Abstract
Although treatment utilization for depression and anxiety symptoms has increased substantially in the United States and elsewhere, it remains unclear whether the underlying population distribution of psychological distress is changing over time. We estimated age, period, and cohort effects using data from 2 countries over more than 20 years, including National Health Interview Surveys from 1997 to 2010 (n = 447,058) and Canadian Community Health Surveys from 2000 to 2007 (n = 125,306). Psychological distress was measured with the Kessler Psychological Distress Scale. By period, both countries showed the highest levels of psychological distress in 2001 and the lowest levels in 2007. By age, psychological distress was highest in adolescence and during the late 40s and early 50s. By cohort, Canadian Community Health Survey results indicated a decreasing cohort effect among those born in 1922–1925 through 1935–1939 (β = −0.36, 95% confidence interval: −0.45, −0.27) and then a continuously increasing cohort effect during the remainder of the 20th century through 1989–1992 (β = 0.49, 95% confidence interval: 0.38, 0.61). The National Health Interview Survey data captured earlier-born cohorts and indicated an increased cohort effect for the earliest born (for 1912–1914, β = 0.44, 95% confidence interval: 0.26, 0.61). In sum, individuals in the oldest and more recently born birth cohorts have higher mean psychological distress symptoms compared with those born in midcentury, underscoring the importance of a broad, population-level lens for conceptualizing mental health.
Keywords: age-period-cohort effects, anxiety, Canada, Canadian Community Health Surveys, depression, National Health Interview Surveys, psychological distress, United States
In the past 2 decades, there have been substantial increases in treatment utilization for common psychiatric conditions such as depression and anxiety in many countries (1–5). An open question remains, however, as to what extent the increases in treatment utilization reflect increased ascertainment of existing cases, diagnostic drift to treating less severe cases, or an actual increase in depressive and anxiety symptoms at the population level. To resolve this question, we need data on the community-based distribution of depressive and anxiety symptoms over time.
Studies attempting to address changes in the community-based distribution of depression and anxiety symptoms have been based primarily on cross-sectional samples using retrospective reports. These studies indicate that younger adults are more likely to have a lifetime diagnosis of major depression than older adults (6–11), suggesting an increasing population prevalence in younger generations (typically termed a “cohort effect”), yet retrospective reporting biases in older adults limit inference from cross-sectional studies (12). Longitudinal studies and large meta-analyses of multiple cohorts of children suggest that there were no changes in the incidence and prevalence of major depression, at least in the United States, in the last quarter of the 20th century (13, 14). Similarly, time trend analyses of surveillance data indicate little change in psychological distress from 1997 through 2004 (5).
Population-based data regarding cohort effects on symptoms of psychological distress from the last 10 years are scant; thus, recent trends are virtually unknown. This is critical, because new and emerging risk factors (e.g., social media use (15–17)), as well as changes in established risk factors (e.g., nonmedical prescription drug use, binge drinking (18, 19)) are known to have occurred over this epoch. The extent to which psychological distress has changed over the same period, however, remains unexplored.
Further, a lack of overall population-level changes in prevalence over time could be masking important underlying changes. Specifically, the issue of whether or not there is a cohort effect in common mental health problems in more recent generations is complicated by 2 additional time-varying factors: age effects and period effects. Symptoms of psychological distress follow specific developmental trajectories, with the onset of symptoms most commonly occurring during adolescence (20), heightened levels of psychological distress throughout the adolescent and early adult periods (21), and lower yet varying levels of symptoms thereafter. Thus, it is critical to account for age effects when attempting to isolate cohort effects. Further, overall secular trends that occur across all age groups, known commonly as “period effects,” could also obscure cohort effects unless properly modeled. Existing age-period-cohort (APC) analyses of depressive and anxiety symptoms are few (9, 22, 23) and are based on data that do not reflect current population trends.
To examine whether the distribution of depressive and anxiety symptoms in nontreated population samples has been shifting in recent decades, we need data that repeatedly measure these symptoms across a range of birth cohorts and time periods. The present study uses nationally representative data from 1997 to 2011 with consistent measures of psychological distress from the United States and Canada over the last 15 years to examine whether there is evidence for APC effects at the population level.
METHODS
Sample
National Health Interview Survey
The National Health Interview Survey (NHIS) is a nationally representative, annual cross-sectional survey of noninstitutionalized household civilian adults (aged ≥18 years) in the United States, conducted by the National Center for Health Statistics and the US Census Bureau (18). Assessments are conducted in person in the respondents’ households. The topic of psychological distress was introduced into the survey in 1997 (24). We used data from heads of households, with a total sample size of 447,058 (range, 36,116 (in 1997) to 21,781 (in 2008)). In all US-based surveillance surveys, response rates have declined in the past decade. In these data, response rates similarly fell from greater than 90% in 1997–2000 to 79.5% in 2010 (18). Nonresponse weighting adjustments are included in the sampling weights.
Canadian Community Health Survey
Canadian Community Health Survey (CCHS) cycles 2000–2001, 2003, 2005, and 2007 were analyzed using the public release data files. The CCHS is a cross-sectional survey conducted by Statistics Canada (http://www.statcan.gc.ca) examining individuals aged 12 years and older living in private dwellings in all 13 Canadian provinces and territories. The survey excludes those living on Indian reserves or Crown lands and those in the armed forces, and the public use files do not include data from the 3 Canadian territories. Approximately 130,000 respondents were surveyed in each cycle; response rates ranged from 77.6% (in 2007) to 84.7% (in 2000–2001). Select provinces per cycle included psychological distress measures; the percentage of respondents who received psychological distress measures ranged from 9.3% in 2003 to 47.2% in 2005, for a total analytical sample size of 126,306.
Note that the age ranges in the 2 surveys differ, with the CCHS beginning at age 12 years and the NHIS beginning at age 18 years. Further, the time periods of the 2 surveys differ, with the CCHS covering 2000–2001, 2003, 2005, and 2007 and the NHIS covering the continuous period from 1997 through 2011. Because of these differences in age and period coverage, we were able to include more information on younger birth cohorts in the CCHS and more information on older birth cohorts in the NHIS.
Measures
Psychological distress and depressive symptoms
Psychological distress was measured in both the NHIS and CCHS through the 6-Item Kessler Psychological Distress Scale (K-6) (24, 25). The K-6 queries the frequency of 6 items related to nonspecific and nondiagnostic psychological distress experienced in the past 30 days on a 5-point scale from “all of the time” to “none of the time.” Respondents were asked how often they feel 1) nervous, 2) hopeless, 3) restless or fidgety, 4) so depressed that nothing could cheer you up, 5) that everything was an effort, and 6) worthless. The K-6 has good reliability and validity as a continuous measure of nonspecific psychological distress in both US (5, 24, 25) and international samples (26, 27).
