Abstract
Objective
On October 1, 2013, the reporting of diagnoses and procedures in the U.S. will transition from the clinical modification of the ninth revision of the International Classification of Diseases (ICD-9-CM) to the tenth revision (ICD-10). We estimate the impact of conversion to ICD-10 on Medicare MS-DRG payments to hospitals using 2009 Medicare data.
Methods
Using the ICD-9-CM MS-DRG v27 (FY 2010), the converted ICD-10 MS-DRG v27, and the ICD-10 to ICD-9-CM Reimbursement Map for fiscal year 2010, we estimate the impact on aggregate payments to hospitals and the distribution of payments across hospitals.
Results
Although the transition from the ICD-9-CM to the ICD-10 version of MS-DRGs resulted in 1.68 percent of the patients being assigned to a different MS-DRG, payment increases and decreases due to the changes in MS-DRG assignment essentially netted out, resulting in a minimal impact on aggregate payments to hospitals (+0.05 percent) and on the distribution of payments across hospital types (-0.01 to +0.18 percent). Mapping ICD-10 data back to ICD-9-CM, and using the ICD-9-CM MS-DRGs, resulted in 3.66 percent of patients being assigned to a different MS-DRG, a modest decrease in aggregate payments to hospitals (-0.34 percent), and modest changes in the distribution of payments across hospital types (-0.14 to -0.46 percent).
Discussion
As demonstrated by MS-DRGs, a direct conversion of an application to ICD-10 can produce consistent results with the ICD-9-CM version of the application. However, the use of mappings between ICD-10 and ICD-9-CM will produce less consistent results, especially if the mapping is not tailored to the specific application.
Key words: ICD-10, Mapping, Payment Impact, MS-DRGs, Medicare
Since 1979, the U.S. has used the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) to report diagnosis data across all sites of service and procedure data for inpatient care. On October 1, 2013, ICD-9-CM will be replaced by the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) to report diagnosis data across all sites of service, and the International Classification of Diseases, Tenth Revision, Procedure Coding System (ICD-10-PCS) to report inpatient procedure data. ICD-10-CM/PCS substantially increases the level of clinical detail that can be captured and reported. In the FY 2009 update of ICD-9-CM, there were 14,025 diagnosis codes and 3,824 procedure codes. In the FY 2010 update of ICD-10-CM, there were 69,101 diagnosis codes and in ICD-10-PCS there were 71,957 procedure codes. For brevity ICD-10-CM/PCS will be referred to as ICD-10.
Since diagnosis and procedure based patient classification systems, such as the Diagnosis Related Groups (DRGs), are used in payment methodologies, payers must adapt their payment systems to ICD-10. Payers can either directly convert their payment systems to be based on ICD-10 codes or use a mapping system, such as the Reimbursement Map from the Centers for Medicare & Medicaid Services (CMS), to convert reported ICD-10 codes to ICD-9-CM and then process the converted codes using ICD-9-CM based applications. Under a mapping approach, as providers submit claims with ICD-10 codes, the payer would map each code to an equivalent ICD-9-CM code (or codes) so existing ICD-9-CM based payment applications could continue to be used by the payer. In many areas, ICD-10 classifies clinical conditions and procedures differently from ICD-9-CM. As a result, the conversion of complex payment methodologies, or the use of maps from ICD-10 to ICD-9-CM, could have an unintended impact on aggregate payments to providers or the distribution of payments across providers.
Medicare uses the Medicare Severity-Diagnosis Related Groups (MS-DRGs) as the basis of payment in the Medicare inpatient prospective payment system (IPPS). CMS has posted an ICD-10 version of MS-DRGs on its Web site (Centers for Medicare & Medicaid Services [CMS], 2010a). The availability of both versions of MS-DRGs can provide the basis for quantifying the impact on aggregate payments to hospitals, and the distribution of payments across hospitals, arising from the conversion of MS-DRGs to ICD-10. In addition, CMS has posted an ICD-10 to ICD-9-CM Reimbursement Map on its Web site (CMS, 2010b). The Reimbursement Map selects a single ICD-9-CM coding alternative that represents the most reasonable match for each ICD-10 code for the purpose of MS-DRG assignment. The availability of the reimbursement map can provide the basis for quantifying the impact on aggregate payments to hospitals, and the distribution of payments across hospitals, resulting from the use of the ICD-9-CM version of the MS-DRGs with mapped ICD-10 data.
