Abstract
Aims/Objectives
Insulin clearance may decline as an early compensatory mechanism to deteriorating insulin sensitivity. However, no previous studies have investigated the association of subclinical inflammation or impaired fibrinolysis with insulin clearance. We examined the association between plasminogen activator inhibitor (PAI)-1, C-reactive protein (CRP), tumor necrosis factor (TNF)-α, leptin and fibrinogen and the progression of metabolic clearance rate of insulin (MCRI) over time.
Methods
We studied 784 non-diabetic Caucasians, Hispanics and African-Americans in the Insulin Resistance Atherosclerosis Study (IRAS). Insulin sensitivity (SI), acute insulin response (AIR) and MCRI were determined from frequently sampled intravenous glucose tolerance tests at baseline and at 5-year follow-up. Inflammatory and fibrinolytic proteins were measured in fasting plasma at baseline.
Results
MCRI declined significantly by 29% in 5-year follow-up. We observed a significant association between higher plasma PAI-1 and the decline in MCRI in multivariable-adjusted regression models (β= −0.045 [−0.081, −0.0091]). Higher plasma CRP and leptin were associated with a decline in MCRI in unadjusted models, however, these associations were non-significant after adjusting for body mass index and waist circumference (β= −0.016 [−0.041, 0.0083] for CRP, β= −0.044 [−0.10, 0.011] for leptin). Higher plasma TNF-α was associated with a decline in MCRI in unadjusted (β= −0.071 [−0.14, −0.00087]), but not in multivariable-adjusted (β= −0.056 [−0.13, 0.017]) models. Plasma fibrinogen was not associated with the change in MCRI.
Conclusions/Interpretation
We identified that higher plasma PAI-1 (but not CRP, TNF-α, leptin or fibrinogen) independently predicts the progressive decline of insulin clearance in the multi-ethnic cohort of the IRAS.
Keywords: C-reactive protein, fibrinogen, leptin, metabolic clearance of insulin, plasminogen activator inhibitor-1, tumor necrosis factor-α
Introduction
Insulin resistance and beta-cell dysfunction have long been recognised as critical pathophysiological disorders underlying type 2 diabetes. Risk factors for these important metabolic traits have also been extensively researched [1–2]. Insulin clearance is an integrated part of the metabolism of insulin, and reduced insulin clearance serves as an adaptive mechanism in response to insulin resistance to preserve beta-cell function in pre-diabetes states [3]. However, the determinants of reduced insulin clearance have not been well-studied.
It is well-established that type 2 diabetes is associated with low-grade inflammation which involves a cytokine-mediated acute-phase response and other inflammatory processes related to obesity [4]. In addition, impaired fibrinolysis has been linked to type 2 diabetes [5]. Previous prospective studies have demonstrated that inflammatory and fibrinolytic proteins predict incident diabetes [6–8]. Insulin secretion, sensitivity and clearance are closely related physiological processes. Subclinical inflammation and impaired fibrinolysis may act through insulin resistance [9–11] and possibly beta-cell dysfunction to impact on insulin clearance, hence increasing the risk of diabetes.
To our knowledge, no studies have investigated the association of subclinical inflammation and impaired fibrinolysis with insulin clearance. Exploring these relationships is crucial to gain insight into potential pathophysiological mechanisms for the development of diabetes. Therefore, we aimed to examine the association between inflammatory and fibrinolytic proteins at baseline, including plasminogen activator inhibitor (PAI)-1, C-reactive protein (CRP), tumor necrosis factor (TNF)-α, leptin and fibrinogen, and the change in metabolic clearance rate of insulin (MCRI) at 5-year follow-up in the Insulin Resistance Atherosclerosis Study (IRAS).
Research designs and methods
Study population
The study population comprised participants in the IRAS, a multicenter epidemiological study designed to investigate the relationships between insulin resistance, atherosclerosis and its known risk factors among non-Hispanic whites, Hispanics and African-Americans. Between October 1992 and April 1994, the IRAS recruited 1,625 participants from four clinical centres located in San Antonio, TX, San Luis Valley, CO, Oakland, CA and Los Angeles, CA. The recruitment strategy aimed to identify sufficient numbers of participants in each ethnic, age, sex and glucose tolerance group to allow for comparison between and within these groups. Although the IRAS investigators purposely over-sampled individuals with impaired glucose tolerance, 44% of the study population had normal glucose tolerance at baseline. In addition, the fasting blood glucose levels in the IRAS were comparable to those in the second National Health and Nutrition Examination Survey (NHANES II) in participants with normal or impaired glucose tolerance [12]. The institutional review boards at each site approved the study protocol and all participants provided written informed consent. The current analysis included 784 non-diabetic participants who attended both baseline and follow-up examinations. Participants with prevalent diabetes at baseline (n=573) and missing data on MCRI on either examination (n=268) were excluded from the study. Among the 268 participants without MCRI data, 163 of them did not attend follow-up examinations. MCRI was not determined at baseline or follow-up examinations in the remaining 105 participants due to technical issues. The characteristics of these 268 participants at baseline were similar to those with data on MCRI in term of age, sex, ethnicity, BMI and glucose tolerance status.
Clinical measurements and procedures
The IRAS protocol required two visits, one week apart. Both baseline and follow-up examinations were conducted in the morning using identical procedures. Participants were asked before each visit to fast for 12 hours, to abstain from alcohol and heavy exercise for 24 hours, and to abstain from smoking the morning of the examination. The duration of fasting was recorded and confirmed by asking “What time and date did you last eat and/or drink anything other than water, including candy and chewing gum?” No participants were excluded from the study because they did not fast properly.