The CCHS included the 10-Item Kessler Psychological Distress Scale (K-10), measured in 2003, 2005, and 2007, and the Composite International Diagnostic Interview Short Form (CIDI-SF) depression scale (measured at all waves). The K-10 includes the 6 questions from the K-6 plus 4 additional questions; a direct comparison found little difference between the 2 instruments for assessing depressive and anxiety symptoms in a general population sample (27).
Doctor-diagnosed depression
One concern about the interpretation of trends in symptoms versus trends in ascertainment is that, because respondents are more likely to receive treatment for psychological distress over time, psychological distress symptoms may decrease in the population because of treatment; alternatively, individuals may be more likely to report higher levels of psychological distress because of increased awareness of their moods. In the CCHS, respondents were asked separately whether a doctor had ever diagnosed them with a mood disorder or anxiety disorder; example disorders were given for each. In a supplementary analysis, we examined APC models among those with no lifetime doctor diagnosis of a mood disorder to separate trends in ascertainment of cases from underlying symptom development.
Age, period, and birth cohort
In the CCHS, information on age was available within the following ranges: 12–14 years, and then 5-year age groups beginning with 15–19 years and continuing through 75–79 years. Data from individuals over 80 years of age were grouped together. To estimate the range of birth cohorts for each age group, we estimate the mean age within the category (e.g., age 13 years for the group aged 12–14 years, age 17 years for the group aged 15–19 years), subtracted the mean age from the survey year, and estimated the 5-year bounds around that subtracted estimate.
In the NHIS, individual year of age was available for all respondents. Birth cohort was calculated by subtracting individual age from the survey year and then grouped into 5-year categories.
Sociodemographic variables
In both the CCHS and the NHIS, we estimated APC models separately by sex, as well as highest level of household education as follows: 1) less than high school; 2) completed high school; 3) some postsecondary education; 4) postsecondary education graduate. Household education was used because individuals in the CCHS were as young as 12 years and may not have achieved their final educational positions.
Statistical analysis
In the CCHS, not all provinces included the K-6 measure in all waves. Mean K-6 score differed significantly by province (F = 294.81, degrees of freedom = 9, P < 0.001). Subjects from Quebec had the highest mean psychological distress scores, and subjects from Ontario had the lowest. These differences confound trends over time; thus, we regressed the K-6 scale on a categorical indicator of province across the 4 waves to factor out variance in the measure due to province. Residual values no longer had any relation to province. We used the residual as our measure of psychological distress in APC modeling of CCHS data.
Next, we examined the demographic distribution of psychological distress by sex, age, and education, testing for differences within survey wave with linear regression. Finally, we used the intrinsic estimator (IE) for APC analysis, using the approach developed by Yang et al. (28–30). We provide a detailed overview of the IE in Web material (available at http://aje.oxfordjournals.org/). Briefly, the IE provides a unique estimable function that is invariant to model constraints; substantial research has demonstrated the statistical properties of the IE for valid APC analysis (28–30). The IE produces coefficients of the effects of age, period, and cohort, and these coefficients provide estimates of the mean change in psychological distress associated with a particular APC group relative to the mean for all APC groups combined. We use the publicly available add-on file for the IE algorithm (29), available in Stata statistical software (31).
We estimated APC effects by country, sex, and highest and lowest levels of completed education; in the CCHS, we additionally estimated APC effects among those with no history of doctor-diagnosed depression or anxiety. In the CCHS, we also used the K-10 and CIDI-SF depression scores as additional supplementary outcomes. In a sensitivity analysis, we analyzed K-6 as an outcome in Quebec separately because Quebec was the only province that included the K-6 measure in at least 3 waves of the study.
RESULTS
Demographic correlates of psychological distress at each wave
CCHS
In Table 1 we describe the demographic distribution of K-6 residuals after regressing out the effect of province. Women had higher distress than men at each wave. By age, those who were 21–25 years had the highest level of distress at each wave. By education, those with a high school degree but no postsecondary degree had the highest level of distress in 2000–2001, 2005, and 2007. Those with less than a high school education had the highest level of distress in 2003.
Table 1.
Demographic Distribution of Psychological Distressa in the Canadian General Population (n = 126,306), 2000–2007
| Characteristic | Residual K-6 Valuesb After Province Regression (SE) by Year |
|||
|---|---|---|---|---|
| 2000–2001 | 2003 | 2005 | 2007 | |
| Sex | ||||
| Male | −0.19 (0.02) | −0.23 (0.01) | −0.28 (0.06) | −0.56 (0.07) |
| Female | 0.72 (0.06) | 0.13 (0.01) | 0.21 (0.03) | 0.04 (0.02) |
| Age, years | ||||
| 12–14 | 0.39 (0.02) | −0.08 (0.08) | 0.41 (0.09) | −0.13 (0.18) |
| 15–17 | 1.13 (0.05) | 0.60 (0.14) | 0.91 (0.04) | 0.66 (0.03) |
| 18–20 | ||||
| 21–25 | 1.23 (0.10) | 0.59 (0.08) | 0.82 (0.05) | 0.24 (0.02) |
| 26–30 | 0.68 (0.06) | 0.31 (0.06) | 0.40 (0.03) | 0.20 (0.03) |
| 31–35 | 0.46 (0.03) | −0.07 (0.04) | 0.07 (0.110) | 0.00 (0.01) |
| 36–40 | 0.57 (0.06) | −0.06 (0.09) | 0.08 (0.03) | −0.12 (0.10) |
| 41–45 | 0.32 (0.04) | −0.10 (0.05) | −0.04 (0.08) | −0.09 (0.10) |
| 46–50 | 0.35 (0.03) | 0.18 (0.02) | −0.08 (0.03) | −0.27 (0.06) |
| 51–55 | 0.05 (0.03) | −0.23 (0.14) | −0.27 (0.05) | −0.41 (0.02) |
| 56–60 | −0.43 (0.01) | −0.23 (0.10) | −0.44 (0.08) | −0.42 (0.04) |
| 61–65 | −0.69 (0.02) | −0.56 (0.10) | −0.74 (0.02) | −0.76 (0.04) |
| 66–70 | −0.60 (0.03) | −0.41 (0.09) | −0.93 (0.08) | −1.03 (0.03) |
| 71–75 | −0.50 (0.05) | −0.64 (0.05) | −1.09 (0.11) | −1.14 (0.10) |
| 76–80 | −0.30 (0.06) | −0.79 (0.14) | −0.88 (0.03) | −1.20 (0.05) |
| >80 | ||||
| Education | ||||
| Less than high school | 0.50 (0.04 | 0.24 (0.03) | 0.18 (0.13) | −0.17 (0.11) |
| Completed high school | 0.01 (0.02) | −0.02 (0.02) | −0.09 (0.01) | −0.28 (0.07) |
| Some postsecondary but no degree | 0.82 (0.09) | 0.15 (0.06) | 0.45 (0.07) | 0.24 (0.02) |
| Postsecondary degree | 0.12 (0.04) | −0.29 (0.02) | −0.19 (0.03) | −0.35 (0.02) |
Abbreviation: K-6, 6-Item Kessler Psychological Distress Scale; SE, standard error.
a Psychological distress varied across sex, age, and educational level at P < 0.01.
b Psychological distress score based on residual value from linear regression of K-6 score on a categorical indicator of Canadian province of residence because of differential distributions of K-6 values across provinces. The K-6 indicates the frequency of 6 items related to nonspecific and nondiagnostic psychological distress experienced in the past 30 days (24, 25).
