Abstract
Objective
The primary objective was to estimate the burden of invasive pneumococcal disease (IPD) in children aged 1 month to 12 years in South Asian countries.
Methods
We searched three electronic databases (PubMed, Embase and the Cochrane Library) using a comprehensive search strategy, we manually searched published databases (Index Medicus and Current Contents) and we also searched the bibliographies of the included studies and retrieved reviews. The searches were current through June 2013. Eligible studies (community-based and hospital-based) were pooled and a separate analysis for India was also completed. A meta-regression analysis and heterogeneity analysis were performed. The protocol was registered with PROSPERO registration number CRD42013004483.
Results
A total of 22 studies surveying 36,714 children were included in the systematic review. Hospital-based prospective studies from South Asia showed that 3.57% of children had IPD, and 15% of all bacterial pneumonia cases were due to Streptococcus pneumoniae. Indian studies showed that the incidence of IPD was 10.58% in children admitted to hospitals with suspected invasive bacterial diseases, and 24% of all bacterial pneumonia cases were due to S. pneumonia. Population-based studies from South Asian countries showed that 12.8% of confirmed invasive bacterial diseases were caused by S. pneumonia whereas retrospective hospital-based studies showed that 28% of invasive bacterial diseases were due to S. pneumoniae. Meta-regression showed that there was a significant influence of the antigen testing method for diagnosing IPD on IPD prevalence.
Conclusion
S. pneumoniae is responsible for a substantial bacterial disease burden in children of South Asian countries including India despite the presence of high heterogeneity in this meta-analysis. Treatment guidelines must be formulated, and preventive measures like vaccines must also be considered.
Introduction
Worldwide, pneumonia is the leading infectious cause of mortality in children under five years of age [1]. Besides pneumonia, meningitis and sepsis are also amongst the top killers of children in the world [1]. World Health Organization (WHO) estimates have shown that more than 90% of all deaths due to pneumonia in children under the age of five occur in 40 countries. The most deaths caused by pneumonia occur in India, with Pakistan, Bangladesh and Afghanistan following close behind [2]. Morris et al. predicted that the mortality rates of children under five years of age attributable to pneumonia are similar in Sub-Saharan Africa and South Asia [3].
According to estimates, more than half of the new cases of clinical pneumonia are concentrated in five countries, three of which are in South Asia, i.e., India, Bangladesh and Pakistan [4]. This core of South Asian countries has a high incidence of clinical pneumonia, with India having the highest number of new cases detected worldwide. The mortality rates for children under five years of age in the South Asian region ranges from 17/1000 for Sri Lanka to 149/1000 for Afghanistan. Pneumonia claims the lives of 11% of children under the age of five in India, the Maldives, Bangladesh and Pakistan, 23% in Afghanistan, 19% in Bhutan and 6% in Sri Lanka [5].
Modern evidence on the aetiology of pneumonia is based on two types of studies. The first type is hospital-based prospective studies, which rely on culture methods, and the second type is vaccine trials, which measure the reduction in the burden of a disease by specific vaccines against the disease [6], [7]. Both types of studies have found Streptococcus pneumoniae to be the leading cause of pneumonia. S. pneumoniae is an encapsulated diplococcus with over 90 known capsular serotypes. It causes a wide spectrum of diseases ranging from fatal invasive diseases like pneumonia, meningitis and sepsis to noninvasive diseases like otitis media and sinusitis [8]. S. pneumoniae affects both extremes of age, i.e., children and the elderly. South Asian countries have the highest incidence of mortality due to invasive pneumococcal disease (IPD) [8]. Moreover, S. pneumoniae infections are the leading vaccine preventable causes of mortality in children under the age of five worldwide [8].
Although vaccines against S. pneumoniae are available in South Asian countries, the majority have not included them in their respective immunization schedules. This omission is due to the paucity of data available on the burden of pneumococcal diseases and the lack of information on the prevalent S. pneumoniae serotypes in this region. Hence, this systematic review was conducted to provide these data.
Objectives
The primary objective of this systematic review is to determine the pneumococcal disease burden in children aged 1 month to 12 years in South Asian countries. These data can help policymakers make decisions regarding the need for including pneumococcal vaccines in national immunization schedules.
Methods
Inclusion Criteria
1 Published Studies: prospective or retrospective studies that included children aged 1 month to 12 years from South Asian countries.
2 Isolation of S. pneumoniae from included subjects.
3 Minimum 12 months of surveillance.
Two authors decided upon the inclusion of studies, and others performed quality assessment. Discrepancies, if any, were resolved by discussion.
If the required data were not available, we contacted the authors and attempted to retrieve the missing data. Studies that commented only on pneumococcal serotypes and/or antibiotic resistance were excluded from the pooled analysis. We excluded case reports, editorials, vaccine studies, literature reviews and studies in which nasopharyngeal aspirates, throat swabs or oropharyngeal swabs were the only samples used to determine the causative organism.
Literature Search
We performed a systematic search of the published literature and also tried to acquire unpublished data from various investigators of the region. The searches were current as of June 2013. We identified articles with information on IPD amongst children aged 1 month to 12 years. We searched three databases: Medline via Ovid and PubMed, Embase and The Cochrane Library. The reference lists of the obtained articles were further searched for additional studies. Published databases (Index Medicus and Current Contents) were also manually searched. Non-English articles were not included. The search details are given in Appendix S1. Searching was performed independently by two authors.
General Definitions
South Asia includes Afghanistan, Pakistan, India, Nepal, Bhutan, Bangladesh, Sri Lanka and the Maldives.
Burden of pneumococcal disease: We defined the burden of pneumococcal disease as the number of positive pneumococcal isolates from the suspected population (children aged 1 month to 12 years).
Hospital Based Surveillance Studies are those, which involve monitoring a disease at a single facility or small number of facilities.
Population Based Surveillance Studies are those, which involve identifying all new cases of the disease under surveillance in a defined population.
Disease Definitions
1 Pneumonia [9]
Symptoms: cough or difficult breathing. Signs: respiratory rate >50 breaths per minute for infants aged two months to less than one year, respiratory rate >40 breaths per minute for children aged one to five years, and no chest indrawing, stridor or danger signs.
2 Severe pneumonia [9]
Symptoms: cough or difficult breathing plus any general danger sign, chest indrawing or stridor in a calm child. General danger signs for children aged two months to five years include the inability to drink or breastfeed, vomiting, convulsions and lethargy or loss of consciousness.
-
3 Meningitis [9]
Suspected: Any person with sudden onset of fever and one of the following signs: neck stiffness, altered consciousness or other meningeal sign.
-
Probable: A suspected case with cerebrospinal fluid (CSF) examination showing at least one of the following:
turbid appearance;
leukocytosis (>100 cells/mm3);
leukocytosis (10–100 cells/mm3) and either elevated protein (>100 mg/dl) or decreased glucose (<40 mg/dl).
Confirmed: A case that is laboratory-confirmed by growing (i.e., culturing) or identifying (i.e., using antigen detection methods) a bacterial pathogen (pneumococcus) in the CSF or blood of a child with a clinical syndrome consistent with bacterial meningitis.
4 Nonpneumonia nonmeningitis
All infections other than pneumonia and meningitis were categorized under this heading.
5 Invasive pneumococcal disease
When pneumococcus is identified from one of the otherwise sterile sites of the body, such as blood, CSF or pleural fluid, either by culture, the latex agglutination test (LAT), polymerase chain reaction (PCR) or another technique.
Data Collection and Management
Four authors independently abstracted data from the included studies in a predesigned pro forma that included study design, setting, number of suspected cases, site for sample collection, number of samples collected for culture, number of cultures positive for pneumococcus and prior use of antibiotic. The data from hospital-based and population-based studies were abstracted separately. Authors were contacted to obtain missing data. To resolve discrepancies regarding the abstracted data, a consensus was drawn by discussion with the other reviewers. If discrepancies were not resolved, the data were not included in the pooled analysis.
Data Analysis
Data analysis was performed using STATA-MP 12, two-core, which is manufactured by Stata Corp., Ltd. Similar data from the studies were pooled for analysis. We calculated the proportion of pneumococcus isolated from the total bacterial isolates of the study population. The proportion of invasive pneumococcal disease from total suspected population was calculated using the total number of children with suspected invasive disease in the study as the denominator and for calculating the proportion of invasive pneumococcal disease from invasive bacterial disease the denominator used was the number of children with positive bacterial isolates either by culture or antigen testing. Additional analysis was performed to calculate the incidence of IPD in South Asian children less than 5 years of age and in Indian children aged 1 month to 12 years. Subgroup analysis was performed for pneumonia and meningitis. Data from hospital-based prospective studies, hospital-based retrospective studies and community-based studies were analysed separately. We calculated I2, Tau2 and the Z test for heterogeneity amongst the studies, and the Galbraith plot was used to represent the heterogeneity. To analyse publication bias, Begg's test, Kendall's score, Egger's linear regression and the funnel plot were used.