During the first visit, a 75-gram oral glucose tolerance test was administered. During the second visit, insulin sensitivity (SI), acute insulin response (AIR) and MCRI were determined from a frequently sampled intravenous glucose tolerance test (FSIGTT), with two modifications to the original protocol [13]. First, insulin, instead of tolbutamide, was injected to ensure adequate levels of plasma insulin to calculate insulin sensitivity accurately across a broad range of glucose tolerance [14]. Second, a reduced sampling protocol, using 12 instead of 30 samples, was followed for pragmatic reasons [15]. Insulin resistance, expressed as SI, was calculated using minimal model analysis. Insulin secretion was measured by AIR defined as the average increase in plasma insulin at time points 2 and 4 minutes after infusing glucose [16]. MCRI was calculated as the ratio of the insulin dose over the incremental area under the curve of insulin from 20 minutes to infinity [17] using the following equation:
where Dose represents the amount of insulin injected at 20 min, Ins(t) the plasma insulin concentration in standard units (μU/ml) at each FSIGTT sampling point and Ins(0) the fasting plasma insulin concentration determined before injecting glucose in the FSIGTT.
Anthropometric measurements (height, weight, waist circumference) and resting blood pressure were performed. Body mass index (BMI) was calculated as weight in kg divided by height in m2. All measurements were taken in duplicate following standardised procedures and the averages of these measurements were used in the analyses. Participants provided information on demographics (age, sex, ethnicity), lifestyle factors (smoking, alcohol consumption, energy expenditure) and family history of diabetes in validated questionnaires by self-report [12].
Biochemical analysis
Participants provided a fasting blood draw at each examination. Plasma glucose was measured using the glucose oxidase technique on an auto-analyser. Plasma samples which were used for the measurement of inflammatory and fibrinolytic proteins were prepared, frozen and stored at −70°C at the study centres within 90 minutes of the blood draw. Frozen samples were shipped on a monthly basis to the Laboratory for Clinical Biochemistry Research at the University of Vermont for measurements [6]. PAI-1 was determined in citrated plasma using a two-site immunoassay that is sensitive to free PAI-1, but not to PAI-1 complexed with t-PA, with a coefficient of variation (CV) of 14.0% [18]. Plasma CRP was measured by an in-house ultrasensitive competitive immunoassay, with an inter-assay CV of 8.9% [19]. Following the original method of Clauss [20], fibrinogen was measured in citrated plasma with a modified clot-rate assay using the Diagnostica STAGO ST4 instrument, with a CV of 3.0% [21]. Plasma leptin was measured using a radioimmunoassay, with an inter-assay CV of 7.0% [22]. TNF-α was measured in citrated plasma using a Quantikine HS Human TNF-α immunoassay (R&D Systems, Minneapolis, MN) [23]. Plasma lipids and lipoproteins, including triacylglycerol (TG) and high-density-lipoprotein (HDL)-cholesterol were determined using methods from the Lipid Research Clinics [24]. Alanine transaminase (ALT) was determined by enzymatic colorimetric assays [25].
Statistical analysis
We summarised the characteristics of participants stratified by thirds of the MCRI distribution at baseline, using median and interquartile range for continuous variables and percentages for categorical variables. We used analysis of variance, Kruskal-Wallis tests and Chi-squared tests to test whether continuous and categorical variables differed across the distribution of MCRI.
Since the distribution of PAI-1, CRP, TNF-α, SI, AIR and MCRI (at baseline and at follow-up) were skewed, we natural log-transformed them for normality. Because of the presence of 0 values for SI in the data, we added a constant of 1 to all values before the log-transformation. We used unadjusted and multivariable linear regression to explore the association between PAI-1, CRP, TNF-α, leptin and fibrinogen at baseline as continuous exposures, and the change in MCRI between two examinations as continuous outcomes. In regression models, we modeled MCRI at follow-up as the continuous outcome, and adjusted for MCRI at baseline simultaneously to determine the estimates for the change in MCRI between two examinations. We presented the regression coefficients (β) with their 95% confidence intervals (CI).
We included covariates in multivariable models if they were associated with both the exposure and the outcome, or if they were of a priori clinical relevance. Potential confounders included age, sex, ethnicity, smoking, alcohol consumption, energy expenditure, family history of diabetes, BMI, waist circumference, HDL-cholesterol, TG, ALT, fasting blood glucose, SI and AIR. Multivariable-adjusted regression models were based on 784 participants with data on MCRI at baseline and at follow-up; sample sizes in full multivariate models range from 750–784 due to occasional missing values on exposures and covariates. We examined the interaction of each of the inflammatory and fibrinolytic proteins with age, sex, ethnicity, BMI, SI, AIR and glycemic status at baseline on the difference in MCRI between examinations. We plotted the frequency distribution of the yearly change in MCRI from baseline to 5-year follow-up.
In sensitivity analyses, we additionally adjusted for the use of glucose-lowering medications and incident diabetes to determine if these variables were confounders. To test the robustness of the association between plasma PAI-1 and the change in MCRI, we also adjusted for plasma CRP in this multivariable-adjusted regression model. Statistical analyses were performed using STATA 12.0 (StataCorp, College Station, TX, USA).
Results
The current study included 784 non-diabetic individuals who had measurements of MCRI at both baseline and follow-up examinations in the IRAS cohort. Participants had an average age of 55 years (interquartile range 47 to 62 years) and 45% were women. The ethnic distribution for non-Hispanic whites, African-Americans and Hispanics were 40%, 25% and 34% respectively. The median MCRI was 5.28 L/min (interquartile range 3.92 to 7.10 L/min) at baseline. Characteristics of the study population by thirds of the distribution of MCRI at baseline are shown in Table 1. Demographics, e.g. age, sex, and lifestyle factors, e.g. alcohol consumption, smoking, were similar between thirds of the MCRI distribution. Participants with MCRI in the bottom third of the baseline distribution, i.e., those with the lowest insulin clearance, compared with those in the top third, were more likely to be Hispanics, have family history of diabetes and have lower energy expenditure. In addition, they had higher values of BMI, waist circumference, plasma triacylglycerol, systolic blood pressure, fasting blood glucose and AIR, but lower values of SI and HDL-cholesterol. At baseline, the median levels of plasma inflammatory and fibrinolytic proteins were 327 pmol/l for PAI-1, 16.2 nmol/l for CRP, 3.4 ng/l for TNF-α, 7.9 μmol/l for fibrinogen and 12.7 μg/l for leptin.
Table 1.