NHIS
In Table 2 we describe the demographic correlates of psychological distress at each wave in the NHIS data. Similar to results from the CCHS, results from the NHIS showed that women had consistently higher distress than men. Distress was generally highest in young adulthood (age 18–20 years), declined through early adulthood, and increased again with a peak around age 46–50 years. By education, those in the lowest educational strata consistently had the highest level of psychological distress.
Table 2.
Demographic Distribution of Psychological Distressa in the US General Population (n = 447,058), 1997–2010
| Characteristic | Psychological Distress in the US General Population by Year, mean K-6 scoreb (SE) |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | |
| Sex | |||||||||||||||
| Male | 2.22 (0.04) | 2.05 (0.04) | 1.73 (0.03) | 1.87 (0.04) | 2.29 (0.04) | 1.89 (0.04) | 1.92 (0.04) | 2.02 (0.04) | 1.99 (0.04) | 1.94 (0.04) | 1.84 (0.04) | 2.15 (0.05) | 2.25 (0.05) | 2.31 (0.04) | 2.24 (0.04) |
| Female | 2.85 (0.04) | 2.73 (0.04) | 2.39 (0.04) | 2.48 (0.04) | 2.92 (0.05) | 2.53 (0.04) | 2.64 (0.04) | 2.65 (0.04) | 2.64 (0.04) | 2.56 (0.04) | 2.41 (0.04) | 2.70 (0.05) | 2.77 (0.05) | 2.83 (0.04) | 2.70 (0.04) |
| Age, years | |||||||||||||||
| 18–20 | 2.60 (0.12) | 2.68 (0.15) | 2.30 (0.12) | 2.37 (0.15) | 2.68 (0.13) | 2.23 (0.15) | 2.17 (0.12) | 2.36 (0.18) | 2.48 (0.16) | 2.30 (0.16) | 2.33 (0.20) | 2.76 (0.22) | 2.61 (0.19) | 2.61 (0.17) | 2.40 (0.16) |
| 21–25 | 2.79 (0.09) | 2.62 (0.09) | 2.30 (0.08) | 2.40 (0.09) | 3.02 (0.10) | 2.39 (0.09) | 2.38 (0.11) | 2.57 (0.10) | 2.42 (0.09) | 2.25 (0.09) | 2.19 (0.11) | 2.56 (0.11) | 2.65 (0.10) | 2.74 (0.09) | 2.42 (0.09) |
| 26–30 | 2.45 (0.07) | 2.43 (0.07) | 2.08 (0.07) | 2.24 (0.08) | 2.57 (0.08) | 2.02 (0.07) | 2.35 (0.08) | 2.23 (0.08) | 2.20 (0.08) | 2.28 (0.09) | 2.20 (0.09) | 2.36 (0.10) | 2.68 (0.10) | 2.75 (0.10) | 2.31 (0.07) |
| 31–35 | 2.51 (0.07) | 2.37 (0.07) | 1.98 (0.07) | 2.04 (0.07) | 2.54 (0.08) | 2.12 (0.08) | 2.21 (0.07) | 2.27 (0.08) | 2.17 (0.08) | 2.21 (0.11) | 2.14 (0.08) | 2.42 (0.10) | 2.49 (0.09) | 2.54 (0.09) | 2.58 (0.08) |
| 36–40 | 2.55 (0.07) | 2.33 (0.07) | 2.09 (0.07) | 2.14 (0.07) | 2.68 (0.08) | 2.24 (0.07) | 2.29 (0.08) | 2.33 (0.08) | 2.31 (0.08) | 2.11 (0.09) | 2.11 (0.09) | 2.52 (0.11) | 2.61 (0.11) | 2.68 (0.09) | 2.42 (0.08) |
| 41–45 | 2.63 (0.07) | 2.45 (0.08) | 2.19 (0.08) | 2.25 (0.08) | 2.53 (0.08) | 2.25 (0.08) | 2.34 (0.08) | 2.40 (0.08) | 2.37 (0.07) | 2.18 (0.10) | 2.15 (0.09) | 2.40 (0.10) | 2.86 (0.12) | 2.57 (0.10) | 2.55 (0.09) |
| 46–50 | 2.61 (0.08) | 2.33 (0.07) | 2.20 (0.08) | 2.30 (0.08) | 2.75 (0.09) | 2.48 (0.09) | 2.28 (0.09) | 2.53 (0.09) | 2.39 (0.08) | 2.40 (0.09) | 2.32 (0.10) | 2.53 (0.10) | 2.74 (0.10) | 2.67 (0.08) | 2.68 (0.09) |
| 51–55 | 2.74 (0.09) | 2.64 (0.10) | 2.22 (0.09) | 2.34 (0.10) | 2.76 (0.09) | 2.55 (0.11) | 2.49 (0.08) | 2.47 (0.09) | 2.61 (0.09) | 2.54 (0.11) | 2.08 (0.10) | 2.68 (0.11) | 2.54 (0.10) | 2.75 (0.11) | 2.65 (0.09) |