Results
Data Reviewed
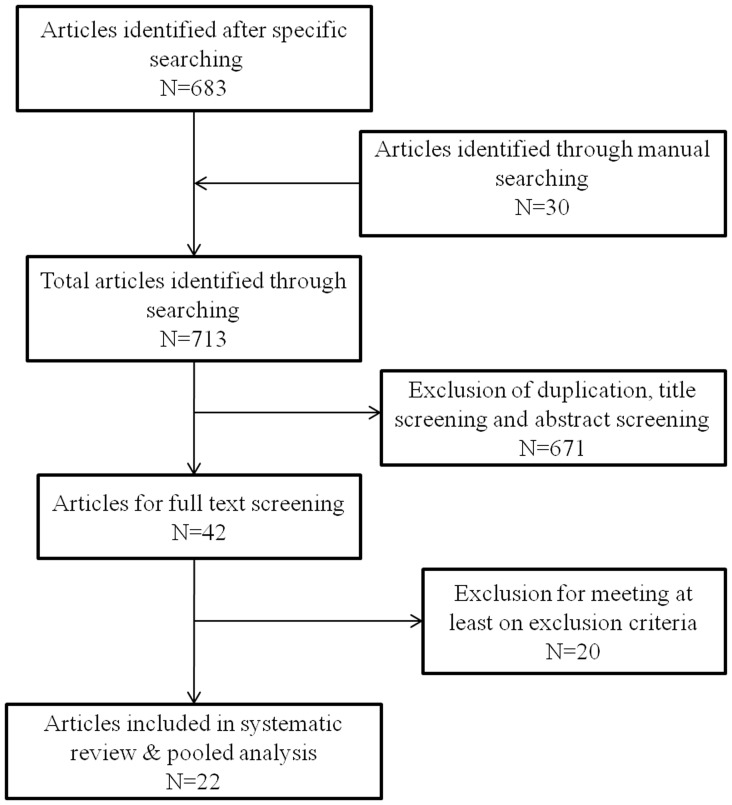
We found 713 published articles through electronic and manual searches. After screening the titles and abstracts, 42 full-text articles were retrieved, of which 22 studies fulfilled the inclusion criteria and were included in the analysis (Figure 1, Table 1) [10]–[31]. Twenty studies were excluded from the systematic review [32]–[51], as shown in Table 2. The total number of children surveyed was 36,714. Of these subjects, 2,539 children were confirmed to have a bacterial disease. A total of 663 children less than 12 years of age were confirmed to have IPD. A detailed analysis of each study type was completed separately and is described below.
Figure 1. Flow diagram of search results.
Table 1. Characteristics of included studies.
| Serial no. | Country (ref) | Setting | Study year | Duration (months) | Syndromes/diseases studied | Diagnostic method | Prior antibiotic usage | Population (age) | Number of positive bacterial growth | Number of cases with S. pneumoniae |
| 1 | India [10] | Hospital based prospective study | Sep'78–Feb'81 | 29 | Meningitis | CSF gram stain, culture & CIEP | Reported prior antibiotic usage | 70 (<15 years) | 29 | 13 |
| 2 | India [11] | Hospital based prospective study | Feb'85–Dec'87 | 23 | Pneumonia | Blood culture | Did not report prior antibiotic usage | 331 (<6 years) | 28 | 8 |
| 3 | India [12] | Hospital based prospective study | Jan'89–Apr'90 | 16 | Meningitis | CSF culture, Gram stain and LAT | Did not report prior antibiotic usage | 114 (2 mth-11 yr) | 55 | 15 |
| 4 | India [13] | Hospital based prospective study | Sep'88–Aug'89 | 12 | Pneumonia | Blood culture, Throat swab and NPA culture | Did not report prior antibiotic usage | 132 (<12 years) | 34 | 13 |
| 5 | India [14] | Hospital based prospective study | 1993–1997 | 48 | Pneumonia, Meningitis, Septicemia | Blood culture and CSF culture | Reported prior antibiotic usage | 5738 (<12 yrs) | N.A. | 156 |
| 6 | India [15] | Hospital based prospective study | Sep'94–Apr'96 | 20 | Meningitis | CSF culture, cel count, biochemistry and LAT | Reported prior antibiotic use | 100 (1mth – 12 yrs) | 35 | 12 |
| 7 | India [16] | Hospital based prospective study | Mar'95–Feb'97 | 24 | Pneumonia | Blood culture, Throat swab and NPA culture | Did not report prior antibiotic usage | 95 (2mths - 5 yrs) | 15 | 5 |
| 8 | India [17] | Hospital based prospective study | Jul'00–Jul'01 | 12 | Meningitis | CSF culture | Reported prior antibiotic use | 150 (<12 yrs.) | 40 | 6 |
| 9 | Bangladesh [18] | Population based prospective study | 1999–2001 | 24 | Pneumonia | Blood culture | Did not report prior antibiotic usage | 18,983 (<5 years) | 331(840) | 7 |
| 10 | Bangladesh [19] | Population based prospective study | 2004–2006 | 24 | Severe Pneumonia | Blood culture | Did not report prior antibiotic usage | 6167 (<5 years) | 315(5949) | 34 |
| 11 | India [20] | Hospital Based retrospective study | Jan'96–Dec'05 | 120 | Meningitis | Records, CSF culture & LAT | Did not report prior antibiotic usage | 51 (<12 years) | 40 | 28 |
| 12 | India [21] | Hospital based prospective study | Feb'03–Jan'07 | 48 | Meningitis | CSF culture & LAT | Reported prior antibiotic use | 535 (<5 years) | 214 | 94 |
| 13 | Bangladesh [22] | Population based prospective study | Jul'04–Jun'07 | 36 | Pneumonia, Meningitis, Septicemia | Blood & CSF culture | Did not report prior antibiotic usage | 6966 (<5 years) | 93 | 26 |
| 14 | Srilanka [23] | Hospital based prospective study | Jan'05–Mar'07 | 27 | Pneumonia, Meningitis, Septicemia | Blood & CSF culture | Reported prior antibiotic use | 3642 (<5 years) | 585 | 37 |
| 15 | Bangladesh [24] | Hospital based prospective study | May'04–Apr'07 | 36 | Pneumonia | Blood culture | Reported prior antibiotic use | 4155 (<5 years) | 161 | 10 |
| 16 | Nepal [25] | Hospital based prospective study | Apr'05–Dec'06 | 21 | Pneumonia, Meningitis, Septicemia | Blood & CSF cultures | Reported prior antibiotic use | 885 (<5 years) | 47 | 17 |
| 17 | Nepal [26] | Hospital based prospective study | Nov'04–Mar'07 | 29 | Pneumonia, Meningitis, Septicemia | Blood & CSF cultures | Reported prior antibiotic use | 2529 (<5 years) | 276 | 51 |
| 18 | India [27] | Hospital Based retrospective study | Jan'06–Dec'06 | 12 | Pneumonia, Meningitis, Septicemia | Records | Did not report prior antibiotic usage | 2219 (<5 years) | N.A. | 61 |
| 19 | Pakistan [28] | Hospital based prospective study | May'05–Apr'06 | 12 | Meningitis | CSF culture | Reported prior antibiotic use | 2690 (<5 years) | 83 | 32 |
| 20 | Pakistan [29] | Population based prospective study | 2007–2008 | 15 | Pneumonia | Blood cultures | Did not report prior antibiotic usage | 5570 (<5 years) | 36(1147) | 1 |
| 21 | Nepal [30] | Hospital based prospective study | Apr'05–Dec'06 | 21 | Pneumonia, Meningitis, Septicemia | Blood and CSF culture | Reported prior antibiotic use | 2039 (<12 years) | 151 | 36 |
| 22 | India [31] | Hospital based prospective study | Sep'91–Jul'92 | 12 | Pneumonia | Blood culture, LAT | Reported prior antibiotic use | 110 (<5 years) | 62 | 32 |
Table 2. Characteristics of excluded studies.