Characteristics of non-diabetic participants in the IRAS, stratified by the distribution of MCRI at baseline
| N | Bottom third | Middle third | Top third | p-value | |
|---|---|---|---|---|---|
|
| |||||
| Metabolic clearance of insulin (l/min) | 784 | 3.47 (2.79, 3.92) | 5.28 (4.79, 5.71) | 8.01 (7.11, 9.76) | |
|
| |||||
| Age (years) | 784 | 54 (46, 61) | 55 (48, 63) | 55 (49, 63) | 0.23 |
|
| |||||
| Sex (% female) | 784 | 53.8 | 57.5 | 53.6 | 0.61 |
|
| |||||
| Ethnicity (%) | |||||
| Non-Hispanic whites | 784 | 32.1 | 38.7 | 49.8 | <0.001 |
| African-Americans | 25.6 | 29.5 | 21.1 | ||
| Hispanics | 42.4 | 31.8 | 29.1 | ||
|
| |||||
| Family history of diabetes (%) | 784 | 47.0 | 42.2 | 31.4 | 0.001 |
|
| |||||
| Current drinker (%) | 784 | 74.4 | 72.7 | 74.0 | 0.79 |
|
| |||||
| Current smoker (%) | 784 | 11.8 | 13.8 | 14.6 | 0.90 |
|
| |||||
| Total energy expenditure (kJ/kg/day) | 780 | 158 (150, 177) | 161 (149, 181) | 164 (152, 186) | 0.026 |
|
| |||||
| Body mass index (kg/m2) | 783 | 30.1 (27.7, 35.9) | 27.2 (25.2, 29.6) | 25.2 (23.2, 27.4) | <0.0001 |
|
| |||||
| Waist circumference (cm) | 782 | 97.7 (90.0, 104.5) | 89.1 (80.9, 95.3) | 84.3 (76.0, 91.0) | <0.0001 |
|
| |||||
| Triacylglycerol (mmol/l) | 781 | 1.55 (1.10, 2.08) | 1.15 (0.84, 1.76) | 1.08 (0.82, 1.59) | <0.0001 |
|
| |||||
| HDL-cholesterol (mmol/l) | 782 | 1.01 (0.85, 1.24) | 1.17 (0.95, 1.37) | 1.27 (1.06, 1.58) | <0.0001 |
|
| |||||
| Systolic blood pressure (mmHg) | 784 | 121 (111, 135) | 119 (109, 131) | 118 (108, 130) | 0.015 |
|
| |||||
| Fasting blood glucose (mmol/l) | 781 | 5.49 (5.16, 5.99) | 5.38 (5.05, 5.77) | 5.22 (4.94, 5.72) | <0.0001 |
|
| |||||
| Acute insulin response (μU/ml) | 784 | 66.3 (35.7, 105.7) | 44.3 (22.0, 71.0) | 25.3 (14.3, 45.7) | <0.0001 |
|
| |||||
| Insulin sensitivity (x10−4 min−1 [μU/l]−1) | 766 | 0.83 (0.43, 1.20) | 1.70 (1.19, 2.34) | 3.42 (2.31, 4.82) | <0.0001 |
|
| |||||
| CRP (nmol/l) | 783 | 23.1 (13.4, 53.2) | 15.8 (6.67, 25.8) | 10.2 (5.43, 21.0) | <0.0001 |
|
| |||||
| Fibrinogen (μmol/l) | 780 | 8.14 (7.32, 9.32) | 7.94 (7.03, 8.99) | 7.70 (6.79, 8.58) | <0.0001 |
|
| |||||
| Leptin (μg/l) | 750 | 20.3 (9.0, 33.2) | 13.2 (6.2, 23.9) | 8.0 (4.2, 16.6) | <0.0001 |
|
| |||||
| PAI-1 (pmol/l) | 779 | 462 (288, 692) | 327 (173, 500) | 250 (154, 365) | <0.0001 |
|
| |||||
| TNF-α (ng/l) | 783 | 3.79 (2.90, 4.73) | 3.32 (2.50, 4.27) | 3.21 (2.55, 4.03) | <0.0001 |
|
| |||||
| ALT (U/l) | 781 | 20 (14, 28) | 15 (11, 20) | 14 (9, 19) | <0.0001 |
|
| |||||
| Impaired glucose tolerance (%) | 784 | 43.1 | 31.4 | 23.4 | <0.0001 |
Data presented are medians (interquartile range) or n (%)
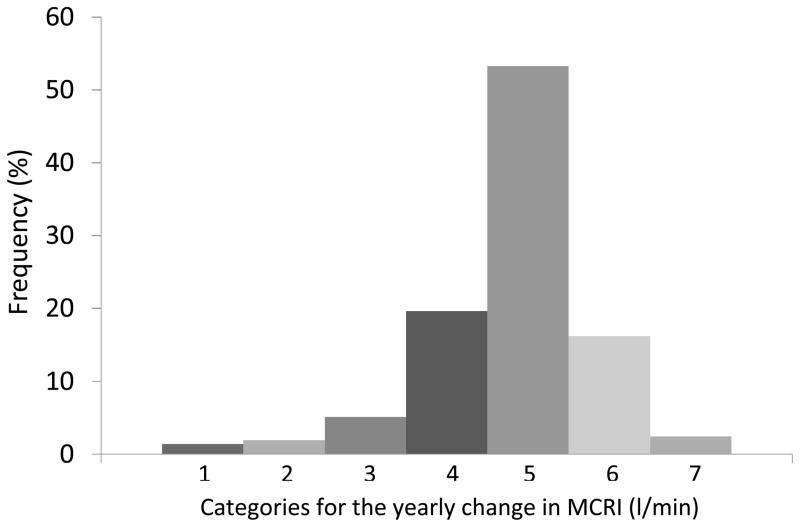
The median duration of follow-up was 5.2 years (interquartile range 5.0 to 5.4 years). MCRI declined by 29% between the baseline and 5-year follow-up examinations (p<0.001). The median decline of MCRI per year was 0.28 l/min (interquartile range 0.55 to 0.066 l/min). More than 50% of the participants had a yearly decline in MCRI in the range of 0.01 to 0.50 l/min (Figure 1). At follow-up, 124 participants were ascertained with the diagnosis of type 2 diabetes. Among these participants, 49 were on glucose lowering medications. Values of waist circumference and BMI were significantly higher, whereas value of SI was significantly lower. In addition, participants reported smoking less and having lower energy expenditure.