| 56–60 | 2.43 (0.10) | 2.40 (0.11) | 2.06 (0.10) | 2.08 (0.10) | 2.77 (0.10) | 2.35 (0.10) | 2.59 (0.11) | 2.43 (0.09) | 2.41 (0.09) | 2.48 (0.11) | 2.33 (0.11) | 2.55 (0.11) | 2.60 (0.11) | 3.02 (0.11) | 2.96 (0.11) |
| 61–65 | 2.41 (0.10) | 2.02 (0.10) | 1.83 (0.10) | 1.95 (0.10) | 2.39 (0.11) | 1.95 (0.09) | 2.19 (0.10) | 2.23 (0.10) | 2.12 (0.09) | 2.27 (0.12) | 2.13 (0.14) | 2.41 (0.11) | 2.38 (0.10) | 2.48 (0.10) | 2.47 (0.09) |
| 66–70 | 2.19 (0.09) | 2.06 (0.10) | 1.71 (0.11) | 2.07 (0.12) | 2.29 (0.10) | 1.75 (0.09) | 1.97 (0.10) | 1.96 (0.10) | 2.01 (0.09) | 1.95 (0.11) | 1.83 (0.12) | 1.97 (0.11) | 1.89 (0.10) | 2.16 (0.09) | 2.21 (0.09) |
| 71–75 | 2.14 (0.10) | 2.14 (0.11) | 1.53 (0.09) | 2.03 (0.10) | 2.24 (0.11) | 2.03 (0.12) | 2.06 (0.11) | 1.94 (0.10) | 2.07 (0.11) | 2.00 (0.14) | 2.01 (0.14) | 1.95 (0.12) | 1.96 (0.12) | 1.92 (0.10) | 2.09 (0.10) |
| 76–80 | 2.55 (0.12) | 2.36 (0.12) | 1.88 (0.10) | 1.94 (0.11) | 2.23 (0.11) | 1.81 (0.11) | 1.92 (0.12) | 2.32 (0.11) | 2.39 (0.13) | 2.09 (0.14) | 1.83 (0.12) | 2.00 (0.13) | 1.97 (0.12) | 1.95 (0.12) | 1.91 (0.11) |
| >80 | 2.89 (0.12) | 2.73 (0.13) | 2.09 (0.12) | 2.19 (0.10) | 2.54 (0.11) | 2.20 (0.12) | 2.25 (0.11) | 2.32 (0.10) | 2.44 (0.11) | 2.19 (0.11) | 1.83 (0.11) | 2.42 (0.14) | 2.19 (0.13) | 2.12 (0.09) | 2.15 (0.09) |
| Education | |||||||||||||||
| Less than high school | 3.48 (0.07) | 3.35 (0.08) | 2.67 (0.07) | 2.99 (0.09) | 3.50 (0.09) | 2.95 (0.08) | 3.10 (0.09) | 3.28 (0.09) | 3.23 (0.08) | 3.01 (0.10) | 2.74 (0.09) | 3.25 (0.10) | 3.29 (0.10) | 3.46 (0.09) | 3.48 (0.08) |
| Completed high school | 2.52 (0.05) | 2.42 (0.05) | 2.15 (0.05) | 2.24 (0.05) | 2.63 (0.05) | 2.33 (0.06) | 2.29 (0.06) | 2.44 (0.05) | 2.41 (0.05) | 2.31 (0.06) | 2.35 (0.07) | 2.60 (0.07) | 2.75 (0.07) | 2.78 (0.06) | 2.73 (0.06) |
| Some postsecondary but no degree | 2.56 (0.05) | 2.41 (0.05) | 2.15 (0.05) | 2.26 (0.06) | 2.70 (0.06) | 2.23 (0.05) | 2.41 (0.06) | 2.39 (0.06) | 2.40 (0.06) | 2.46 (0.07) | 2.21 (0.07) | 2.52 (0.08) | 2.66 (0.08) | 2.74 (0.07) | 2.58 (0.05) |
| Postsecondary degree | 1.99 (0.04) | 1.85 (0.04) | 1.65 (0.04) | 1.67 (0.04) | 2.10 (0.04) | 1.77 (0.04) | 1.81 (0.04) | 1.83 (0.04) | 1.82 (0.04) | 1.77 (0.04) | 1.68 (0.04) | 1.93 (0.05) | 1.96 (0.04) | 2.04 (0.04) | 1.88 (0.03) |
Abbreviation: K-6, 6-Item Kessler Psychological Distress Scale; SE, standard error.
a Psychological distress varied across sex, age, and education at P < 0.01.
Age, period, and cohort effects in psychological distress
Age effects
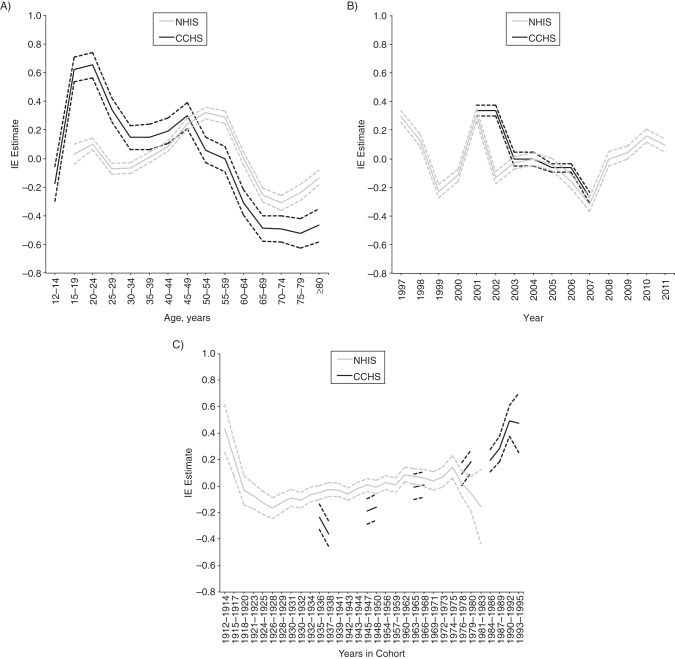
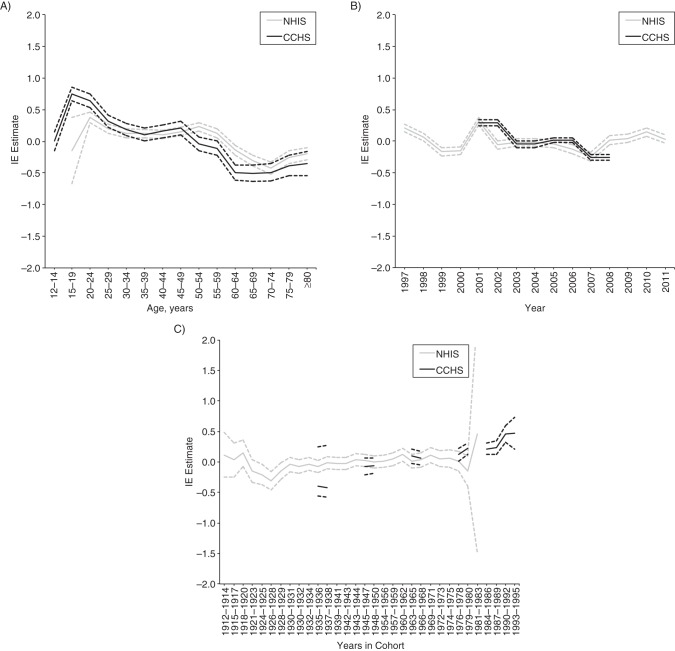
In the CCHS, psychological distress was highest in late adolescence and early adulthood. Distress peaked at age 20–24 years (β = 0.65, 95% confidence interval (CI): 0.56, 0.74), with a rapid decline thereafter except for a noticeable increase at age 45–49 years (β = 0.30, 95% CI: 0.21, 0.39). In the NHIS, psychological distress peaked at age 50–54 years (β = 0.32, 95% CI: 0.28, 0.36) (Figure 1).