| S. no | Study name | Comments |
| 1. | Patwari et al, 1988 [46] | No available data on causative organism |
| 2. | Mastro et al 1991 [41] | Antibiotic resistance only |
| 3. | Mastro et al,1993 [42] | Study period is <1 year, Nasopharyngeal aspirates only |
| 4. | Awasthi et al 1997 [35] | No data on S. pneumoniae |
| 5. | Saha et al 1997 [48] | Serotype details only |
| 6. | Saha et al 1999 [49] | Mentions about antibiotic resistance only |
| 7. | Jebaraj et al 1999 [40] | Nasopharyngeal colonization study |
| 8. | Addo-Yobo et al 2004 [50] | Randomized controlled trial, has mixed data of Asia and Africa and South America also |
| 9. | Acharya et al 2003 [32] | Does not report for S. pneumoniae |
| 10. | Mehta et al,2003 [44] | Tells about Antibiotic resistance only does not give the details of S. pneumoniae and other causative organism |
| 11. | Bansal et al, 2006 [36] | Not reported S. pneumoniae so cannot be included |
| 12. | Bharti et al, 2006 [38] | No information on S. pneumoniae |
| 13. | Hussain et al 2006 [39] | Cost of treatment study |
| 14. | Nizami et al 2006 [45] | Oropharyngeal aspirate only |
| 15. | SPEAR study 2008 [34] | Study does tell only about India but has included other regions which are not a part of South Asia, Randomized Control Trial |
| 16. | Agarwal et al, 2009 [33] | Short report; No data for S. pneumoniae |
| 17. | Saha et al 2009 [51] | Serotype details only |
| 18. | Rijal et al 2010 [47] | Serotype details only |
| 19. | Mathisen et al 2010 [43] | Study on viruses |
| 20. | Bansal et al, 2004 [37] | Study of adults |
Hospital-based Prospective Studies
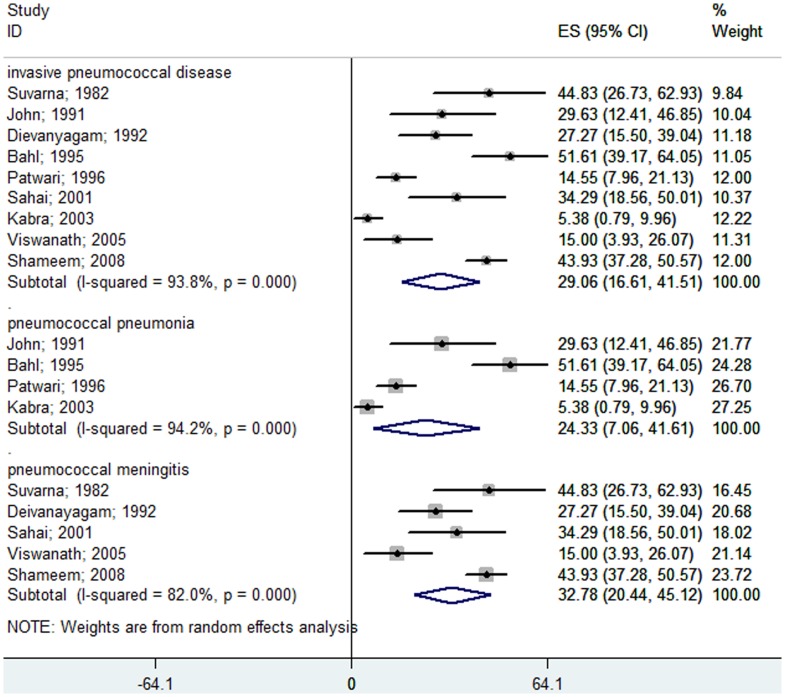
South Asian Countries: (children aged 1 month to 12 years)
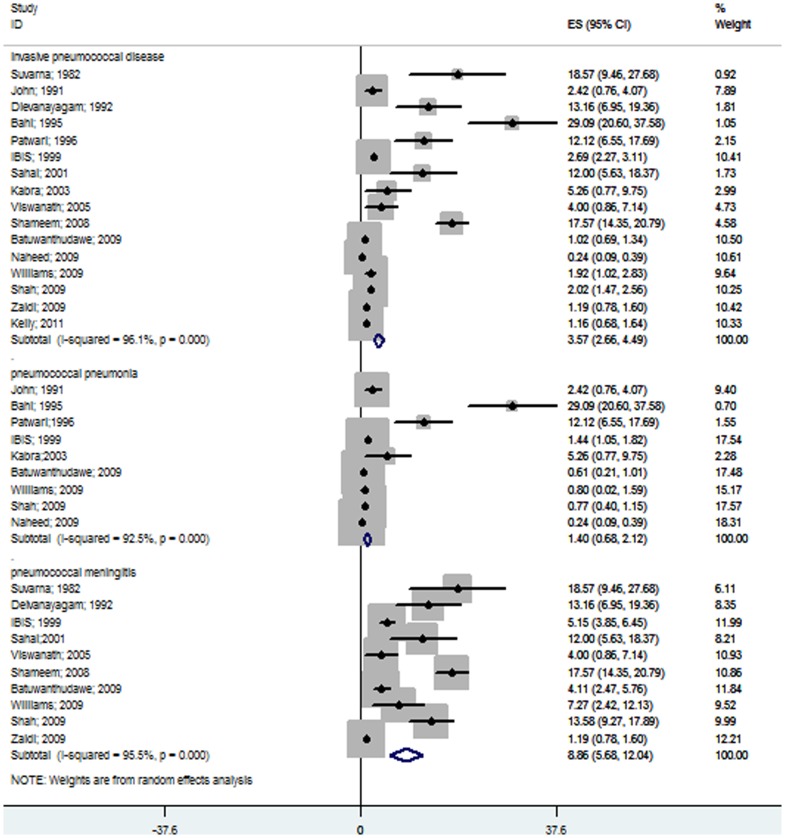
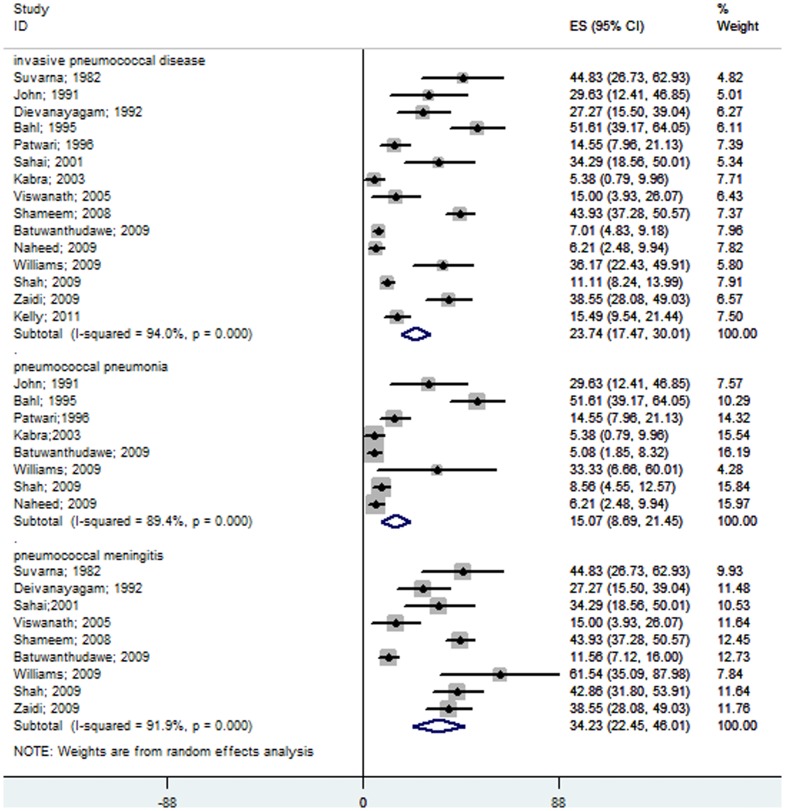
We identified sixteen hospital-based prospective studies from various South Asian countries [10]–[17], [21], [23]–[26], [28], [30], [31], and the pooled analysis using the random effects model showed that 3.57% (95% CI 2.66–4.49) of children admitted to hospitals with suspected invasive bacterial diseases were due to S. pneumoniae. Nine studies showed that only 1.4% (95% CI 0.68–2.12) of children admitted with severe pneumonia were due to pneumococcus (Figure 2) [11], [13], [14], [16], [23]–[26], [31]. Ten studies found that in 8.86% (95% CI 5.68–12.4) of children with probable or confirmed meningitis, S. pneumoniae was the causative organism (Figure 2) [10], [12], [14], [15], [17], [21], [23], [25], [26], [28]. Of the positive bacterial isolates from cases of invasive bacterial diseases, 23.74% (95% CI 17.47–30.01) were identified as S. pneumoniae by culture, LAT or PCR. Isolates from patients with severe pneumonia and pyogenic meningitis showed that 15.07% (95% CI 8.69–21.45) and 34.23% (95% CI 22.45–46.01) were due to S. pneumonia, respectively (Figure 3). Pneumococcus contributed insignificantly to all causes of pneumonia, but was still one of the leading causes of bacterial pneumonia as demonstrated by the meta-analysis.
