Abstract
Childhood obesity has become major health concern for physicians, parents, and health agencies around the world. Childhood obesity is associated with an increased risk for other diseases not only during youth but also later in life, including diabetes, arterial hypertension, coronary artery disease, and fatty liver disease. Importantly, obesity accelerates atherosclerosis progression already in children and young adults. With regard to pathophysiological changes in the vasculature, the striking similarities between physiological changes related to aging and obesity-related abnormalities are compatible with the concept that obesity causes “premature” vascular aging. This article reviews factors underlying the accelerated vascular disease development due to obesity. It also highlights the importance of recognizing childhood obesity as a disease condition and its permissive role in aggravating the development of other diseases. The importance of childhood obesity for disease susceptibility later in life, and the need for prevention and treatment are also discussed.
Keywords: atherosclerosis, non-alcoholic steatohepatitis, diabetes, insulin resistance, stroke, myocardial infarction, physical exercise, cardiovascular risk, hypertension, vascular programming
Childhood obesity: a health problem gone global
Childhood obesity has been of medical interest for more than 150 years1, 2. Until the middle of the 20th century the prevalence of obesity in the general population of the United States was relatively moderate3. However, in the last two decades the prevalence has risen to epidemic proportions4, 5, 6. In fact, 34.4 percent of the population of the United States are now considered overweight (and not obese) and 33.9 percent are considered to be obese7, affecting more than 200 million people. Similarly, the number of children diagnosed with obesity and/or obesity-related diabetes has been continuously increasing over the past 20 years in countries around the world8, 9, 10. In 2010 in the United States, 17 percent of children and adolescents were obese – including those with severe obesity11, with the prevalence of obesity having tripled since 19803. Particularly worrisome is the 10.4% prevalence of obesity among the 2 to 5 year olds in the US12, with other parts of the world catching up13, 14. The World Health Organization (WHO) defines obesity (in adults: BMI >30 kg/m2) as a disease for which excessive calorie intake, in conjunction with lack of physical exercise, have been identified as major predisposing and aggravating factors15, 16. Obesity also serves as soil for the development of other diseases15, particularly insulin resistance (pre-diabetes), type 2 diabetes mellitus, arterial hypertension, dyslipidemia/hypertriglyceridemia, and fatty liver disease/non-alcoholic steatohepatitis (NASH)15, 17, 18. At the same time, obesity also worsens these conditions once they have developed15. In addition, mutations in certain genes such as the leptin receptor are associated with early-onset childhood obesity and excessive body mass indices19, 20, 21. High birth weights or diabetes of the mother (pregnancy-associated diabetes) have been proposed as potential factors affecting postnatal health, and lack of breastfeeding has been suggested to contribute to a higher risk for obesity during adolescence22. A number of other factors have been associated with a higher risk to develop obesity, which include the disease susceptibility of certain ethnic groups, poverty and/or low socioeconomic status, which are often associated with a low health concerns/self-concern3, 7. By contrast, some Asian countries such as Japan which have a very low overall prevalence of obesity23. This may be in part due to composition of Asian diets, while excess access to inexpensive, high calorie food has been identified as a major factor contributing to the rising number of obese children in countries such as the USA and in European countries24. Not surprisingly, childhood obesity has also been steadily growing in China where over the past decades people have in part adopted Western dietary patterns24. Increased health risk is not limited to obesity, but already apparent with overweight. Indeed, long-term studies following the health of overweight children for more than 40 years found significantly increased risks for a number of diseases25 (Figure 1).
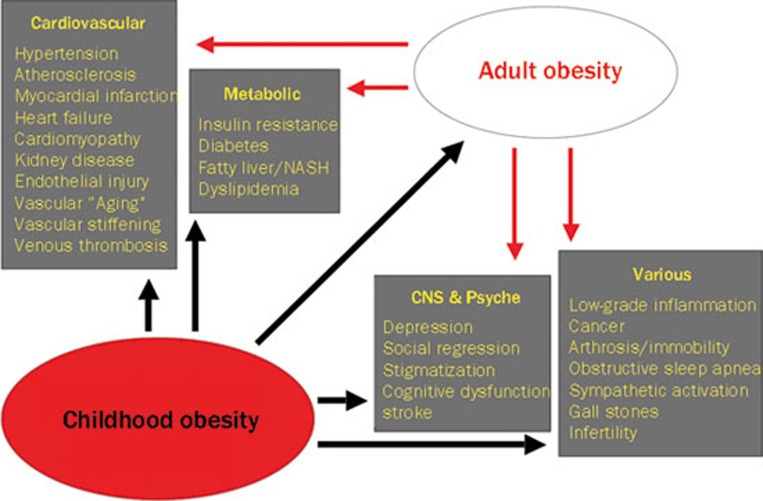
Figure 1.