This paper uses the ICD-9-CM MS-DRG v27 (FY 2010), the converted ICD-10 MS-DRG v27, and the ICD-10 to ICD-9-CM Reimbursement Map for fiscal year 2010, to estimate the impact on aggregate payments to hospitals and the distribution of payments across hospitals. Payments based on the MS-DRGs assigned using ICD-9-CM coded data with the ICD-9-CM version of the MS-DRGs are compared to:
Payments based on the MS-DRGs assigned using ICD-10 coded data with the ICD- 10 version of the MS-DRGs.
Payments based on the MS-DRGs assigned using ICD-10 coded data converted back to ICD-9-CM, using the Reimbursement Map with the ICD-9-CM version of the MS-DRGs.
Methods
Creating an ICD-10 Database
Since there is no large scale database available that contains diagnosis and procedure data coded in ICD-10, it was necessary to create a simulated ICD-10 database by using the General Equivalence Mappings (GEMs). The GEMs are a comprehensive, translation dictionary between ICD-9-CM and ICD-10. Taking the complete meaning of a code as a single unit, the GEMs identify the most appropriate translation(s) to the other code set. There is an ICD-9-CM to ICD-10 GEM and an ICD-10 to ICD-9-CM GEM for both diagnoses and procedures. CMS has posted the GEMs on its Web site (CMS, 2010c).
The database used to create the simulated ICD-10 data was the FY 2009 Medicare Provider Analysis and Review (MedPAR) data. The FY 2009 MedPAR database contained all Medicare inpatient claims from acute care hospitals with a discharge date in from 10/1/2008 through 9/30/2009. There were 10,984,798 inpatient claims coded in ICD-9-CM in the FY 2009 MedPAR database.
For each MedPAR record in the 2009 database, a plausible ICD-10 record was created using the GEMs. Given the information available in the ICD-9-CM codes on the record, the objective of the translation was to create a correctly coded ICD-10 version of the same record. Due to the increased specificity of ICD-10, a single ICD-9-CM code often translates to multiple ICD-10 codes in the GEMs. The translation process required selecting a single ICD-10 code from among the alternative possible translations in the GEMs. A set of context specific translation rules was developed to automate the selection of the best possible ICD-10 translation alternative. The ICD-9-CM codes on a record were not translated one-by-one, but instead the entire contents of the record were taken into account in creating a translated version. By evaluating the entire record coded as ICD-9-CM, the selection of the ICD-10 codes that best represented how the record could be translated was done in the context of the complete ICD-9-CM based description of the patient, thereby improving the accuracy of the ICD-10 replication of the record.
The context specific translation rules employed to create an ICD-10 coded version of the MedPAR database were as follows:
If an ICD-9-CM code is translated to only a single ICD-10 code in the GEMs, the ICD-9-CM code is translated to the corresponding ICD-10 code.
For single ICD-9-CM codes that translate to multiple ICD-10 alternatives, the ICD-10 to ICD-9-CM GEM is used in a reverse lookup to determine if any of the alternative codes also translate back to the code being translated. If such ICD-10 to ICD-9-CM translations are present, the possible ICD-10 code translations are limited to those alternatives. For example, in the GEMs ICD-9-CM code 250.40 (Diabetes with renal manifestations, type II or unspecified type, not stated as uncontrolled) translates to ICD-10 codes E11.21 (Type 2 diabetes mellitus with diabetic nephropathy), E11.22 (Type 2 diabetes mellitus with diabetic chronic kidney disease) and E11.29 (Type 2 diabetes mellitus with other diabetic kidney complication). Thus, there are three separate ICD-10 codes for type II diabetes with renal manifestations. In the ICD-10 to ICD-9-CM GEMs, only ICD-10 code E11.29 translates back to ICD-9-CM code 250.40, because E11.21 and E11.22 require two ICD-9-CM codes to be translated in order to express their full meaning (i.e., additional codes for nephropathy or chronic kidney disease). Therefore, from the ICD-10 perspective, only E11.29 translates to code 250.40 in the GEMs and represents the best ICD-10 translation alternative for ICD-9-CM code 250.40.
