Abstract
Objective
To examine the validity of the International Classification of Diseases, 10th revision (ICD-10) codes for hyponatraemia in the nationwide population-based Danish National Registry of Patients (DNRP) among inpatients of all ages.
Design
Population-based validation study.
Setting
All somatic hospitals in the North and Central Denmark Regions from 2006 through 2011.
Participants:
Patients of all ages admitted to hospital (n=819 701 individual patients) during the study period. The patient could be included in the study more than once, and our study did not restrict to patients with serum sodium measurements (total of n=2 186 642 hospitalisations).
Main outcome measure
We validated ICD-10 discharge diagnoses of hyponatraemia recorded in the DNRP, using serum sodium measurements obtained from the laboratory information systems (LABKA) research database as the gold standard. One sodium value <135 mmol/L measured at any time during hospitalisation confirmed the diagnosis. We estimated sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) for ICD-10 codes for hyponatraemia overall and for cut-off points for increasing hyponatraemia severity.
Result
An ICD-10 code for hyponatraemia was recorded in the DNRP in 5850 of the 2 186 642 hospitalisations identified. According to laboratory measurements, however, hyponatraemia was present in 306 418 (14%) hospitalisations. Sensitivity of hyponatraemia diagnoses was 1.8% (95% CI 1.7% to 1.8%). For sodium values <115 mmol/L, sensitivity was 34.3% (95% CI 32.6% to 35.9%). The overall PPV was 92.5% (95% CI 91.8% to 93.1%) and decreased with increasing hyponatraemia severity. Specificity and NPV were high for all cut-off points (≥99.8% and ≥86.2%, respectively). Patients with hyponatraemia without a corresponding ICD-10 discharge diagnosis were younger and had higher Charlson Comorbidity Index scores than patients with hyponatraemia with a hyponatraemia code in the DNRP.
Conclusions
ICD-10 codes for hyponatraemia in the DNRP have high specificity but very low sensitivity. Laboratory test results, not discharge diagnoses, should be used to ascertain hyponatraemia.
Keywords: Epidemiology, Statistics & Research Methods
Strengths and limitation of this study.
This is the first study to validate the International Classification of Diseases, 10th revision code for hyponatraemia in hospitalised patients of all ages.
We used a population-based design, utilizing unambiguous individual-level linkage between registries containing complete data on all hospitalisations and laboratory measurements, thereby ensuring a large sample size and virtually eliminating the risk of selection bias.
We did not consider the duration of hyponatraemia. Sensitivity may have been higher if the presence of hyponatraemia required that it was detected in more than one laboratory measurement during hospitalisation.
Introduction
Hyponatraemia, defined as a serum sodium value <135 mmol/L, is the most common electrolyte abnormality encountered in clinical practice.1 It can be caused by a large variety of conditions, such as heart failure, kidney failure, cirrhosis, syndrome of an inappropriate antidiuretic hormone, vomiting and diarrhoea, and can also be a side effect of several medications.2 Results of recent studies have indicated that even a mild-to-moderate level of hyponatraemia may be an important predictor of poor prognosis in patients with cardiovascular disease, kidney and liver disease and cancer.3–8 However, key aspects of the aetiology and prognosis of hyponatraemia remain unknown.
The Danish population-based medical registries may offer a unique opportunity for studies of the epidemiology of hyponatraemia, if data are valid. However, as symptoms of mild and moderate hyponatraemia may be vague, and concealed by or construed as symptoms of an underlying disease, it is likely that the condition will not be reported.9 10 Thus, use of only inpatient discharge diagnoses of hyponatraemia in epidemiological studies may cause bias that can affect the validity of study results.11
Until now, only one study has investigated the validity of the International Classification of Diseases, 10th revision (ICD-10) codes for hyponatraemia. This Canadian study was restricted to patients 66 years of age or older with serum sodium values at the time of emergency department contact or at hospital admission.12 The sensitivity of hyponatraemia coding was found to be as low as 7%. For inpatients younger than 66 years, knowledge of the validity of hyponatraemia diagnoses is limited to a study performed in a single hospital in the Netherlands using ICD-9 codes for hyponatraemia. In this study, sensitivity was found to be just below 2%, using hospital laboratory data as the reference standard.13 Similar results were found in a study examining the validity of outpatient professional ICD-9 claims for hyponatraemia in the USA.14
We therefore conducted the first population-based study examining the validity of ICD-10 inpatient discharge diagnoses of hyponatraemia in the Danish National Registry of Patients (DNRP), including patients of all ages.
Methods
Setting and data collection
We used the DNRP to identify all admissions to hospitals in the North and Central Denmark Regions (2.1 million inhabitants in the study period) from 1 January 2006 to 31 December 2011. The DNRP contains information, including date of admission and discharge, department code and discharge diagnoses, on all admissions to Danish non-psychiatric hospitals since 1977.15 16
By use of the unique 10-digit civil registration number, assigned to all Danish residents since 1968,17 we linked each patient's DNRP data to the clinical laboratory information system (LABKA) research database. For patients living in the North and Central Denmark Regions, data on virtually all specimens analysed in clinical laboratories by hospitals and medical practitioners are entered into a computer-based clinical laboratory information system, which functions as a routine diagnostic tool for medical personnel.18 Data are transferred electronically to the LABKA research database, managed by Aarhus University. Analyses are coded according to the NPU (Nomenclature, Properties and Units) system. The LABKA research database contains the civil registration number, time and date of blood sampling, and identification code of the requesting physician or hospital department.18 We used the LABKA research database to retrieve information on all serum sodium measurements recorded during each of the identified hospitalisations.
