Abstract
Aim:
To investigate the molecular interaction of peroxisome proliferator-activated receptor γ (PPARγ) with 17β-estradiol (E) in the regulation of adipogenesis.
Methods:
Female ovariectomized (OVX) mice and differentiated 3T3-L1 adipocytes were treated with combinations of the PPARγ agonist troglitazone or E, and the variables and determinants of adipogenesis were measured using in vivo and in vitro approaches.
Results:
Troglitazone (250 mg·kg−1·d−1 for 13 weeks) decreased the size of adipocytes without the change in white adipose tissue (WAT) mass and increased the expression of adipocyte-specific genes, such as PPARγ, adipocyte fatty acid binding protein, and lipoprotein lipase, compared with OVX control mice. E (0.05 mg/pellet, sc implanted) significantly reduced WAT mass, adipocyte size, and adipose marker gene expression. When mice were concomitantly treated with troglitazone and E, E blunted the effects of troglitazone on WAT mass, adipocyte size, and adipose PPARγ target gene expression. Consistent with the in vivo data, E (10 μmol/L) treatment inhibited lipid accumulation and the expression of adipocyte-specific genes caused by troglitazone (10 μmol/L) in 3T3-L1 cells. E (10 μmol/L) also decreased troglitazone-induced PPARγ reporter activity through both estrogen receptor (ER) α and ERβ. Mechanistic studies indicated that E (0.1 μmol/L) decreased the DNA binding of PPARγ induced by troglitazone (1 μmol/L) and inhibited the recruitment of the PPARγ coactivator CREB-binding protein.
Conclusion:
These results suggest that in vivo and in vitro treatment of E interferes with the actions of PPARγ on adipogenesis by down-regulating adipogenesis-related genes, which are mediated through the inhibition of PPARγ coactivator recruitment. In addition, it is likely that the activities of PPARγ activators may be enhanced in estrogen-deficient states.
Keywords: PPARγ, adipogenesis, 17β-estradiol, troglitazone, coactivator recruitment, ovariectomized mice, 3T3-L1 cells
Introduction
Peroxisome proliferator-activated receptor γ (PPARγ) is a ligand-activated transcription factor that plays a central role in adipocyte gene expression and differentiation. It is expressed at high levels, specifically in white (WAT) and brown adipose tissue (BAT), and its expression is turned on before transcriptional activation of most adipose-specific genes1. The importance of PPARγ in adipocyte differentiation has been extensively studied in vitro using a variety of cell types, including fibroblasts, adipocytes, and stem cell lines2, 3, 4. Thiazolidinediones (TZDs) are PPARγ agonists that promote adipogenesis, enhance lipid accumulation, and induce the expression of PPARγ-responsive genes during adipogenesis in these cell types4, 5. In adipose tissue, most PPARγ target genes are directly implicated in lipogenic pathways, including lipoprotein lipase (LPL), adipocyte fatty acid binding protein (aP2), acyl-CoA synthase, and fatty acid transport protein. The role of PPARγ in adipocyte development in vivo is also shown in several mouse models6. Embryonic stem cells lacking PPARγ cannot contribute to fat formation, and the PPARγ mutant mouse is deficient for WAT and BAT3, 7, 8, 9. In adult mice, PPARγ ablation in WAT and BAT results in adipocyte death within a few days, demonstrating that PPARγ is also required for the in vivo survival of mature adipocytes10. In addition to adipocyte development, TZDs induce the apoptosis of large adipocytes, resulting in adipose tissue remodeling11, 12.
Adipose tissue is also a target for sex steroids because sex steroid receptors are expressed in rat and human adipose tissues13, 14. In particular, 17β-estradiol (E) has been recognized as a major factor in regulating adipose tissue metabolism in females. Ovariectomy in rodents leads to weight gain, primarily in the form of adipose tissue, which is reversed by physiologic E replacement15, 16. Loss of circulating E is associated with an increase in adiposity during menopause, whereas postmenopausal women who receive E replacement therapy do not display the characteristic abdominal weight gain pattern usually associated with menopause17. E also plays an important role in regulating adipocyte differentiation and development. E represses adipogenic differentiation and maturation via an estrogen receptor (ER)-dependent mechanism in human and mouse bone marrow stromal cells18, 19. The phytoestrogen genistein, which has high affinity for ERs, inhibits adipocyte differentiation, lipid accumulation, and the expression of adipocyte-specific genes in primary human adipocytes20. E was also reported to stimulate the proliferation of human preadipocytes, which can remain undifferentiated cells, into adipocytes21.
Both PPARγ and ERs are members of the nuclear hormone receptor superfamily of ligand-activated transcription factors, and they share similar cofactors22, 23, 24. Transcriptional stimulation and suppression, in response to ligand binding to PPARγ or ERs, are mediated by interactions with coactivator proteins, such as steroid receptor coactivator-1 (SRC-1) and CREB-binding protein (CBP), and corepressor proteins, such as nuclear receptor CoR (a silencing mediator of retinoic acid) and thyroid hormone receptor. It has previously been shown that competition between nuclear receptors for coactivator binding results in a negative cross-talk between nuclear receptors25, 26.
Several studies have suggested that a mutual signaling cross-talk exists between ERs and PPARγ. ERs are capable of inhibiting ligand-induced PPARγ activation in two different breast cancer cell lines27. Noticeably, it was reported that E regulates PPARγ activity on adipogenesis in KS483 cells, which concurrently differentiate into osteoblasts and adipocytes28. Our previous results showed that PPARγ did not induce adipogenesis in female mice with functioning ovaries, indicating that PPARγ activity on adipogenesis might be influenced by estrogens29. In addition, there is evidence that lack of E may potentiate the actions of TZDs on adipogenesis28, 30. Thus, we hypothesized that PPARγ-induced adipogenesis might be suppressed by E in females.
The aim of this study was to determine the molecular mechanism by which E inhibits the actions of troglitazone, a TZD PPARγ agonist, on adipogenesis in female mice. Using in vivo and in vitro approaches, we show that E suppresses the actions of troglitazone-activated PPARγ on adipogenesis and suppresses adipose-specific gene expression through inhibition of PPARγ coactivator recruitment.
Materials and methods
Animal treatments
For all experiments, 8-week-old female mice (C57BL/6J) were housed and bred at the Korea Research Institute of Bioscience and Biotechnology under pathogen-free conditions with a standard 12-h light/dark cycle. Prior to the administration of special diets, mice were fed standard rodent chow and water ad libitum. Female mice were ovariectomized (OVX) and then randomly divided into four groups (n=8 per group), which showed uniformity in response to each treatment in the pilot study. The first group was fed a regular chow diet (CJ, Incheon, Korea) for 13 weeks. The second group was given the same chow diet supplemented with troglitazone (Sankyo, Tokyo, Japan). Troglitazone (250 mg·kg−1·d−1) was given as food admixture at the concentration of 0.2%. The third group was fed a chow diet and subcutaneously implanted with E (0.05 mg per pellet; Innovative Research of America, Sarasota, FL, USA). The final group was given the troglitazone-supplemented diet and was also implanted with E.
In all experiments, body weights were measured daily using a top-loading balance, and the person measuring the body weight was blind to each treatment group. Animals were sacrificed by cervical dislocation, and tissues were harvested, weighed, snap-frozen in liquid nitrogen, and stored at -80 °C until use. All animal experiments were approved by the Institutional Animal Care and Use Committee of Mokwon University and followed National Research Council Guidelines.
Histological analysis
For hematoxylin and eosin (HE) staining, WAT was fixed in 10% phosphate-buffered formalin for 1 d and processed in a routine manner for paraffin sectioning. Tissue sections (4 μm) were cut and stained with HE for microscopic examination. To quantify adipocyte size, the HE-stained sections were analyzed using the Image-Pro Plus analysis system (Media Cybernetics, Bethesda, MD, USA).