Some ICD-9-CM procedure codes do not contain a specification of the anatomic site of the procedure. As a result, such procedure codes translate to many anatomically specific ICD-10 procedure codes in the GEMs. In order to select among the anatomically specific alternative codes, the body system of the ICD-9-CM code reported as the principal diagnosis is used to select the best possible translation alternative. For example, ICD-9-CM code 92.27 (Implantation or insertion of radioactive element) has 263 possible anatomic site alternatives. If the principal diagnosis is a prostate diagnosis, the anatomic site for the ICD-10, radioactive element, implant code translation is the prostate.
Some diagnoses or procedures that can be coded as a single code in ICD-10 require multiple ICD-9-CM codes (a “cluster”) to be present on the record to express the same meaning. For example, ICD-10 diagnosis code L89.44 (pressure ulcer of contiguous site of back, buttock and hip, stage IV) requires that four separate ICD-9-CM codes, specifying the three ulcer sites and the stage, be coded in order to replicate the full meaning of the ICD-10 code. When all the codes in a cluster are present, they are translated to a single ICD-10 code.
Some ICD-9-CM codes contain a specification of multiple diseases or procedures. ICD-9-CM “combination” codes require multiple ICD-10 codes to be reported in order to replicate the codes on the record. When a combination code is present, the translation process replicates the code to multiple ICD-10 codes corresponding to the individual diseases or procedures contained in the combination code. For example, the translation process for ICD-9-CM diagnosis code 038.12 (Methicillin resistant staph aureus septicemia), which includes both the diagnosis of staph aureus septicemia and the fact that the organism is resistant to treatment with methicillin, replicates to two ICD-10 codes: one corresponding to the staph aureus sepsis and the other corresponding to the resistance of the organism to antibiotics. ICD-9-CM procedure code 48.52 (open abdominoperineal resection of the rectum), which includes both resection of the rectum and colostomy creation, translates to two ICD-10 codes: one corresponding to the resection of the rectum and the other corresponding to the creation of the colostomy.
Some diagnoses are gender-specific in ICD-10, but not in ICD-9-CM. When translating a non-gender-specific ICD-9-CM code whose corresponding ICD-10 codes are gender-specific, the gender of the patient reported on the claim is used to select the appropriate ICD-10 alternative.
For some conditions comprised of a manifestation with an associated underlying cause, the ICD-10-CM and ICD-9-CM coding rules for selecting the principal diagnosis are different. For example, when a patient is admitted for anemia secondary to chronic kidney disease, ICD-9-CM coding rules require that the anemia be coded as the principal diagnosis, whereas ICD-10-CM coding rules require that the chronic kidney disease be coded as the principal diagnosis. For all claims that contain a principal and a secondary diagnosis for which this coding rule difference is applicable (e.g., all records with anemia as the principal diagnosis and chronic kidney disease as a secondary diagnosis), the secondary diagnosis code representing the underlying cause is made the principal diagnosis and the principal diagnosis representing the manifestation is made a secondary diagnosis.
Adjunct codes in ICD-9-CM are sometimes needed to fully specify a procedure (e.g., for a PTCA, adjunct codes are used to specify the number of sites, number of vessels, whether a drug-eluting stent was used, and whether the site was a bifurcation). Adjunct codes are not needed in ICD-10-PCS, since a single ICD-10 code contains all the information needed to describe all aspects of a procedure. Adjunct codes, along with the ICD-9-CM underlying procedure code, are translated to a single ICD-10 code.
Once all of the context specific translation rules were applied, there still could remain some ICD-9-CM codes on a record that had more than one possible ICD-10 translation. In most instances, this was due to ICD-10 having axes of classification (e.g., laterality–left or right), or more detailed anatomic specificity than could be deduced from any of the ICD-9-CM codes on the record. Because the objective was to create an ICD-10 coded version of each record in the MedPAR data, it was necessary to select from among the remaining ICD-10 translations. However, which alternative translation was selected would not have an impact on MS-DRG assignment, because the choices were among patient attributes that were not codable in ICD-9-CM; therefore, they were not used to assign patients to different MS-DRGs. Since the native ICD-10 MS-DRGs were constructed to replicate the native ICD-9-CM MS-DRGs, ICD-10 codes that differentiated patients based on attributes not contained in ICD-9-CM were all assigned to the same MS-DRG. For example, the operative approach used to reach the site of a procedure (e.g., open, percutaneous, etc.) is always specified in ICD-10, but rarely specified in ICD-9-CM. For an ICD-9-CM procedure code that lacked any specification of the operative approach, all the different ICD-10 operative approach codes for the corresponding procedure were assigned to the same ICD-10 MS-DRG. Thus, which operative approach was selected for the ICD-10 translation of the procedure code did not affect MS-DRG assignment. Since under these circumstances the selection from among alternative translations would have no impact on MS-DRG assignment, the final translation for the code was selected randomly from among the remaining possible translations using a uniform probability distribution. Approximately 19 percent of the code translations required a random selection from among residual possible ICD-10 translations.