Figure 1.
Frequency distribution of the yearly change in MCRI (l/min) between baseline and 5-year follow-up examinations. Categories for the yearly change in MCRI (l/min): 1 = min to −2.0; 2 = −1.99 to −1.50; 3 = 1.49 to −1.00; 4 = −0.99 to −0.50; 5 = −0.49 to 0; 6 = 0.01 to 0.50; 7 = 0.51 to max
Higher PAI-1 was associated with a decline in MCRI in unadjusted regression models (β= −0.060 [−0.092, −0.028], p<0.001). The association remained significant after adjusting for age, sex, ethnicity, alcohol consumption, smoking, energy expenditure, family history of diabetes, HDL-cholesterol, TG, ALT, BMI, waist circumference, fasting blood glucose, SI and AIR (β= −0.045 [−0.081, −0.0091], p=0.014). In unadjusted linear regression analysis, higher plasma CRP was associated with a significant decline in MCRI (β= −0.035 [−0.059,−0.011], p=0.004). The association remained significant after adjusting for demographics (β= −0.046 [−0.071, −0.021], p<0.001). However, additional adjustment for BMI and waist circumference attenuated the association to non-significance (β= −0.016 [−0.041, 0.0083]). Similarly, we observed a significant association between increased plasma leptin and decline in MCRI in an unadjusted linear regression model (β= −0.035 [−0.066, −0.0041], p=0.026) and after adjusting for demographics (β= −0.15 [−0.19, −0.099], p<0.001). The association was no longer statistically significant after adjusting for BMI and waist circumference (β= −0.044 [−0.10, 0.011]).
Higher plasma TNF-α was associated with a decline of MCRI in unadjusted regression models (β= −0.071 [−0.14, −0.00087], p=0.047) and in models adjusted for age, sex and ethnicity (β= −0.12 [−0.20, −0.048], p=0.001). Adjusting for BMI and waist circumference attenuated the association, but it remained statistically significant (β= −0.085 [−0.16, −0.014], p=0.020). However, the association was not significant after further adjustment of HDL-cholesterol, TG and ALT (β= −0.056 [−0.13, 0.016]). Fibrinogen was not associated with the change in MCRI (Table 2). We did not find significant interactions of any of the inflammatory proteins with age, sex, ethnicity, BMI, SI, AIR, and glycemic status at baseline on the change in MCRI over time. In sensitivity analysis, including the use of glucose-lowering medications and incident diabetes, or plasma CRP, in the multivariable-adjusted regression models did not change the significant association between plasma PAI and the decline in MCRI materially.
Table 2.
Estimated regression coefficients (95% confidence intervals) on the association between plasma inflammatory proteins at baseline and at 5-year follow-up in the IRAS
| Outcome: follow-up ln(MCRI) | Beta-coefficients (95% CI) | p-value |
|---|---|---|
| Ln(CRP) n=783 | ||
| Adjusted for baseline ln(MCRI) | −0.035 (−0.059, −0.011) | 0.004 |
| + age, sex, ethnicity | −0.046 (−0.071, −0.021) | <0.001 |
| + BMI, waist circumference | −0.016 (−0.041, 0.0083) | 0.193 |
| + smoking, alcohol consumption, energy expenditure, family history of diabetes | −0.015 (−0.040, 0.0098) | 0.234 |
| + HDL, TG, ALT | −0.017 (−0.042, 0.0076) | 0.174 |
| + FBG, SI, AIR | −0.013 (−0.038, 0.012) | 0.311 |
| Ln(PAI-1) n=779 | ||
| Adjusted for baseline ln(MCRI) | −0.060 (−0.092, −0.028) | <0.001 |
| + age, sex, ethnicity | −0.096 (−0.13, −0.062) | <0.001 |
| + BMI, waist circumference | −0.060 (−0.094, −0.026) | 0.001 |
| + smoking, alcohol consumption, energy expenditure, family history of diabetes | −0.057 (−0.092, −0.022) | 0.001 |
| + HDL, TG, ALT | −0.047 (−0.083, −0.012) | 0.009 |
| + FBG, SI, AIR | −0.045 (−0.081, −0.091) | 0.014 |
| Fibrinogen n=780 | ||
| Adjusted for baseline ln(MCRI) | −0.00040 (−0.00088, 0.000075) | 0.099 |
| + age, sex, ethnicity | −0.00046 (−0.00095, 0.000028) | 0.065 |
| + BMI, waist circumference | 0.000040 (−0.00044, 0.00052) | 0.870 |
| + smoking, alcohol consumption, energy expenditure, family history of diabetes | 0.000077 (−0.00041, 0.00057) | 0.758 |
| + HDL, TG, ALT | 0.000066 (−0.00042, 0.00055) | 0.791 |
| + FBG, SI, AIR | 0.000043 (−0.0044, 0.00053) | 0.861 |
| Ln(leptin) n=750 | ||
| Adjusted for baseline ln(MCRI) | −0.035 (−0.066, −0.0044) | 0.026 |
| + age, sex, ethnicity | −0.15 (−0.19, −0.099) | <0.001 |
| + BMI, waist circumference | −0.044 (−0.10, 0.011) | 0.115 |
| + smoking, alcohol consumption, energy expenditure, family history of diabetes | −0.041 (−0.097, 0.014) | 0.146 |
| + HDL, TG, ALT | −0.059 (−0.11, −0.0037) | 0.037 |
| + FBG, SI, AIR | −0.042 (−0.098, 0.014) | 0.140 |
| Ln(TNF-α) n=779 | ||
| Adjusted for baseline ln(MCRI) | −0.071 (−0.14, −0.00087) | 0.047 |
| + age, sex, ethnicity | −0.12 (−0.20, −0.048) | 0.001 |
| + BMI, waist circumference | −0.085 (−0.16, −0.014) | 0.020 |
| + smoking, alcohol consumption, energy expenditure, family history of diabetes | −0.076 (−0.15, −0.0039) | 0.039 |
| + HDL, TG, ALT | −0.056 (−0.13, 0.016) | 0.126 |
| + FBG, SI, AIR | −0.056 (−0.13, 0.017) | 0.129 |
Discussion
In non-diabetic individuals participating in the IRAS, higher plasma PAI-1 at baseline was associated with lower MCRI at 5-year follow-up. The significant association remained after adjusting for MCRI at baseline, demographics, lifestyle factors and established risk factors for diabetes, including BMI and directly measured SI. We observed an inverse association of plasma CRP and leptin at baseline with MCRI at follow-up, however, these associations were confounded by indexes of obesity and abdominal adiposity, i.e., BMI and waist circumference. We also observed that the inverse association between plasma TNF-α at baseline and the MCRI at follow-up was confounded by HDL-cholesterol, TG and ALT. Plasma fibrinogen was not associated with the change in MCRI. To our knowledge, this is the first study to investigate the association of plasma inflammatory and fibrinolytic proteins with the dynamic change of MCRI over time.