Induction of preadipocyte differentiation
Mouse 3T3-L1 cells (ATCC) were proliferated in 6-well plates in DMEM containing 10% bovine calf serum (Invitrogen, Carlsbad, CA, USA). After cells were kept confluent for 2 d, they were incubated in an MDI induction medium (d 0) containing 0.5 mmol/L 1-methyl-3-isobutyl-xanthin, 1 μmol/L dexamethasone, and 1 μg/mL insulin in DMEM with 10% fetal bovine serum (FBS) (Invitrogen). The cultures were continued for 2 d to induce adipocyte differentiation. Thereafter, cells were cultured in DMEM with 10% FBS for the rest of the differentiation process. All other treatments were administered on d 0 to d 2 only, and the medium was changed every other day. Cells were stained at d 6 with Oil-red O and photographed.
Analysis of target gene expression
Total cellular RNA was prepared from parametrial WAT and 3T3-L1 cells using Trizol reagent (Invitrogen). For Northern blot analysis, RNA was analyzed by electrophoresis on 0.22 mol/L formaldehyde-containing 1.2% agarose gels. The separated RNA was transferred to Nytran membranes (Schneicher & Schuell, Dassel, Germany) by downward capillary transfer in the presence of 20× SSC buffer (3 mol/L NaCl and 0.3 mol/L sodium citrate, pH 7.0), then UV cross-linked and baked for 2 h at 80 °C. Probe hybridization and washing were performed using standard techniques. Blots were exposed to PhosphorImager screen cassettes and were visualized using a Molecular Dynamics Storm 860 PhosphorImager system (Sunnyvale, CA, USA). The probes used in this study were 32P-labeled by the random-primer method using a Ready-to-Go DNA Labeling kit (Amersham-Pharmacia Biotech, Piscataway, NJ, USA). Densitometric analysis of the mRNA signals was performed using ImageQuant image analysis software (Molecular Dynamics).
For RT-PCR analysis, after 2 μg of total RNA was reverse-transcribed using Moloney murine leukemia virus reverse transcriptase (MMLV-RT; Promega, Madison, WI, USA) and an antisense primer, cDNA was generated, the RNA was denatured for 5 min at 72 °C and then immediately placed on ice for 5 min. Denatured RNA was mixed with MMLV-RT, MMLV-RT buffer, and a dNTP mixture and incubated for 1 h at 42 °C. Synthesized cDNA fragments were amplified by PCR in an MJ Research Thermocycler (Waltham, MA, USA). The PCR primers used for gene expression analysis are shown in Table 1. The cDNA was mixed with PCR primers, Taq DNA polymerase (Solgent, Daejeon, Korea), and a dNTP mixture. The reaction consisted of 24-34 cycles of denaturation for 1 min at 94 °C, annealing for 1 min at 52–58 °C, and elongation for 1 min at 72 °C. The PCR products were analyzed by electrophoresis on a 1% agarose gel. Relative expression levels were presented as a ratio of target gene cDNA to β-actin cDNA. PCR products were quantified from agarose gels using the GeneGenius (Syngene, Cambridge, UK).
Table 1. Sequences of oligonucleotide primers and PCR conditions.
| Genes | Size (bp) | Primer sequences | Annealing (°C) | Cycle |
|---|---|---|---|---|
| PPARγ | 340 | Forward: 5′-attctggcccaccaacttcgg-3′ Reverse: 5′-tggaagcctgatgctttatcccca-3′ | 58 | 28 |
| aP2 | 417 | Forward: 5′-caaaatgtgtgatgcctttgtg-3′ Reverse: 5′-ctcttcctttggctcatgcc-3′ | 58 | 24 |
| LPL | 770 | Forward: 5′-atggagagcaaagccctgc-3′ Reverse: 5′-agtcctctctctgcaatcca-3′ | 52 | 34 |
| β-acitn | 350 | Forward: 5′-tggaatcctgtggcatccatgaaa-3′ Reverse: 5′-taaaacgcagctcagtaacagtcc-3′ | 58 | 28 |
Transfection assays
The expression vectors for pSG5-mPPARγ and PPRE3-tk-luc reporter genes were generously provided by Dr Frank GONZALEZ (National Cancer Institute, NIH, Bethesda, MD, USA). Expression vectors for pcDNA-ERα and pcDNA-ERβ were generously provided by Dr Matt BUROW (Tulane University Medical Center, New Orleans, LA, USA). Expression vectors for VP16-mPPARγ and GAL-CBP were generously provided by Steve KLIEWER (University of Texas Southwestern Medical Center, Dallas, TX, USA), and expression vectors for VP16-hERα and VP16-hERβ were generously provided by Dr Donald MCDONNELL (Duke University Medical Center, Durham, NC, USA). The GAL4-UAS luciferase reporter plasmid (pFR-Luc) was obtained from Stratagene (La Jolla, CA, USA). The murine preadipocyte cell line 3T3-L1 cells and monkey kidney cell line CV-1 cells were routinely cultured in DMEM containing 10% FBS, penicillin G (100 U/mL), streptomycin sulfate (100 μg/mL), amphotericin B (0.25 μg/mL), and 2-mercaptoethanol (50 μmol/L). Cells were seeded in 6-well tissue culture plates (2×104 cells/well) for 24 h prior to transfection. For all transfections, 200 ng/well of each of the appropriate plasmids were used. Transfections were performed using lipofectamine (Invitrogen) according to the manufacturer's instructions. After 6 h, the culture medium was changed and the test compounds, troglitazone and E (Sigma), were added. After incubation for 24 h in the presence of these chemicals, the cells were washed twice with phosphate-buffered saline and assayed for luciferase and β-galactosidase activities using commercial kits according to the manufacturer's instructions (Promega).
Electrophoretic mobility shift assay
The binding of PPARγ to a PPAR-specific oligonucleotide probe was accomplished by adding 8 μg of crude nuclear extract from WAT to each gel shift reaction mixture. An oligonucleotide consensus DR-1 element was synthesized with the following sequence: 5′–GAACTAGGTCAAAGGTCATCCCCT–3′ along with an oligonucleotide of a complementary sequence (Geno Tech, Daejeon, Korea). The oligonucleotides were mixed (50 ng/μL final concentration) and denatured by heating them to 95 °C for 10 min in 0.1 mol/L Tris-HCl and 50 mmol/L MgCl2 (pH 7.9). They were then allowed to anneal by slowly cooling to room temperature. The annealed oligonucleotides were end-labeled with [γ-32P]ATP using T4 polynucleotide kinase according to the supplier's instructions (Promega). In a total volume of 20 μL of binding buffer [25 mmol/L Tris-HCl (pH 7.5), 40 mmol/L KCl, 0.5 mmol/L MgCl2, 0.1 mmol/L EDTA, 1 mmol/L dithiothreitol, and 10% glycerol], the following components were combined: 1 μg of poly(dI-dC), 2 μL of nuclear extract, and the indicated concentrations of troglitazone or E dissolved in DMSO. For a supershift experiment, 2 μg of goat anti-human PPARγ antibody (Santa Cruz Biotechnology, Santa Cruz, CA, USA) was added to the reaction mixture prior to the oligonucleotide probe. After a 20-min incubation at room temperature, 20 000 cpm of the labeled oligonucleotide was added, and the incubation was continued for a further 20 min. The samples were analyzed on a 5% non-denaturing polyacrylamide gel, containing 2.5% glycerol, in 0.4×TBE (1×=89 mmol/L Tri-HCl, 89 mmol/L boric acid, and 2 mmol/L EDTA). After drying, the gels were exposed to PhosphorImager screen cassettes and were visualized using a Molecular Dynamics Storm 860 PhosphorImager system.