Hyponatraemia diagnosis (ICD-10 code algorithm)
At hospital discharge, the attending physician assigns one primary diagnosis, reflecting the main reason for hospitalisation and treatment and up to 19 secondary diagnoses regarding additional clinically relevant conditions, including underlying diseases, complications and symptoms.19 Diagnoses recorded in the DNRP have been coded according to the ICD-10 since 1994.16
We developed an algorithm based on ICD-10 codes to identify primary and secondary discharge diagnoses of hyponatraemia recorded in the DNRP for each hospitalisation. The following ICD-10 codes were included in the algorithm: E87.1 (hypo-osmolality and hyponatraemia), E87.1A (hyponatraemia) and P74.2B (hyponatraemia in newborns (Danish version of ICD-10)).
Gold standard (laboratory serum sodium measurements)
We used serum sodium measurements recorded in the LABKA research database as the gold standard to confirm or disconfirm a diagnosis of hyponatraemia identified by the ICD-10 algorithm. Hyponatraemia was defined as serum sodium values <135 mmol/L for patients older than 30 days and <133 mmol/L for infants 30 days of age or younger.20 Patients were considered to have hyponatraemia if at least one hyponatraemic serum sodium value was recorded during their hospitalisation. If no serum sodium measurement was available, the patient was assumed to have a non-hyponatraemic serum sodium value (135–145 mmol/L). The following cut-off points for increasing severity of hyponatraemia were chosen: 135, 130, 125, 120 and 115 mmol/L.13 The corresponding levels for infants less than 31 days of age were 133, 128, 123, 118 and 113 mmol/L.
Other variables
For each patient, we assessed comorbidity by information retrieved from the DNRP on the conditions included in the Charlson Comorbidity Index (CCI). The CCI includes 19 medical conditions, each assigned a weighted score between 1 and 6. The sum of these individual scores is used as a measure of a patient's comorbidity burden.21 22 We calculated CCI scores for each patient and defined three comorbidity levels: low (CCI score 0), medium (CCI score 1–2) and high (CCI score of 3 or above). We included morbidities recorded within 10 years prior to the current hospitalisation, as conditions requiring hospital treatment within this timeframe would most likely influence the attending physician's diagnostic approach and evaluation during the current hospitalisation.
Furthermore, we obtained information on the department of admission and year of admission from the DNRP. Departments were categorised in the following five groups: internal medicine, surgery, gynaecology/obstetrics, paediatrics and other.
Statistical analysis
Patients with a hyponatraemic serum sodium value recorded in the LABKA research database were divided into two categories: Those with an ICD-10 code for hyponatraemia in the DNRP and those without. We described both groups of patients in terms of gender, age (median and associated IQR), department of admission, CCI score and specific comorbidities.
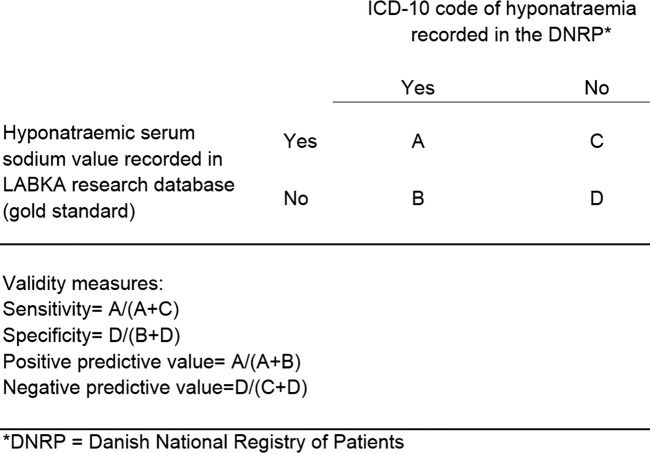
We estimated the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV; figure 1) for ICD-10 codes for hyponatraemia in the DNRP with corresponding 95% CI, using the exact method for binomial proportions. We defined sensitivity as the probability of an ICD-10 code for hyponatraemia being registered in the DNRP, when the laboratory test result identified the presence of hyponatraemia. Specificity was defined as the probability of an ICD-10 code for hyponatraemia not being registered in the DNRP, when hyponatraemia was not identified in laboratory test results. We estimated the PPV as the proportion of patients for whom an ICD-10 code for hyponatraemia recorded in the DNRP could be confirmed by a serum sodium measurement, and NPV as the proportion of patients with no ICD-10 code for hyponatraemia in the DNRP, for whom non-hyponatraemic or no serum sodium values were recorded in the LABKA research database. The analyses were repeated for all hyponatraemia cut-off points and after stratification by age group categories, department of admission and admission year.
Figure 1.
Schematic 2×2 table and validity measure estimation formulas.
Finally, we conducted four sensitivity analyses. First, we performed a complete case analysis, a method for dealing with missing data considering only participants with recorded values for all covariates,23 meaning that only patients with at least one serum sodium measurement during their hospitalisation were included in the analysis. We did so, in order to evaluate the assumption that patients without a serum sodium measurement were normonatraemic. In the second sensitivity analysis, we included only patients with more than one serum sodium measurement during their hospitalisation. In the third sensitivity analysis, we included only the ICD-10 codes E87.1A (hyponatraemia) and P74.2B (hyponatraemia in newborns). Because epidemiological studies often focus on incident cases, we performed a post hoc sensitivity analysis in which we restricted to the first hospitalisation for each patient in the study period.
Data analyses were performed using the statistical software package STATA (V.12; Stata Corp, College Station, Texas, USA).
All data were obtained from Danish public registries. According to Danish law their use does require informed consent or ethics committee approval.
