Abstract
Background
Of patients undergoing cardiac surgery in the United States, 15–20% are re-hospitalized within 30-days. Current models to predict readmission have not evaluated the association between severity of post-operative acute kidney injury (AKI) and 30-day readmissions.
Methods
We collected data from 2,209 consecutive patients who underwent either coronary artery bypass (CABG) or valve surgery at seven member hospitals of the Northern New England Cardiovascular Disease Study Group Cardiac Surgery Registry (NNE) between July 2008 and December 2010. Administrative data at each hospital was searched to identify all patients readmitted to the index hospital within 30 days of discharge. We defined AKI Stages by the AKI Network definition of 0.3 or 50% increase (Stage 1), 2-fold increase (stage 2) and a 3-fold or 0.5 increase if the baseline serum creatinine was at least 4.0 (mg/dL) or new dialysis (stage 3). We evaluate the association between stages of AKI and 30-day readmission using multivariate logistic regression.
Results
There were 260 patients readmitted within 30-days (12.1%). The median time to readmission was 9 (IQR 4–16) days. Patients not developing AKI following cardiac surgery had a 30-day readmission rate of 9.3% compared to patients developing AKI stage 1 (16.1%), AKI stage 2 (21.8%) and AKI stage 3 (28.6%, p <0.001). Adjusted odds ratios for AKI stage 1 (1.81; 1.35, 2.44), stage 2 (2.39; 1.38, 4.14) and stage 3 (3.47; 1.85–6.50). Models to predict readmission were significantly improved with the addition of AKI stage (c-statistic 0.65, p = 0.001) and net reclassification rate of 14.6% (95%CI: 5.05% to 24.14%, p = .003).
Conclusions
In addition to more traditional patient characteristics, the severity of post-operative AKI should be used when assessing a patient’s risk for readmission.
Subject Codes: Coronary artery bypass grafts; CABG; Kidney; renal function; failure; dialysis; Outcomes (incl mortality, morbidity, survival, etc.); Surgery; complications; Readmission
Introduction
One in every five patients return to the hospital within 30-days for unplanned readmissions. [1] Current models to predict the occurrence of 30-day readmission with patient characteristics have been met with limited success. [2] Others have explored the use of less traditional risk factors for readmission such as discharge hemoglobin and serum sodium. [3] One common adverse outcome in open heart surgery patients is acute kidney injury (AKI), which has been directly tied to short- and long-term mortality after cardiac surgery [4, 5] and associated with readmissions in patients hospitalized with heart failure [6] or acute myocardial infarction. [7] However, other studies have not identified an association between increased severity of AKI and an increased likelihood of readmission.
AKI may serve as a risk factor for other organ injury. [8] Scheel and colleagues demonstrate markers of cellular injury in other organs following acute injury to the kidneys including the heart, brain, liver, gut, bone, and lungs. [9] Injury or failing of these organs - specifically circulatory issues and heart failure, infection, digestive system, fluid and electrolyte imbalance, and anemia – have also been associated with a higher rates of 30-day readmission after cardiac surgery. [10]
Some studies have reported post-procedure acute kidney injury or renal failure as a significant risk factor for 30-day readmissions. [6, 11, 12] However, no report has evaluated a severity index for AKI using the Acute Kidney Injury Network (AKIN) [13] staging criteria as a risk marker for determining early risk of 30-day readmission after cardiac surgery. Based on the evidence associating AKI to end-organ damage and end-organ damage with readmissions, we postulate severity of AKI using the AKIN staging criteria could serve as a risk factor for 30-day readmission. Therefore, we examined if post-cardiac surgery AKI stage (no AKI, AKI stage 1, stage 2, and stage 3) is associated with 30-day readmissions.