Statistical analysis
Unless otherwise noted, all values are expressed as mean± standard deviation (SD). All data were analyzed by the unpaired, Student's t-test for significant differences between the mean values of each group using SigmaPlot 2001 (SPSS, Chicago, IL, USA).
Results
Body weight, WAT mass, and adipocyte size
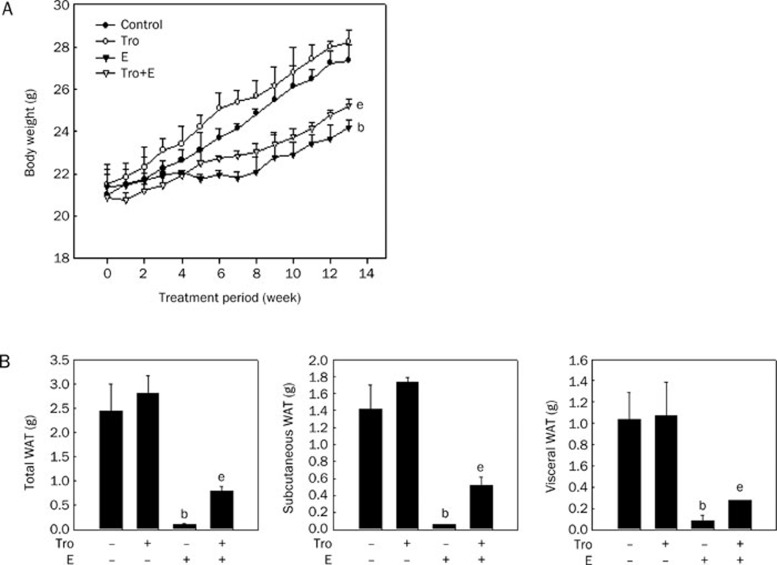
Troglitazone did not cause significant changes in body and WAT weights; whereas E significantly decreased both compared with controls (Figure 1). A combination of troglitazone and E significantly reduced body and WAT weights compared with troglitazone alone, although not to the same extent as E alone.
Figure 1.
Body weight and WAT mass. Body weight (A) and WAT mass (B) were determined after 13 weeks of treatment with troglitazone (Tro; 250 mgkg−1·d−1), 17β-estradiol (E; 0.05 mg/pellet), or Tro plus E in female OVX mice (n=8/group). All values are expressed as mean±SD. bP<0.05 vs control group. eP<0.05 vs Tro group.
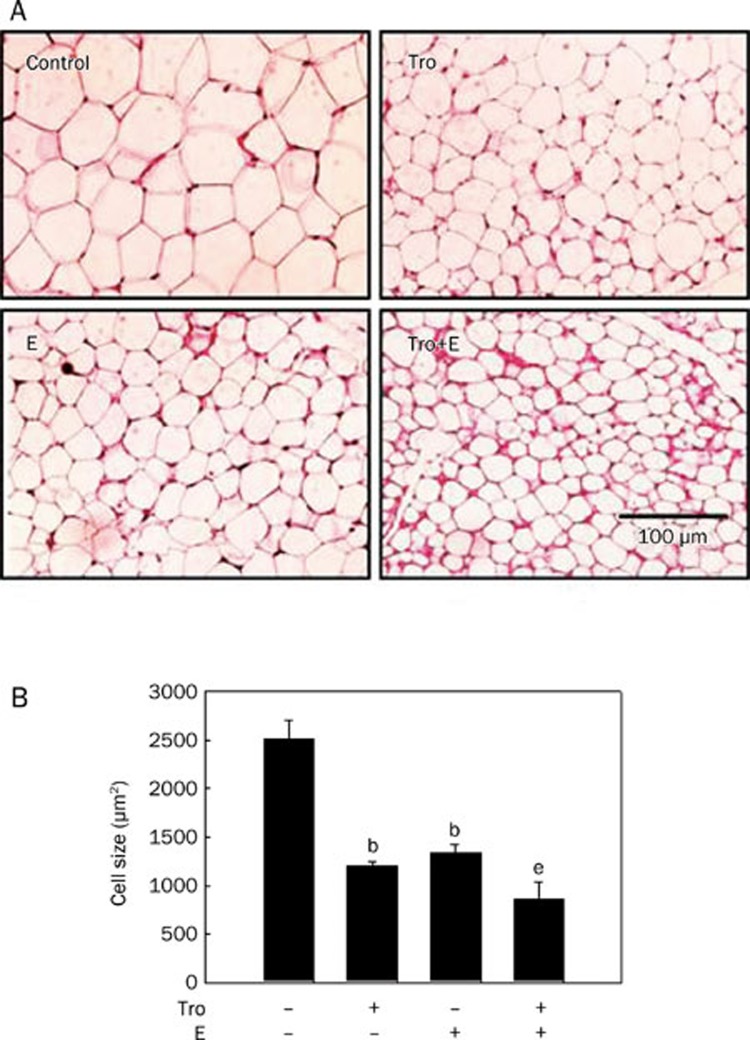
Histological analysis showed that, compared with control, troglitazone and E decreased the size of adipocytes in parametrial WAT by 52.3% and 46.6%, respectively (Figure 2). The adipocyte size was further reduced by concomitant treatment with troglitazone and E.
Figure 2.
Histological analysis of parametrial WAT stained with hematoxylin and eosin (original magnification ×200). Adult female mice (n=8/group) received a chow diet with troglitazone (Tro; 250 mgkg−1·d−1), 17β-estradiol (E; 0.05 mg/pellet), or Tro plus E for 13 weeks. (A) Representative hematoxylin and eosin (HE)-stained sections (4 μm thick) of female parametrial adipose tissue. (B) HE-stained sections were analyzed with an image analysis system, and the size of the adipocytes was quantified. All values are expressed as mean±SD. bP<0.05 vs control group. eP<0.05 vs Tro group.