Simulating Payments
Version 27 of the MS-DRGs was independently assigned to the FY 2009 MedPAR data three times as follows:
The ICD-9-CM MS-DRG grouper was used to assign the MS-DRGs to the source ICD-9-CM MedPAR data.
The ICD-10 MS-DRG grouper was used to assign the MS-DRG to the ICD-10 version of the MedPAR data.
The ICD-10 version of the MedPAR data was then mapped back to ICD-9-CM codes using the Reimbursement Map. The ICD-9-CM MS-DRG grouper was then used to assign the MS-DRGs to this mapped version of the MedPAR data.
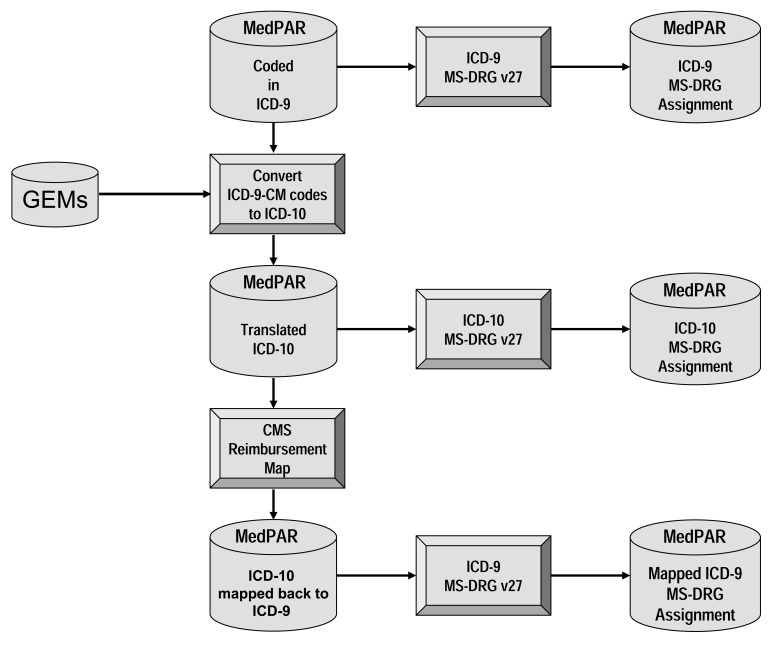
For brevity, the three different MS-DRG groupings of the FY 2009 MedPAR data will be referred to as native ICD-9-CM, native ICD-10, and mapped ICD-9-CM, respectively. Figure 1 summarizes the process of obtaining the three different MS-DRG assignments.
Figure 1. Overview of process of assigning MS-DRGs to the MedPAR data.
Inlier and outlier payments were calculated for each claim in the MedPAR data using FY 2010 Medicare payment rules for operating and capital payment, including wage index, disproportionate share hospital (DSH), and indirect medical education (IME) adjustments. A fixed loss threshold of $20,185 from the FY 2009 final rule was used to calculate additional outlier payments.
The payment calculation was applied to acute care hospitals falling under the Medicare IPPS, including hospitals in Puerto Rico. Non-IPPS hospitals were removed from the database, including skilled nursing facilities, long-term care hospitals, rehabilitation hospitals, psychiatric hospitals, critical access hospitals, children's hospitals, and oncology hospitals. Further, hospitals that had insufficient or inaccurate cost report information, or with missing IME or DSH adjustment factors, were also excluded from the database. Cases from IPPS hospitals in stand-alone units were also excluded. The final analysis database contained 3,383 short-term acute hospitals representing 10,934,386 Medicare discharges.