Aggravating effect of childhood obesity on the life-time risk for other disease conditions, including a greater risk for adult obesity, which itself continues to worsen disease development.
Atherosclerosis begins in childhood
Obese children are at a higher risk for accelerated development of vascular disease26, which is aggravated by the worsening of risk factors secondary to obesity. Atherosclerosis, a systemic chronic inflammatory disease of the large arteries, is the main cause of cardiovascular and cerebrovascular events27. The disease accounts for the majority of deaths due to myocardial infarction and stroke in Western as well as in Eastern and developing countries27. First vascular abnormalities, inflammatory changes and plaque development can be observed in children already in the first year of life28; consistent with these observations, the disease process begins in utero, during which the precursor of the atherosclerotic plaque — the “fatty streak” — is already present29, 30. The development of fatty streaks, which represent inflammatory accumulations of macrophages in the subintimal space — is aggravated by maternal hypercholesterolemia and thus sets the basis for vascular disease later in life30. The cause of cardiovascular and cerebrovascular events most often is due to rupture of “soft” atherosclerotic plaques filled with a lipid core underlying a thinned fibrous cap27, pathological findings some of which are already present in young adults26, 31. Plaque development is accelerated in the presence of risk factors such as arterial hypertension, dyslipidemia, diabetes, male sex, and obesity, which are equally important for children and adults26, 31. Interestingly, girls and young women appear to be largely protected from the aggravating effect of obesity on plaque progression26. Among all cardiovascular risk factors, obesity is of particular importance since it aggravates several other risk factors such as arterial hypertension, insulin resistance/diabetes, or dyslipidemia.
Childhood obesity causes changes consistent with “Premature” vascular aging
Inflammation also plays a role for insulin resistance and metabolic changes associated with obesity32 and abnormal inflammatory activation has been reported to occur in obese children33. In both children and adults, obesity causes generalized injury to the vasculature. This process also involves inflammatory activation, both locally in the vascular wall32 as well as in adipose tissue34. Inflammation also underlies insulin resistance (pre-diabetes) and type 2 diabetes34, conditions originally believed to be restricted to elderly individuals, but now increasingly found in obese juveniles35, 36. Similarly, an important aspect of obesity-associated vascular injury obtained from preclinical and clinical studies, is that many of the vascular changes found in obesity are highly similar to those seen with aging37, which not only represents a physiological process but in itself represents a strong and independent risk factor for future cardiovascular events37. As with aging37, experimental or human obesity shows an attenuation of endothelium-dependent vasodilation38, 39, a decrease in NO bioactivity38, 39 in conjunction with NO synthase uncoupling37, an increase in prostanoid-mediated endothelium-dependent contractions40, 41, 42, telomere shortening43, 44, 45, 46, increased vascular stiffness47, and increased arterial intima-media thickness26, 48. Obesity also increases tissue levels of endothelin-138, 49, 50, a strong vasoconstrictor peptide and atherogenic growth factor and proinflammatory stimulus51. Picard and Guarente recently reported interactions between life-span regulating genes and adipose tissue functions52. Thus, obesity can be considered a process which is compatible with accelerated aging which may — at least in part — explain the accelerated atherosclerosis development in children and young adults with obesity26.
Potential role for post-natal dietary vascular programming
A few years ago results from two clinical studies were reported that childhood obesity is associated with a several fold increased risk for cardiovascular events in adult life, even if body weight had meanwhile normalized9, 53, 54. These very intriguing observations, which are in part supported by an earlier study55, not only emphasize the importance of childhood obesity prevention but also suggest that still unknown mechanisms exist that must be set-off by the “childhood obesity environment” and, once activated, remain irreversibly active until later in life irrespective of changes in body weight. Thus, possible local “post-natal dietary programming” mechanisms may contribute to the underlying disease-promoting process in the arterial wall. Alternatively, acceletated progression of atherosclerosis in youth due to obesity may simply lead to established, irreversible atherosclerotic lesions that no longer can be affected by weight normalization. Indeed, advanced coronary artery disease present in their late teenage years and death from myocardial infarction has been described in young men exposed to extremely high stress conditions56, 57.