Figure 2. Forest plot showing the proportion of IPD from hospital-based prospective studies on South Asian children aged 1 month to 12 years with suspected invasive bacterial disease.
The plot also shows the subgroup analysis for the pneumococcal pneumonia cases among all of the pneumonia patients and for the pneumococcal meningitis cases among all of the meningitis patients.
Figure 3. Forest plot showing the proportion of IPD from hospital-based prospective studies in South Asian children aged 1 month to 12 years with confirmed invasive bacterial disease.
The plot also shows a subgroup analysis for the pneumococcal pneumonia cases among all of the bacterial pneumonia patients and for the pneumococcal meningitis cases among all of the pyogenic meningitis patients.
South Asian Countries (Children <5 years of age)
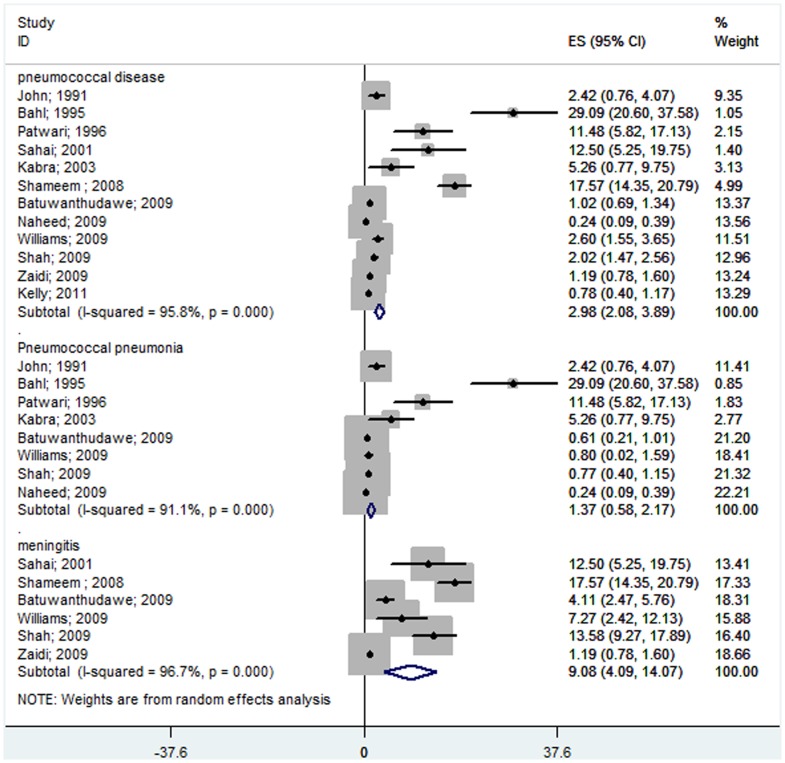
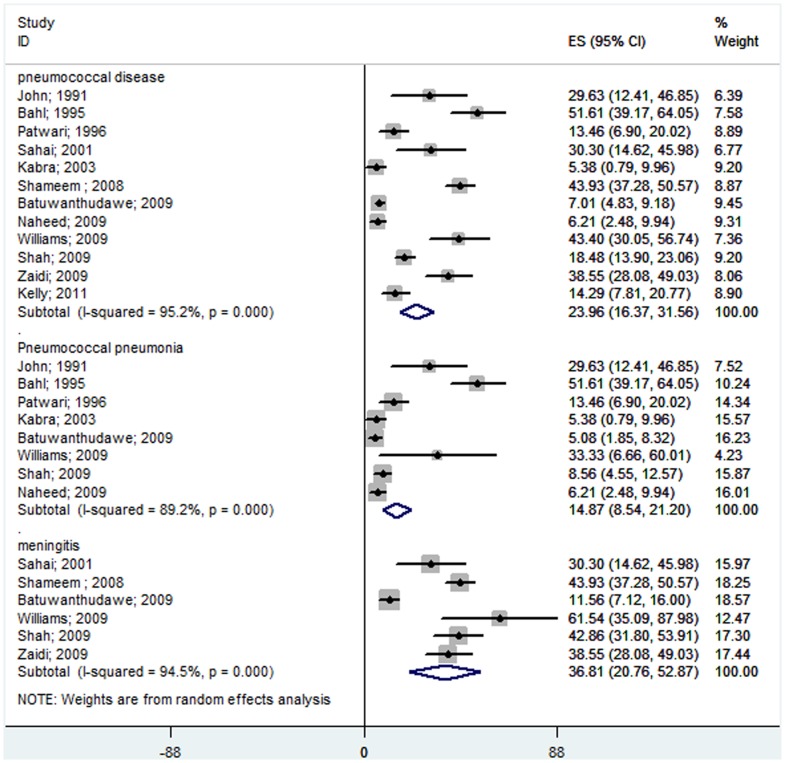
Of the 16 studies included, only 12 studies [11], [13], [15], [16], [21], [23]–[26], [28], [30], [31] published data on children less than 5 years of age. The meta-analysis showed that 2.98% (95% CI 2.08–3.89%) of children less than 5 years of age who were hospitalized with suspected invasive bacterial disease had S. pneumoniae infections. In South Asian children less than 5 years of age, the rate of pneumococcal pneumoniae was 1.37% (95% CI 0.58–2.17%) and the rate of pneumonia and pneumococcal meningitis of all causes was 9.08% (95% CI 4.09–14.07%) (Figure 4). In this age group, pneumococcus caused approximately 24% of all confirmed, invasive, bacterial diseases (Figure 5). Pneumococcal pneumonia was responsible for 14.87% (95% CI 8.54–21.20%) of all cases of bacterial pneumonia, and pneumococcal meningitis was responsible for 36.81% (95% CI 20.76–52.87%) of all cases of pyogenic meningitis (Figure 5).
Figure 4. Forest plot showing the proportion of IPD from hospital-based prospective studies in South Asian children under the age of 5 with suspected invasive bacterial disease.
The plot also shows a subgroup analysis for the pneumococcal pneumonia cases among all of the pneumonia patients and for the pneumococcal meningitis cases among all of the meningitis patients.
Figure 5. Forest plot showing the proportion of IPD from hospital-based prospective studies in South Asian children less than 5 years of age with confirmed invasive bacterial disease.
The plot also shows a subgroup analysis for the pneumococcal pneumonia cases among all the bacterial pneumonia patients and for the pneumococcal meningitis cases among all of the pyogenic meningitis patients.
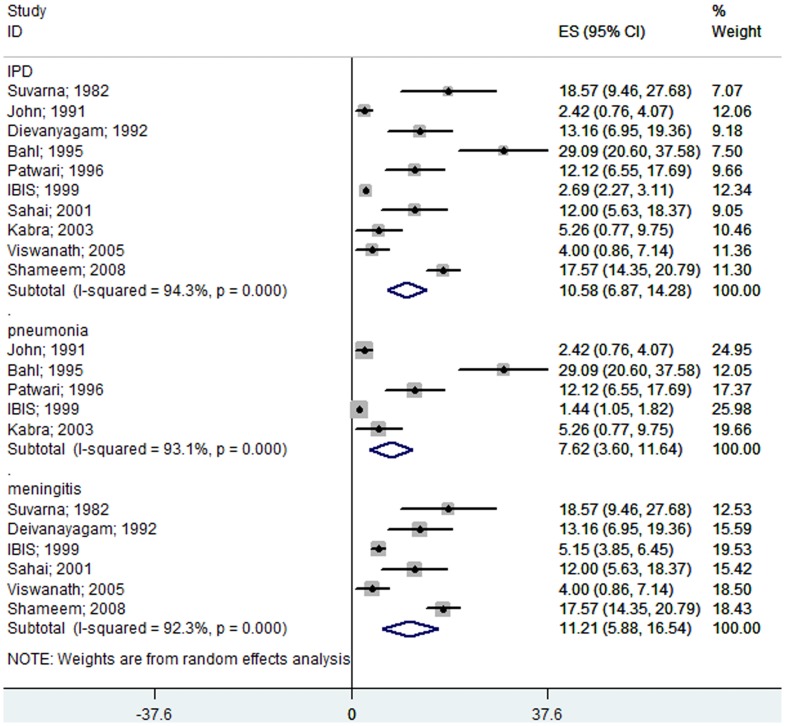
Hospital-based Studies (India)
Ten Indian studies [10]–[17], [21], [31] showed that S. pneumoniae causes 10.58% (95% CI 6.87–14.28) of invasive diseases, 7.62% (95% CI 3.6–11.64) of severe pneumonia cases, and 11.21% (95% CI 5.88–16.54) of meningitis cases in children with suspected bacterial diseases aged 1 month to 12 years (Figure 6). Streptococcus was a major bacterium isolated from severe pneumonia and pyogenic meningitis cases. S. pneumoniae was confirmed in 24.3% (95% CI 7.06–41.61) of bacterial isolates from pneumonia cases and in 32.78% (95% CI 20.44–45.12) of pyogenic meningitis cases (Figure 7).