It is well-established that higher plasma PAI-1 is a central feature of metabolic syndrome [26], and higher levels prevail through the continuum of insulin resistance, from impaired glucose tolerance to diabetes [27]. Previous observations from the IRAS cohort showed that both plasma PAI-1 at baseline and the progression of plasma PAI-1 over time predicts incident type 2 diabetes, independent of known risk factors for diabetes [6, 28]. Pharmaceutical and lifestyle interventions to treat diabetes, such as dietary modification and weight reduction [29], metformin [30], thiazolidinedione [31] and insulin [32] have been shown to decrease plasma PAI-1. In this study, however, when we included incident diabetes and use of glucose-lowering medications in the regression models, we observed minimal change in the magnitude of the association between plasma PAI-1 and reduced MCRI.
The association between higher plasma PAI-1 and reduced MCRI may be mediated by inflammation. In sensitivity analyses, however, adjustment for plasma CRP did not alter the significant association between higher plasma PAI-1 and the decline of MCRI. This observation provides further support for a mechanism specific to PAI-1, which may represent a yet unmeasured inflammatory mechanism. It has also been suggested that higher PAI-1 indicates compromised fibrinolysis more than an inflammatory process [28]. Tissue plasminogen activator (tPA) antigen, which is less variable than plasma PAI-1, has been shown to predict incident type 2 diabetes [36] and gestational diabetes [37]. Therefore, it is possible that the association between plasma PAI-1 and the decline of MCRI that we observed was linked to the PAI-1 and tPA antigen complex, through a mechanism involving impaired fibrinolysis.
It is conceivable that the association of higher plasma PAI-1 with reduced insulin clearance over time may reflect hepatic dysfunction, given both the primary role of the liver in insulin clearance [33] and the association of liver injury with higher plasma PAI-1 [34]. Although the significant association remained after adjusting for ALT, transaminases such as ALT are indirect measures of liver function, and thus we may not be able to capture fully the role of liver disease in the present study. As such, we may have observed a stronger magnitude of attenuation if liver function had been measured directly, e.g. by liver biopsy. Although the liver is a crucial site for lipid metabolism, adjusting for HDL-cholesterol and TG did not confound the association between plasma PAI-1 and the decline in MCRI. Furthermore, plasma PAI-1 has been significantly associated with the degree of liver steatosis [35] and it is possible that liver fat, which was not measured directly in the IRAS, links plasma PAI-1 to reduced insulin clearance.
We observed that the association between plasma CRP and the decline of MCRI over time was significantly confounded by measures of obesity and abdominal adiposity, but not by insulin resistance. Although a meta-analysis of 16 prospective studies demonstrated that plasma CRP was associated with the risk of incident type 2 diabetes, studies that adjusted for abdominal adiposity reported a much weaker association than those that did not make these adjustments, indicating a possibility of residual confounding [7]. To further support the notion that plasma CRP may not be causally related to type 2 diabetes, CRP haplotypes showed null associations with insulin resistance, glycemia and risk of diabetes in Mendelian randomization [38]. Since insulin clearance is closely related to insulin resistance [39], it is unlikely that plasma CRP independently predicts the progressive decline of MCRI as shown in our data.
Similar to plasma CRP, the association between plasma TNF-α and the decline of MCRI was attenuated after adjusting for BMI and waist circumference, as well as HDL-cholesterol and TG. TNF-α is an inflammatory adipokine expressed primarily by monocytes and macrophages, and it plays an important role in adipocyte function and obesity-related insulin resistance [40]. There is an overexpression of TNF-α in the adipose tissues of obese persons, and plasma TNF-α is directly related to BMI and hyperinsulinemia [41]. In addition, TNF-α is a potent regulator in lipid metabolism through mechanisms that increase the synthesis of free fatty acids, promote lipogenesis, induce lipolysis and inhibit enzymes related to lipid metabolism [42], whereas elevated TG and decreased HDL-cholesterol are associated with insulin resistance [43]. Cross-sectional studies have shown a positive association between plasma TNF-α and insulin resistance [23, 44]. However, prospective studies on the association between plasma TNF-α and incident diabetes showed inconsistent results, likely due to confounding by insulin resistance. Although no previous studies have investigated the association between plasma TNF-α and MCRI, the null association that we observed is consistent with the literature on insulin resistance.
Leptin is an adipocytokine secreted almost exclusively by adipose tissues in proportion to total fat mass [45]. Higher plasma leptin was associated with an acute-phase response in individuals with type 2 diabetes, confirming its role as an inflammatory marker [46]. A cross-sectional study on 30 non-diabetic individuals of different ethnicities (Chinese, Asian Indians and Caucasians) reported a significant inverse association between plasma leptin and MCRI, independent of BMI, waist-hip ratio and percentage of body fat and ethnicity; however, this study did not adjust for insulin sensitivity [47]. In contrast, we observed that the association between plasma leptin and change in MCRI over time was confounded by BMI and waist circumference. Insulin clearance is a highly heritable trait [48], thus ethnic differences between the studies in metabolic characteristics, such as plasma leptin concentration, distribution of body fat and degree of insulin sensitivity and clearance, may exist. In addition, the prospective design of our study may also explain the inconsistent findings with previous cross-sectional studies.