Continued need for disease prevention
Aside from highly complex disease processes, simple factors such as overnutrition and lack of knowledge about obesity prevention, respectively, are likely to be at least equally important. This can be exemplified by a case report from Germany where parents fed their infant almost exclusively with sugared water58. This infant developed severe obesity and at 2 years of age, was diagnosed with early cerebrovascular disease58 similar to increased vascular stiffening found in obese juveniles59, conditions normally found only at much later stages in life. Not surprisingly, reducing body weight in obese juveniles is associated with markedly improved cognitive function60, and recent data suggest that even cerebral and cerebellar development is negatively affected by childhood obesity61. Thus, awareness and education of parents12, educators, and pediatric medical staff should remain one of the key goals in order to achieve prevention of childhood obesity which, subsequently, should also result in a reduction of diseases associated with it. One of the questions is how we can monitor vascular health. The function of the vasculature, particularly endothelium-dependent vasomotion, reflects quite well the overall health status of the arterial system62. Human obesity, characterized by accumulation of ectopic (particularly visceral) fat63, is associated with abnormal endothelium-dependent vasomotion and enhanced contractility to endothelin-164, 65. Accordingly, a reduction in energy intake66 or reduction in body weight67 improves vascular function in obese patients. In human resistance arteries obesity is associated with vascular hypertrophy as indicated by an increased media-to-lumen ratio68, and a recent important study demonstrated that functional vascular abnormalities observed in obese individuals can be largely normalized by lowering body weight by reducing intra-abdominal fat mass in adults67. Thus, any reduction of obesity — in children as well as adults — is likely to translate into improved overall health and survival4, 15, 69. Indeed, preserved endothelium-dependent vasoreactivity is associated with greater survival in patients with cardiovascular disease62. Possibly, reducing subcutaneous fat may also have some beneficial effect on the pro-inflammatory risk profile70, 71.
Physical activity as therapeutic
The question remains of how to achieve a sustained reduction of childhood obesity, both at the individual level as well as for overall prevalence72. One of the central components of obesity prevention and therapy or – if absent a promotor of obesity — is physical exercise4, 73, 74, 75. Physical inactivity is a key cause contributing to and worsening childhood obesity76, and has now even become a concern in developing countries77. Exercise not only has a number of beneficial effects on several risk factors associated with obesity (reduction of sympathetic activation and blood pressure, improved lipid profile, improved insulin sensitivity4, 73, 74, 75), but also improves consumption of excess energy stores of fat and thus helps to reduce adipose tissue mass78. There is recent evidence that regular exercise may even infer with cellular processes associated with vascular aging79. A most recent study indicates that vascular elasticity as a function of age is also increased in obese children compared with their lean counterparts80, indicative of accelerated vascular growth and maturation and thus compatible with early aging. It is important, both for therapy and prevention of childhood obesity, that sufficient and regular exercise becomes and remains a part of children's everyday life in conjunction with normal calorie intake. It has been recently shown that weight loss in children reduces inflammatory activation81, one of the key factors for vascular disease progression82. Caloric restriction prolongs life in a number of species, including rodents and primates83, 84. It can only be speculated that in humans “global caloric restriction” in those countries with excess access to food would have similar effects on life expectancy and overall well-being5. Indeed some countries have taken political measures such as issuing special taxes on fat as the dietary componant with highest energy value85, 86. The prevention of childhood obesity is a chance that must be taken early in life by parents, health professionals, educators, and politicians69. Fortunately, health agencies have already begun to implement this need into their information policies provided to parents12 with whom children spend the most time. If we succeed with this task of promoting, achieving, and maintaining health among children — including a regular “regimen” of physical exercise16, 87, 88 —, this will ultimately reduce the number of tomorrow's patients and enable healthy aging at a low cardiovascular risk89.
Acknowledgments
The project was supported by the Swiss National Science Foundation (Projects Nr 108 258 and Nr 122 504).