Figure 6. Forest plot showing the proportion of IPD from hospital-based prospective studies in Indian children aged 1 month to 12 years with suspected invasive bacterial disease.
The plot also shows a subgroup analysis for the pneumococcal pneumonia cases among all of the pneumonia patients and for the pneumococcal meningitis cases among all of the meningitis patients.
Figure 7. Forest plot showing the proportion of IPD from hospital-based prospective studies in Indian children aged 1 month to 12 years with confirmed invasive bacterial disease.
The plot also shows a subgroup analysis for the pneumococcal pneumonia cases among all of the bacterial pneumonia patients and for the pneumococcal meningitis cases among all of the pyogenic meningitis patients
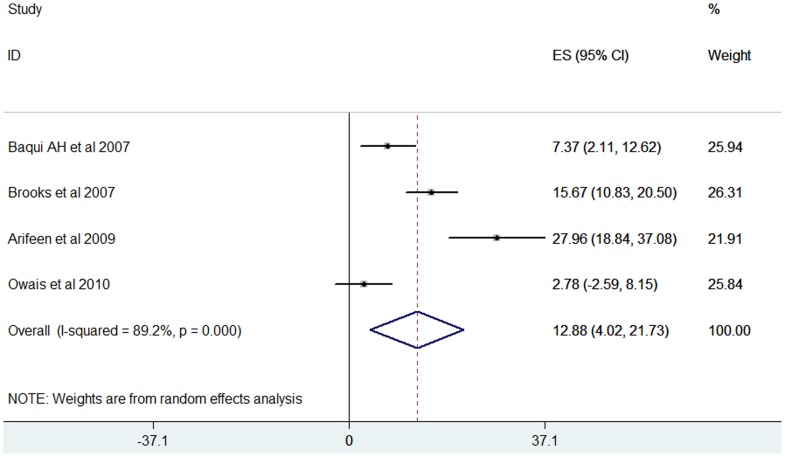
Population-based Studies
Four population-based, active surveillance studies from South Asian countries were included in the review [18], [19], [22], [29]. These studies were conducted in Pakistan and Bangladesh and only examined children less than 5 years of age. These studies showed that S. pneumoniae was present in 12.88% (95% CI 4.02–21.73) of all positive bacterial isolates (Figure 8).
Figure 8. Forest plot showing the proportion of IPD from population-based prospective studies in South Asian children aged 1 month to 12 years with suspected invasive bacterial disease.
Hospital-based Retrospective Studies
Two hospital-based retrospective studies from India were included in this review [20], [27]. The pooled data showed that S. pneumoniae was present in 28.36% (95% CI 22.74–79.46) of isolates from the total number of admitted patients with invasive bacterial diseases.
Meta-regression Analysis
Table 3 shows the results of the final model in which age (<5 years versus any age up to 12 years), setting (hospital versus community), diagnostic method (culture versus culture + LAT), study centre (multicentre versus single site) and organ system (clinical sepsis versus specific organ system) were estimated as random effects parameters. Associations between prevalence rates and predictors were assessed using the multivariate method including the predictors that were found to be significant in the univariate meta-regression. The odds of IPD were increased by 9% in studies using culture as well as LAT as diagnostic modalities when compared to studies using culture testing alone, and this association showed a trend toward significance (OR 1.09; 95% CI: 0.99–1.21). Similarly, the IPD prevalence was significantly lowered by 10% in studies where all suspected IPD cases involving any body organ were enrolled in comparison to studies where only subjects with pneumonia or meningitis (i.e., single organ involvement) were investigated (OR 0.90; 95% CI: 0.81–0.99) (Table 3)
Table 3. Univariate and multivariate meta-regression of IPD prevalence.
| Odds ratio# | 95% CI# | P value# | Odds ratio* | 95% CI* | P value* | |
| Age (<5 years vs. any age upto 12 years) | 0.93 | 0.82–1.06 | 0.271 | |||
| Surveillance setting (Hospital versus community), | 1.10 | 0.96–1.26 | 0.139 | |||
| Diagnostic testing method(Culture versus culture + LAT) | 1.11 | 0.99–1.24 | 0.066 | 1.09 | 0.99–1.21 | 0.083 |
| Study centre(Multicentric versus single site) | 0.97 | 0.86–1.10 | 0.630 | |||
| Organ system(Any clinical sepsis versus specific organ system alone) | 0.89 | 0.80–0.99 | 0.036 | 0.9 | 0.81–0.99 | 0.046 |
for univariate meta-regression; *for multivariate meta-regression.
Publication Bias
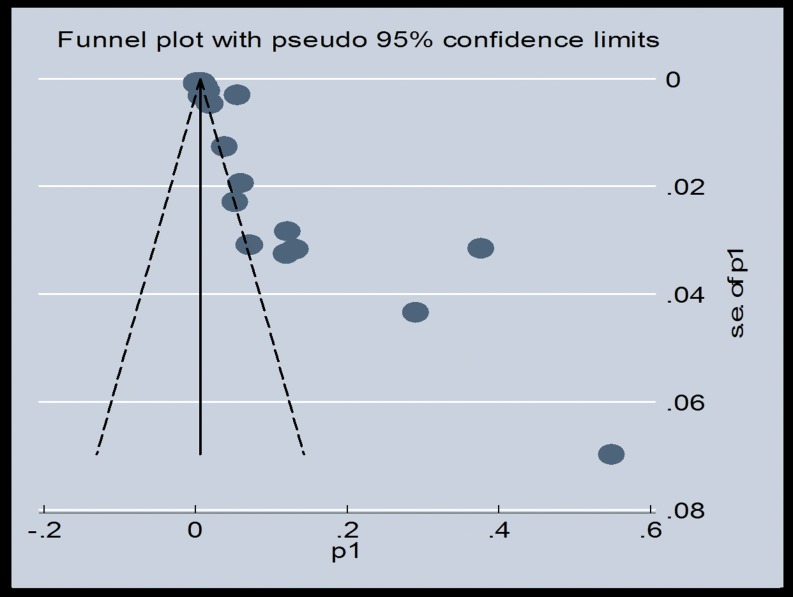
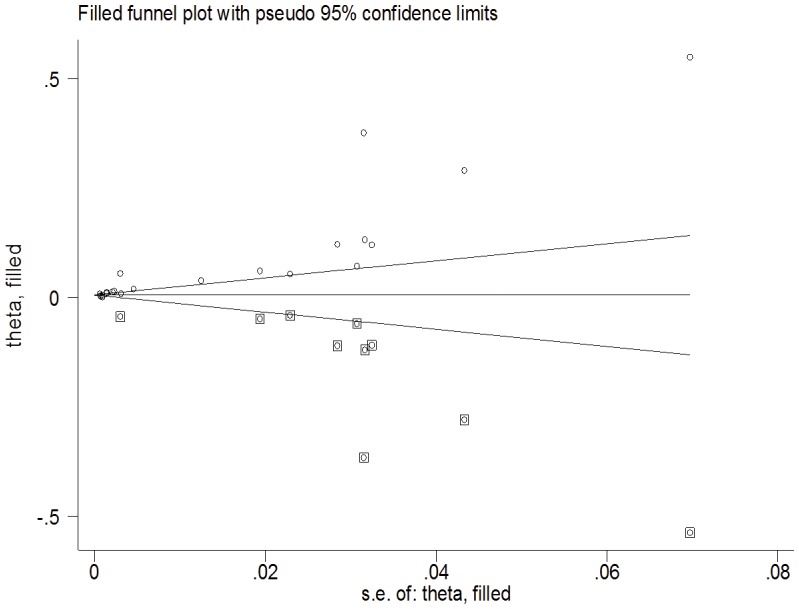
We used Begg's test to identify any publication bias in the review. A significant P-value of 0.003 in the above output of Kendall's tau by Begg's test indicates the presence of publication bias in this meta-analysis. However, Egger's linear regression test showed a nonsignificant coefficient (2.63) of publication bias (95% CI: −3.62 to 8.88) (P-value 0.39). We also used the funnel plot (Figure 9) to identify publication bias. The funnel plot was asymmetric and indicated that there were missing studies. Using the trim and fill method in our meta-analysis, it was shown that 10 studies were missing. Under the random-effects model, the point estimate and 95% CI for the pooled prevalence of the combined studies was 2% (1.5–2.5%), which was reduced to 0.09% (0.03–1.5%) using the trim and fill method (Figure 10).