Results
Characteristics
We identified 2 186 642 hospitalisations (819 701 individual patients) within the study period. For 1 308 740 (60%) hospitalisations, at least one serum sodium measurement was recorded in the LABKA research database, and for 1 037 647 (47%) hospitalisations subsequent measurements were recorded. According to the recorded serum sodium value, hyponatraemia was present in 306 418 hospitalisations (14%). In the DNRP, we identified 5850 hospitalisations with an ICD-10 code of hyponatraemia (hypo-osmolality and hyponatraemia=3722, hyponatraemia=2124, hyponatraemia in newborns=4) among all 2 186 642 hospitalisations. Of these, 440 did not have a hyponatraemic serum sodium value recorded in the LABKA research database.
Table 1 shows the distribution of hospitalisations by the presence/absence of an ICD-10 diagnosis of hyponatraemia recorded in the DNRP, by gender, age and comorbidity variables, for patients with hyponatraemic serum sodium values. Patients who had an ICD-10 code of hyponatraemia recorded in the DNRP and a corresponding hyponatraemic serum sodium measurement were on average older, more often female, more likely admitted to an internal medicine department and characterised by lower comorbidity levels than patients with no hyponatraemia diagnosis in the DNRP, but having hyponatraemic serum sodium values recorded in the LABKA research database. Cerebrovascular disease, dementia and ulcer disease were the only comorbidities that were more frequently found in patients with an ICD-10 code for hyponatraemia and corresponding hyponatraemic serum sodium value, compared to patients with hyponatraemia without a hyponatraemia diagnosis in the DNRP (table 1).
Table 1.
Characteristics of hospitalisations identified in the DNRP from 2006 to 2011
| Hospitalisations with at least on serum sodium value <135 mmol/L recorded in the LABKA research database |
All hospitalisations (n=2 186 642), n (%) | ||
|---|---|---|---|
| ICD-10 code of hyponatraemia in the DNRP (n=5410), n (%) | No ICD-10 code of hyponatraemia in the DNRP* (n=301 008), n (%) | ||
| Sex | |||
| Female | 3643 (67.3) | 148 120 (49.3) | 1 168 803 (53.5) |
| Male | 1767 (32.7) | 152 588 (50.7) | 1 017 839 (46.5) |
| Age, years | |||
| Median (IQR) | 77.3 (65.7–84.9) | 67.4 (54.2–78.2) | 54.7 (29.3–71.1) |
| Department of admission | |||
| Internal medicine | 5173 (95.6) | 184 848 (61.6) | 943 121 (43.1) |
| Surgical | 184 (3.4) | 88 378 (29.4) | 630 525 (28.8) |
| Gynaecological/obstetric | 10 (0.2) | 7104 (2.4) | 347 365 (15.9) |
| Paediatric | 29 (0.5) | 15 830 (5.3) | 165 289 (7.6) |
| Other | 14 (0.3) | 4848 (1.6) | 100 342 (4.6) |
| CCI level (score) | |||
| Low (0) | 2075 (38.4) | 100 398 (33.4) | 1 232 762 (56.4) |
| Medium (1–2) | 2182 (40.3) | 106 874 (35.5) | 588 783 (26.9) |
| High (≥3) | 1153 (21.3) | 93 736 (31.1) | 365 097 (16.7) |
| Specific comorbidities | |||
| Myocardial infarction | 312 (5.8) | 23 269 (7.7) | 108 373 (5.0) |
| Congestive heart failure | 460 (8.5) | 31 236 (10.4) | 121 429 (5.6) |
| Peripheral vascular disease | 464 (8.6) | 29 356 (9.8) | 115 620 (5.3) |
| Cerebrovascular disease | 1017 (18.8) | 39 466 (13.1) | 182 304 (8.3) |
| Dementia | 107 (3.1) | 4247 (1.4) | 20 711 (1.0) |
| Chronic pulmonary disease | 870 (16.1) | 48 726 (16.2) | 231 121 (10.6) |
| Connective tissue disease | 291 (5.4) | 13 990 (4.7) | 73 299 (3.4) |
| Ulcer disease | 450 (8.3) | 20 645 (6.9) | 79 050 (3.6) |
| Mild liver disease | 189 (3.5) | 13 413 (4.5) | 37 698 (1.7) |
| Moderate-to-severe liver disease | 66 (1.2) | 6279 (2.1) | 14 999 (0.7) |
| Diabetes I and II | 521 (9.6) | 39 995 (13.3) | 150 205 (6.9) |
| Diabetes with complications | 269 (5.0) | 25 083 (8.3) | 85 035 (3.9) |
| Hemiplegia | 35 (0.7) | 2462 (0.8) | 16 060 (0.7) |
| Moderate-to-severe renal disease | 143 (2.6) | 20 123 (6.7) | 75 441 (3.5) |
| Malignant tumour | 781 (14.4) | 64 882 (21.6) | 312 845 (14.3) |
| Leukaemia | 22 (0.4) | 4636 (1.5) | 17 190 (0.8) |
| Lymphoma | 51 (0.9) | 7096 (2.4) | 25 348 (1.2) |
| Metastatic cancer | 183 (3.4) | 23 948 (8.0) | 105 512 (4.8) |
| AIDS | 3 (0.1) | 475 (0.2) | 2014 (0.1) |
CCI, Charlson Comorbidity Index; DNRP, Danish National Registry of Patients; ICD-10, International Classification of Diseases, 10th revision.