References
- Don WG. Remarkable case of obesity in a hindoo boy aged twelve years. Lancet. 1859;73:363. [Google Scholar]
- Ellis RW, Tallermann KM. Obesity in childhood: A study of fifty cases. Lancet. 1934;ii:615–20. [Google Scholar]
- http://www.cdc.gov/obesity/data/trends.html (accessed Dec 1, 2011
- Barton M, Furrer J. Cardiovascular consequences of the obesity pandemic: need for action. Expert Opin Investig Drugs. 2003;12:1757–9. doi: 10.1517/13543784.12.11.1757. [DOI] [PubMed] [Google Scholar]
- Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352:1138–45. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- Stewart ST, Cutler DM, Rosen AB. Forecasting the effects of obesity and smoking on U.S. life expectancy. N Engl J Med. 2009;361:2252–60. doi: 10.1056/NEJMsa0900459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- http://www.cdc.gov/obesity/data/index.html (accessed Dec 1, 2011
- Yanovski JA. Pediatric obesity. Rev Endocr Metab Disord. 2001;2:371–83. doi: 10.1023/a:1011800532068. [DOI] [PubMed] [Google Scholar]
- Ludwig DS. Childhood obesity — the shape of things to come. N Engl J Med. 2007;357:2325–7. doi: 10.1056/NEJMp0706538. [DOI] [PubMed] [Google Scholar]
- Wright C. A US epidemic: childhood obesity. J Physician Assist Educ. 2011;21:39–41. doi: 10.1097/01367895-201021020-00008. [DOI] [PubMed] [Google Scholar]
- Skelton JA, Cook SR, Auinger P, Klein JD, Barlow SE. Prevalence and trends of severe obesity among US children and adolescents. Acad Pediatr. 2009;9:322–9. doi: 10.1016/j.acap.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- http://www.cdc.gov/healthyweight/children/index.html (accessed December 1, 2011
- Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. Obes Rev. 2004;5:4–104. doi: 10.1111/j.1467-789X.2004.00133.x. [DOI] [PubMed] [Google Scholar]
- Lobstein T. The prevention of obesity in children. Pediatr Endocrinol Rev. 2004;1:471–5. [PubMed] [Google Scholar]
- Daniels SR, Pratt CA, Hayman LL. Reduction of risk for cardiovascular disease in children and adolescents. Circulation. 2011;124:1673–86. doi: 10.1161/CIRCULATIONAHA.110.016170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadeau KJ, Maahs DM, Daniels SR, Eckel RH. Childhood obesity and cardiovascular disease: links and prevention strategies. Nat Rev Cardiol. 2011;8:513–25. doi: 10.1038/nrcardio.2011.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schattenberg JM, Schuppan D. Nonalcoholic steatohepatitis: the therapeutic challenge of a global epidemic. Curr Opin Lipidol. 2010;22:479–88. doi: 10.1097/MOL.0b013e32834c7cfc. [DOI] [PubMed] [Google Scholar]
- Ahmed MH, Abu EO, Byrne CD. Non-alcoholic fatty liver disease (NAFLD): new challenge for general practitioners and important burden for health authorities. Prim Care Diabetes. 2010;4:129–37. doi: 10.1016/j.pcd.2010.02.004. [DOI] [PubMed] [Google Scholar]
- O'Rahilly S. Human obesity and insulin resistance: Lessons from human genetics. Clin Biochem. 2011;44:451. [Google Scholar]
- O'Rahilly S. Human genetics illuminates the paths to metabolic disease. Nature. 2009;462:307–14. doi: 10.1038/nature08532. [DOI] [PubMed] [Google Scholar]
- O'Rahilly S, Farooqi IS. Human obesity as a heritable disorder of the central control of energy balance. Int J Obes (Lond) 2008;32:S55–61. doi: 10.1038/ijo.2008.239. [DOI] [PubMed] [Google Scholar]
- Gillman MW, Rifas-Shiman SL, Camargo CA Jr, Berkey CS, Frazier AL, Rockett HR, et al. Risk of overweight among adolescents who were breast fed as infants. JAMA. 2001;285:2461–7. doi: 10.1001/jama.285.19.2461. [DOI] [PubMed] [Google Scholar]
- Fujita T. The metabolic syndrome in Japan. Nat Clin Pract Cardiovasc Med. 2008;5:S15–8. doi: 10.1038/ncpcardio0808. [DOI] [PubMed] [Google Scholar]