Figure 9. Funnel plot showing the publication bias.
Figure 10. Corrected funnel plot using the trim and fill method.
Heterogeneity
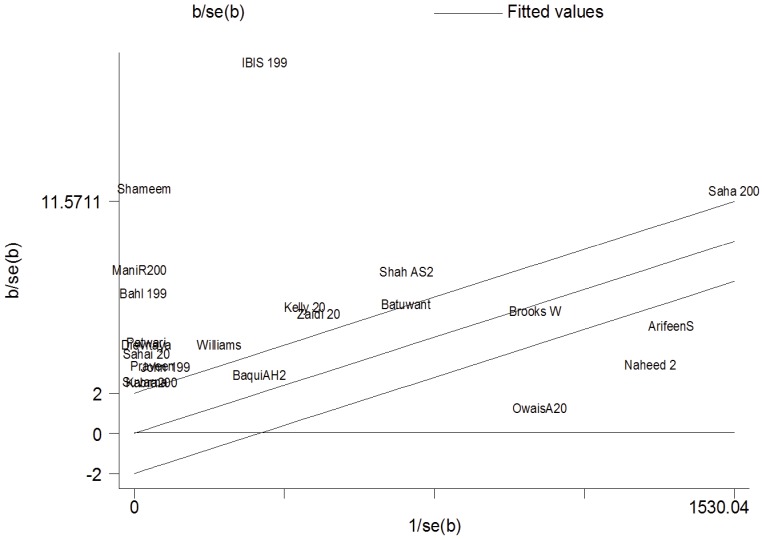
For each trial, the z statistic (effect size/standard error [SE] of effect size) was plotted against the reciprocal SE (1/SE) of the effect size. The unweighted regression line was constrained through the origin with its 95% CI, and it showed a slope equal to the overall pooled prevalence estimate in the fixed effects meta-analysis.
The position of each trial on the horizontal axis gives an indication of the weight allocated to it in the meta-analysis. The position on the vertical axis represents the contribution of each trial to the Q statistic for heterogeneity (Figure 11). The results of the I2 analysis and Tau2 analysis are shown in Table 4.
Figure 11. Galbraith plot showing heterogeneity.
Table 4. Heterogeneity analysis for hospital-based and population-based studies.
| Heterogeneity statistics | Degree of freedom | P | I-squared** | Tau-squared | z test | p value | |
| Hospital based | 617.12 | 16 | 0.000 | 97.4% | 0.0002 | 8.57 | 0.000 |
| Population based | 39.16 | 4 | 0.000 | 89.8% | 0.0000 | 3.51 | 0.000 |
| Overall | 684.91 | 21 | 0.000 | 96.9% | 0.0001 | 7.92 | 0.000 |
**I-squared: the variation in Effect Size attributable to heterogeneity.
Note: Between-group heterogeneity was not calculated. Significance test(s) of ES = 0.
Discussion
The meta-analysis showed that only 1.4% of all severe pneumonia cases in South Asia were due to pneumococcus, which contrasts with the results of other reviews. However, when we examined the bacterial isolates, pneumococcus had a significant contribution in severe pneumonia patients, and it is clearly a major bacterium responsible for severe pneumonia and meningitis. Although several other pathogens including viruses were detected, pneumococcus is an important pathogen that causes severe pneumonia and requires hospitalization.
In India, pneumococcus is a frequent cause of invasive bacterial diseases. It is a common bacterium isolated from children with severe bacterial pneumonia and children with pyogenic meningitis. This meta-analysis demonstrates that IPDs are more common in India than in other South Asian countries.
Although the results come from surveillance studies, which are not generally considered good quality evidence, the studies included in this review were characterized by quality, and they were based on a pretested questionnaire and were rated accordingly. Most of the hospital-based studies were from tertiary care centres where sick and referred patients are admitted, and overestimates are expected. Prior antibiotic use is also common in these patients, which alters the results. In this review, 12 studies reported prior antibiotic usage in 18% of children. This high rate of antibiotic use must have affected the isolation of the causative bacteria. Only the population-based studies from Bangladesh and Pakistan matched the inclusion criteria. Thus, the lack of population-based studies from other countries weakens this meta-analysis. The heterogeneity, due to the different sample sizes, age groups and syndromes investigated in the individual studies, was significant as estimated by the I2 and Tau2 tests, and thus, a random effects model was used [52].
This is the first systematic review of IPDs in South Asia. The meta-analysis showed that S. pneumoniae was the most common bacterium isolated. Though there was a difference in the figures obtained from hospital- and community-based studies, both types of studies reported a high number of cases with S. pneumoniae infections.
O' Brien et al. performed a global estimation of the IPD burden and found that India had the highest mortality due to IPD [8]. Rudan et al. showed that India had the highest number of new cases diagnosed worldwide [4]. Johnson et al. tried to determine the most prevalent pneumococcal serotypes globally and found that serotype 14 was the most common cause of IPD in every region, and serotype 1 was common in Asia [53]. Our findings suggest that pneumococcus is the bacterium most commonly isolated by culture, LAT or PCR in fluids from otherwise sterile sites, which suggests that it is the most common aetiologic agent responsible for invasive bacterial diseases in the region. The previous research confirms the same findings using different methods. We analysed the observed frequency of S. pneumoniae through a meta-regression framework. In this respect, we accounted for the influence of various covariates on the observed prevalence of S. pneumoniae, such as age, diagnostic test used, surveillance setting, study centre and organ system involved.
The results show that pneumococcus poses a significant burden on the healthcare system and also affects the economic condition of patient's family. Steps should be taken to counter this organism, which could involve preventive measures by immunizing against S. pneumonia with vaccines like PCV-7, PCV-13 and PCV-10 and also by providing a clean and hygienic environment. Additionally, these steps could involve providing easily approachable healthcare facilities, low-cost antibiotics and home-based follow-ups. Preventive steps should be the first approach. Pakistan is the only country from South Asia to realize the importance of prevention by introducing PCV-10 into its immunization schedule with the help of the GAVI alliance. Bangladesh will also introduce the vaccine shortly. Because India forms the largest part of South Asia and as the data suggests it also forms the largest pneumococcal hub, preventive steps should be initiated in India soon. Most of the Indian data is based on nasopharyngeal sampling, which does not describe the aetiologic role of S. pneumoniae but only provides information about its carriage. As described by Johnson et al. [53], PCV-10 or PCV-13 could prevent 80% of all pneumococcal diseases, and a relevant vaccine should be introduced after determining the prevalent serotypes.
Furthermore, increasing drug resistance is creating another problem. Studies from South Asia have shown that there is increasing drug resistance to available antibiotics. In the IndiaCLEN Short Course Amoxycillin Therapy for Pneumonia (ISCAP) trial, the resistance pattern of S. pneumoniae to various antibiotics was: cotrimoxazole 66.3%, chloramphenicol 9.0%, oxacillin 15.9% and erythromycin 2.8% [54]. The Asian Network for Surveillance of Resistant Pathogens (ANSORP) study reported that 41% of strains were not susceptible to penicillin in Sri Lanka, and this rate was approximately 4% in India [55]. Kunango et al. reported that out of 150 clinical isolates from invasive pneumococcal infections, only 11 (7.3%) isolates were relatively resistant to penicillin, although 64 were resistant to one or more antibiotics, especially cotrimoxazole, tetracycline and chloramphenicol [56]. Unpublished data from one site of a multicentric trial IndiaCLEN severe pneumonia oral therapy (ISPOT) study in India showed that in approximately 38% of children with severe radiologically-confirmed pneumonia, S. pneumoniae was isolated from the nasopharyngeal aspirates or throat swabs. The study also showed that oral amoxicillin administered at home was effective in treating severe pneumonia. The No Shots study from Pakistan concluded that home treatment with high-dose oral amoxicillin in cases of severe pneumonia is equivalent to WHO recommendations [57]. Similarly, another study from Pakistan showed that local health workers were able to treat severe pneumonia cases at home with high-dose amoxicillin [58]. Moreover, Das and Singh showed that oral amoxicillin administered either in a hospital or in a community setting was effective in treating severe pneumonia and was not inferior to the standard treatment [59].