Sensitivity, specificity, PPV and NPV
For 440 (7.5%) of the 5850 hospitalisations with an ICD-10 code for hyponatraemia recorded in the DNRP, no hyponatraemic serum sodium measurement was recorded in the LABKA research database during the hospitalisation (for 178, no measurement was recorded at all). This corresponds to a PPV of an ICD-10 code for hyponatraemia of 92.5% (95% CI 91.8% to 93.1%) for serum sodium values <135 mmol/L (<133 mmol/L for infants 30 days of age or younger). As expected, PPV decreased with lower serum sodium cut-off points. A total of 5410 hospitalisations had both an ICD-10 code recorded in the DNRP and a corresponding hyponatraemic laboratory measurement, resulting in a sensitivity of the ICD-10 codes of 1.8% (95% CI 1.7% to 1.8%). Sensitivity increased with lower cut-off points for serum sodium, reaching 34.3% (95% CI 32.6% to 35.9%) for serum sodium <115 mmol/L. Specificity and NPV for serum sodium <135 mmol/L were 100% (97.5% CI 100%) and 86.2% (95% CI 86.2% to 86.2%), respectively. Specificity and NPV remained high for all serum sodium cut-off points (table 2).
Table 2.
Validity of ICD-10 codes for hyponatraemia recorded in the DNRP, using serum sodium measurements in the LABKA research database as the gold standard
| Hyponatraemic serum sodium value recorded in the LABKA research database (mmol/L) | ICD-10 code for hyponatraemia recorded in the DNRP* |
Validity measures, % (95% CI) | |||||
|---|---|---|---|---|---|---|---|
| Yes | No | Total | |||||
| Overall | |||||||
| Na<135* | Yes | 5410 | 301 008 | 306 418 | Sensitivity | 8 (1.7 to 1.8) | |
| No | 440 | 1 879 784 | 1 880 224 | Specificity | 100 (100 to 100) | ||
| Total | 5850 | 2 180 792 | 2 186 642 | PPV | 92.5 (91.8 to 93.1) | ||
| NPV | 86.2 (86.2 to 86.2) | ||||||
| Cut-off points for increasing severity of hyponatraemia | |||||||
| Na<130† | Yes | 4528 | 80 605 | 85 133 | Sensitivity | 5.3 (5.2 to 5.5) | |
| No | 1322 | 2 100 187 | 2 101 509 | Specificity | 99.9 (99.9 to 99.9) | ||
| Total | 5850 | 2 180 792 | 2 186 642 | PPV | 77.4 (76.3 to 78.5) | ||
| NPV | 96.3 (96.3 to 96.3) | ||||||
| Na<125‡ | Yes | 3261 | 21 544 | 24 805 | Sensitivity | 13.1 (12.7 to 13.6) | |
| No | 2589 | 2 159 248 | 2 161 837 | Specificity | 99.9 (99.9 to 99.9) | ||
| Total | 5850 | 2 180 792 | 2 186 642 | PPV | 55.7 (54.5 to 57.0) | ||
| NPV | 99.0 (99.0 to 99.0) | ||||||
| Na<120§ | Yes | 2061 | 6219 | 8280 | Sensitivity | 24.9 (24.0 to 25.9) | |
| No | 3789 | 2 174 573 | 2 178 362 | Specificity | 99.8 (99.8 to 99.8) | ||
| Total | 5850 | 2 180 792 | 2 186 642 | PPV | 35.2 (34.0 to 36.5) | ||
| NPV | 99.7 (99.7 to 99.7) | ||||||
| Na<115¶ | Yes | 1107 | 2127 | 3234 | Sensitivity | 34.3 (32.6 to 35.9) | |
| No | 4743 | 2 178 665 | 2 183 408 | Specificity | 99.8 (99.8 to 99.8) | ||
| Total | 5850 | 2 180 792 | 2 186 642 | PPV | 18.9 (17.9 to 20.0) | ||
| NPV | 99.9 (99.9 to 99.9) | ||||||
*Corresponding to <133 mmol/L for infants ≤30 days of age.
†Corresponding to <128 mmol/L for infants ≤30 days of age.
‡Corresponding to <123 mmol/L for infants ≤30 days of age.
§Corresponding to <118 mmol/L for infants ≤30 days.
¶Corresponding to <113 mmol/L for infants ≤30 days of age.
DNRP, Danish National Registry of Patients; ICD-10, International Classification of Diseases, 10th revision; NPV, negative predictive value; PPV, positive predictive value.
Sensitivity was higher among admissions to internal medicine departments than among admissions to surgical, gynaecological/obstetric, paediatric and ‘other’ departments (table 3). The validity measures were virtually unchanged across the strata of the admission year.
Table 3.