- McLellan F. Obesity rising to alarming levels around the world. Lancet. 2002;359:1412. doi: 10.1016/S0140-6736(02)08397-6. [DOI] [PubMed] [Google Scholar]
- Mossberg HO. 40-Year follow-up of overweight children. Lancet. 1989;334:491–3. doi: 10.1016/s0140-6736(89)92098-9. [DOI] [PubMed] [Google Scholar]
- McGill HC Jr, McMahan CA, Herderick EE, Zieske AW, Malcom GT, Tracy RE, et al. Obesity accelerates the progression of coronary atherosclerosis in young men. Circulation. 2002;105:2712–8. doi: 10.1161/01.cir.0000018121.67607.ce. [DOI] [PubMed] [Google Scholar]
- Libby P. Atherosclerosis: the new view. Sci Am. 2002;286:46–55. doi: 10.1038/scientificamerican0502-46. [DOI] [PubMed] [Google Scholar]
- Zinserling WD. Untersuchungen über Atherosklerose. 1. Über die Aortaverfettungen bei Kindern. Virchows Arch f Path Anat. 1925;255:677–705. [Google Scholar]
- Napoli C, D'Armiento FP, Mancini FP, Postiglione A, Witztum JL, Palumbo G, et al. Fatty streak formation occurs in human fetal aortas and is greatly enhanced by maternal hypercholesterolemia. Intimal accumulation of low density lipoprotein and its oxidation precede monocyte recruitment into early atherosclerotic lesions. J Clin Invest. 1997;100:2680–90. doi: 10.1172/JCI119813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napoli C, Glass CK, Witztum JL, Deutsch R, D'Armiento FP, Palinski W. Influence of maternal hypercholesterolaemia during pregnancy on progression of early atherosclerotic lesions in childhood: Fate of Early Lesions in Children (FELIC) study. Lancet. 1999;354:1234–41. doi: 10.1016/S0140-6736(99)02131-5. [DOI] [PubMed] [Google Scholar]
- McGill HC Jr, McMahan CA, Zieske AW, Sloop GD, Walcott JV, Troxclair DA, et al. Associations of coronary heart disease risk factors with the intermediate lesion of atherosclerosis in youth. The Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Research Group. Arterioscler Thromb Vasc Biol. 2000;20:1998–2004. doi: 10.1161/01.atv.20.8.1998. [DOI] [PubMed] [Google Scholar]
- Greenstein AS, Khavandi K, Withers SB, Sonoyama K, Clancy O, Jeziorska M, et al. Local inflammation and hypoxia abolish the protective anticontractile properties of perivascular fat in obese patients. Circulation. 2009;119:1661–70. doi: 10.1161/CIRCULATIONAHA.108.821181. [DOI] [PubMed] [Google Scholar]
- Kapiotis S, Holzer G, Schaller G, Haumer M, Widhalm H, Weghuber D, et al. A proinflammatory state is detectable in obese children and is accompanied by functional and morphological vascular changes. Arterioscler Thromb Vasc Biol. 2006;26:2541–6. doi: 10.1161/01.ATV.0000245795.08139.70. [DOI] [PubMed] [Google Scholar]
- Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest. 2003;112:1821–30. doi: 10.1172/JCI19451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, Fisch G, Teague B, Tamborlane WV, Banyas B, Allen K, et al. Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N Engl J Med. 2002;346:802–10. doi: 10.1056/NEJMoa012578. [DOI] [PubMed] [Google Scholar]
- Rocchini AP. Childhood obesity and a diabetes epidemic. N Engl J Med. 2002;346:854–5. doi: 10.1056/NEJM200203143461112. [DOI] [PubMed] [Google Scholar]
- Barton M. Obesity and aging: determinants of endothelial cell dysfunction and atherosclerosis. Pflugers Arch. 2010;460:825–37. doi: 10.1007/s00424-010-0860-y. [DOI] [PubMed] [Google Scholar]
- Damjanovic M, Barton M. Fat intake and cardiovascular response. Curr Hypertens Rep. 2008;10:25–31. doi: 10.1007/s11906-008-0007-0. [DOI] [PubMed] [Google Scholar]
- Naderali EK, Brown MJ, Pickavance LC, Wilding JP, Doyle PJ, Williams G. Dietary obesity in the rat induces endothelial dysfunction without causing insulin resistance: a possible role for triacylglycerols. Clin Sci (Lond) 2001;101:499–506. doi: 10.1042/cs1010499. [DOI] [PubMed] [Google Scholar]