Material and Methods
Patients undergoing coronary artery bypass graft (CABG) surgery and/or valve surgery at any of 7 hospitals contributing 30-day readmission data to the Northern New England Cardiovascular Disease Study Group (NNE) between July 2008 and December 2010 were enrolled in the cohort. Readmissions were identified by searching administrative hospital claims and represent only readmissions to the index site. A total of 2,209 consecutive patients were included along with 268 readmissions to the hospital performing the index cardiac surgery. Twenty-six patients with incomplete pre-operative and postoperative serum creatinine measures were excluded from the analysis leaving a total of 2,183 patients and 260 readmissions occurring within 30-days of discharge from the index cardiac surgery admissions. An interdisciplinary team of physicians and allied health professionals from the NNE developed a systematic chart abstraction tool to standardize the collection of 30-day readmission events and causes of readmission. All institutional review boards for each center reviewed and approved the data collection for the NNE registry and supplementary data collection for readmissions.
The last serum creatinine prior to cardiac surgery and highest post-operative serum creatinine prior to discharge was used to define stage of AKI. AKI stages were defined by the AKI Network definitions as follows: AKIN Stage 1: 0.3 or 50% increase in serum creatinine from baseline; AKIN Stage 2: a 2-fold increase in serum creatinine; and AKIN Stage 3: a 3-fold or 0.5 increase if the baseline serum creatinine was at least 4.0 (mg/dL) or new dialysis-dependent renal failure. [13]
Baseline, operative, and postoperative outcomes were compared using chi-square tests and continuous data using the student’s t-test or Wilcoxon ranksum tests where appropriate. We conducted a backwards stepwise logistic regression removing risk factors that did not reach an alpha <0.1 among only risk factors with an alpha < 0.1 from univariate comparisons. All risk factors meeting an alpha < 0.1 were included in the final model. Two logistic regression models were created modeling the likelihood of 30-day readmission. First, we created a multivariate logistic regression model including other non-renal risk factors predictive of 30-day readmission. Then, we created a full model with AKIN stage added to the other model. To assess the calibration and discrimination ability of these models to predict 30-day readmission, we conducted a Hosmer-Lemeshow goodness of fit test and calculated the area under the receiver operating characteristic (ROC) curve and 95% confidence intervals for each of the three models. We then compared each model’s ROC to determine if the addition of AKIN stage to the risk factors in the first model significantly improved the discrimination of 30-day readmission using ROC comparative statistics described by DeLong and colleagues [14] and using the net reclassification index described by Pencina and colleagues. [15] All models were well calibrated plotting deciles of with observed verses expected values. We then conducted a sensitivity analysis modeling center as a random effect in a multilevel XTME logit model. All analyses were performed using Stata 11.2 (College Station, TX).
Results
There were 260 patients readmitted to their index hospital within 30-days (12.1%). The median time to readmission was 9 (IQR 4–16) days. Readmission rates by center ranged from 6.4% to 18.0%. Patient demographics and procedural characteristics are reported in Tables 1 and 2. The primary causes of readmissions included infections (24%), effusions (20%), and rhythm disturbances (16%) with secondary causes of readmission included congestive heart failure or shortness of breath (28%) and effusions (18%).
Table 1.
Characteristics of Patients With or Without 30-day Readmission
| Characteristic | 30-day Readmission | ||
|---|---|---|---|
| No | Yes | P-value | |
| Number of patients (2,183) | 1,923 | 260 | |
| Demographics | |||
| Age | 66 ± 11 | 67 ± 12 | 0.7 |
| Female | 29 | 33 | 0.2 |
| BMI | 30 ± 6 | 30 ± 7 | 0.6 |
| Comorbidites | |||
| Type 2 diabetes mellitus | 31 | 37 | 0.1 |
| Vascular disease | 27 | 31 | 0.2 |
| COPD | 16 | 20 | 0.044 |
| History of dialysis | 2 | 5 | 0.015 |
| Smoking | 21 | 22 | 0.7 |
| Cardiac History | |||
| Recent MI | 17 | 13 | 0.1 |
| CHF | 20 | 25 | 0.1 |
| Prior CABG | 4 | 3 | 0.3 |
| Prior Valve | 2 | 2 | 0.6 |
| Prior PCI | 18 | 17 | 0.7 |
| NYHA Class IV | 16 | 15 | 0.9 |
| Cardiac Anatomy and Function | |||
| Left main disease ≥ 50% | 29 | 21 | 0.007 |
| Single vessel disease | 32 | 40 | 0.009 |
| Two vessel disease | 27 | 28 | 0.7 |
| Three vessel disease | 36 | 25 | 0.001 |
| Ejection fraction | |||
| <40% | 11 | 12 | 0.9 |
| 40–59% | 13 | 11 | |
| 50–59% | 24 | 24 | |
| ≥60% | 52 | 53 | |
| Preoperative Labs | |||
| WBC >12,000 | 6 | 10 | 0.011 |
| eGFR (mL/min/m2) | 78 ± 24 | 75 ± 30 | 0.1 |
COPD: chornic obstructive pulmonary disease. MI: myocardial infarction. CHF: congestive heart failure. CABG:coronary artery bypass graft surgery. PCI: percutaneuos coronary intervention. WBC: white blood cell count. eGFR: estimated glomerular filtration rate.