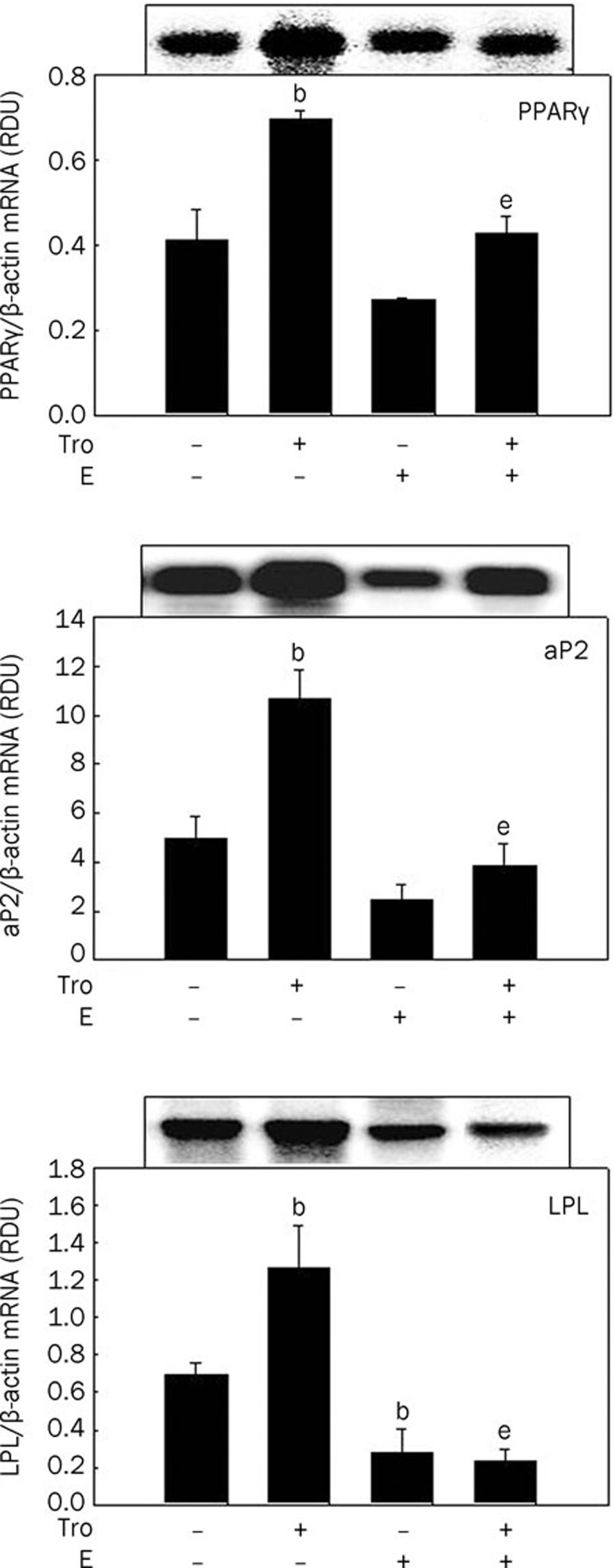
Expression of PPARγ target genes in WAT
To determine whether the effects of E on troglitazone-regulated adipocyte size and WAT mass are associated with changes in PPARγ and PPARγ target gene expression in WAT, we measured mRNA levels of PPARγ and the PPARγ target genes aP2 and LPL. As expected, troglitazone substantially upregulated PPARγ, aP2, and LPL mRNA levels by 69.2%, 114.5%, and 81.9%, respectively, compared with controls, whereas E downregulated PPARγ, aP2, and LPL mRNA levels by 34.2%, 50%, and 60.4%, respectively (Figure 3). Co-administration of troglitazone and E decreased the troglitazone-induced PPARγ, aP2, and LPL mRNA expression by 38.8%, 63.6%, and 81.4%, respectively, compared with troglitazone alone. These results suggest that E may decrease adipose mRNA levels of troglitazone-induced PPARγ target genes, thereby preventing in vivo actions of PPARγ on body weight, WAT weight, and adipocyte size.
Figure 3.
The mRNA expression levels of PPARγ and PPARγ target genes in WAT of female OVX mice. Female OVX mice (n=8/group) received a chow diet with troglitazone (Tro; 250 mg·kg−1·d−1), 17β-estradiol (E; 0.05 mg/pellet), or Tro plus E for 13 weeks. Total RNA was extracted from the parametrial adipose tissue and PPARγ, PPARγ target genes, and β-actin mRNA levels were measured as described in the Materials and methods section. All values are expressed as mean±SD of RDU (relative density units) using β-actin as a reference. Insets show representative autoradiograms of Northern blots used for quantification. bP<0.05 vs control group. eP<0.05 vs Tro group.
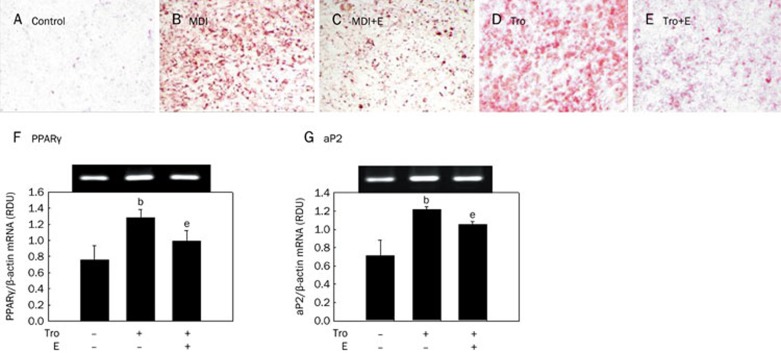
3T3-L1 differentiation and adipocyte-specific gene expression
Accumulation of triglyceride droplets in 3T3-L1 cells was evident on the sixth day following 2 d of MDI (Figure 4B) or troglitazone (Figure 4D) treatment, as shown by positive staining with Oil red O. Treatment of cells with E, however, inhibited triglyceride accumulation. The percentage of differentiated cells in the MDI and E-treated cells was approximately 73% (Figure 4C), and it was 81% in troglitazone and E-treated cells (Figure 4E).
Figure 4.
Adipocyte differentiation and adipose-specific gene expression in 3T3-L1 cells. 3T3-L1 preadipocytes were differentiated into mature adipocytes as described in the Materials and methods section. 3T3-L1 cells were treated with an MDI mix (MDI), 10 μmol/L troglitazone (Tro), 10 μmol/L 17β-estradiol (E), or 10 μmol/L Tro plus 10 μmol/L E. (A–E) At d 6 post-induction, cells were fixed and stained for neutral lipids with Oil red O. Magnification is ×10. (F and G) Total cellular RNA was extracted from differentiated cells on d 6, and mRNA levels of PPARγ, aP2, and β-actin were measured using RT-PCR. Insets show representative RT-PCR bands used for quantifictation. bP<0.05 vs control group. eP<0.05 vs Tro group.
To quantify changes in differentiation degree by troglitazone and E, we analyzed PPARγ and PPARγ-dependent gene expression. Troglitazone substantially upregulated PPARγ (Figure 4F) and aP2 (Figure 4G) mRNA levels by 68.8% and 70.8%, respectively, compared with controls. Whereas co-administration of troglitazone and E significantly decreased troglitazone-induced PPARγ and aP2 mRNA levels by 22.5% and 13.5%, respectively. Thus, E was inhibitory to MDI- or troglitazone-induced differentiation, in part through reductions in PPARγ target gene expression.
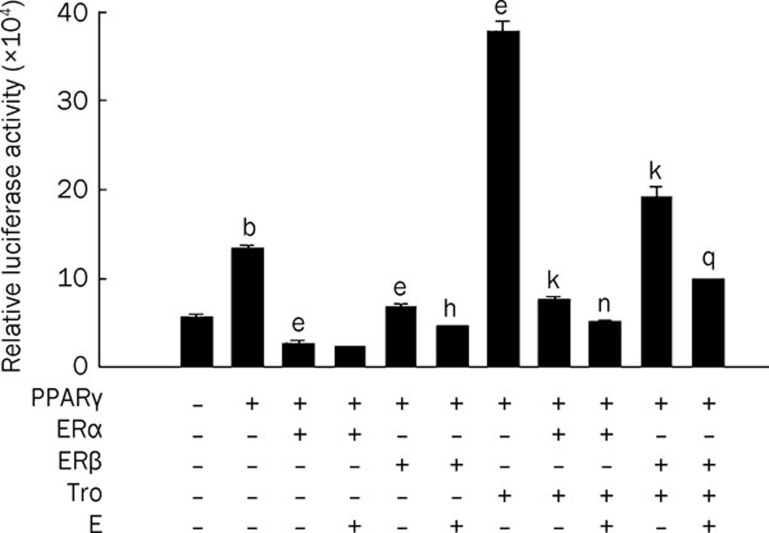
PPARγ reporter gene expression
To examine the mechanism by which E inhibited the troglitazone-induced PPARγ and PPARγ target gene expression, 3T3-L1 preadipocytes were transiently transfected with PPARγ, ERα, and ERβ expression constructs and a luciferase reporter gene construct (PPRE3-tk-luc) containing three copies of the PPRE from the rat acyl-CoA oxidase gene. Overexpression of PPARγ alone significantly increased the expression of the luciferase reporter gene compared with controls (Figure 5, lane 2 vs lane 1), potentially due to endogenous ligands. Troglitazone significantly elevated the luciferase reporter activity induced by PPARγ transfection (Figure 5, lane 7 vs lane 2). Overexpression of ERα or ERβ substantially inhibited the induction of the luciferase activity caused by PPARγ (Figure 5, lanes 3 and 5) as well as PPARγ plus troglitazone (Figure 5, lanes 8 and 10). Moreover, treatment with E led to a further inhibition of constitutive- (Figure 5, lanes 4 and 6) and ligand-dependent PPARγ reporter activities by ERα or ERβ (Figure 5, lanes 9 and 11). These results suggest that E inhibits PPARγ-dependent transactivation through ERα and ERβ.
