsequent embolisation.
Coronary embolisation has not previously been described.
Takotsubo cardiomyopathy is responsible for up to 2.5% of admissions for clinically suspected ST-elevation myocardial infarction 's.
ECG criteria/changes are an unreliable tool to diagnose TS.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Novo S, Akashi Y, Arbustini E, et al. Takotsubo cardiomyopathy: a consensus document. G Ital Cardiol (Rome) 2008;9:785–97 [PubMed] [Google Scholar]
- 2.Eitel I, von Knobelsdorff-Brenkenhoff F, Bernhardt P, et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (takotsubo) cardiomyopathy. JAMA 2011;306:277. [DOI] [PubMed] [Google Scholar]
- 3.Haghi D, Athanasiadis A, Papavassiliu T, et al. Right ventricular involvement in takotsubo cardiomyopathy. Eur Heart J 2006;27:2433–9 [DOI] [PubMed] [Google Scholar]
- 4. doi: 10.1016/j.ijcard.2007.07.002. Pilgrim TM, Wyss TR. Takotsubo Cardiomyopathy or Transient Left Ventricular Apical Ballooning Syndrome: A Systematic Review. Int J Cardiol 2008;124:283–92. [DOI] [PubMed] [Google Scholar]
- 5.Gianni M, Dentali F, Grandi AM, et al. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J 2006;27:1523. [DOI] [PubMed] [Google Scholar]
- 6.Ksuge M, Ebina T, Hibi K, et al. Simple and accurate electrocardiographic criteria to differentiate TS cardiomyopathy from anterior acute MI. JACC 2010; 55:2514–16 [DOI] [PubMed] [Google Scholar]
- 7.Y-Hassan S, Shahgaldi K. Thrombo-Embolic renal infarction in a case of mid-ventricular takotsubo syndrome. Intern Med 2011;50:2175–8 [DOI] [PubMed] [Google Scholar]
- 8.Yoshimura S, Toyoda K, Ohara T, et al. Takotsubo cardiomyopathy in acute stroke. Ann Neurol 2008;64:547–54 [DOI] [PubMed] [Google Scholar]
- 9.Mistuma W, Kodoma M, Ito M, et al. Thromboembolism in TS cardiomyopathy. Int J Cardiol 2010;18:98–100 [DOI] [PubMed] [Google Scholar]
- 10.De Gregorio C, Grimaldi P, Lentini C. Left ventricular thrombus formation and cardioembolic complications in patients with takotsubo-like syndrome: a systematic review. Int J Cardiol 2008;131:18–24 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Right coronary circulation with occluded distal branch.
Left ventriculogram showing classic appearance of TS.