Figure 1.
A) Age, B) period, and C) cohort effects in psychological distress in the Canadian general population (n = 126,306), 2000–2007, and the US general population (n = 447,058), 1997–2011. The intrinsic estimator (IE) estimate is the mean change in psychological distress associated with a particular age-period-cohort group relative to the mean for all age-period-cohort groups combined. CCHS, Canadian Community Health Survey; NHIS, National Health Interview Survey. Solid lines, IE estimates; dotted lines, 95% confidence intervals.
Period effects
In both the CCHS and the NHIS, psychological distress was highest in 2000–2001 (in the CCHS, β = 0.34, 95% CI: 0.30, 0.37; in the NHIS: β = 0.30, 95% CI: 0.26, 0.35). The NHIS data also indicated a peak in the period effect in 1997, as well as increases in the period effect from 2008 to 2010 (Figure 1).
Cohort effects
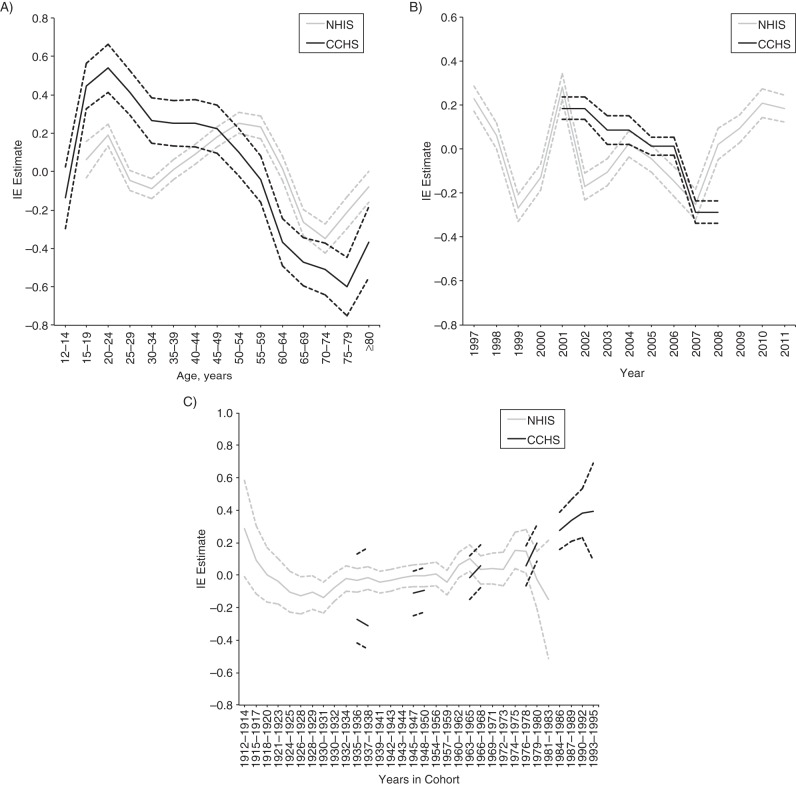
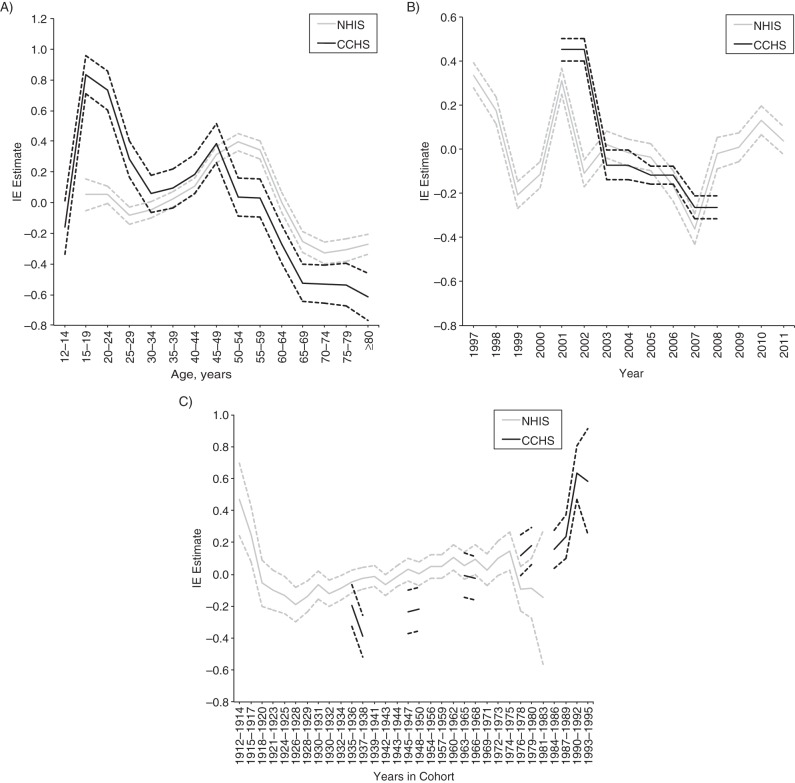
In the CCHS, cohort effects indicated a J-shaped curve in psychological distress, with a decreasing cohort effect among those born in 1922–1925 through 1935–1939 (β = −0.36, 95% CI: −0.45, −0.27) and then a continuously increasing cohort effect among those born across the remainder of the 20th century through the 1989–1992 cohort (β = 0.49, 95% CI: 0.38, 0.61). The NHIS data were able to capture earlier-born cohorts compared with the CCHS, and these data indicated an increased cohort effect for the earliest born (in 1912–1914, β = 0.44, 95% CI: 0.26, 0.61). After a decrease in the cohort effect among those born in 1912–1914 through the 1925 cohort, the cohort effect gradually increased until the 1975 cohort, after which the cohort effect in psychological distress decreased until the latest-born cohort in 1984–1986 (Figure 1). Results stratified by sex were generally consistent with the whole sample, although the increase in psychological distress among those aged 50–54 years in the CCHS was less pronounced in men (Figure 2) than in women (Figure 3).
Figure 2.
A) Age, B) period, and C) cohort effects in psychological distress in the Canadian male population (n = 57,161), 2000–2007, and the US male population (n = 195,636) 1997–2011. The intrinsic estimator (IE) estimate is the mean change in psychological distress associated with a particular age-period-cohort group relative to the mean for all age-period-cohort groups combined. CCHS, Canadian Community Health Survey; NHIS, National Health Interview Survey. Solid lines, IE estimates; dotted lines, 95% confidence intervals.
Figure 3.