Results
The results of the payment impact analysis are contained in Table 1. Relative to the native ICD-9-CM MS-DRGs, the native ICD-10 MS-DRGs assigned 1.68 percent of the patients to a different MS-DRG. The change in MS-DRG assignment was relatively consistent across hospital types with rural hospitals having the smallest change in MS-DRG assignment (1.56 percent), and the 10 percent of hospitals with the biggest indirect medical education adjustment having the largest change in MS-DRG assignment (1.97 percent). Mapping the data back, and using the native ICD-9-CM MS-DRGs, significantly increased the percent of patients assigned to a different MS-DRG to 3.66 percent. The change in MS-DRG assignment, due to the mapping of ICD-10 data back to ICD-9-CM, was relatively consistent across hospital types, with rural hospitals having the smallest change in MS-DRG assignment (2.92 percent) and the top 10 percent of hospitals by bed size having the largest change in MS-DRG assignment (4.00 percent).
Table 1. Payment Impact Redistribution based on MedPAR FY 2009 data.
| Native ICD-10 versus Native ICD-9-CM | Mapped ICD-10 versus Native ICD-9-CM | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Hospital Type | Count Hospitals | Count Discharges | Tot Pay ($000,000) | % Diff MS-DRG | % Diff Payment | % Diff MS-DRG | % Diff Payment |
| All | 3,383 | 10,934,355 | 118,964 | 1.68 | 0.05 | 3.66 | -0.34 |
| IME1 | |||||||
| Top 10% | 102 | 618,479 | 11,403 | 1.97 | 0.18 | 3.85 | -0.14 |
| All others | 3,281 | 10,315,876 | 107,562 | 1.66 | 0.04 | 3.65 | -0.36 |
| DSH2 | |||||||
| Top 20% | 676 | 2,585,777 | 35,555 | 1.79 | 0.07 | 3.79 | -0.25 |
| Middle 60% | 2,031 | 6,306,899 | 63,944 | 1.66 | 0.04 | 3.59 | -0.35 |
| Bottom 20% | 676 | 2,041,679 | 19,465 | 1.59 | 0.05 | 3.72 | -0.46 |
| Location | |||||||
| Large Urban | 1,336 | 5,268,485 | 63,292 | 1.69 | 0.07 | 3.75 | -0.31 |
| Other Urban | 1,093 | 4,150,768 | 44,300 | 1.71 | 0.04 | 3.82 | -0.38 |
| Rural | 954 | 1,515,102 | 11,372 | 1.56 | -0.01 | 2.92 | -0.35 |
| Size | |||||||
| Top 10% | 338 | 3,538,531 | 44,150 | 1.73 | 0.08 | 4.00 | -0.33 |
| All other | 3,045 | 7,395,824 | 74,814 | 1.66 | 0.04 | 3.50 | -0.35 |
IME = Indirect Medical Education
DSH = Disproportionate Share Hospital
Overall the native ICD-10 MS-DRGs relative to the native ICD-9-CM MS-DRGs increased hospital payments by 0.05 percent. Thus, payment increases and decreases due to a change in DRG assignment essentially netted out. The change in payment was relatively consistent across hospital types, with rural hospitals having a 0.01 percent decrease in payment and the 10 percent of hospitals with the biggest indirect medical education adjustment having a 0.18 percent payment increase. Mapping the ICD-10 data back to ICD-9-CM and using the native ICD-9-CM MS-DRGs resulted in an overall payment decrease of 0.34 percent. Thus, mapping the data back, on average, caused patients to be assigned to lower paying MS-DRGs. The decrease in payment, due to the mapping, was relatively consistent across hospital types, with the top 10 percent of hospitals with the highest indirect medical education adjustment having the smallest payment decrease (0.14 percent), and the 20 percent of hospitals with the lowest disproportionate share adjustment having the largest payment decrease (0.46 percent).
Discussion
The results of the payment impact analysis show that the conversion to a native ICD-10 version of MS-DRGs will have a minimal impact on aggregate payments to hospitals and the distribution of payments across hospitals. However, it should be noted that the aggregate payment impact estimate does not reflect changes in hospital coding practices that could occur with the implementation of ICD-10. The objective of the ICD-10 MS-DRG conversion project was to produce an ICD-10 version of MS-DRGs that replicated the ICD-9-CM version. Thus, for data coded in ICD-10, the MS-DRGs would assign “the same MS-DRG had the same case been coded using ICD-9-CM codes” (CMS, 2010d). The development of a complete, native, ICD-10 version of the MS-DRGs allowed ICD-10 codes to be evaluated on an individual basis to determine the most appropriate assignment. As a result, there is a high degree of consistency between the ICD-9-CM and ICD-10 version of the MS-DRGs.