Figure 5.
PPARγ reporter gene expression in 3T3-L1 cells. 3T3-L1 preadipocytes were transiently transfected with pSG5-mPPARγ, reporter plasmid PPRE-TK-Luc, and pcDNA-ERα or pcDNA-ERβ. Cells were treated with 10 μmol/L troglitazone (Tro) and/or 10 μmol/L 17β-estradiol (E). After incubation for 24 h, cells were harvested, lysed, and subsequently assayed for luciferase and β-galactosidase activities. All values are expressed as the mean±SD of relative luciferase units/β-galactosidase activity. Experiments were performed at least three times. bP<0.05 vs control group. eP<0.05 vs PPARγ group. hP<0.05 vs PPARγ/ERβ group. kP<0.05 vs PPARγ/Tro group. nP<0.05 vs PPARγ/Tro/ERα group. qP<0.05 vs PPARγ/Tro/ERβ group.
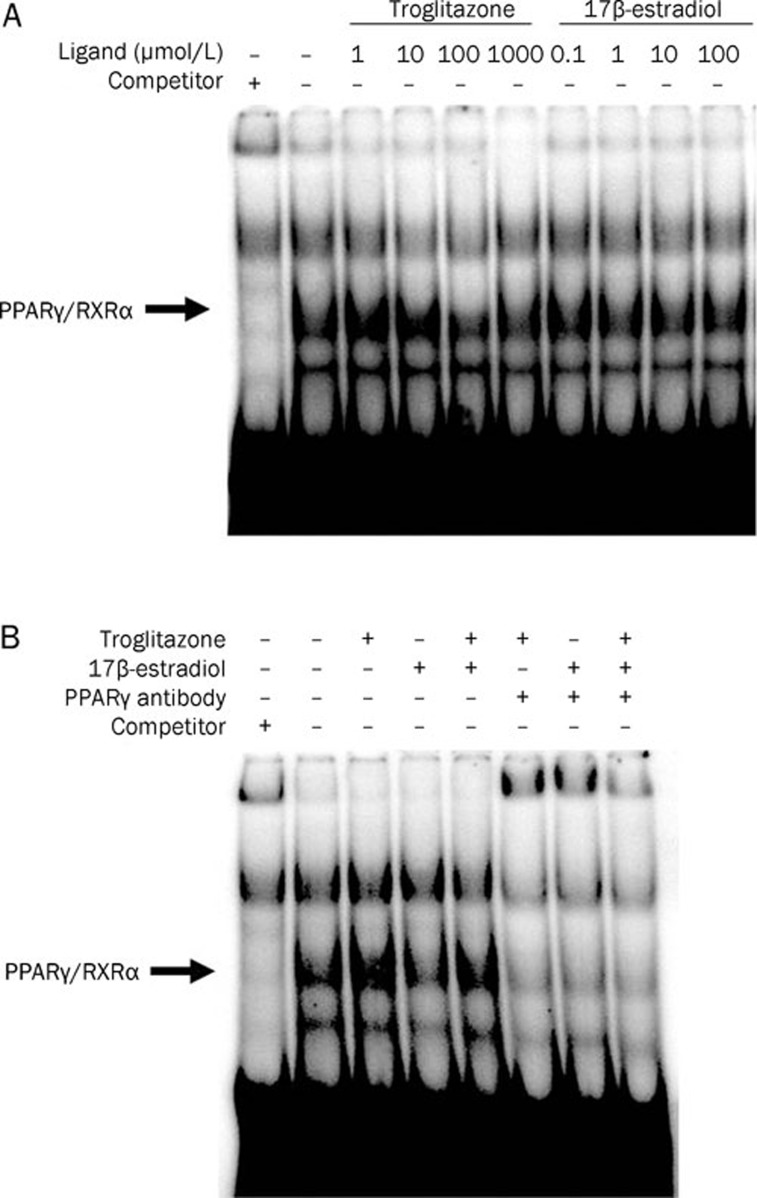
PPARγ binding to DNA
An electrophoretic mobility shift assay (EMSA) was performed to determine whether E interfered with the binding of PPARγ/RXRα to a consensus DR-1 sequence (AGGTCAAAGGTCA). Treatment of a nuclear extract containing the PPARγ/RXRα complex with 1 μmol/L troglitazone increased DNA binding of PPARγ/RXRα compared with vehicle (Figure 6A, lane 3 and Figure 6B, lane 3), whereas 1 μmol/L E decreased DNA binding to the complex (Figure 6A, lane 8 and Figure 6B, lane 4). However, E decreased the troglitazone-induced DNA binding of PPARγ/RXRα, as shown by the combination of troglitazone and E (Figure 6B, lane 5 vs lane 3), suggesting that E prevents PPARγ from binding to DNA. To verify the identity of the PPARγ/RXRα complex, we conducted a supershift assay using an anti-PPARγ antibody. The PPARγ/RXRα complex disappeared when an anti-PPARγ antibody was added (Figure 6B, lanes 6–8).
Figure 6.
Binding of PPARγ to PPRE. EMSAs were performed using nuclear extracts from the WAT of female C57BL/6J mice. (A) While the PPARγ activator troglitazone increased PPARγ binding to the consensus DR-1 sequence containing PPRE, 17β-estradiol decreased the binding of PPARγ. (B) 17β-estradiol (0.1 μmol/L) inhibited the troglitazone (1 μmol/L)-induced PPARγ binding to PPRE. An anti-PPARγ antibody was included to show the identity of the PPARγ/RXRα complexes.
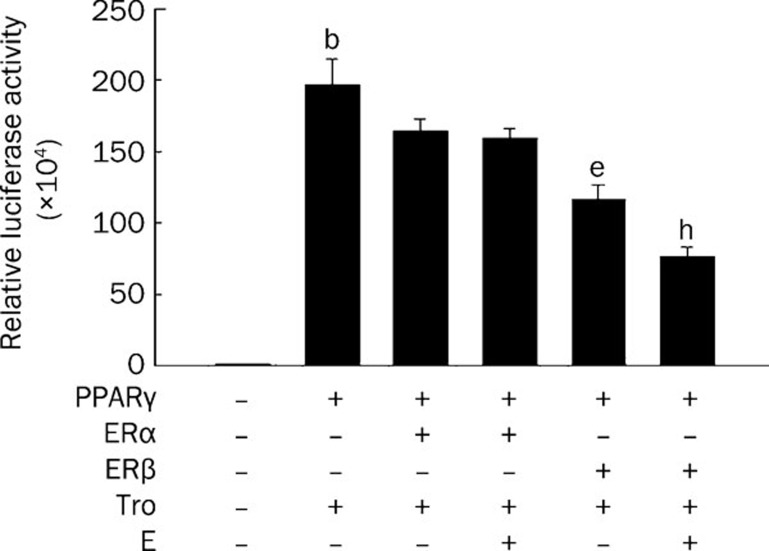
Cofactor recruitment
To determine whether changes in cofactor recruitment are involved in the E-mediated inhibition of PPARγ binding to DNA and PPARγ activity, the coactivator CBP was examined using a mammalian two-hybrid assay. The key components of this assay include the followings: 1) reporter constructs for full-length murine PPARγ fused to the transactivation domain of VP16 and 2) the nuclear receptor-interaction domains of CBP fused to the DNA binding domain of GAL4. In CV-1 cells transfected with PPARγ and CBP, troglitazone caused efficient CBP recruitment, as evidenced by an increase in luciferase reporter gene activity (Figure 7, lane 2 vs lane 1). However, transfection with ERα or ERβ reduced the troglitazone-induced CBP association (Figure 7, lanes 3 and 5), and E markedly decreased the magnitude of the reporter gene inhibition by ERβ (Figure 7, lane 6) but not by ERα (lane 4).