Our data showed that plasma fibrinogen at baseline was not associated with the change in MCRI at follow-up. Although previous studies have reported a cross-sectional association between plasma fibrinogen and insulin resistance [27, 49], plasma fibrinogen did not predict incident type 2 diabetes [28, 50]. Therefore, our observation on the null association between plasma fibrinogen and progression of MCRI is plausible.
In addition to its novel findings, the strengths of this study include the well-characterized multi-ethnic population, prospective design, and detailed measurements of insulin clearance, secretion and sensitivity from FSIGTT. However, our study may be limited by the relatively short period of follow-up and the limited range of inflammatory markers. We also did not have direct measures of insulin clearance. Although the IRAS cohort was enriched with participants with IGT, it is notable that the fasting blood glucose levels of non-diabetic IRAS participants were similar to those in the NHANES in the NGT and IGT categories, and that a considerable proportion of the study population had NGT at baseline. Nevertheless, our findings are likely generalizable only to non-diabetic individuals at risk of glucose intolerance in similar ethnic groups.
In conclusion, we observed a significant association of plasma PAI-1, but not plasma levels of CRP, TNF-α, leptin and fibrinogen, with the progressive decline of MCRI over time. The present study has several important implications. First, it extends the scientific literature on the role of inflammatory and fibrinolytic proteins in the aetiology of type 2 diabetes. Second, our findings point to the need for future studies to prove a causal link between higher plasma PAI-1 and the decline of MCRI, and for randomised controlled trials to test the clinical significance of targeting impaired fibrinolysis as a means to decrease the incidence of type 2 diabetes.
Acknowledgments
Funding
C. C. Lee is supported by a postdoctoral research fellowship from the Banting & Best Diabetes Centre, University of Toronto, Canada. A. J. Hanley holds a Tier II Canada Research Chair in Diabetes Epidemiology. IRAS was supported by grants U01-HL47892, U01-HL47902, DK-29867, R01-58329 from National Heart, Lung and Blood Institute, and grant M01-RR-43 from the National Institutes of Health.
Abbreviations
- AIR
acute insulin response
- CRP
C-reactive protein
- FSIGTT
frequently sampled intravenous glucose tolerance test
- IRAS
Insulin Resistance Atherosclerosis Study
- MCRI
metabolic clearance rate of insulin
- PAI-1
plasminogen activator inhibitor-1
- SI
insulin sensitivity
- TNF-α
tumor necrosis factor-α
Footnotes
Contribution Statement
CCL wrote the manuscript, analysed and interpreted the data, revised critically for important intellectual content and approved the final version for publication. SMH, LEW and MJR designed the study, collected data, interpreted the data, revised critically for important intellectual content and approved the final version for publication. CL, AF, MOG, DS, NCO, JMN and AJH interpreted the data, revised critically for important intellectual content and approved the final version for publication.
References
- 1.Meigs JB. Insulin resistance syndrome? Syndrome X? Multiple metabolic syndrome? A syndrome at all? Factor analysis reveals patterns in the fabric of correlated metabolic risk factors. Am J Epidemiol. 2000;152:908–11. doi: 10.1093/aje/152.10.908. [DOI] [PubMed] [Google Scholar]
- 2.Chan JC, Tong PC, Critchley JA. The insulin resistance syndrome: mechanisms of clustering of cardiovascular risk. Semin Vasc Med. 2002;2:45–57. doi: 10.1055/s-2002-23095. [DOI] [PubMed] [Google Scholar]
- 3.Mittelman SD, Van Citters GW, Kim SP, et al. Longitudinal compensation for fat-induced insulin resistance includes reduced insulin clearance and enhanced beat-cell response. Diabetes. 2005;49:2116–25. doi: 10.2337/diabetes.49.12.2116. [DOI] [PubMed] [Google Scholar]
- 4.Pickup JC, Crook MA. Is type II diabetes mellitus a disease of the innate immune system? Diabetologia. 1998;41:1241–8. doi: 10.1007/s001250051058. [DOI] [PubMed] [Google Scholar]
- 5.Trost S, Pratley R, Sobel B. Impaired fibrinolysis and risk for cardiovascular disease in the metabolic syndrome and type 2 diabetes. Curr Diab Rep. 2006;6:47–54. doi: 10.1007/s11892-006-0052-5. [DOI] [PubMed] [Google Scholar]
- 6.Festa A, D’Agostino R, Tracy RP, Haffner SM. Elevated levels of acute-phase proteins and plasminogen activator inhibitor-1 predict the development of type 2 diabetes. The Insulin Resistance Atherosclerosis Study. Diabetes. 2002;51:1131–7. doi: 10.2337/diabetes.51.4.1131. [DOI] [PubMed] [Google Scholar]
- 7.Lee CC, Adler AI, Sandhu MS, et al. Association of C-reactive protein with type 2 diabetes: prospective analysis and meta-analysis. Diabetologia. 2009;52:1040–7. doi: 10.1007/s00125-009-1338-3. [DOI] [PubMed] [Google Scholar]
- 8.Gkrania-Klotsas E, Ye Z, Cooper AJ, et al. Differential white blood cell count and type 2 diabetes: systematic review and meta-analysis of cross-sectional and prospective studies. PLoS One. 2010;5:e13405. doi: 10.1371/journal.pone.0013405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Festa A, D’Agostino R, Howard G, et al. Chronic subclinical inflammation as part of the insulin resistance syndrome. Circulation. 2000;102:42–7. doi: 10.1161/01.cir.102.1.42. [DOI] [PubMed] [Google Scholar]