- Traupe T, Lang M, Goettsch W, Munter K, Morawietz H, Vetter W, et al. Obesity increases prostanoid-mediated vasoconstriction and vascular thromboxane receptor gene expression. J Hypertens. 2002;20:2239–45. doi: 10.1097/00004872-200211000-00024. [DOI] [PubMed] [Google Scholar]
- Traupe T, D'Uscio L, Muenter K, Morawietz H, Vetter W, Barton M. Effects of obesity on endothelium-dependent reactivity during acute nitric oxide synthase inhibition: modulatory role of endothelin. Clin Sci (Lond) 2002;103:13S–5S. doi: 10.1042/CS103S013S. [DOI] [PubMed] [Google Scholar]
- Bhattacharya I, Damjanovic M, Gut A, Hager S, Perez-Dominguez A, Minotti R, et al. Childhood obesity induced by a high-fat diet causes premature vascular aging involving endothelium-dependent mechanisms. Hypertension. 2008;52:e89. [Google Scholar]
- Buxton JL, Walters RG, Visvikis-Siest S, Meyre D, Froguel P, Blakemore AI. Childhood obesity is associated with shorter leukocyte telomere length. J Clin Endocrinol Metab. 2011;96:1500–5. doi: 10.1210/jc.2010-2924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niemann B, Chen Y, Teschner M, Li L, Silber RE, Rohrbach S. Obesity induces signs of premature cardiac aging in younger patients: the role of mitochondria. J Am Coll Cardiol. 2011;57:577–85. doi: 10.1016/j.jacc.2010.09.040. [DOI] [PubMed] [Google Scholar]
- Lee M, Martin H, Firpo MA, Demerath EW. Inverse association between adiposity and telomere length: The Fels Longitudinal Study. Am J Hum Biol. 2011;23:100–6. doi: 10.1002/ajhb.21109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz VA, Mainous AG, Player MS, Everett CJ. Telomere length and adiposity in a racially diverse sample. Int J Obes (Lond) 2010;34:261–5. doi: 10.1038/ijo.2009.198. [DOI] [PubMed] [Google Scholar]
- Tounian P, Aggoun Y, Dubern B, Varille V, Guy-Grand B, Sidi D, et al. Presence of increased stiffness of the common carotid artery and endothelial dysfunction in severely obese children: a prospective study. Lancet. 2001;358:1400–4. doi: 10.1016/S0140-6736(01)06525-4. [DOI] [PubMed] [Google Scholar]
- Woo KS, Chook P, Yu CW, Sung RY, Qiao M, Leung SS, et al. Overweight in children is associated with arterial endothelial dysfunction and intima-media thickening. Int J Obes Relat Metab Disord. 2004;28:852–7. doi: 10.1038/sj.ijo.0802539. [DOI] [PubMed] [Google Scholar]
- Barton M, Carmona R, Morawietz H, d'Uscio LV, Goettsch W, Hillen H, et al. Obesity is associated with tissue-specific activation of renal angiotensin-converting enzyme in vivo: evidence for a regulatory role of endothelin. Hypertension. 2000;35:329–36. doi: 10.1161/01.hyp.35.1.329. [DOI] [PubMed] [Google Scholar]
- Barton M, Carmona R, Ortmann J, Krieger JE, Traupe T. Obesity-associated activation of angiotensin and endothelin in the cardiovascular system. Int J Biochem Cell Biol. 2003;35:826–37. doi: 10.1016/s1357-2725(02)00307-2. [DOI] [PubMed] [Google Scholar]
- Barton M, Yanagisawa M. Endothelin: 20 years from discovery to therapy. Can J Physiol Pharmacol. 2008;86:485–98. doi: 10.1139/Y08-059. [DOI] [PubMed] [Google Scholar]
- Picard F, Guarente L. Molecular links between aging and adipose tissue. Int J Obes Relat Metab Disord. 2005;29:S36–9. doi: 10.1038/sj.ijo.0802912. [DOI] [PubMed] [Google Scholar]
- Bibbins-Domingo K, Coxson P, Pletcher MJ, Lightwood J, Goldman L. Adolescent overweight and future adult coronary heart disease. N Engl J Med. 2007;357:2371–9. doi: 10.1056/NEJMsa073166. [DOI] [PubMed] [Google Scholar]
- Baker JL, Olsen LW, Sorensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007;357:2329–37. doi: 10.1056/NEJMoa072515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell DJ, Frankel SJ, Nanchahal K, Peters TJ, Davey Smith G. Childhood obesity and adult cardiovascular mortality: a 57-y follow-up study based on the Boyd Orr cohort. Am J Clin Nutr. 1998;67:1111–8. doi: 10.1093/ajcn/67.6.1111. [DOI] [PubMed] [Google Scholar]