Figure 7.
PPARγ coactivator recruitment. A mammalian two-hybrid assay was used to detect the ligand-dependent interaction of PPARγ with CBP. CV-1 cells were transiently transfected with expression plasmids for VP16-mPPARγ, GAL-CBP, reporter plasmid pFR-Luc, and VP16-hERα or VP16-hERβ. All values are expressed as the mean±SD for three experiments. bP<0.05 vs control group. eP<0.05 vs PPARγ/Tro group. hP<0.05 vs PPARγ/Tro/ERβ group.
Discussion
The present study demonstrates that in vivo and in vitro treatments with E negatively regulate the troglitazone-activated PPARγ actions on adipogenesis and adipocyte-specific gene expression. We further show that these events are mediated, at least in part, through the E inhibition of PPARγ coactivator recruitment.
Mice treated with troglitazone for 13 weeks exhibited a significant decrease in adipocyte size without changes in body weight gain and WAT weight compared with chow diet-fed controls. These data support previous results showing that troglitazone increased the number of small adipocytes without affecting body weight gain and WAT mass in obese Zucker rats31. However, a combination of troglitazone and E upset the effect of troglitazone. Body weight gain and WAT mass were decreased and adipocyte size was further decreased compared with troglitazone alone. According to the results from Kadowaki et al and Yamauchi et al, supraphysiological activation of PPARγ by PPARγ agonists stimulated the adipocyte differentiation and apoptosis of large adipocytes, thereby preventing adipocyte hypertrophy and increasing the small adipocytes, whereas reductions in PPARγ activity decreased adipocyte size and WAT mass via activation of fatty acid oxidation and energy dissipation12, 32. It is thought that both supraphysiological activation of PPARγ by PPARγ agonists and inhibition of PPARγ activity by E can lead to the reduced size of adipocytes through different mechanisms of action. Thus, these results suggest that reduced PPARγ activity by E decreases the size of adipocytes and WAT mass.
The development of fat cells from preadipocytes, or adipogenesis, includes the followings: morphological changes, cessation of cell growth, expression of many lipogenic enzymes, and extensive lipid accumulation33. As expected, troglitazone increased the accumulation of triglyceride droplets in 3T3-L1 cells compared with vehicle-treated controls. However, E treatment prevented this troglitazone-induced lipid accumulation, indicating that E has an inhibitory effect on troglitazone-induced adipogenesis. Similarly, adipogenic differentiation and maturation are reported to be reduced by E and genistein via an ER-dependent mechanism18, 19, 20. PPARγ transcriptional activity and its effects on adipogenic differentiation were enhanced in the absence of E, whereas E inhibited PPARγ-mediated adipocyte differentiation18, 28. These results are paralleled by enhanced adipogenesis in E-deprived rats treated with the PPARγ agonist rosiglitazone30. Moreover, our previous study showed that troglitazone treatment did not significantly increase the smaller size of adipocytes in parametrial adipose tissue in female mice with functioning ovaries, although it did increase the number of small adipocytes in male animals29. Thus, PPARγ does not seem to be involved in the regulation of adipogenesis in female mice with functioning ovaries, suggesting that the effects of troglitazone on adipogenesis may be disrupted by a sex-related factor, namely E, in female mice.
Adipogenesis is initiated by the production of the key transcription factor PPARγ, which is responsible for inducing the expression of adipocyte-specific genes. Consistent with the effects of E on troglitazone-induced adipogenesis, E decreased the expression of PPARγ and the PPARγ target genes aP2 and LPL, which are directly implicated in lipogenic pathways, in both WAT of OVX mice and in 3T3-L1 adipocytes. Previous studies reported that E and genistein may have anti-lipogenic and anti-adipogenic effects by downregulating the expression of adipocyte-specific genes, such as PPARγ, CCAAT/enhancer binding protein α, aP2, and LPL, in OVX mice, primary human adipocytes, and mouse and human bone marrow stromal cells18, 19, 20, 28. Similarly, troglitazone did not affect PPARγ mRNA expression or adipocyte-specific gene expression in E-producing female mice. Thus, these results suggest that E can prevent the ability of troglitazone to regulate adipogenesis and lipogenesis through inhibiting PPARγ and PPARγ target gene expression.
There is evidence to show that a bidirectional signaling cross-talk exists between PPARγ and ERs34, 35, 36, 37, 38. Keller et al demonstrated that the PPARγ/RXRα complex inhibited transcription by ERs through a competition for estrogen response element binding in the vitellogenin A2 promoter34. Wang et al demonstrated that both ERα and ERβ were capable of inhibiting PPARγ transactivation in PPARγ-expressing MDA-MB-231 and MCF-7 breast cancer cells27. Expression of ERα or ERβ lowered both basal and stimulated PPARγ-mediated reporter activities, and deletion of the ER DNA-binding domain rendered ERs unable to inhibit either basal or stimulated PPAR transactivation27. These data suggest that both ERs are capable of repressing PPAR transactivation in these cells. Similar to these results, our results show that E inhibits the levels of troglitazone-induced PPARγ reporter gene activation through both ERα and ERβ in 3T3-L1 preadipocytes. Overexpression of ERα or ERβ decreased basal and troglitazone-induced luciferase reporter activities. Moreover, treatment with E led to a further inhibition of both. Thus, these data indicate that E inhibits PPARγ-dependent transactivation through ERs. Recently, Foryst-Ludwig et al also reported that ERβ inhibited ligand-mediated PPARγ transcriptional activity in 3T3-L1 preadipocytes transfected with PPARγ26. In contrast to our results, these authors found that pioglitazone-stimulated PPARγ activity was not blocked by ERα. This difference may be due to differences in the PPARγ agonists used in the transfection assays. While pioglitazone stimulation substantially increased luciferase activity by 15-fold in their system, troglitazone increased such activity by only three-fold in our system. Accordingly, ERα may be able to inhibit the troglitazone-induced luciferase activity, but not suppress the pronounced activation of PPARγ by pioglitazone.
The molecular mechanism by which E-activated ERs inhibit PPARγ transactivation was examined by EMSA and a mammalian two-hybrid assay. EMSA revealed that E inhibited DNA binding of PPARγ. Treatment of a nuclear extract with troglitazone increased PPARγ-binding activity, but E interfered with the troglitazone-induced DNA binding of PPARγ. Similarly, other research has shown that E and E-like compounds inhibited the DNA-binding activity of PPARγ and that nuclear extracts isolated from adipose tissues of ERβ-KO mice showed increased binding of endogenous PPARγ in comparison with wild-type mice26. PPARγ-binding activity was also markedly decreased in the phytoestrogen genistein-treated cells compared with untreated control39. The mammalian two-hybrid assay showed that E significantly decreased the troglitazone-induced CBP association in the presence of ERα or ERβ and that this effect was more prominent by ERβ. It has previously been shown that competition of nuclear receptors for coactivator binding results in a negative cross-talk between nuclear receptors25. Overexpression of nuclear coactivators, such as SRC-1 and transcriptional intermediary factor 2, prevented the ERβ-mediated inhibition of PPARγ activity26. Considering that both PPARγ and the ERs belong to the nuclear hormone receptor superfamily and share similar coactivators22, 23, 24, 40, our data suggest that the suppressive effects of the ERs may be a result of CBP interaction with ERs, thereby preventing the binding of PPARγ to CBP.