Table 2.
Procedural Characteristics and Outcomes of Patients With or Without 30-day Readmission
| Characteristic | 30-day Readmission | ||
|---|---|---|---|
| No | Yes | P-value | |
| Procedural characteristics | |||
| Priority | |||
| Emergent | 5 | 6 | 0.5 |
| Urgent | 51 | 48 | |
| Elective | 44 | 46 | |
| Procedure | |||
| CABG | 61 | 51 | 0.007 |
| Valve | 22 | 30 | |
| CABG/valve | 17 | 19 | |
| On-pump proceedure | 90 | 96 | 0.004 |
| Nadir Hematocrit on pump <20 | 13 | 19 | 0.007 |
| Cardiopulmonary bypass time (min) | 120 ± 54 | 123 ± 56 | 0.4 |
| Time to initial extubation (min) | 17 ± 65 | 18 ± 35 | 1.0 |
| Intraoperative myocardial infarction | 2 | 3 | 0.8 |
| Return to bypass | 4 | 5 | 0.8 |
| Management | |||
| RBC Transfusions | |||
| None | 68 | 59 | 0.001 |
| One | 9 | 10 | |
| Two | 10 | 10 | |
| Three or more | 13 | 22 | |
| Use of 1 or more inotropes | |||
| Arrive to ICU | 44 | 44 | 1.0 |
| After 4 hours | 37 | 44 | 0.035 |
| After 48 hours | 11 | 15 | 0.1 |
| Acute Kidney Injury Severity | |||
| No AKI | 72 | 54 | <0.001 |
| Stage 1 | 23 | 32 | |
| Stage 2 | 4 | 7 | |
| Stage 3 | 2 | 6 | |
| Adverse Outcomes | |||
| Low-cardiac output failure | 8 | 10 | 0.3 |
| Stroke | 1 | 1 | 0.5 |
| Mediatinitis | 0 | 3 | <0.001 |
| Reintubation | 4 | 4 | 0.9 |
| Return to operating room for bleeding | 3 | 4 | 0.4 |
| New atrial fibrillation | 33 | 40 | 0.019 |
| Leg wound infection | 1 | 1 | 0.5 |
| Pneumonia | 2 | 1 | 0.3 |
CABG: coronary artery bypass graft surgery. RBC: packed red blood cell transfusion. ICU: intensive care unit.