- Enos WF, Beyer JC, Holmes R. Pathogenesis of the coronary disease in the American soldiers killed in Korea. JAMA. 1955;158:912–5. doi: 10.1001/jama.1955.02960110018005. [DOI] [PubMed] [Google Scholar]
- McNamara J, Molot M, Stremple J, Cutting R. Coronary artery disease in combat casualities in Vietnam. JAMA. 1971;216:1185–7. [PubMed] [Google Scholar]
- Weghuber D, Zaknun D, Nasel C, Willforth-Ehringer A, Muller T, Boriss-Riedl M, et al. Early cerebrovascular disease in a 2-year-old with extreme obesity and complete metabolic syndrome due to feeding of excessively high amounts of energy. Eur J Pediatr. 2007;166:37–41. doi: 10.1007/s00431-006-0204-2. [DOI] [PubMed] [Google Scholar]
- Gungor N, Thompson T, Sutton-Tyrrell K, Janosky J, Arslanian S. Early signs of cardiovascular disease in youth with obesity and type 2 diabetes. Diabetes Care. 2005;28:1219–21. doi: 10.2337/diacare.28.5.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barton SB, Walker LL, Lambert G, Gately PJ, Hill AJ. Cognitive change in obese adolescents losing weight. Obes Res. 2004;12:313–9. doi: 10.1038/oby.2004.39. [DOI] [PubMed] [Google Scholar]
- Miller JL, Couch J, Schwenk K, Long M, Towler S, Theriaque DW, et al. Early childhood obesity is associated with compromised cerebellar development. Dev Neuropsychol. 2009;34:272–83. doi: 10.1080/87565640802530961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrmann J, Lerman A. The endothelium — the cardiovascular health barometer. Herz. 2008;33:343–53. doi: 10.1007/s00059-008-3088-2. [DOI] [PubMed] [Google Scholar]
- Britton KA, Fox CS. Ectopic fat depots and cardiovascular disease. Circulation. 2011;124:e837–41. doi: 10.1161/CIRCULATIONAHA.111.077602. [DOI] [PubMed] [Google Scholar]
- Cardillo C, Campia U, Iantorno M, Panza JA. Enhanced vascular activity of endogenous endothelin-1 in obese hypertensive patients. Hypertension. 2004;43:36–40. doi: 10.1161/01.HYP.0000103868.45064.81. [DOI] [PubMed] [Google Scholar]
- Georgescu A, Popov D, Constantin A, Nemecz M, Alexandru N, Cochior D, et al. Dysfunction of human subcutaneous fat arterioles in obesity alone or obesity associated with type 2 diabetes. Clin Sci (Lond) 2011;120:463–72. doi: 10.1042/CS20100355. [DOI] [PubMed] [Google Scholar]
- Dessi-Fulgheri P, Sarzani R, Serenelli M, Tamburrini P, Spagnolo D, Giantomassi L, et al. Low calorie diet enhances renal, hemodynamic, and humoral effects of exogenous atrial natriuretic peptide in obese hypertensives. Hypertension. 1999;33:658–62. doi: 10.1161/01.hyp.33.2.658. [DOI] [PubMed] [Google Scholar]
- De Ciuceis C, Porteri E, Rizzoni D, Corbellini C, La Boria E, Boari GE, et al. Effects of weight loss on structural and functional alterations of subcutaneous small arteries in obese patients. Hypertension. 2011;58:29–36. doi: 10.1161/HYPERTENSIONAHA.111.171082. [DOI] [PubMed] [Google Scholar]
- Rizzoni D, De Ciuceis C, Porteri E, Semeraro F, Rosei EA. Structural alterations in small resistance arteries in obesity. Basic Clin Pharmacol Toxicol. 2012;110:56–62. doi: 10.1111/j.1742-7843.2011.00786.x. [DOI] [PubMed] [Google Scholar]
- Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]
- Hamdy O, Porramatikul S, Al-Ozairi E. Metabolic obesity: the paradox between visceral and subcutaneous fat. Curr Diabetes Rev. 2006;2:367–73. doi: 10.2174/1573399810602040367. [DOI] [PubMed] [Google Scholar]
- Marfella R, Grella R, Rizzo MR, Barbieri M, Ferraraccio F, Cacciapuoti F, et al. Role of subcutaneous abdominal fat on cardiac function and proinflammatory cytokines in premenopausal obese women. Ann Plast Surg. 2009;63:490–5. doi: 10.1097/SAP.0b013e3181955cdb. [DOI] [PubMed] [Google Scholar]