A) Age, B) period, and C) cohort effects in psychological distress in the Canadian female population (n = 69,145), 2000–2007, and the US female population (n = 251,422), 1997–2011. The intrinsic estimator (IE) estimate is the mean change in psychological distress associated with a particular age-period-cohort group relative to the mean for all age-period-cohort groups combined. CCHS, Canadian Community Health Survey; NHIS, National Health Interview Survey. Solid lines, IE estimates; dotted lines, 95% confidence intervals.
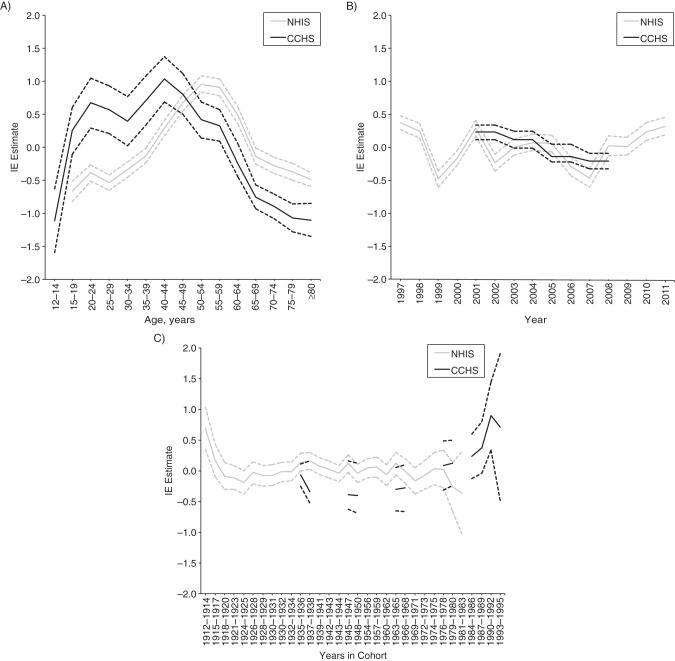
By lowest and highest education
Results indicated that age and period effects were more pronounced in those with low household education (Figure 4). Cohort effects were generally consistent. One notable difference is that the 1984–1986 cohort had an increase in the cohort effect in the NHIS data for those in the high educational strata only, although the confidence interval was wide (β = 0.47, 95% CI: −1.49, 2.4) (Figure 5).
Figure 4.
A) Age, B) period, and C) cohort effects in psychological distress in the Canadian population with lower household educational attainment (n = 78,629), 2000–2007, and the US population with lower household educational attainment (n = 145,919), 1997–2011. The intrinsic estimator (IE) estimate is the mean change in psychological distress associated with a particular age-period-cohort group relative to the mean for all age-period-cohort groups combined. CCHS, Canadian Community Health Survey; NHIS, National Health Interview Survey. Solid lines, IE estimates; dotted lines, 95% confidence intervals.
Figure 5.
A) Age, B) period, and C) cohort effects in psychological distress in the Canadian population with higher household educational attainment (n = 41,405), 2000–2007, and the US population with higher household educational attainment (n = 86,007), 1997–2011. The intrinsic estimator (IE) estimate is the mean change in psychological distress associated with a particular age-period-cohort group relative to the mean for all age-period-cohort groups combined. CCHS, Canadian Community Health Survey; NHIS, National Health Interview Survey. Solid lines, IE estimates; dotted lines, 95% confidence intervals.
Sensitivity analyses
Because sensitivity analyses were conducted only in the CCHS without comparison to the NHIS, we estimated wider cohort groups to show a continuous trend line. Models indicated no change in the underlying APC effects among those with no diagnosed depression and no diagnosed anxiety (Web Figure 1) and when using the K-10 score rather than K-6 score as the outcome (Web Figure 2). Similar to the main analysis, in all sensitivity analyses, age effects peaked in young adulthood and middle age (45–49 years), period effects decreased across waves of data collection, and cohort effects indicated a general increase in psychological distress symptoms among more recently born cohorts. When examining the CIDI-SF as an outcome (Web Figure 2), we found that the age effect peaked at 20–24 years (β = 0.21, 95% CI: 0.18, 0.24). Period and cohort effects were similar. Finally, in Quebec, the only province with K-6 measures in at least 3 waves, APC effects were similar to those in the main analysis (Web Figure 3).
DISCUSSION
The present study estimates APC effects in nonspecific psychological distress across the general population of Canada in the last decade and in the United States across the last 2 decades. In the United States, the oldest birth cohorts (born 1912–1914) demonstrate the highest levels of psychological distress, with a decrease thereafter, a gradual increase from cohorts born in the mid-1920s through the late 1970s, and a decrease among cohorts born in the early- to mid-1980s. In the CCHS, there is a general increase in psychological distress from cohorts born in the mid-1930s through the early- to mid-1990s. We demonstrate these effects while factoring out variance attributable to age and time period and demonstrate consistency of the effect by sex and educational status and among those with no history of doctor-diagnosed depression or anxiety disorder. Taken together, these findings indicate converging evidence for a change in the mean population level of psychological distress across birth cohorts, with evidence for higher overall risk in the very old and the very young.
Of note, we see in these data countervailing effects for some periods of time, with decreasing period effects at the same time cohort effects are increasing. Formal APC analyses allowed for the detection of these types of countervailing effects. Several previous longitudinal studies found no increase in depressive symptoms in more recent cohorts (13, 14) and suggested that increases in prevalence based on clinical visits are an artifact of increased ascertainment (1, 2, 4). A previous study examining time trends in K-6 symptoms in NHIS data from 1997 through 2004 documented little change over time (5); however, we demonstrate that many of the increases in K-6 scores occurred after 2004. The current APC analysis suggests that prior findings of no change over time could be caused in part by the balancing of negative period effects with positive cohort effects.
Increases in psychological distress among younger birth cohorts in Canada now aging into their 20s could indicate a confluence of both macro-level social and environmental factors in how young adults engage with each other and with the broader environment. We note that we did not have comparable data on birth cohorts in the United States, and available data indicate that birth cohorts of the early 1980s did not show a similar increase in psychological distress. Nonetheless, speculation regarding the drivers of the increase among young Canadians is potentially hypothesis generating. For example, the global financial downturn in economic activity in the past several years has been particularly problematic for young adults emerging into the labor market (32). Increases in psychological distress among young Canadian adults could, in part, reflect financial stress. Alternatively, or in addition, emerging research suggests that young people who engage with online social media can have elevated symptoms of anxiety and depression through increased online cyber-bullying and perceptions of inadequacy in comparison to peers (15–17, 25). Finally, there is evidence of cohort effects in substance use, including binge drinking (33), marijuana use (34, 35), and increasingly, the nonmedical use of prescription medication (19, 36). Given correlations between substance use and depressive symptoms (29, 37), increases in prescription drug use could be a potential driver of the cohort effects in psychological distress, or vice versa. The present study does not estimate the contribution of these factors; rather we document APC effects, allowing for generative hypotheses about how these effects may have arisen, potentially through macro-level processes.