Validity of ICD-10 codes for hyponatraemia recorded in the DNRP, stratified by age group categories, year and department of admission, for serum sodium values <135* and <125 mmol/L†
| Sensitivity, % (95% CI) |
Specificity, % (95% CI) |
PPV, % (95% CI) |
NPV % (95% CI) |
|||||
|---|---|---|---|---|---|---|---|---|
| <135 mmol/L | <125 mmol/L | <135 mmol/L | <125 mmol/L | <135 mmol/L | <125 mmol/L | <135 mmol/L | <125 mmol/L | |
| Age, years | ||||||||
| <15 | 0.2 (0.1 to 0.2) | 3.0 (1.5 to 5.2) | 100 (100 to 100) | 100 (100 to 100) | 84.4 (67.2 to 94.7) | 34.4 (18.6 to 53.2) | 94.6 (94.6 to 94.7) | 99.9 (99.9 to 99.9) |
| 15–34 | 0.2 (0.2 to 0.3) | 4.7 (3.0 to 6.9) | 100 (100 to 100) | 100 (100 to 100) | 80.0 (65.4 to 90.4) | 51.1 (35.8 to 66.3) | 95.5 (95.4 to 95.5) | 99.9 (99.9 to 99.9) |
| 35–49 | 0.9 (0.8 to 1.0) | 7.8 (6.7 to 9.0) | 100 (100 to 100) | 100 (100 to 100) | 91.3 (87.3 to 94.4) | 67.2 (61.2 to 72.8) | 90.8 (90.7 to 90.9) | 99.3 (99.3 to 99.3) |
| 50–64 | 1.3 (1.3 to 1.4) | 9.6 (8.9 to 10.3) | 100 (100 to 100) | 99.9 (99.9 to 99.9) | 93.9 (92.2 to 95.3) | 69.6 (66.7 to 72.3) | 83.6 (83.5 to 83.7) | 98.5 (98.4 to 98.5) |
| 65–79 | 1.8 (1.7 to 1.9) | 13.6 (12.9 to 14.4) | 100 (100 to 100) | 99.8 (99.8 to 99.8) | 92.9 (91.7 to 94.0) | 57.2 (55.0 to 59.3) | 79.1 (78.9 to 79.2) | 98.5 (98.4 to 98.5) |
| ≥80 | 3.4 (3.3 to 3.6) | 21.0 (19.9 to 22.1) | 99.9 (99.9 to 99.9) | 99.5 (99.5 to 99.5) | 92.0 (90.8 to 93.0) | 47.7 (45.7 to 49.7) | 75.7 (75.5 to 75.9) | 98.3 (98.3 to 98.4) |
| Admission year | ||||||||
| 2006 | 1.5 (1.4 to 1.7) | 12.5 (11.5 to 13.5) | 100 (100 to 100) | 99.9 (99.9 to 99.9) | 92.8 (90.8 to 94.5) | 66.6 (63.2 to 69.9) | 86.8 (86.6 to 86.9) | 99.0 (98.9 to 99.0) |
| 2007 | 1.4 (1.3 to 1.5) | 12.0 (11.0 to 13.1) | 100 (100 to 100) | 99.9 (99.9 to 99.9) | 94.4 (92.4 to 96.0) | 65.3 (61.6 to 68.8) | 87.0 (86.9 to 87.1) | 99.0 (99.0 to 99.1) |
| 2008 | 1.7 (1.6 to 1.8) | 12.3 (11.3 to 13.3) | 100 (100 to 100) | 99.9 (99.9 to 99.9) | 91.1 (89.1 to 92.8) | 53.6 (50.4 to 56.8) | 85.9 (85.8 to 86.1) | 99.0 (98.9 to 99.0) |
| 2009 | 1.8 (1.7 to 1.9) | 12.6 (11.6 to 13.6) | 100 (100 to 100) | 99.9 (99.8 to 99.9) | 93.4 (91.7 to 94.8) | 51.4 (48.4 to 54.5) | 85.5 (85.3 to 85.6) | 99.0 (98.9 to 99.0) |
| 2010 | 1.9 (1.8 to 2.0) | 14.2 (13.2 to 15.4) | 100 (100 to 100) | 99.9 (99.9 to 99.9) | 91.6 (89.8 to 93.2) | 54.4 (51.4 to 57.4) | 86.3 (86.2 to 86.4) | 99.1 (99.0 to 99.1) |
| 2011 | 2.2 (2.0 to 2.3) | 15.2 (14.1 to 16.4) | 100 (100 to 100) | 99.9 (99.9 to 99.9) | 92.2 (90.6 to 93.6) | 49.8 (47.0 to 52.7) | 85.8 (85.7 to 85.9) | 99.1 (99.0 to 99.1) |
| Department | ||||||||
| Internal medicine | 2.7 (2.7 to 2.8) | 16.5 (16.0 to 17.0) | 99.9 (99.9 to 100) | 99.7 (99.7 to 99.7) | 92.8 (92.1 to 93.4) | 56.0 (54.7 to 57.3) | 80.3 (80.2 to 80.4) | 98.3 (98.3 to 98.3) |
| Surgical | 0.2 (0.2 to 0.2) | 2.3 (1.9 to 2.8) | 100 (100 to 100) | 100 (100 to 100) | 90.6 (85.8 to 94.3) | 57.6 (50.5 to 64.5) | 86.0 (85.9 to 86.1) | 99.2 (99.2 to 99.2) |
| Gynaecological/obstetric | 0.1 (0.1 to 0.3) | 3.1 (1.2 to 6.7) | 100 (100 to 100) | 100 (100 to 100) | 76.9 (46.2 to 95.0) | 46.2 (19.2 to 74.9) | 98.0 (97.9 to 98.0) | 99.9 (99.9 to 100) |
| Paediatric | 0.2 (0.1 to 0.3) | 3.4 (1.7 to 5.8) | 100 (100 to 100) | 100 (100 to 100) | 85.3 (68.9 to 95.0) | 35.3 (19.7 to 53.5) | 90.4 (90.3 to 90.6) | 99.8 (99.8 to 99.8) |
| Other | 0.3 (0.2 to 0.5) | 1.5 (0.4 to 3.9) | 100 (100 to 100) | 100 (100 to 100) | 58.3 (36.6 to 77.9) | 16.7 (4.74 to 37.4) | 95.2 (95.0 to 95.3) | 99.7 (99.7 to 99.8) |
*Corresponding to <133 mmol/L for infants ≤30 days of age.
†Corresponding to <123 mmol/L for infants ≤30 days of age.
DNRP, Danish National Registry of Patients; ICD-10, International Classification of Diseases, 10th revision; NPV, negative predictive value; PPV, positive predictive value.
Sensitivity analyses
Compared to the primary analyses, we observed no changes in either sensitivity or specificity estimates when including only patients with at least one serum sodium measurement during their hospitalisation in the analysis. PPV increased slightly for all serum sodium cut-off points, while NPV decreased for the three highest cut-off points. Including only patients with more than one serum sodium measurement also yielded almost identical results (table 4).
Table 4.