- Wieting JM. Cause and effect in childhood obesity: solutions for a national epidemic. J Am Osteopath Assoc. 2008;108:545–52. [PubMed] [Google Scholar]
- Scheen AJ. Current management strategies for coexisting diabetes mellitus and obesity. Drugs. 2003;63:1165–84. doi: 10.2165/00003495-200363120-00001. [DOI] [PubMed] [Google Scholar]
- Carroll JF, Kyser CK. Exercise training in obesity lowers blood pressure independent of weight change. Med Sci Sports Exerc. 2002;34:596–601. doi: 10.1097/00005768-200204000-00006. [DOI] [PubMed] [Google Scholar]
- Kiess W, Reich A, Muller G, Galler A, Kapellen T, Raile K, et al. Obesity in childhood and adolescence: clinical diagnosis and management. J Pediatr Endocrinol Metab. 2001;14:1431–40. [PubMed] [Google Scholar]
- Lazarou C, Soteriades ES. Children's physical activity, TV watching and obesity in Cyprus: the CYKIDS study. Eur J Public Health. 2010;20:70–7. doi: 10.1093/eurpub/ckp093. [DOI] [PubMed] [Google Scholar]
- Onywera VO. Childhood obesity and physical inactivity threat in Africa: strategies for a healthy future. Glob Health Promot. 2011;17:45–6. doi: 10.1177/1757975910363937. [DOI] [PubMed] [Google Scholar]
- Sothern MS. Obesity prevention in children: physical activity and nutrition. Nutrition. 2004;20:704–8. doi: 10.1016/j.nut.2004.04.007. [DOI] [PubMed] [Google Scholar]
- Werner C, Furster T, Widmann T, Poss J, Roggia C, Hanhoun M, et al. Physical exercise prevents cellular senescence in circulating leukocytes and in the vessel wall. Circulation. 2009;120:2438–47. doi: 10.1161/CIRCULATIONAHA.109.861005. [DOI] [PubMed] [Google Scholar]
- Tryggestad JB, Thompson DM, Copeland KC, Short KR. Obese children have higher arterial elasticity without a difference in endothelial function: the role of body composition. Obesity (Silver Spring) 2012;20:165–71. doi: 10.1038/oby.2011.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hoorenbeeck K, Franckx H, Debode P, Aerts P, Wouters K, Ramet J, et al. Weight loss and sleep-disordered breathing in childhood obesity: effects on inflammation and uric acid. Obesity (Silver Spring) 2012;20:172–7. doi: 10.1038/oby.2011.282. [DOI] [PubMed] [Google Scholar]
- Barton M, Minotti R, Haas E. Inflammation and atherosclerosis. Circ Res. 2007;101:750–1. doi: 10.1161/CIRCRESAHA.107.162487. [DOI] [PubMed] [Google Scholar]
- Goto S, Takahashi R, Araki S, Nakamoto H. Dietary restriction initiated in late adulthood can reverse age-related alterations of protein and protein metabolism. Ann N Y Acad Sci. 2002;959:50–6. doi: 10.1111/j.1749-6632.2002.tb02082.x. [DOI] [PubMed] [Google Scholar]
- Colman RJ, Anderson RM, Johnson SC, Kastman EK, Kosmatka KJ, Beasley TM, et al. Caloric restriction delays disease onset and mortality in rhesus monkeys. Science. 2009;325:201–4. doi: 10.1126/science.1173635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkins R. Danes impose 25% tax increases on ice cream, chocolate, and sweets to curb disease. BMJ. 2010;341:c3592. doi: 10.1136/bmj.c3592. [DOI] [PubMed] [Google Scholar]
- Alemanno A, Carreno I. Fat taxes in the EU between fiscal austerity and the fight against obesity. Eur J Risk Regul. 2011;4:571–6. [Google Scholar]
- Daniels SR, Pratt CA, Hayman LL. Recent advances in preventive cardiology and lifestyle medicine. Reduction of risk for cardiovascular disease in children and adolescents. Circulation. 2011;124:1673–86. doi: 10.1161/CIRCULATIONAHA.110.016170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutin B. Diet vs exercise for the prevention of pediatric obesity: the role of exercise. Int J Obes (Lond) 2011;35:29–32. doi: 10.1038/ijo.2010.140. [DOI] [PubMed] [Google Scholar]
- Barton M. Aging and biomedicine 2005: where should we go from here. Cardiovasc Res. 2005;66:187–9. doi: 10.1016/j.cardiores.2005.03.003. [DOI] [PubMed] [Google Scholar]