The age effects in psychological distress were similar between the 2 countries within the age overlap across studies, though there was a peak in distress slightly earlier (at age 45–49 years) in the Canadian data compared with the US data (at age 50–54 years). In Canada, we were able to document a late adolescent peak in psychological distress, consistent with other research (6, 14, 38). Previous studies have indicated that psychological distress among women increases in the late 40s, coincident with the perimenopausal period of life (19). This is consistent with our evidence indicating that the age effect in this life stage was more pronounced among women than men. It is also possible that the interpretation and meaning of psychological distress questions change across ages; thus, measurement invariance underlying at least some of these effects is possible.
Period effects were also consistent across the 2 studies within the time period that overlapped between studies. In the Canadian data, distress symptoms were highest in 2000–2001, and the period effect decreased thereafter through 2007. In the US data, we see the same decreased period effect over the same period, but unlike in the Canadian data, we are able to contrast the trend across the early- to mid-2000s with trends before and after that period. It seems reasonable to hypothesize that the attack on the World Trade Center on September 11, 2001, may at least in part underlie this period effect (39). However, most of the interviews for both studies were conducted prior to September 2001, suggesting that the World Trade Center attacks may not be a full explanation. The US data also indicate increasing period effects from 2007 to 2010; these increases are coincident with the major financial crises in the United States and subsequent economic recession.
More broadly, whereas APC analyses are descriptive and do not test specific mechanistic hypotheses, they suggest the potential importance of social, economic, and cultural environments in shaping mental health. There is an increasing focus in research on identifying the neurobiological and genetic underpinnings of depression and other mental health outcomes, drilling down to understand the molecular and biological roots of these disorders. Although identification of these micro-level mechanisms is important, we suggest that a complementary focus on the macro-level exposures that create broad population shifts in outcomes, such as depressive and anxiety symptoms, is also important for 2 reasons. First, macro-level exposures that drive shifts in population prevalence over time may be crucial causes of psychological distress to identify for prevention and intervention (40) but are difficult to quantify in traditional studies because they are ubiquitous in the population at any 1 point in time. Second, quantifying risks associated with such macro-level exposures may be important for the prediction and forecasting of future trends in mental health outcomes (41).
Limitations of the studies are noted. First, in the CCHS, not all provinces included measures of psychological distress at all waves, and there were differences in mean psychological distress across provinces. We addressed this analytically by factoring out variance due to province from the estimates by using linear regression, but we note that some residual confounding due to province is possible. Second, psychological distress is based on self-report of the respondents rather than clinical diagnoses in both studies. However, the K-6 scale is widely used, well validated, and reliable (5, 24, 25). Further, we were able to document similar effects using alternative outcomes in the CCHS, including the K-10 and CIDI-SF depressive symptom scales.
The substantial strengths of this study mitigate the limitations. The present study is the largest to date to examine APC effects in psychological distress. Data are drawn from 2 countries containing a diverse array of provinces and subpopulations. Our data indicate that individuals in the oldest cohorts (in the United States), as well as more recently born cohorts (in Canada), have higher psychological distress, signaling a potential need for the promotion of treatment resources. At the same time, overall levels of psychological distress are also increasing in the population, based on US data after 2007, suggesting that broad macro-level mechanisms that negatively affect mental health should be measured and incorporated into ongoing surveillance efforts.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, Columbia University, New York, New York (Katherine M. Keyes); Department of Psychology, University of Manitoba, Winnipeg, Manitoba, Canada (Ryan Nicholson, Jolene Kinley); Department of Psychiatry, Stanford University, Stanford, California (Sarah Raposo); Department of Psychiatry, University of California San Diego, San Diego, California (Murray B. Stein); Department of Family and Preventive Medicine, University of California San Diego, San Diego, California (Murray B. Stein); Veterans Affairs San Diego Health Care System, San Diego, California (Murray B. Stein); Faculty of Health Sciences, Simon Fraser University, Vancouver, British Columbia, Canada (Elliot M. Goldner); Department of Psychiatry, University of Manitoba, Winnipeg, Manitoba, Canada (Jitender Sareen); Department of Psychology, University of Manitoba, Winnipeg, Manitoba, Canada (Jitender Sareen); and Department of Community Health Sciences, University of Manitoba, Winnipeg, Manitoba, Canada (Jitender Sareen).
This study was supported by the National Institutes of Health (grant K01-AA021511 to K.M.K.) and the Manitoba Health Research Council Chair Award to J.S.
Conflict of interest: none declared.
REFERENCES
- 1.Marcus SC, Olfson M. National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry. 2010;67(12):1265–1273. doi: 10.1001/archgenpsychiatry.2010.151. [DOI] [PubMed] [Google Scholar]
- 2.Moreno C, Laje G, Blanco C, et al. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch Gen Psychiatry. 2007;64(9):1032–1039. doi: 10.1001/archpsyc.64.9.1032. [DOI] [PubMed] [Google Scholar]
- 3.Olfson M, Marcus SC. National patterns in antidepressant medication treatment. Arch Gen Psychiatry. 2009;66(8):848–856. doi: 10.1001/archgenpsychiatry.2009.81. [DOI] [PubMed] [Google Scholar]
- 4.Olfson M, Marcus SC, Druss B, et al. National trends in the outpatient treatment of depression. JAMA. 2002;287(2):203–209. doi: 10.1001/jama.287.2.203. [DOI] [PubMed] [Google Scholar]
- 5.Pirraglia PA, Hampton JM, Rosen AB, et al. Psychological distress and trends in healthcare expenditures and outpatient healthcare. Am J Manag Care. 2011;17(5):319–328. [PMC free article] [PubMed] [Google Scholar]
- 6.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC, McGonagle KA, Nelson CB, et al. Sex and depression in the national comorbidity survey. II: Cohort effects. J Affect Disord. 1994;30(1):15–26. doi: 10.1016/0165-0327(94)90147-3. [DOI] [PubMed] [Google Scholar]