Sensitivity analyses
| Hyponatraemic serum sodium value recorded in the LABKA research database (mmol/L) | Primary analysis (including all admissions for all patients in the study period), % (95% CI) | Sensitivity analyses |
||||
|---|---|---|---|---|---|---|
| Requiring at least one serum sodium measurement during hospitalisation, % (95% CI) | Requiring >1 serum sodium measurement during hospitalisation, % (95% CI) | ICD-10 algorithm restricted to code E87.1A and P74.2B, % (95% CI) | Restricting to first admission per patient in the study period, % (95% CI) | |||
| Overall | ||||||
| Na<135 | Sensitivity | 1.8 (1.7 to 1.8) | 1.8 (1.7 to 1.8) | 1.9 (1.8 to 2.0) | 0.7 (0.6 to 0.7) | 1.7 (1.7 to 1.9) |
| Specificity | 100 (100 to 100) | 100 (100 to 100) | 100 (100 to 100) | 100 (100 to 100) | 100 (100 to 100) | |
| PPV | 92.5 (91.8 to 93.1) | 95.4 (94.8 to 95.9) | 95.8 (95.2 to 96.3) | 94.6 (93.6 to 95.6) | 93.5 (92.0 to 94.7) | |
| NPV | 86.2 (86.2 to 86.2) | 76.9 (76.8 to 77.0) | 74.7 (74.6 to 74.8) | 86.1 (86.0 to 86.1) | 91.6 (91.6 to 91.7) | |
| Cut-off points for increasing severity of hyponatraemia | ||||||
| Na<130 | Sensitivity | 5.3 (5.2 to 5.5) | 5.3 (5.2 to 5.5) | 5.6 (5.4 to 5.7) | 2.1 (2.0 to 2.2) | 6.3 (5.9 to 6.7) |
| Specificity | 99.9 (99.9 to 99.9) | 99.9 (99.9 to 99.9) | 99.9 (99.9 to 99.9) | 100 (100 to 100) | 100 (100 to 100) | |
| PPV | 77.4 (76.3 to 78.5) | 79.8 (78.7 to 80.9) | 80.5 (79.4 to 81.6) | 83.0 (81.4 to 84.6) | 82.2 (80.7 to 84.8) | |
| NPV | 96.3 (96.3 to 96.3) | 93.8 (93.8 to 93.9) | 93.0 (93.0 to 93.1) | 96.2 (96.2 to 96.2) | 97.9 (97.9 to 98.0) | |
| Na<125 | Sensitivity | 13.1 (12.7 to 13.6) | 13.1 (12.7 to 13.6) | 13.6 (13.1 to 14.0) | 5.4 (5.1 to 5.7) | 15.6 (14.6 to 16.6) |
| Specificity | 99.9 (99.9 to 99.9) | 99.8 (99.8 to 99.8) | 99.8 (99.8 to 99.8) | 100 (100 to 100) | 99.9 (99.9 to 99.9) | |
| PPV | 55.7 (54.5 to 57.0) | 57.5 (56.2 to 58.8) | 57.9 (56.5 to 59.2) | 62.5 (60.4 to 64.5) | 62.3 (59.6 to 64.8) | |
| NPV | 99.0 (99.0 to 99.0) | 98.3 (98.3 to 98.4) | 98.1 (98.1 to 98.1) | 98.9 (98.9 to 98.9) | 99.4 (99.4 to 99.4) | |
| Na<120 | Sensitivity | 24.9 (24.0 to 25.9) | 24.9 (24.0 to 25.8) | 25.4 (24.5 to 26.4) | 6.3 (5.8 to 6.9) | 29.3 (27.3 to 31.3) |
| Specificity | 99.8 (99.8 to 99.8) | 99.7 (99.7 to 99.7) | 99.7 (99.7 to 99.7) | 100 (100 to 100) | 99.9 (99.9 to 99.9) | |
| PPV | 35.2 (34.0 to 36.5) | 36.3 (35.1 to 37.6) | 36.3 (35.0 to 37.6) | 50.6 (47.5 to 53.7) | 43.7 (41.0 to 46.4) | |
| NPV | 99.7 (99.7 to 99.7) | 99.5 (99.5 to 99.5) | 99.5 (99.4 to 99.5) | 99.6 (99.6 to 99.7) | 99.8 (99.8 to 99.8) | |
| Na<115 | Sensitivity | 34.3 (32.6 to 35.9) | 34.2 (32.6 to 35.9) | 34.9 (33.1 to 36.6) | 9.3 (8.3 to 10.3) | 38.8 (35.5 to 42.1) |
| Specificity | 99.8 (99.8 to 99.8) | 99.7 (99.6 to 99.7) | 99.6 (99.6 to 99.6) | 100 (100 to 100) | 99.9 (99.9 to 99.9) | |
| PPV | 18.9 (17.9 to 20.0) | 19.5 (18.5 to 20.6) | 19.5 (18.4 to 20.6) | 28.8 (26.1 to 31.7) | 24.2 (22.0 to 26.6) | |
| NPV | 99.9 (99.9 to 99.9) | 99.8 (99.8 to 99.8) | 99.8 (99.8 to 99.8) | 99.9 (99.9 to 99.9) | 99.9 (99.9 to 99.9) | |
ICD-10, International Classification of Diseases, 10th revision; NPV, negative predictive value; PPV, positive predictive value.
After restriction to the most specific ICD-10 codes for hyponatraemia, PPV increased slightly and sensitivity decreased (94.6% (95% CI 93.6% to 95.6%) and 0.7% (95% CI 0.6% to 0.7%), respectively). Estimates of specificity and NPV were virtually unchanged (table 4).
We observed a slight increase in sensitivity for serum sodium cut-off points <130 mmol/L but not for the overall estimate when restricting to the first hospitalisation in the study period. PPV and NPV generally increased, although only very slightly for the overall estimate (table 4).