- 10.Haffner SM, Mykkanen L, Rainwater DL, Karhapaa P, Laakso M. Is leptin concentration associated with the insulin resistance syndrome in nondiabetic men? Obes Res. 1999;7:164–9. doi: 10.1002/j.1550-8528.1999.tb00698.x. [DOI] [PubMed] [Google Scholar]
- 11.Sakkinen PA, Wahl P, Cushman M, Lewis MR, Tracy RP. Clustering of procoagulation, inflammation, and fibrinolysis variables with metabolic factors in insulin resistance syndrome. Am J Epidemiol. 2000;152:897–907. doi: 10.1093/aje/152.10.897. [DOI] [PubMed] [Google Scholar]
- 12.Wagenknecht LE, Mayer EJ, Rewers M, et al. The insulin resistance atherosclerosis study (IRAS) objectives, design, and recruitment results. Ann Epidemiol. 1995;5:464–72. doi: 10.1016/1047-2797(95)00062-3. [DOI] [PubMed] [Google Scholar]
- 13.Bergman RN, Finegood DT, Ader M, et al. Assessment of insulin sensitivity in vivo. Endocrine Rev. 1985;6:45–86. doi: 10.1210/edrv-6-1-45. [DOI] [PubMed] [Google Scholar]
- 14.Welch S, Gebhart SS, Bergman RN, Phillips LS. Minimal model analysis of intravenous glucose tolerance test derived insulin sensitivity in diabetic subjects. J Clin Endocrinol Metab. 1990;71:1508–18. doi: 10.1210/jcem-71-6-1508. [DOI] [PubMed] [Google Scholar]
- 15.Steil GM, Volund A, Kahn SE, Bergman RN. Reduced sample number for calculation of insulin sensitivity and glucose effectiveness from the minimal model: suitability for use in population studies. Diabetes. 1993;42:250–6. doi: 10.2337/diab.42.2.250. [DOI] [PubMed] [Google Scholar]
- 16.Lorenzo C, Wagenknecht LE, D’Agostino RB, Jr, et al. Insulin resistance, beta-cell dysfunction, and conversion to type 2 diabetes in multiethnic population: the Insulin Resistance Atherosclerosis Study. Diabetes Care. 2010;33:67–72. doi: 10.2337/dc09-1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Polonsky KS, Pugh W, Jaspan JB, et al. C-peptide and insulin secretion. Relationship between peripheral concentrations of C-peptide and insulin and their section rates in the dog. J Clin Invest. 1984;74:1821–9. doi: 10.1172/JCI111601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Declerck P, Collen D. Measurement of plasminogen activator inhibitor 1 (PAI-1) in plasma with various monoclonal antibody-based enzyme-linked immunosorbent assays. Thromb Res. 1990;10(suppl):3–9. doi: 10.1016/0049-3848(90)90373-k. [DOI] [PubMed] [Google Scholar]
- 19.Macy E, Hayes T, Tracy R. Variability in the measurement of C-reactive protein in healthy subjects: implications for reference interval and epidemiological applications. Clin Chem. 1997;43:52–8. [PubMed] [Google Scholar]
- 20.Clauss A. Rapid physiological coagulation method for the determination of fibrinogen. Acta Haematol. 1957;17:237–46. doi: 10.1159/000205234. [DOI] [PubMed] [Google Scholar]
- 21.Geffken D, Keating F, Kennedy M, et al. The measurement of fibrinogen in population-based research: studies on instrumentation and methodology. Arch Pathol Lab Med. 1994;118:1106–9. [PubMed] [Google Scholar]
- 22.Lorenzo C, Nath SD, Hanley AJ, Abboud HE, Haffner SM. Relation of low glomerular filtration rate to metabolic disorders in individuals without diabetes and with normoalbuminuria. Clin J Am Soc Nephrol. 2008;3:783–9. doi: 10.2215/CJN.02730707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Olson NC, Callas PW, Hanley AJ, et al. Circulating Levels of TNF-α Are Associated with Impaired Glucose Tolerance, Increased Insulin Resistance, and Ethnicity: The Insulin Resistance Atherosclerosis Study. J Clin Endocrinol Metab. 2012;97:1032–40. doi: 10.1210/jc.2011-2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Howard BV, Mayer-Davis EJ, Goff D, et al. Relationships between insulin resistance and lipoproteins in nondiabetic African Americans, Hispanics, and non-Hispanic whites: the Insulin Resistance Atherosclerosis Study. Metabolism. 1998;47:1174–9. doi: 10.1016/s0026-0495(98)90319-5. [DOI] [PubMed] [Google Scholar]
- 25.Wagenknecht LE, Palmer ND, Bowden DW, et al. Association of PNPLA3 with non-alcoholic fatty liver disease in a minority cohort: the Insulin Resistance Atherosclerosis Family Study. Liver Int. 2011;31:412–6. doi: 10.1111/j.1478-3231.2010.02444.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Juhan-Vague I, Alessi MC, Mavri A, Morange PE. Plasminogen activator inhibitor-1, inflammation, obesity, insulin resistance and vascular risk. J Thromb Haemost. 2003;1:1575–9. doi: 10.1046/j.1538-7836.2003.00279.x. [DOI] [PubMed] [Google Scholar]
- 27.Festa A, D’Agostino R, Jr, Mykkanen L, et al. Relative contribution of insulin and its precursors to fibrinogen and PAI-1 in large population with different states of glucose tolerance: the Insulin Resistance Atherosclerosis Study (IRAS) Arterioscler Thromb Vasc Biol. 1999;19:562–8. doi: 10.1161/01.atv.19.3.562. [DOI] [PubMed] [Google Scholar]
- 28.Festa A, Williams K, Tracy RP, Wagenknecht LE, Haffner SM. Progression of plasminogen activator inhibitor-1 and fibrinogen levels in relation to incident type 2 diabetes. Circulation. 2006;113:1753–9. doi: 10.1161/CIRCULATIONAHA.106.616177. [DOI] [PubMed] [Google Scholar]
- 29.Lee KW, Lip GY. Effects of lifestyle on hemostasis, fibrinolysis and platelet reactivity: a systematic review. Arch Intern Med. 2003;163:2368–92. doi: 10.1001/archinte.163.19.2368. [DOI] [PubMed] [Google Scholar]