Mapping ICD-10 data back to ICD-9-CM and using the ICD-9-CM version of MS-DRGs produced a greater impact on aggregate payments to hospitals and the distribution of payments across hospitals. Any mapping will inherently produce less consistent results, because a single choice between mapping alternatives is uniformly applied across all DRGs, whereas in a native conversion, context specific judgment can be used to independently assign translation alternatives on a DRG-by-DRG basis. The Reimbursement Map used in this analysis was biased for inpatient care. The ICD-10 to ICD-9-CM code maps were selected based on inpatient code frequency data, in the five percent of mappings where there were multiple ICD-9-CM map alternatives, and were not necessarily the closest map in terms of meaning. Thus, the use of the Reimbursement Map could be problematic if applied to convert ICD-10 data to ICD-9-CM for use with other types of ICD-9-CM based applications, such as outpatient systems.
The ICD-10 MS-DRGs replicate the ICD-9-CM MS-DRGs. As such, they do not take advantage of the increased specificity of ICD-10. If the ICD-10 MS-DRGs had been optimized for ICD-10, there could have been a substantial shift of patients across MS-DRGs that would make them inconsistent with the existing MS-DRG payment weights. Since there is no substantial database available in ICD-10, there is no way of recalibrating the MS-DRG payment weights to correspond to ICD-10 optimized MS-DRGs. The converted ICD-10 database developed for this project created an ICD-10 database with records coded in ICD-10, but at a level of specificity corresponding to ICD-9-CM. In other words, the records were coded in ICD-10 based on only the information that was available within ICD-9-CM.When additional information was required to complete the ICD-10 coding, it was inferred by randomly selecting from among the alternative possibilities. Such an approach is sufficient for the purpose of comparing the impact of replicated versions of MS-DRGs, because the additional information needed for ICD-10 coding would not be expected to impact the MS-DRG assignment of the replicated versions. However, such an approach could not be used as the basis for establishing payment weights of optimized ICD-10 MS-DRGs, because the additional information would be expected to impact the MS-DRG assignment of the ICD-10 optimized MS-DRGs. It can be anticipated that CMS will begin to optimize MS-DRGs for ICD-10 once ICD-10 coded data becomes available, allowing the MS-DRG payment weights to be simultaneously recalibrated.
There have been many misconceptions regarding the use of the GEMs. As a translation dictionary, the GEMs provide a starting point for the conversion of ICD-9-CM based applications to a native ICD-10 version of the application. This is how the GEMs were used to create the ICD-10 MS-DRGs. Any attempt to use the GEMs to map ICD-9-CM data to ICD-10 data, as opposed to converting an application to a native ICD-10 version, is extremely problematic. The use of the GEMs to convert ICD-9-CM coded patient records to ICD-10 for this project was possible only because of two special circumstances: First, the use of the converted data was strictly limited to the testing of a replicated ICD-10 application in which the additional specificity of ICD-10 was not utilized. Second, only the aggregate financial impact results were evaluated. Because a large sample size of nearly 11 million records was used in the analysis, a reliable aggregate estimate of financial impact could be obtained, even though a random selection from among equally plausible ICD-10 alternatives was sometimes necessary in order to convert an individual record. Except in these very narrow circumstances, it is not possible to reliably convert an ICD-9-CM database that corresponds to the full specificity of ICD-10, because the necessary information is simply not available in ICD-9-CM.
Another misconception is that the GEMs can be used to create a single universal mapping that can be used to map input ICD-10 data to ICD-9-CM, allowing existing ICD-9-CM applications to continue to be used. As evidenced by the Reimbursement Map, the GEMs can be used to create an ICD-10 to ICD-9-CM map. However, the Reimbursement Map was developed largely using inpatient MedPAR data. For other applications, the mapping choices could have differed (e.g., mapping choices can be quite different for an inpatient versus outpatient application). Thus, a universal map is not feasible without a potential loss of accuracy for some applications. The results obtained in this study for MS-DRGs using the Reimbursement Map are best case results. If a specific ICD-10 to ICD-9-CM map developed for another purpose, had been used, it is highly likely that the impact on aggregate payments to hospitals, and the distribution of payments across hospitals, would have been substantially greater.