- 8.Klerman GL, Weissman MM. Increasing rates of depression. JAMA. 1989;261(15):2229–2235. [PubMed] [Google Scholar]
- 9.Wickramaratne PJ, Weissman MM, Leaf PJ, et al. Age, period and cohort effects on the risk of major depression: results from five United States communities. J Clin Epidemiol. 1989;42(4):333–343. doi: 10.1016/0895-4356(89)90038-3. [DOI] [PubMed] [Google Scholar]
- 10.Leon AC, Klerman GL, Wickramaratne P. Continuing female predominance in depressive illness. Am J Public Health. 1993;83(5):754–757. doi: 10.2105/ajph.83.5.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burke KC, Burke JD, Jr, Rae DS, et al. Comparing age at onset of major depression and other psychiatric disorders by birth cohorts in five US community populations. Arch Gen Psychiatry. 1991;48(9):789–795. doi: 10.1001/archpsyc.1991.01810330013002. [DOI] [PubMed] [Google Scholar]
- 12.Keyes KM, Liu X. Age, period, and birth cohort effects in psychiatric disorders in the USA. In: Koenen K, Rudenstine S, Susser E, Galea S, editors. A Life Course Approach to Mental Disorders. New York, NY: Oxford University Press; 2013. pp. 46–57. [Google Scholar]
- 13.Jane Costello E, Erkanli A, Angold A. Is there an epidemic of child or adolescent depression? J Child Psychol Psychiatry. 2006;47(12):1263–1271. doi: 10.1111/j.1469-7610.2006.01682.x. [DOI] [PubMed] [Google Scholar]
- 14.Murphy JM, Laird NM, Monson RR, et al. Incidence of depression in the Stirling County Study: historical and comparative perspectives. Psychol Med. 2000;30(3):505–514. doi: 10.1017/s0033291799002044. [DOI] [PubMed] [Google Scholar]
- 15.Przybylski AK, Murayama K, DeHaan CR, et al. Motivational, emotional, and behavioral correlates of fear of missing out. Comput Human Behav. 2013;29(4):1841–1848. [Google Scholar]
- 16.Bauman S, Toomey RB, Walker JL. Associations among bullying, cyberbullying, and suicide in high school students. J Adolesc. 2013;36(2):341–350. doi: 10.1016/j.adolescence.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 17.Krasnova H, Wenninger H, Widjaja T, et al. Envy on Facebook: A Hidden Threat to Users’ Life Satisfaction?. Presented at: International Conference on Wirtschaftsinformatik/Business Information Systems; February 27–March 1, 2013; Leipzig, Germany. [Google Scholar]
- 18.National Health Interview Survey. Centers for Disease Control and Prevention. 2013. http://www.cdc.gov/nchs/nhis.htm . Accessed March 12, 2014.
- 19.Martins SS, Keyes KM, Storr CL, et al. Birth-cohort trends in lifetime and past-year prescription opioid-use disorder resulting from nonmedical use: results from two national surveys. J Stud Alcohol Drugs. 2010;71(4):480–487. doi: 10.15288/jsad.2010.71.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hasin DS, Goodwin RD, Stinson FS, et al. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 21.Jager J. A developmental shift in black-white differences in depressive affect across adolescence and early adulthood: the influence of early adult social roles and socio-economic status. Int J Behav Dev. 2011;35(5):457–469. doi: 10.1177/0165025411417504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lavori PW, Klerman GL, Keller MB, et al. Age-period-cohort analysis of secular trends in onset of major depression: findings in siblings of patients with major affective disorder. J Psychiatr Res. 1987;21(1):23–35. doi: 10.1016/0022-3956(87)90006-9. [DOI] [PubMed] [Google Scholar]
- 23.Warshaw MG, Klerman GL, Lavori PW. The use of conditional probabilities to examine age-period-cohort data: further evidence for a period effect in major depressive disorder. J Affect Disord. 1991;23(3):119–129. doi: 10.1016/0165-0327(91)90024-m. [DOI] [PubMed] [Google Scholar]
- 24.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 25.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 26.Andrews G, Slade T. Interpreting scores on the Kessler Psychological Distress Scale (K10) Aust N Z J Public Health. 2001;25(6):494–497. doi: 10.1111/j.1467-842x.2001.tb00310.x. [DOI] [PubMed] [Google Scholar]
- 27.Furukawa TA, Kessler RC, Slade T, et al. The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychol Med. 2003;33(2):357–362. doi: 10.1017/s0033291702006700. [DOI] [PubMed] [Google Scholar]
- 28.Yang Y, Fu WJ, Land KC. A methodological comparison of age-period-cohort models: the intrinsic estimator and conventional generalized linear models. Sociol Methodol. 2004;34(1):75–110. [Google Scholar]
- 29.Yang Y, Schulhofer-Wohl S, Fu WJ, et al. The intrinsic estimator for age-period-cohort analysis: what it is and how to use it. AJS. 2008;113(6):1697–1736. [Google Scholar]
- 30.Fu WJ. Ridge estimator in singulah oesiun with application to age-period-cohort analysis of disease rates. Commun Stat Theor Methods. 2000;29(2):263–278. [Google Scholar]
- 31.Stata Corporation. College Station, TX: Stata Corporation; 2005. Stata statistical software, release 9. [Google Scholar]
- 32.Stuckler D, Basu S. The Body Economic: Why Austerity Kills. New York, NY: Basic Books; 2013. [Google Scholar]
- 33.Keyes KM, Miech R. Age, period, and cohort effects in heavy episodic drinking in the US from 1985 to 2009. Drug Alcohol Depend. 2013;132(1-2):140–148. doi: 10.1016/j.drugalcdep.2013.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Keyes KM, Schulenberg JE, O'Malley PM, et al. The social norms of birth cohorts and adolescent marijuana use in the United States, 1976–2007. Addiction. 2011;106(10):1790–1800. doi: 10.1111/j.1360-0443.2011.03485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miech R, Koester S. Trends in U.S., past-year marijuana use from 1985 to 2009: an age-period-cohort analysis. Drug Alcohol Depend. 2012;124(3):259–267. doi: 10.1016/j.drugalcdep.2012.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Miech R, Bohnert A, Heard K, et al. Increasing use of nonmedical analgesics among younger cohorts in the United States: a birth cohort effect. J Adolesc Health. 2013;52(1):35–41. doi: 10.1016/j.jadohealth.2012.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cerdá M, Bordelois PM, Keyes KM, et al. Cumulative and recent psychiatric symptoms as predictors of substance use onset: Does timing matter? Addiction. 2013;108(12):2119–2128. doi: 10.1111/add.12323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Seedat S, Scott KM, Angermeyer MC, et al. Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Arch Gen Psychiatry. 2009;66(7):785–795. doi: 10.1001/archgenpsychiatry.2009.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Henriksen CA, Bolton JM, Sareen J. The psychological impact of terrorist attacks: examining a dose-response relationship between exposure to 9/11 and Axis I mental disorders. Depress Anxiety. 2010;27(11):993–1000. doi: 10.1002/da.20742. [DOI] [PubMed] [Google Scholar]
- 40.Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985;14(1):32–38. doi: 10.1093/ije/14.1.32. [DOI] [PubMed] [Google Scholar]
- 41.Janssens AC, van Duijn CM. Genome-based prediction of common diseases: advances and prospects. Hum Mol Genet. 2008;17(R2):R166–R173. doi: 10.1093/hmg/ddn250. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.