- 30.Nagi DK, Yudkin JS. Effects of metformin on insulin resistance, risk factors for cardiovascular disease and plasminogen activator inhibitor in NIDDM subjects. A study of two ethnic groups. Diabetes Care. 1993;16:621–9. doi: 10.2337/diacare.16.4.621. [DOI] [PubMed] [Google Scholar]
- 31.Fonseca VA, Reynolds T, Hemphill D, et al. Effect of troglitazone on fibrinolysis and activated coagulation in patients with non-insulin-dependent diabetes mellitus. J Diabetes Complications. 1998;12:181–6. doi: 10.1016/s1056-8727(97)00109-8. [DOI] [PubMed] [Google Scholar]
- 32.Jain SK, Nagi DK, Slavin BM, Lumb PJ, Yudkin JS. Insulin therapy in type 2 diabetic subjects suppresses plasminogen activator inhibitor (PAI-1) activity and proinsulin-like molecules independently of glycemic control. Diabet Med. 1993;10:27–32. doi: 10.1111/j.1464-5491.1993.tb01992.x. [DOI] [PubMed] [Google Scholar]
- 33.Duckworth WC, Bennett RG, Hamel FG. Insulin degradation: progress and potential. Endocr Rev. 1998;19:608–24. doi: 10.1210/edrv.19.5.0349. [DOI] [PubMed] [Google Scholar]
- 34.Inoue K, Sugawara Y, Kubota K, Takayama T, Makuuchi M. Induction of type I plasminogen activator inhibitor in human liver ischemia and reperfusion. J Hepatol. 2000;33:407–14. doi: 10.1016/s0168-8278(00)80276-7. [DOI] [PubMed] [Google Scholar]
- 35.de Larrañaga G, Wingeyer SP, Graffigna M, et al. Plasma plasminogen activator inhibitor-1 levels and nonalcoholic fatty liver in individuals with features of metabolic syndrome. Clin Appl Thromb Hemost. 2008;14:319–24. doi: 10.1177/1076029607304094. [DOI] [PubMed] [Google Scholar]
- 36.Eliasson MC, Jansson JH, Lindahl B, Stegmayr B. High levels of tissue plasminogen activator (tPA) antigen precede the development of type 2 diaebtes in a longitudinal population study. The Northern Sweden MONICA study. Cardiovasc Diabetol. 2003;2:19. doi: 10.1186/1475-2840-2-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Savvidou M, Nelson SM, Makgoba M, et al. First-trimester prediction of gestational diabetes mellitus: examining the potential of combining maternal characteristics and laboratory measures. Diabetes. 2010;59:3017–22. doi: 10.2337/db10-0688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brunner EJ, Kivimaki M, Witte DR, et al. Inflammation, insulin resistance and diabetes – Mendelian Randomization using CRP haplotypes points upstream. PLoS Med. 2008;5(8):e155. doi: 10.1371/journal.pmed.0050155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Flier JS, Minaker KL, Landsberg L, et al. Impaired in vivo insulin clearance in patients with severe target-cell resistance to insulin. Diabetes. 1982;31:132–5. doi: 10.2337/diab.31.2.132. [DOI] [PubMed] [Google Scholar]
- 40.Cawthorn WP, Sethi JK. TNF-alpha and adipocyte biology. FEBS Lett. 2008;582:117–31. doi: 10.1016/j.febslet.2007.11.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hotamisligil GS, Arner P, Caro JF, Atkinson RL, Spiegelman BM. Increased adipose tissue expression of tumor necrosis factor-alpha in human obesity and insulin resistance. J Clin Invest. 1995;95:2409–15. doi: 10.1172/JCI117936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen X, Xun K, Chen L, Wang Y. TNF-alpha, a potent lipid metabolism regulator. Cell Biochem Funct. 2009;27:407–16. doi: 10.1002/cbf.1596. [DOI] [PubMed] [Google Scholar]
- 43.Laakso M, Sarlund H, Mykkänen L. Insulin resistance is associated with lipid and lipoprotein abnormalities in subjects with varying degrees of glucose tolerance. Arteriosclerosis. 1990;10:223–31. doi: 10.1161/01.atv.10.2.223. [DOI] [PubMed] [Google Scholar]
- 44.Plomgaard P, Nielsen AR, Fischer CP, et al. Associations between insulin resistance and TNF-alpha in plasma, skeletal muscle and adipose tissue in humans with and without type 2 diabetes. Diabetologia. 2007;50:2562–71. doi: 10.1007/s00125-007-0834-6. [DOI] [PubMed] [Google Scholar]
- 45.Kershaw EE, Flier JS. Adipose tissue as an endocrine organ. J Clin Endocrinol Metab. 2004;89:2548–56. doi: 10.1210/jc.2004-0395. [DOI] [PubMed] [Google Scholar]
- 46.Pickup JC, Chusney GD, Mattock MB. The innate immune response and type 2 diabetes: evident that leptin is associated with a stress-related (acute-phase) reaction. Clin Endocrinol (Oxf) 2000;52:107–12. doi: 10.1046/j.1365-2265.2000.00921.x. [DOI] [PubMed] [Google Scholar]
- 47.Liew CF, Seah ES, Yeo KP, Lee KO, Wise SD. Lean, nondiabetic Asian Indians have decreased insulin sensitivity and insulin clearance, and raised leptin compared to Caucasians and Chinese subjects. International Journal of Obesity. 2003;27:784–9. doi: 10.1038/sj.ijo.0802307. [DOI] [PubMed] [Google Scholar]
- 48.Goodarzi MO, Taylor KD, Guo X, et al. Variation in the gene for muscle-specific AMP deaminase is associated with insulin clearance, a highly heritable trait. Diabetes. 2005;54:1222–7. doi: 10.2337/diabetes.54.4.1222. [DOI] [PubMed] [Google Scholar]
- 49.Mohamed-Ali V, Gould MM, Gillies S, et al. Association of proinsulin-like molecules with lipids and fibrinogen in non-diabetic subjects: evidence against a modulating role for insulin. Diabetologia. 1995;38:1110–6. doi: 10.1007/BF00402183. [DOI] [PubMed] [Google Scholar]
- 50.Bertom AG, Burke G, Owusu JA, et al. Inflammation and the incidence of type 2 diabetes. The Multi-Ethnic Study of Atherosclerosis (MESA) Diabetes Care. 2010;33:804–10. doi: 10.2337/dc09-1679. [DOI] [PMC free article] [PubMed] [Google Scholar]