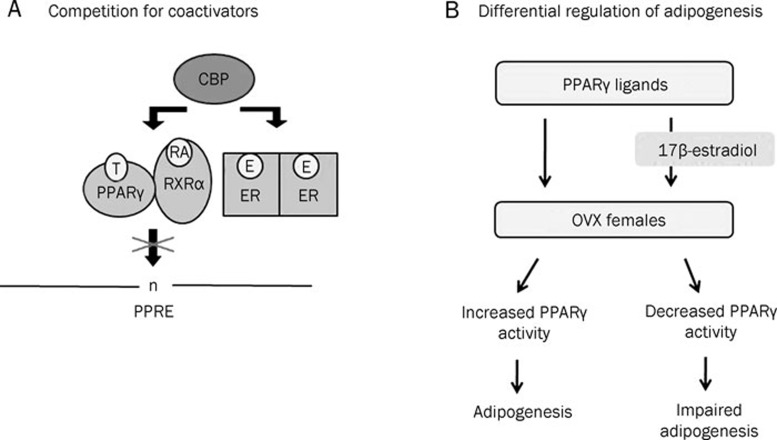
In conclusion, in vivo and in vitro studies demonstrate that E inhibits PPARγ-mediated adipogenesis and adipocyte-specific gene expression. Our data also suggest that the coactivator CBP is involved in this inhibition (Figure 8A). In addition, the use of PPARγ activators may be effective in E-deficient states, such as in men and postmenopausal women (Figure 8B).
Figure 8.
A proposed mechanism for the inhibition of PPARγ-induced adipogenesis by 17β-estradiol. (A) Competition between PPARγ and estrogen receptors (ERs) for coactivator binding, which results in decreased PPRE binding of PPARγ. (B) Inhibition of PPARγ actions on adipogenesis by 17β-estradiol (E). E impairs the ability of PPARγ ligands to induce adipogenesis in female ovariectomized (OVX) mice. T, troglitazone; RA, 9-cis-retinoic acid.
Author contributions
Michung YOON designed the research, analyzed the data, and wrote the paper. Sunhyo JEONG performed the research, analyzed the data, and wrote the paper.
Abbreviations
aP2, adipocyte fatty acid binding protein; BAT, brown adipose tissue; CBP, CREB-binding protein; E, 17β-estradiol; ER, estrogen receptor; HE, hematoxylin and eosin; LPL, lipoprotein lipase; MMLV-RT, Moloney murine leukemia virus reverse transcriptase; OVX, ovariectomized; PPARγ, peroxisome proliferator-activated receptor γ PPRE, PPAR response element; TZDs, thiazolidinediones; WAT, white adipose tissue.
Acknowledgments
This work was supported by Mid-career Researcher Program (No 2009-0083990) and Female Scientist Program (No 2010-0017313) through an NRF grant funded by the MEST, Korea.
References
- Kliewer SA, Forman BM, Blumberg B, Ong ES, Borgmeyer U, Mangelsdorf DJ, et al. Differential expression and activation of a family of murine peroxisome proliferator-activated receptors. Proc Natl Acad Sci USA. 1994;91:7355–9. doi: 10.1073/pnas.91.15.7355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tontonoz P, Hu E, Spiegelman BM. Stimulation of adipogenesis in fibroblasts by PPAR gamma 2, a lipid-activated transcription factor. Cell. 1994;79:1147–56. doi: 10.1016/0092-8674(94)90006-x. [DOI] [PubMed] [Google Scholar]
- Rosen ED, Sarraf P, Troy AE, Bradwin G, Moore K, Milstone DS, et al. PPAR gamma is required for the differentiation of adipose tissue in vivo and in vitro. Mol Cell. 1999;4:611–7. doi: 10.1016/s1097-2765(00)80211-7. [DOI] [PubMed] [Google Scholar]
- Sottile V, Seuwen K. Bone morphogenetic protein-2 stimulates adipogenic differentiation of mesenchymal precursor cells in synergy with BRL 49653 (rosiglitazone) FEBS Lett. 2000;475:203–4. doi: 10.1016/s0014-5793(00)01655-0. [DOI] [PubMed] [Google Scholar]
- Gimble JM, Robinson CE, Wu X, Kelly KA, Rodriguez BR, Kliewer SA, et al. Peroxisome proliferator-activated receptor-gamma activation by thiazolidinediones induces adipogenesis in bone marrow stromal cells. Mol Pharmacol. 1996;50:1087–94. [PubMed] [Google Scholar]
- Lefterova MI, Lazar MA. New developments in adipogenesis. Trends Endocrinol Metab. 2009;20:107–14. doi: 10.1016/j.tem.2008.11.005. [DOI] [PubMed] [Google Scholar]
- He W, Barak Y, Hevener A, Olson P, Liao D, Le J, et al. Adipose-specific peroxisome proliferator-activated receptor gamma knockout causes insulin resistance in fat and liver but not in muscle. Proc Natl Acad Sci USA. 2003;100:15712–7. doi: 10.1073/pnas.2536828100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones JR, Barrick C, Kim KA, Lindner J, Blondeau B, Fujimoto Y, et al. Deletion of PPARgamma in adipose tissues of mice protects against high fat diet-induced obesity and insulin resistance. Proc Natl Acad Sci USA. 2005;102:6207–12. doi: 10.1073/pnas.0306743102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Fu M, Cui T, Xiong C, Xu K, Zhong W, et al. Selective disruption of PPARgamma 2 impairs the development of adipose tissue and insulin sensitivity. Proc Natl Acad Sci USA. 2004;101:10703–8. doi: 10.1073/pnas.0403652101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai T, Takakuwa R, Marchand S, Dentz E, Bornert JM, Messaddeq N, et al. Peroxisome proliferator-activated receptor gamma is required in mature white and brown adipocytes for their survival in the mouse. Proc Natl Acad Sci USA. 2004;101:4543–7. doi: 10.1073/pnas.0400356101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auwerx J. PPARgamma, the ultimate thrifty gene. Diabetologia. 1999;42:1033–49. doi: 10.1007/s001250051268. [DOI] [PubMed] [Google Scholar]
- Kadowaki T, Hara K, Yamauchi T, Terauchi Y, Tobe K, Nagai R. Molecular mechanism of insulin resistance and obesity. Exp Biol Med (Maywood) 2003;228:1111–7. doi: 10.1177/153537020322801003. [DOI] [PubMed] [Google Scholar]
- Pedersen SB, Børglum JD, Eriksen EF, Richelsen B. Nuclear estradiol binding in rat adipocytes. Regional variations and regulatory influences of hormones. Biochim Biophys Acta. 1991;1093:80–6. doi: 10.1016/0167-4889(91)90141-j. [DOI] [PubMed] [Google Scholar]
- Dieudonne MN, Pecquery R, Leneveu MC, Giudicelli Y. Opposite effects of androgens and estrogens on adipogenesis in rat preadipocytes: evidence for sex and site-related specificities and possible involvement of insulin-like growth factor 1 receptor and peroxisome proliferator-activated receptor gamma2. Endocrinology. 2000;141:649–56. doi: 10.1210/endo.141.2.7293. [DOI] [PubMed] [Google Scholar]
- Jeong S, Han M, Lee H, Kim M, Kim J, Nicol CJ, et al. Effects of fenofibrate on high fat diet-induced body weight gain and adiposity in female C57BL/6J mice. Metabolism. 2004;53:1284–9. doi: 10.1016/j.metabol.2004.05.003. [DOI] [PubMed] [Google Scholar]
- Jeong S, Yoon M. Inhibition of the actions of peroxisome proliferator-activated receptor alpha on obesity by estrogen. Obesity (Silver Spring) 2007;15:1430–40. doi: 10.1038/oby.2007.171. [DOI] [PubMed] [Google Scholar]
- Carani C, Qin K, Simoni M, Faustini-Fustini M, Serpente S, Boyd J, et al. Effect of testosterone and estradiol in a man with aromatase deficiency. N Engl J Med. 1997;337:91–5. doi: 10.1056/NEJM199707103370204. [DOI] [PubMed] [Google Scholar]