The authors strongly feel that there is a need for the introduction of a pneumococcal conjugate vaccine in South Asian countries. The prevalent serotypes should first be determined in order to introduce a relevant vaccine. Drug resistance should be assessed, and treatment guidelines should then be revisited in view of increasing drug resistance.
Supporting Information
PRISMA checklist.
(DOCX)
Detailed Search strategy.
(DOCX)
Acknowledgments
We would like to thank Dr. Samir K. Saha (ICDDR, Bangladesh), Dr. Z.A. Bhutta and Dr. S.Q. Nizami (AKU, Karachi, Pakistan) for providing us with their publications on pneumonia. We would also like to thank Dr. Jeeva Shankar (AIIMS, New Delhi) and Dr. Kay Dickerson (John Hopkins University, US) for helping us with the statistical methods.
Funding Statement
The review was supported and funded by ICMR, New Delhi (grant number 5/7/592/11-RHN). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Liu L, Johnson HL, Cousens S, Perin J, Scott S, et al. (2012) Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 379: 2151–2161. [DOI] [PubMed] [Google Scholar]
- 2.WHO (2007) World health statistics. Geneva
- 3. Morris SS, Black RE, Tomaskovic L (2003) Predicting the distribution of under-five deaths by cause in countries without adequate vital registration systems. Int J Epidemiol 32: 1041–1051. [DOI] [PubMed] [Google Scholar]
- 4. Rudan I, Boschi-Pinto C, Biloglav Z, Mulholland K, Campbell H (2008) Epidemiology and etiology of childhood pneumonia. Bull World Health Organ 86: 408–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Childinfo website. Available: http://www.childinfo.org/country_list.php.
- 6. Shann F (1986) Etiology of severe pneumonia in children in developing countries. Pediatr Infect Dis 5: 247–252. [DOI] [PubMed] [Google Scholar]
- 7. Mulholland EK (2004) Use of vaccine trials to estimate burden of disease. J Health Popul Nutr 22: 257–267. [PubMed] [Google Scholar]
- 8. O'Brien KL, Wolfson LJ, Watt JP, Henkle E, Deloria-Knoll M, et al. (2009) Burden of disease caused by Streptococcus pneumoniae in children younger than 5 years: global estimates. Lancet 374: 893–902. [DOI] [PubMed] [Google Scholar]
- 9.WHO (March, 2009) Global literature review of Haemophilus influenzae type b and Streptococcus pneumoniae invasive disease among children less than five years of age,1980–2005. Available: http://whqlibdoc.who.int/hq/2009/WHO_IVB_09.02_eng.pdf.
- 10. Suvarna Devi P, Murthy SN, Nathsharma KC, Murthy US (1982) Etiological study of pyogenic meningitis in children by CIEP. Indian Pediatrics 19: 317–320. [PubMed] [Google Scholar]
- 11. John TJ, Cherian T, Steinhoff MC, Simoes EA, John M (1991) Etiology of acute respiratory infections in children in tropical southern India. Rev Infect Dis 13 Suppl 6S463–469. [DOI] [PubMed] [Google Scholar]
- 12. Deivanayagam N, Ashok TP, Nedunchelian K, Ahamed SS, Mala N (1993) Bacterial meningitis: diagnosis by latex agglutination test and clinical features. Indian Pediatr 30: 495–500. [PubMed] [Google Scholar]
- 13. Patwari AK, Bisht S, Srinivasan A, Deb M, Chattopadhya D (1996) Aetiology of pneumonia in hospitalized children. J Trop Pediatr 42: 15–20. [DOI] [PubMed] [Google Scholar]
- 14. Thomas K (1999) IBIS Group INCLEN (1999) Prospective multicentre hospital surveillance of Streptococcus pneumoniae disease in India. Invasive Bacterial Infection Surveillance (IBIS) Group, International Clinical Epidemiology Network (INCLEN). Lancet 353: 1216–1221. [PubMed] [Google Scholar]
- 15. Sahai S, Mahadevan S, Srinivasan S, Kanungo R (2001) Childhood bacterial meningitis in Pondicherry, South India. Indian J Pediatr 68: 839–841. [DOI] [PubMed] [Google Scholar]
- 16. Kabra SK, Lodha R, Broor S, Chaudhary R, Ghosh M, et al. (2003) Etiology of acute lower respiratory tract infection. Indian J Pediatr 70: 33–36. [DOI] [PubMed] [Google Scholar]
- 17. Viswanath G, Praveen, Hanumanthappa AR, Chandrappa NR, Mahesh CB (2007) Bacteriological study of pyogenic meningitis with special reference to latex agglutination. Indian J Pathol Microbiol 50: 97–100. [PubMed] [Google Scholar]
- 18. Baqui AH, Rahman M, Zaman K, El Arifeen S, Chowdhury HR, et al. (2007) A population-based study of hospital admission incidence rate and bacterial aetiology of acute lower respiratory infections in children aged less than five years in Bangladesh. J Health Popul Nutr 25: 179–188. [PMC free article] [PubMed] [Google Scholar]
- 19. Brooks WA, Breiman RF, Goswami D, Hossain A, Alam K, et al. (2007) Invasive pneumococcal disease burden and implications for vaccine policy in urban Bangladesh. Am J Trop Med Hyg 77: 795–801. [PubMed] [Google Scholar]
- 20. Mani R, Pradhan S, Nagarathna S, Wasiulla R, Chandramuki A (2007) Bacteriological profile of community acquired acute bacterial meningitis: a ten-year retrospective study in a tertiary neurocare centre in South India. Indian J Med Microbiol 25: 108–114. [DOI] [PubMed] [Google Scholar]
- 21. Shameem S, Vinod Kumar CS, Neelagund YF (2008) Bacterial meningitis: rapid diagnosis and microbial profile: a multicentered study. J Commun Dis 40: 111–120. [PubMed] [Google Scholar]
- 22. Arifeen SE, Saha SK, Rahman S, Rahman KM, Rahman SM, et al. (2009) Invasive pneumococcal disease among children in rural Bangladesh: results from a population-based surveillance. Clin Infect Dis 48 Suppl 2S103–113. [DOI] [PubMed] [Google Scholar]
- 23. Batuwanthudawe R, Karunarathne K, Dassanayake M, de Silva S, Lalitha MK, et al. (2009) Surveillance of invasive pneumococcal disease in Colombo, Sri Lanka. Clin Infect Dis 48 Suppl 2S136–140. [DOI] [PubMed] [Google Scholar]
- 24. Naheed A, Saha SK, Breiman RF, Khatun F, Brooks WA, et al. (2009) Multihospital surveillance of pneumonia burden among children aged <5 years hospitalized for pneumonia in Bangladesh. Clin Infect Dis 48 Suppl 2S82–89. [DOI] [PubMed] [Google Scholar]
- 25. Williams EJ, Thorson S, Maskey M, Mahat S, Hamaluba M, et al. (2009) Hospital-based surveillance of invasive pneumococcal disease among young children in urban Nepal. Clin Infect Dis 48 Suppl 2S114–122. [DOI] [PubMed] [Google Scholar]
- 26. Shah AS, Knoll MD, Sharma PR, Moisi JC, Kulkarni P, et al. (2009) Invasive pneumococcal disease in Kanti Children's Hospital, Nepal, as observed by the South Asian Pneumococcal Alliance network. Clin Infect Dis 48 Suppl 2S123–128. [DOI] [PubMed] [Google Scholar]
- 27. Shah AS, Nisarga R, Ravi Kumar KL, Hubler R, Herrera G, et al. (2009) Establishment of population-based surveillance for invasive pneumococcal disease in Bangalore, India. Indian J Med Sci 63: 498–507. [PubMed] [Google Scholar]
- 28. Zaidi AK, Khan H, Lasi R, Mahesar W (2009) Surveillance of pneumococcal meningitis among children in Sindh, southern Pakistan. Clin Infect Dis 48 Suppl 2S129–135. [DOI] [PubMed] [Google Scholar]
- 29. Owais A, Tikmani SS, Sultana S, Zaman U, Ahmed I, et al. (2010) Incidence of pneumonia, bacteremia, and invasive pneumococcal disease in Pakistani children. Trop Med Int Health 15: 1029–1036. [DOI] [PubMed] [Google Scholar]