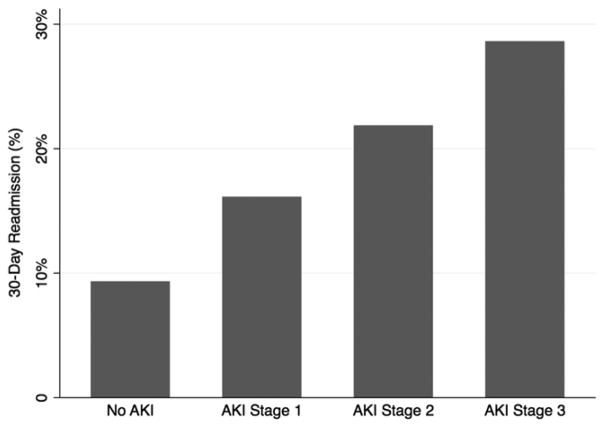
Patients without AKI following cardiac surgery had a 30-day readmission rate of 9.3% compared to patients developing AKI stage 1 (16.1%), AKI stage 2 (21.8%) and AKI stage 3 (28.6%, p <0.001, Figure 1). Compared to patients without AKI (referent category), the unadjusted odds ratios for AKI stage 1 was 1.81 (95%CI 1.35, 2.44), for stage 2 was 2.39 (95%CI 1.38, 4.14) and for stage 3 was 3.47 (95%CI 1.85–6.50). Patient and procedural characteristics predictive of 30-day readmission in a multivariate model without AKIN stage included pre-operative white blood cell count >12,000, number of disease vessels (1 or 2 compare to 3 vessel disease), on-pump surgery, nadir hematocrit on pump<20, and development of mediastinits. This model using other non-renal risk factors had a Hosmer-Lemeshow goodness of fit chi-square of 4.44 and p-value of 0.3 with a ROC curve of 0.60 (95%CI: 0.56, 0.63). We then tested the addition of AKIN stage to the multivariate model. We found that none of the other non-renal risk factors dropped out of the model and AKIN stage significantly improved the model’s ability to predict 30-day readmissions after cardiac surgery with p-value of 0.001. The final model combining the number of other risk factors from model 2 and the AKIN stages had a goodness of fit chi-square of 5.25 and p-value 0.4 with ROC 0.65 (95%CI: 0.61, 0.68). The net reclassification rate method also demonstrated significant model improvement of AKIN stage compared to other risk factors alone was 14.6% (95%CI: 5.05%, 24.14%, p = .003). Figure 2 presents the odds ratios for AKIN stage and other risk factors used to create the final model with AKIN stage. When center was used in a multilevel random effects model, the odds ratios for AKIN Stages 1, 2, and 3 compared to no AKI in the fully adjusted model remained consistent with odds ratios and 95% CIs as follows: 1.83 (1.35, 2.47), 2.47 (1.42, 4.30), and 3.33 (1.77, 6.28), respectively with all p-values <0.001.
Figure 1.
30-day readmission rates of patients without AKI, developing AKI stage 1, AKI stage 2 and AKI stage.
Figure 2.
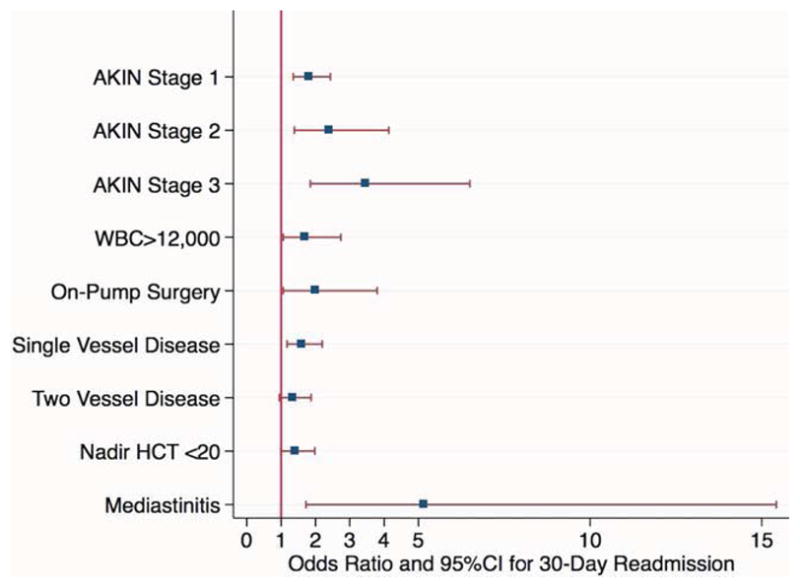
Odds ratios.