- Okazaki R, Inoue D, Shibata M, Saika M, Kido S, Ooka H, et al. Estrogen promotes early osteoblast differentiation and inhibits adipocyte differentiation in mouse bone marrow stromal cell lines that express estrogen receptor (ER) alpha or beta. Endocrinology. 2002;143:2349–56. doi: 10.1210/endo.143.6.8854. [DOI] [PubMed] [Google Scholar]
- Heim M, Frank O, Kampmann G, Sochocky N, Pennimpede T, Fuchs P, et al. The phytoestrogen genistein enhances osteogenesis and represses adipogenic differentiation of human primary bone marrow stromal cells. Endocrinology. 2004;145:848–59. doi: 10.1210/en.2003-1014. [DOI] [PubMed] [Google Scholar]
- Park HJ, Della-Fera MA, Hausman DB, Rayalam S, Ambati S, Baile CA. Genistein inhibits differentiation of primary human adipocytes. J Nutr Biochem. 2009;20:140–8. doi: 10.1016/j.jnutbio.2008.01.006. [DOI] [PubMed] [Google Scholar]
- Roncari DA, Van RL. Promotion of human adipocyte precursor replication by 17beta-estradiol in culture. J Clin Invest. 1978;62:503–8. doi: 10.1172/JCI109153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gronemeyer H, Gustafsson JA, Laudet V. Principles for modulation of the nuclear receptor superfamily. Nat Rev Drug Discov. 2004;3:950–64. doi: 10.1038/nrd1551. [DOI] [PubMed] [Google Scholar]
- Glass CK. Going nuclear in metabolic and cardiovascular disease. J Clin Invest. 2006;116:556–60. doi: 10.1172/JCI27913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan HP, Ishizuka T, Chui PC, Lehrke M, Lazar MA. Corepressors selectively control the transcriptional activity of PPARgamma in adipocytes. Genes Dev. 2005;19:453–61. doi: 10.1101/gad.1263305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez GN, Webb P, Shinsako JH, Baxter JD, Greene GL, Kushner PJ. Titration by estrogen receptor activation function-2 of targets that are downstream from coactivators. Mol Endocrinol. 1999;13:897–909. doi: 10.1210/mend.13.6.0283. [DOI] [PubMed] [Google Scholar]
- Foryst-Ludwig A, Clemenz M, Hohmann S, Hartge M, Sprang C, Frost N, et al. Metabolic actions of estrogen receptor beta (ERbeta) are mediated by a negative cross-talk with PPARgamma. PLoS Genet. 2008;4:e1000108. doi: 10.1371/journal.pgen.1000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Kilgore MW. Signal cross-talk between estrogen receptor alpha and beta and the peroxisome proliferator-activated receptor gamma1 in MDA-MB-231 and MCF-7 breast cancer cells. Mol Cell Endocrinol. 2002;194:123–33. doi: 10.1016/s0303-7207(02)00154-5. [DOI] [PubMed] [Google Scholar]
- Dang ZC, van Bezooijien RL, Karperien M, Papapoulos SE, Lowik CW. Exposure of KS483 cells to estrogen enhances osteogensis and inhibits adipogenesis. J Bone Miner Res. 2002;17:394–405. doi: 10.1359/jbmr.2002.17.3.394. [DOI] [PubMed] [Google Scholar]
- Yoon M, Jeong S. Peroxisome proliferator-activated receptor γ is not associated with adipogenesis in female mice. J Biomed Lab Sci. 2008;14:139–46. [Google Scholar]
- Sottile V, Seuwen K, Kneissel M. Enhanced marrow adipogenesis and bone resorption in estrogen-deprived rats treated with the PPARgamma agonist BRL49653 (rosiglitazone) Calcif Tissue Int. 2004;75:329–37. doi: 10.1007/s00223-004-0224-8. [DOI] [PubMed] [Google Scholar]
- Okuno A, Tamemoto H, Tobe K, Ueki K, Mori Y, Iwamoto K, et al. Troglitazone increases the number of small adipocytes without the change of white adipose tissue mass in obese Zucker rats. J Clin Invest. 1998;101:1354–61. doi: 10.1172/JCI1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamauchi T, Kamon J, Waki H, Murakami K, Motojima K, Komeda K, et al. The mechanisms by which both heterozygous peroxisome proliferator-activated receptor gamma (PPARgamma) deficiency and PPARgamma agonist improve insulin resistance. J Biol Chem. 2001;276:41245–54. doi: 10.1074/jbc.M103241200. [DOI] [PubMed] [Google Scholar]
- Rosen ED, Spiegelman BM. Molecular regulation of adipogenesis. Annu Rev Cell Dev Biol. 2000;16:145–71. doi: 10.1146/annurev.cellbio.16.1.145. [DOI] [PubMed] [Google Scholar]
- Keller H, Givel F, Perroud M, Wahli W. Signaling cross-talk between peroxisome proliferator-activated receptor/retinoid X receptor and estrogen receptor through estrogen response elements. Mol Endocrinol. 1995;9:794–804. doi: 10.1210/mend.9.7.7476963. [DOI] [PubMed] [Google Scholar]
- Nunez SB, Medin JA, Keller H, Wang K, Ozato K, Wahli W, et al. Retinoid X receptor beta and peroxisome proliferator-activated receptor activate an estrogen response element. Recent Prog Horm Res. 1995;50:409–16. doi: 10.1016/b978-0-12-571150-0.50029-9. [DOI] [PubMed] [Google Scholar]
- Zhu Y, Kan L, Qi C, Kanwar YS, Yeldandi AV, Rao MS, et al. Isolation and characterization of peroxisome proliferator-activated receptor (PPAR) interacting protein (PRIP) as a coactivator for PPAR. J Biol Chem. 2000;275:13510–6. doi: 10.1074/jbc.275.18.13510. [DOI] [PubMed] [Google Scholar]
- Nunez SB, Medin JA, Braissant O, Kemp L, Wahli W, Ozato K, et al. Retinoid X receptor and peroxisome proliferator-activated receptor activate an estrogen responsive gene independent of the estrogen receptor. Mol Cell Endocrinol. 1997;127:27–40. doi: 10.1016/s0303-7207(96)03980-9. [DOI] [PubMed] [Google Scholar]
- Tcherepanova I, Puigserver P, Norris JD, Spiegelman BM, McDonnell DP. Modulation of estrogen receptor-alpha transcriptional activity by the coactivator PGC-1. J Biol Chem. 2000;275:16302–8. doi: 10.1074/jbc.M001364200. [DOI] [PubMed] [Google Scholar]
- Liao QC, Li YL, Qin YF, Quarles LD, Xu KK, Li R, et al. Inhibition of adipocyte differentiation by phytoestrogen genistein through a potential downregulation of extracellular signal-regulated kinases 1/2 activity. J Cell Biochem. 2008;104:1853–64. doi: 10.1002/jcb.21753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar R, Thompson EB. The structure of the nuclear hormone receptors. Steroids. 1999;64:310–9. doi: 10.1016/s0039-128x(99)00014-8. [DOI] [PubMed] [Google Scholar]