- 30. Kelly DF, Thorson S, Maskey M, Mahat S, Shrestha U, et al. (2011) The burden of vaccine-preventable invasive bacterial infections and pneumonia in children admitted to hospital in urban Nepal. Int J Infect Dis 15: e17–23. [DOI] [PubMed] [Google Scholar]
- 31. Bahl R, Mishra S, Sharma D, Singhal A, Kumari S (1995) A bacteriological study in hospitalized children with pneumonia. Ann Trop Paediatr 15: 173–177. [DOI] [PubMed] [Google Scholar]
- 32. Acharya D, Prasanna KS, Nair S, Rao RS (2003) Acute respiratory infections in children: a community based longitudinal study in south India. Indian J Public Health 47: 7–13. [PubMed] [Google Scholar]
- 33. Agarwal J, Awasthi S, Rajput A, Tiwari M, Jain A (2009) Atypical bacterial pathogens in community-acquired pneumonia in children: a hospital-based study. Trop Doct 39: 109–111. [DOI] [PubMed] [Google Scholar]
- 34. Asghar R, Banajeh S, Egas J, Hibberd P, Iqbal I, et al. (2008) Chloramphenicol versus ampicillin plus gentamicin for community acquired very severe pneumonia among children aged 2–59 months in low resource settings: multicentre randomised controlled trial (SPEAR study). BMJ 336: 80–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Awasthi S, Pande VK (1997) Seasonal pattern of morbidities in preschool slum children in Lucknow, north India. Indian Pediatr 34: 987–993. [PubMed] [Google Scholar]
- 36. Bansal A, Singhi SC, Jayashree M (2006) Penicillin and gentamicin therapy vs amoxicillin/clavulanate in severe hypoxemic pneumonia. Indian J Pediatr 73: 305–309. [DOI] [PubMed] [Google Scholar]
- 37. Bansal S, Kashyap S, Pal LS, Goel A (2004) Clinical and bacteriological profile of community acquired pneumonia in Shimla, Himachal Pradesh. Indian J Chest Dis Allied Sci 46: 17–22. [PubMed] [Google Scholar]
- 38. Bharti B, Bharti S, Verma V (2006) Severe pneumonia in a remote hilly area: integrated management of childhood illness. Indian J Pediatr 73: 33–37. [DOI] [PubMed] [Google Scholar]
- 39. Hussain H, Waters H, Omer SB, Khan A, Baig IY, et al. (2006) The cost of treatment for child pneumonias and meningitis in the Northern Areas of Pakistan. Int J Health Plann Manage 21: 229–238. [DOI] [PubMed] [Google Scholar]
- 40. Jebaraj R, Cherian T, Raghupathy P, Brahmadathan KN, Lalitha MK, et al. (1999) Nasopharyngeal colonization of infants in southern India with Streptococcus pneumoniae. Epidemiol Infect 123: 383–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Mastro TD, Ghafoor A, Nomani NK, Ishaq Z, Anwar F, et al. (1991) Antimicrobial resistance of pneumococci in children with acute lower respiratory tract infection in Pakistan. Lancet 337: 156–159. [DOI] [PubMed] [Google Scholar]
- 42. Mastro TD, Nomani NK, Ishaq Z, Ghafoor A, Shaukat NF, et al. (1993) Use of nasopharyngeal isolates of Streptococcus pneumoniae and Haemophilus influenzae from children in Pakistan for surveillance for antimicrobial resistance. Pediatr Infect Dis J 12: 824–830. [DOI] [PubMed] [Google Scholar]
- 43. Mathisen M, Strand TA, Sharma BN, Chandyo RK, Valentiner-Branth P, et al. (2010) Clinical presentation and severity of viral community-acquired pneumonia in young Nepalese children. Pediatr Infect Dis J 29: e1–6. [DOI] [PubMed] [Google Scholar]
- 44. Mehta PN (2003) Choosing antibiotics for community acquired pneumonia. Indian Pediatr 40: 958–964. [PubMed] [Google Scholar]
- 45. Nizami SQ, Bhutta ZA, Hasan R (2006) Incidence of acute respiratory infections in children 2 months to 5 years of age in periurban communities in Karachi, Pakistan. J Pak Med Assoc 56: 163–167. [PubMed] [Google Scholar]
- 46. Patwari AK, Aneja S, Mandal RN, Mullick DN (1988) Acute respiratory infections in children: a hospital based report. Indian Pediatr 25: 613–617. [PubMed] [Google Scholar]
- 47. Rijal B, Tandukar S, Adhikari R, Tuladhar NR, Sharma PR, et al. (2010) Antimicrobial susceptibility pattern and serotyping of Streptococcus pneumoniae isolated from Kanti Children Hospital in Nepal. Kathmandu Univ Med J (KUMJ) 8: 164–168. [DOI] [PubMed] [Google Scholar]
- 48. Saha SK, Rikitomi N, Biswas D, Watanabe K, Ruhulamin M, et al. (1997) Serotypes of Streptococcus pneumoniae causing invasive childhood infections in Bangladesh, 1992 to 1995. J Clin Microbiol 35: 785–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Saha SK, Rikitomi N, Ruhulamin M, Masaki H, Hanif M, et al. (1999) Antimicrobial resistance and serotype distribution of Streptococcus pneumoniae strains causing childhood infections in Bangladesh, 1993 to 1997. J Clin Microbiol 37: 798–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Addo-Yobo E, Chisaka N, Hassan M, Hibberd P, Lozano JM, et al. (2004) Oral amoxicillin versus injectable penicillin for severe pneumonia in children aged 3 to 59 months: a randomised multicentre equivalency study. Lancet 364: 1141–1148. [DOI] [PubMed] [Google Scholar]
- 51. Saha SK, Naheed A, El Arifeen S, Islam M, Al-Emran H, et al. (2009) Surveillance for invasive Streptococcus pneumoniae disease among hospitalized children in Bangladesh: antimicrobial susceptibility and serotype distribution. Clin Infect Dis 48 Suppl 2S75–81. [DOI] [PubMed] [Google Scholar]
- 52. Huedo-Medina TB, Sanchez-Meca J, Marin-Martinez F, Botella J (2006) Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods 11: 193–206. [DOI] [PubMed] [Google Scholar]
- 53.Johnson HL, Deloria-Knoll M, Levine OS, Stoszek SK, Freimanis Hance L, et al. (2010) Systematic evaluation of serotypes causing invasive pneumococcal disease among children under five: the pneumococcal global serotype project. PLoS Med 7. [DOI] [PMC free article] [PubMed]
- 54. Agarwal G, Awasthi S, Kabra SK, Kaul A, Singhi S, et al. (2004) Three day versus five day treatment with amoxicillin for non-severe pneumonia in young children: a multicentre randomised controlled trial. BMJ 328: 791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Song JH, Lee NY, Ichiyama S, Yoshida R, Hirakata Y, et al. (1999) Spread of drug-resistant Streptococcus pneumoniae in Asian countries: Asian Network for Surveillance of Resistant Pathogens (ANSORP) Study. Clin Infect Dis 28: 1206–1211. [DOI] [PubMed] [Google Scholar]
- 56. Kanungo R, Rajalakshmi B (2001) Serotype distribution & antimicrobial resistance in Streptococcus pneumoniae causing invasive & other infections in south India. Indian J Med Res 114: 127–132. [PubMed] [Google Scholar]
- 57. Hazir T, Fox LM, Nisar YB, Fox MP, Ashraf YP, et al. (2008) Ambulatory short-course high-dose oral amoxicillin for treatment of severe pneumonia in children: a randomised equivalency trial. Lancet 371: 49–56. [DOI] [PubMed] [Google Scholar]
- 58. Soofi S, Ahmed S, Fox MP, MacLeod WB, Thea DM, et al. Effectiveness of community case management of severe pneumonia with oral amoxicillin in children aged 2–59 months in Matiari district, rural Pakistan: a cluster-randomised controlled trial. Lancet 379: 729–737. [DOI] [PubMed] [Google Scholar]
- 59. Das RR, Singh M (2013) Treatment of severe community-acquired pneumonia with oral amoxicillin in under-five children in developing country: a systematic review. PLoS One 8: e66232. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA checklist.
(DOCX)
Detailed Search strategy.
(DOCX)