Discussion
This is the first study to report on the validity of ICD-10 coding of hyponatraemia using comprehensive population-based medical registries and including patients of all ages. A record of a hyponatraemia diagnosis in the DNRP was found to be specific to and highly predictive of hyponatraemia confirmed by laboratory values. However, the disorder was greatly under-reported, though to a lesser extent in patients admitted to an internal medicine department compared to other departments. We found sensitivity to be low even for severe degrees of hyponatraemia. These results were robust when we used a stricter definition of hyponatraemia and complete case analysis.
Our findings correspond to those of Movig et al's13 single-centre study conducted in the Netherlands, in which ICD-9-CM coding of hyponatraemia in inpatient discharge records was compared with hospital laboratory data. As in our study, sensitivity at the cut-off point of 135 mmol/L was 1.7%, and increased with decreasing serum sodium levels. Sensitivity thus reached 30.6% for values below 115 mmol/L. In addition, their estimates for PPV, NPV and specificity were similar to our results (91.7%, 79.5% and <99.9%, respectively). A Canadian study by Gandhi et al12 examined ICD-10 coding for hyponatraemia and reported a sensitivity of 6.4% for the cut-off point of <135 mmol/L and 41.7% for the cut-off point of 125 mmol/L. The study, however, was restricted to patients ≥66 years of age presenting with serum sodium values at the time of admission or emergency department contact. In line with their results, we found that the median age of patients with an ICD-10 code of hyponatraemia recorded in the DNRP, which could be confirmed by laboratory results, was higher than that of patients with hyponatraemia with no ICD-10 code for hyponatraemia recorded in the DNRP. However, the sensitivity estimates did not reach those found by Gandhi et al even for patients 65–79 and ≥80 years of age. Shea et al14 also reported higher sensitivity compared to our results (3.5% for a cut-off point of <136 mmol/L and 29.6% for the cut-off point of 125 mmol/L) in their study examining the validity of ICD-9 codes of hyponatraemia in an outpatient managed-care population. Outpatient serum sodium laboratory tests were compared with outpatient professional ICD-9 claims registered within 15 days before or after the laboratory claim. The PPV was 62.6% for serum sodium levels <136 mmol/L and 10.4% for levels <125 mmol/L. As noted in the paper, detected hyponatraemia may be the cause for follow-up visits in an outpatient setting, without the need for repeat measurements. This could lead to a lower PPV compared to our study and the study by Movig et al. In addition, managed-care claims databases encompass an employer-based commercially insured population. Thus, Shea et al's study may not be representative of elderly populations, in which prevalence of hyponatraemia is high.24 25 This may also explain why their results differed from ours.
The major strengths of our study are its population-based design and unambiguous individual-level linkage between registries containing complete data on all hospitalisations and laboratory tests in a well-defined population. This eliminates the risk of selection bias. Several potential study limitations must be considered. We relied on only one (the lowest) serum sodium value recorded to define the presence of hyponatraemia, and did not consider the duration of hyponatraemia. Clinicians may be more likely to regard hyponatraemia as clinically relevant, and hence to include the condition in discharge diagnoses, if it is detected in more than one measurement. In this context, it is important to note that patient transfers between departments are registered as separate admissions in the DNRP and that we examined the validity of ICD-10 coding for each registered admission. The PPV may have been even higher if we had considered contiguous admissions as a single admission. Finally, we chose to include patients without serum sodium measurements and to consider them as normonatraemic in the main analysis. We did so to detect false-positive diagnoses and thereby obtain accurate estimates of predictive values. Serum sodium is often measured as a routine procedure, and rarely due to specific suspicion. Although frequently measured, the proportion of patients with unacknowledged hyponatraemia is most often unknown. We therefore performed a complete case analysis, including only patients with serum sodium measurements. As the results did not differ markedly from those of the primary analysis, we believe that including patients without serum sodium measurements in the normonatraemic group was justified.
We can only speculate on the reasons for the low sensitivity of the ICD-10 coding of hyponatraemia found in our study. A diagnosis of hyponatraemia was less likely to be recorded in patients with high levels of comorbidity, which may indicate that hyponatraemia is mainly considered a bystander of the underlying diseases. If hyponatraemia is mild or transient, and does not require intervention or specific attention, it may not warrant documentation. However, even for very severe hyponatraemia (<115 mmol/L), which is potentially fatal and requires immediate intervention, sensitivity was low. We believe that this most likely reflects negligence of proper coding practice rather than lack of attention to the clinical importance of low serum sodium levels. With the increasing use of electronic medical records, it would be feasible and worthwhile to automatically assign discharge diagnoses to patients with gross abnormal laboratory values. However, the ultimate responsibility for summarising the most important reasons for treatment and care still rests on the discharging physician. Our results suggest that hyponatraemia is not coded in the presence of coexisting illness deemed more important, and that the fact that hyponatraemia may be an important indicator of a poor prognosis is not yet acknowledged.
The results of this validation study emphasise the need for caution when relying on ICD-10 codes for hyponatraemia in research. Based on the estimated PPV and specificity, patients with an ICD-10 code of hyponatraemia can safely be assumed to actually have hyponatraemia. However, the low sensitivity renders the ICD-10 codes inappropriate for use in studies examining prevalence, incidence and absolute risk, due to a high degree of misclassification. Sensitivity increased with decreasing serum sodium levels, suggesting that studies using ICD-codes to identify hyponatraemia would be based mainly on severe cases. Furthermore, our results indicate that quality of registration differs according to age, gender and morbidity status. Hence, studies may be susceptible to differential misclassification, again resulting in biased results.
Conclusion
We found that the ICD-10 coding of hyponatraemia in DNRP has high specificity but is highly incomplete, resulting in very low sensitivity. When available, laboratory test results for serum sodium will more correctly identify patients with hyponatraemia.