We explored the potential reasons for AKIN stage and readmission by summarizing the association between AKIN stage and important procedural characteristics and endpoints in Table 4. We also evaluated the AKIN stage assessed using the serum creatinine closest to discharge. AKIN stage closest to discharge had readmission rates for no AKI, and AKIN stages 1–3 as follows: 10%, 13%, 16%, 27%, respectively. Patients with full recovery of AKI prior to discharge still had high rates of readmission (21% verses 10%).
Table 4.
Procedural Characteristics and Outcomes of Patients With or Without Acute Kidney Injury
| Characteristic | No AKI | AKIN Stage
|
P-Value | ||
|---|---|---|---|---|---|
| AKI Stage 1 | AKI Stage 2 | AKI Stage 3 | |||
| Number of patients | 1518 | 522 | 87 | 56 | |
| Procedural characteristics | |||||
| Cardiopulmonary bypass time (min) | 117 ± 53 | 122 ± 51 | 136 ± 60 | 152 ± 82 | <0.001 |
| Time to initial extubation (min) | 14 ± 61 | 19 ± 36 | 33 ± 84 | 61 ± 159 | <0.001 |
| Intraoperative myocardial infarction | 2 | 3 | 3 | 2 | 0.766 |
| Return to bypass | 3 | 6 | 7 | 7 | 0.009 |
| Management | |||||
| RBC Transfusions | |||||
| None | 73 | 56 | 38 | 29 | <0.001 |
| One | 8 | 11 | 9 | 14 | |
| Two | 9 | 13 | 18 | 7 | |
| Three or more | 10 | 19 | 34 | 50 | |
| Use of 1 or more inotropes | |||||
| Arrive to ICU | 41 | 49 | 54 | 61 | <0.001 |
| After 4 hours | 34 | 45 | 45 | 55 | <0.001 |
| After 48 hours | 8 | 17 | 25 | 43 | <0.001 |
| Adverse Outcomes | |||||
| Low-cardiac output failure | 6 | 11 | 15 | 27 | <0.001 |
| New heart failure | 11 | 22 | 27 | 29 | <0.001 |
| Stroke | 1 | 1 | 1 | 2 | 0.921 |
| Mediatinitis | 0 | 1 | 1 | 5 | <0.001 |
| Reintubation | 1 | 6 | 14 | 27 | <0.001 |
| Return to operating room for bleeding | 3 | 4 | 5 | 7 | 0.317 |
| New atrial fibrillation | 29 | 40 | 56 | 57 | <0.001 |
| Leg wound infection | 0 | 1 | 5 | 2 | <0.001 |
| Pneumonia | 1 | 2 | 7 | 12 | <0.001 |
RBC: packed red blood cell transfusion. Low cardiac output failure is defined as receiving an intra- or post-operative intra-arterial balloon pump or use of 2 or more inotropes at 48 hours after surgery.
Comment
In this study we examined the relationship of AKIN stages to 30-day readmission following consecutive live discharges from cardiac surgery. We demonstrated that the risk of 30-day readmission incrementally increases with each increase in AKIN stage. This monotonic relationship was constant with and without adjustment for patient and procedural risk factors for 30-day readmission. We believe the use of AKIN staging criteria should be incorporated into risk models for 30-day readmission, while other novel risk factors should be considered and evaluated to continually improve the prediction of readmissions after cardiac surgery.
Thirty-day readmission rates have been targeted by the Centers for Medicare and Medicaid Services (CMS) as a quality measure. According to the Affordable Care Act (ACA), hospitals with higher than expected readmissions receive a financial penalty. [16] While financial incentives tied to readmissions may drive hospitals reduce to readmissions, concerns remain for the safety of patients as hospitals engage efforts to prevent these events.