To illustrate the problem with using a map, the All Patient Refined DRGs (APR DRGs) were assigned to the ICD-9-CM data, then reassigned using the converted ICD-10 data mapped back. APR DRGs contain a detailed four level definition of severity of illness, and are widely used in comparative public reports and in Medicaid and commercial payer payment systems (Averill, Goldfield, Muldoon, Steinbeck, Grant, 2002). Mapping ICD-10 data back to ICD-9-CM and reassigning the APR DRG resulted in 4.90 percent of the patients being assigned to a different APR DRG. The increased number of patients with a different APR DRG assignment is likely the result of the use of a map that was not tailored to APR DRGs. If the mapping had been developed specifically for APR DRGs, the number of patients assigned to a different APR DRG would likely have been lower. However, as with MS-DRGs, the primary reason a mapping produces less consistent results is because a single choice among mapping alternatives is uniformly applied across all DRGs, instead of being evaluated on a DRG-by-DRG basis.
If payers do not convert their core payment and claims adjudication systems to native ICD-10 versions, and instead use an ICD-10 to ICD-9-CM mapping in order to continue to use their existing ICD-9-CM based systems, there are potential biases and unintended results of such an approach. This is especially true if a payer attempts to use a single uniform mapping across all systems. Fortunately, as evidenced by the development of the native ICD-10 version of the MS-DRGs, CMS appears to be moving toward creating native ICD-10 versions of its systems, instead of mapping ICD-10 data to ICD-9-CM and continuing to use ICD-9-CM based systems.
Conclusions
The transition from the ICD-9-CM version of the MS-DRGs to the ICD-10 version of the MS-DRGs will have a minimal impact on aggregate payments to hospitals (+0.05 percent) and on the distribution of payments across hospital types (-0.01 to +0.18 percent). Mapping ICD-10 data back to ICD-9-CM, and using the ICD-9-CM version of MS-DRGs, would have a modest impact on aggregate payments to hospitals (-0.34 percent) and the distribution of payments across hospital types (-0.14 to -0.46 percent). Although the transition from the ICD-9-CM version of the MS-DRGs to the ICD-10 version resulted in 1.68 percent of the patients being assigned to different MS-DRGs, payment increases and decreases due to a change in DRG assignment essentially netted out. Since the GEMs were used as the basis for creating the ICD-10 version of the MS-DRGs, the consistency achieved between the ICD-9-CM and ICD-10 MS-DRGs demonstrates that the GEMs can provide an effective basis for converting ICD-9-CM based applications to ICD-10.
Mapping ICD-10 data back to ICD-9-CM, and using the ICD-9-CM version, resulted in 3.66 percent of the patients being assigned to different MS-DRGs, with a bias toward lower paying MS-DRGs as evidenced by an overall 0.34 percent payment decrease. The bias was present even though the Reimbursement Map was developed relying on Medicare inpatient patient data. Applying the Reimbursement Map to the APR DRGs resulted in 4.90 percent of patients changing APR DRGs, demonstrating that the use of a map that is not tailored to the specific application will produce less consistent results. As demonstrated by MS-DRGs, a native ICD-10 version of an application can produce consistent results with the ICD-9-CM version of the application. However, the use of mappings will produce less consistent results, especially if the mapping is not tailored to the specific application.
References
- Averill RF, Goldfield NI, Muldoon J, Steinbeck BA, Grant TM. A Closer Look at All-Patient Refined DRGs. Journa l of AHIMA / American Health Information Management Association. 2002 Jan;73(1):46–50. [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services (CMS) ICD-10-CM/PCS MS-DRGv26 Definitions Manual Table of Contents. 2010a Retrieved from http://www.cms.gov/ICD10/17_ICD10_MS_DRG_Conversion_Project.asp.
- Centers for Medicare and Medicaid Services (CMS) 2010 Mapping. 2010b Retrieved from http://www.cms.gov/ICD10/13_2010_ICD10PCS.asp. [PubMed]
- Centers for Medicare and Medicaid Services (CMS) 2010 ICD-10-CM a nd GEMs. 2010 ICD-10-PCS and GEMs. 2010c Retrieved from http://www.cms.gov/ICD10/01_Overview.asp.
- Centers for Medicare and Medicaid Services (CMS) Converting MS-DRGs 26.0 to ICD-10-CM and ICD-10-PCS. 2010d Retrieved from http://www.cms.gov/ICD10/17_ICD10_MS_DRG_Conversion_Project. [PubMed]