Supplementary Material
Footnotes
Contributors: LH-B participated in the design of the study, performed the data analysis, provided interpretation of study results and drafted the manuscript. SPU participated in the acquisition and analysis of data. CFC and HTS participated in the design of the study, provided interpretation of study results and helped draft the manuscript. TR and JOLJ contributed to the interpretation of study results and helped draft the manuscript. All authors read and approved the final manuscript.
Funding: This work was supported by the Clinical Epidemiology Research Foundation and by the Danish Cancer Society (grant no. R73-A4284-13-S17).
Competing interests: JOLJ has received an unrestricted research grant and lecture fees from Otsuka Pharma Scandinavia AB. TR has received lecture fees from Otsuka Pharma Scandinavia AB. LH-B, CFC, SPU and HTS are salaried employees of the Department of Clinical Epidemiology, Aarhus University Hospital. The Department of Clinical Epidemiology receives funding from companies in the form of research grants to (and administered by) Aarhus University.
Ethics approval: The study was approved by the Danish Data Protection Agency (record number 2006-53-1396).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Upadhyay A, Jaber BL, Madias NE. Incidence and prevalence of hyponatremia. Am J Med 2006;119(Suppl 1):S30–5 [DOI] [PubMed] [Google Scholar]
- 2.Rose BD. Clinical physiology of acid-base and electrolyte disorders. 3rd edn New York: McGraw-Hill information Services Company, 1989 [Google Scholar]
- 3.Waikar SS, Curhan GC, Brunelli SM. Mortality associated with low serum sodium concentration in maintenance hemodialysis. Am J Med 2011;124:77–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doshi SM, Shah P, Lei X, et al. Hyponatremia in hospitalized cancer patients and its impact on clinical outcomes. Am J Kidney Dis 2012;59:222–8 [DOI] [PubMed] [Google Scholar]
- 5.Goldberg A, Hammerman H, Petcherski S, et al. Prognostic importance of hyponatremia in acute ST-elevation myocardial infarction. Am J Med 2004;117:242–8 [DOI] [PubMed] [Google Scholar]
- 6.Kovesdy CP, Lott EH, Lu JL, et al. Hyponatremia, hypernatremia and mortality in patients with chronic kidney disease with and without congestive heart failure. Circulation 2012;125:677–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scherz N, Labarere J, Mean M, et al. Prognostic importance of hyponatremia in patients with acute pulmonary embolism. Am J Respir Crit Care Med 2010;182:1178–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wald R, Jaber BL, Price LL, et al. Impact of hospital-associated hyponatremia on selected outcomes. Arch Intern Med 2010;170:294–302 [DOI] [PubMed] [Google Scholar]
- 9.Chawla A, Sterns RH, Nigwekar SU, et al. Mortality and serum sodium: do patients die from or with hyponatremia? Clin J Am Soc Nephrol 2011;6:960–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marco J, Barba R, Matia P, et al. Low prevalence of hyponatremia codification in departments of internal medicine and its prognostic implications. Curr Med Res Opin 2013;29:1757–62 [DOI] [PubMed] [Google Scholar]
- 11.Sorensen HT, Sabroe S, Olsen J. A framework for evaluation of secondary data sources for epidemiological research. Int J Epidemiol 1996;25:435–42 [DOI] [PubMed] [Google Scholar]
- 12.Gandhi S, Shariff SZ, Fleet JL, et al. Validity of the International Classification of Diseases 10th revision code for hospitalisation with hyponatraemia in elderly patients. BMJ Open 2012;2:e001727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Movig KL, Leufkens HG, Lenderink AW, et al. Validity of hospital discharge International Classification of Diseases (ICD) codes for identifying patients with hyponatremia. J Clin Epidemiol 2003;56:530–5 [DOI] [PubMed] [Google Scholar]
- 14.Shea AM, Curtis LH, Szczech LA, et al. Sensitivity of International Classification of Diseases codes for hyponatremia among commercially insured outpatients in the United States. BMC Nephrol 2008;9:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Andersen TF, Madsen M, Jorgensen J, et al. The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull 1999;46:263–8 [PubMed] [Google Scholar]
- 16.Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health 2011;39(Suppl 7):30–3 [DOI] [PubMed] [Google Scholar]
- 17.Pedersen CB. The Danish Civil Registration System. Scand J Public Health 2011;39(Suppl 7):22–5 [DOI] [PubMed] [Google Scholar]
- 18.Grann AF, Erichsen R, Nielsen AG, et al. Existing data sources for clinical epidemiology: the clinical laboratory information system (LABKA) research database at Aarhus University, Denmark. Clin Epidemiol 2011;3:133–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. SSI—Joint Content for Basic Registration of Hospital Patients. http://www.ssi.dk/Sundhedsdataogit/Indberetning%20og%20patientregistrering/Patientregistrering/Faellesindhold.aspx (accessed 18 Dec 2013; updated 9 Dec 2013)
- 20.2011. Laboratory Manual for Hospitals in the North Jutland Region. http://www.laboratorievejledning.dk/prog/view.aspx?AfsnitID=103&KapitelID=26&UKapitelID=194 (accessed 15 Dec 2013; updated 20 Dec 2011)
- 21.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83 [DOI] [PubMed] [Google Scholar]
- 22.Thygesen SK, Christiansen CF, Christensen S, et al. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol 2011;11:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greenland S, Finkle WD. A critical look at methods for handling missing covariates in epidemiologic regression analyses. Am J Epidemiol 1995;142:1255–64 [DOI] [PubMed] [Google Scholar]
- 24.Hawkins RC. Age and gender as risk factors for hyponatremia and hypernatremia. Clin Chim Acta 2003;337:169–72 [DOI] [PubMed] [Google Scholar]
- 25.Miller M, Morley JE, Rubenstein LZ. Hyponatremia in a nursing home population. J Am Geriatr Soc 1995;43:1410–13 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.