AKI has been associated with cardiovascular disease and end-organ injury through the cardiorenal syndrome proposed by Ronco and colleagues. [8] Others have noted AKI and damage to renal tubular function is tied to distant end-organ injury including not only the heart, but other vital organs. [9] Karkouti and colleagues also reported a strong, yet modifiable, relationship between preoperative anemia and AKI in cardiac surgery. [17] We recently reported risk factors for AKI duration and identified important modifiable factors for AKI during cardiopulmonary bypass that protected against longer duration of AKI (cold blood cardioplegia, higher nadir hematocrit on bypass) and factors that increased the risk of longer durations of AKI (pump times exceeding 120 minutes and use of ultrafiltration). [18] Recent evidence targeting other perfusion characteristics demonstrates arterial outlet temperature, temperature on admission to the intensive care unit are important novel risk factors for developing AKI. [19] These postulated mechanisms are supported by our study whereby patients with a higher AKIN stage were more likely to have low cardiac output (6.1, 11.5, 14.9, and 26.8 percent), new heart failure (10.8, 22.1, 26.7, and 28.6 percent), higher baseline white blood cell counts (5.7, 4.6, 14.9, and 16.1 percent), and more in-hospital mediastinitis infections (0.3, 1.0, 1.2, and 5.4 percent) for no AKI and AKIN stage 1, 2, and 3, respectively. Based on previous studies and our current research, AKI appears to be tied to the risk of 30-day readmission through heart failure or low cardiac output, inflammation and infection.
We evaluated the predictive ability of an AKI severity index (AKIN stage) and likelihood of 30-day readmission across seven hospitals. We found AKIN stage to be a simple risk factor for evaluating perioperative risk of 30-day readmission. Although we are the first to report on the predictive ability of AKIN stage as a severity index for 30-day readmission, recent studies have supported the association between AKI and readmission predominately in patients hospitalized for heart failure. These reports have identified worsening renal function among patients hospitalized for heart failure has been predictive of mortality and 30-day heart failure readmissions. [20, 21] More recently, others have investigated AKI or the RIFLE criteria and their association with mortality and readmission. Thakar and colleagues also reported that patients hospitalized for heart failure and develop AKI were at a significant increased risk of readmission within 30-days (9.2% versus 6.0%, p=0.0003). [6] Shirakabe and colleagues reported the RIFLE criteria as significant independent risk factors for mortality or heart failure readmissions. [22] However, when heart failure readmissions were abstracted from the one-year events, the RIFLE criteria did not demonstrate a trend in rates of 1-year heart failure readmissions. Contrary to this report, our research supports the use of the AKIN staging criteria demonstrating a significant monotonic trend with stage of AKI and 30-day readmissions after live discharge from cardiac surgery.
Mild and moderate AKI has also been investigated in the ST-elevation myocardial infarction population with readmissions for heart failure, but not all readmissions. Goldberg and colleagues after statistical adjustment demonstrate a significant trend for both transient and persistent moderate to severe AKI (≥ 0.5 mg/dL increase in serum creatinine from baseline) compared to no AKI or mild AKI (≥ 0.3 mg/dL increase in serum creatinine from baseline) and subsequent heart failure admissions – but not recurrent infarctions - after an acute myocardial infarction index hospitalization. [7] Recently, Donze and colleagues reported a generalize HOSPITAL score for readmissions identifying two discharge laboratory values, hemoglobin <12 (g/dL) and sodium <135 (mEq/L) as risk factors for 30-day readmission. [3] Anemia has been associated with AKI in cardiac surgery [17] and sodium tied to renal function. Therefore, this recent report strengthens our plausible association between AKI and readmission and we expand on this research by evaluating the AKIN criteria to 30-day all-cause readmissions in cardiac surgery as a simplified risk tool for 30-day readmissions.
There are limitations to consider for our analysis of AKIN stage and 30-day readmission. First, the ascertainment of readmissions across our seven medical centers are limited to patients presenting back to these medical center or transferred from outlying hospitals. To the extent that there is incomplete ascertainment of the outcome it only serves to weaken the reported relationship, which may actually be stronger. There is, however, the question of causality: is AKI a risk marker for readmission or is decompensated renal function causing readmissions. Currently, we have a limited understanding of this relationship. It is likely that AKI and AKIN stage is acting as a severity index for risk of near-term adverse events such as readmissions and mortality and acting as a surrogate for the physiologic vulnerability of patients.
Our study also has notable strengths. We report on more than one year of consecutive cardiac surgery procedures in the NNE across seven medical centers. We identified and evaluated the predictive ability of AKIN stage as a severity index for 30-day readmission following cardiac surgery. These efforts provide the cardiac surgical community and other practitioners a tool that could be used as a pre-discharge tool for assessing 30-day readmission risk based on the AKIN stage – a higher AKIN stage, a higher risk of 30-day readmission. Further research is needed in this area to continually improve prediction of 30-day readmission following cardiac surgery and validate our results in a larger cohort.
In summary, we demonstrate the significant predictive ability of AKIN stage for 30-day readmission following cardiac surgery. AKIN stage 1 increases the risk of 30-day readmission by 75%, AKIN stage 2 more than doubles the risk, and AKIN stage 3 more than triples the risk of 30-day readmission after adjustment for other non-renal risk factors for readmission. These efforts provide the cardiac surgical community and other practitioners a tool that could be used as a pre-discharge tool for assessing 30-day readmission risk including AKIN stage independent of multiple patient and clinical risk factors, and an opportunity to reassess perioperative and intraoperative processes of care that may impact AKI.
Table 3.
Multivariate Regression for 30-day Readmission
| Characteristic | Odds Ratios (95%CI) for 30-day Readmission | |
|---|---|---|
| Model without AKIN Stage | Model with AKIN Stage | |
| Acute Kidney Injury Severity | ||
| No AKI | - | reference |
| Stage 1 | - | 1.81 (1.35, 2.44) |
| Stage 2 | - | 2.39 (1.38, 4.14) |
| Stage 3 | - | 3.47 (1.85, 6.50) |
| Other risk factors | ||
| WBC>12,000 | 1.83 (1.15, 2.91) | 1.70 (1.06, 2.74) |
| Single vessel disease | 1.57 (1.15, 2.15) | 1.60 (1.17, 2.20) |
| Two vessel disease | 1.35 (0.96, 1.89) | 1.33 (0.95, 1.87) |
| On-pump surgery | 2.08 (1.10, 3.90) | 2.01 (1.06, 3.80) |
| Nadir Hematocrit on pump <20 | 1.50 (1.06, 2.11) | 1.40 (0.99, 1.98) |
| Mediastinitis | 6.80 (2.32, 19.87) | 5.16 (1.72, 15.43) |
| Model Parameters | ||
| Hosmer-Lemeshow goodness of fit | χ2=4.44, p=0.3 | χ2=5.25, p=0.4 |
| ROC curve | 0.60 (0.56, 0.63) | 0.65 (0.61, 0.68) |
| ROC compared to Other Risk Factors | 0.001 | |
AKI: Acute Kideny Injury. ROC: receiver operating characteristic curve. χ2: chi-square value for Hosmer-Lemeshow goodness of fit test.
Acknowledgments
The study was funded in part by the Northern New England Cardiovascular Disease Study Group. Dr. Brown is supported by grant number K01HS018443 from the Agency for Healthcare Research and Quality on Patient Safety and Acute Kidney Injury. Dr. Parikh is supported by grant R01HL085757 from the National Institutes of Health.
Footnotes
There are no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Zitser-Gurevich Y, Simchen E, Galai N, Braun D. Prediction of readmissions after CABG using detailed follow-up data: the Israeli CABG Study (ISCAB) Med Care. 1999;37:625–36. doi: 10.1097/00005650-199907000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Donze J, Aujesky D, Williams D, Schnipper JL. Potentially Avoidable 30-Day Hospital Readmissions in Medical Patients: Derivation and Validation of a Prediction Model. JAMA Intern Med. 2013:1–7. doi: 10.1001/jamainternmed.2013.3023. [DOI] [PubMed] [Google Scholar]
- 4.Brown JR, Cochran RP, Dacey LJ, et al. Perioperative increases in serum creatinine are predictive of increased 90-day mortality after coronary artery bypass graft surgery. Circulation. 2006;114:I409–13. doi: 10.1161/CIRCULATIONAHA.105.000596. [DOI] [PubMed] [Google Scholar]
- 5.Brown JR, Cochran RP, MacKenzie TA, et al. Long-term survival after cardiac surgery is predicted by estimated glomerular filtration rate. Ann Thorac Surg. 2008;86:4–11. doi: 10.1016/j.athoracsur.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Thakar CV, Parikh PJ, Liu Y. Acute kidney injury (AKI) and risk of readmissions in patients with heart failure. Am J Cardiol. 2012;109:1482–6. doi: 10.1016/j.amjcard.2012.01.362. [DOI] [PubMed] [Google Scholar]
- 7.Goldberg A, Kogan E, Hammerman H, Markiewicz W, Aronson D. The impact of transient and persistent acute kidney injury on long-term outcomes after acute myocardial infarction. Kidney Int. 2009;76:900–6. doi: 10.1038/ki.2009.295. [DOI] [PubMed] [Google Scholar]
- 8.Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal syndrome. J Am Coll Cardiol. 2008;52:1527–39. doi: 10.1016/j.jacc.2008.07.051. [DOI] [PubMed] [Google Scholar]
- 9.Scheel PJ, Liu M, Rabb H. Uremic lung: new insights into a forgotten condition. Kidney Int. 2008;74:849–51. doi: 10.1038/ki.2008.390. [DOI] [PubMed] [Google Scholar]
- 10.Li Z, Armstrong EJ, Parker JP, Danielsen B, Romano PS. Hospital variation in readmission after coronary artery bypass surgery in California. Circ Cardiovasc Qual Outcomes. 2012;5:729–37. doi: 10.1161/CIRCOUTCOMES.112.966945. [DOI] [PubMed] [Google Scholar]
- 11.Magnus PC, Chaisson K, Kramer RS, et al. Causes of 30-Day Readmission After Cardiac Surgery in Northern New England. Circulation. 2011;124:A13474. [Google Scholar]
- 12.Shehata N, Forster A, Li L, et al. Does anemia impact hospital readmissions after coronary artery bypass surgery? Transfusion. 2012 doi: 10.1111/trf.12007. [DOI] [PubMed] [Google Scholar]
- 13.Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31. doi: 10.1186/cc5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–45. [PubMed] [Google Scholar]
- 15.Pencina MJ, D’Agostino RB, Sr, D’Agostino RB, Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–72. doi: 10.1002/sim.2929. discussion 207–12. [DOI] [PubMed] [Google Scholar]
- 16.Medicare Payment Advisory Commission (U.S.) Report to the Congress: Medicare and the health care delivery system. Washington, D.C: MedPAC; 2013. [Google Scholar]
- 17.Karkouti K, Wijeysundera DN, Yau TM, et al. Acute kidney injury after cardiac surgery: focus on modifiable risk factors. Circulation. 2009;119:495–502. doi: 10.1161/CIRCULATIONAHA.108.786913. [DOI] [PubMed] [Google Scholar]
- 18.Brown JR, Kramer RS, MacKenzie TA, et al. Determinants of acute kidney injury duration after cardiac surgery: an externally validated tool. Ann Thorac Surg. 2012;93:570–6. doi: 10.1016/j.athoracsur.2011.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Newland R, Tully P, Baker R. Perfusion. 2013. Hyperthermic perfusion during cardiopulmonary bypass and postoperative temperature are independent predictors of acute kidney injury following cardiac surgery. [DOI] [PubMed] [Google Scholar]
- 20.Patel UD, Greiner MA, Fonarow GC, et al. Associations between worsening renal function and 30-day outcomes among Medicare beneficiaries hospitalized with heart failure. Am Heart J. 2010;160:132–138 e1. doi: 10.1016/j.ahj.2010.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Logeart D, Tabet JY, Hittinger L, et al. Transient worsening of renal function during hospitalization for acute heart failure alters outcome. Int J Cardiol. 2008;127:228–32. doi: 10.1016/j.ijcard.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 22.Shirakabe A, Hata N, Kobayashi N, et al. Long-term prognostic impact after acute kidney injury in patients with acute heart failure. Int Heart J. 2012;53:313–9. doi: 10.1536/ihj.53.313. [DOI] [PubMed] [Google Scholar]