Abstract
Background
Borderline personality disorder (BPD) affects 2.7% of adults. About 78% of adults with BPD also develop a substance-related disorder or addiction at some time in their lives. These persons are more impulsive and clinically less stable than BPD patients without substance dependency. They display suicidal behavior to a greater extent, drop out of treatment more often, and have shorter abstinence phases. The combination of borderline personality disorder with addiction requires a special therapeutic approach.
Methods
This review is based on a selective literature search about the treatment of patients with BPD and addiction, with particular attention to Cochrane Reviews and randomized controlled trials (RCT).
Results
The available evidence is scant. In two RCTs, Dialectical Behavior Therapy for Substance Use Disorders (DBT-SUD) was found to improve patients’ overall functional level (standardized mean difference, 1.07–1.78) and to increase the number of abstinence days (effect strength [ES], 1.03) and negative urine samples (ES, 0.75). Dual focus schema therapy (DFST) was evaluated in three RCTs. Because of methodological problems, however, no useful quantitative comparison across trials is possible. In one RCT, dynamic deconstructive psychotherapy (DDP) was found to have only a moderate, statistically insignificant effect. Only a single study provides data about potentially helpful drug therapy over the intermediate term.
Conclusion
Patients with borderline personality disorder and comorbid addiction should be treated as early as possible for both conditions in a thematically hierarchical manner. There is no evidence for any restriction on drug therapy to prevent recurrent addiction in these patients. The psychotherapeutic techniques that can be used (despite the currently inadequate evidence base) include DBT-SUD, DFST, and DDP. These patients need qualified expert counseling in choosing a suitable type of psychotherapy. Specific treatment is available in only a few places, and the relevant treatment networks in Germany are just beginning to be constructed.
The treatment of patients with borderline personality disorder (BPD) and comorbid addiction is complex. Frequently, there is uncertainty among health professionals about how to respond to patients’ self-harm behavior and how to design treatment plans. Consequently, intuition-guided treatment often ends up in difficult, ill-fated, doctor-patient relationships and impedes the use of effective therapeutic interventions.
Case vignette
27-year-old Ms. K. fits the criteria for BPD with comorbid addiction. Clinically, the patient presented with severe daily self-harming by cutting herself at the extremities and repeatedly inflicting burns to various parts of her body. The desired effects of this behavior were relief of tension and self-punishment, with the consequences at times posing a vital threat to the patient. In addition, she consumed excessive amounts of alcohol, combined with heroine, cannabis and benzodiazepine dependences. To that point, periods of abstinence had been interrupted by craving and family conflicts. Ms. K. has been experiencing suicidal ideation, including 4 suicide attempts, since age 14. Numerous treatment were terminated early, either by the patient or the institution.
This paper provides an overview of:
the epidemiology and
the available studies on the efficacy of psychopharmacotherapy as well as psychotherapy, according to the criteria of evidence-based medicine.
The three types of psychotherapy evaluated as being effective will be presented.
Epidemiology
The results from the National Epidemiological Survey on Alcohol and Related Conditions (NESARC) of over 43 000 adult individuals, completed in the United States, showed a point prevalence rate for borderline personality disorders (BPD) of 2.7% (1). Lower income, younger age (<30 years), marital status (separated, divorced, widowed), and lower educational attainment were associated with an increased risk of occurrence of the disorder (2). With 3.0%, BPD was significantly more frequently diagnosed in women than in men (2.4%). However, this difference may be the result of a diagnostic bias and the disorder may be equally distributed between the sexes (3).
Patients with BPD
The most frequent comorbid psychiatric disorders in BPD patients are anxiety and affective disorders, including posttraumatic stress disorder. The overall lifetime prevalence for these comorbidities is approximately 85%, followed by substance-related disorders with a lifetime prevalence of 78% (2). However, two further studies found lower lifetime prevalence rates for the use of dependence-producing substances. In a German sample of 147 patients, lifetime prevalence was similar (57.1% [4) to the 64.1% found in a US study (5). In Germany, tobacco dependence (54%), followed by alcohol dependence (47%) and drug dependence (22%) were the most common substance dependence comorbidities (1). Overall, the probability of occurrence of a drug dependence (odds ratio [OR] 10.1) and alcohol dependence (OR 5.38) or a substance-related disorder in general (OR 4.50) is significantly increased among BPD patients compared with that in the general population (2).
Patients with dependence disorders and various personality disorders
Conversely, increased prevalence rates for personality disorders are also found in patients with dependence disorders, e.g. a rate of approximately 57% in alcohol-related disorders. Here, with 13% of cases the most common diagnosis was BPD (6) (Box).
Box. Alcohol-dependent patients with personality disorder are different from those without personality disorder in that they show.
an increased general psychopathological burden (7)
a lower level of social functioning (9)
shorter periods of abstinence and more frequent relapses (10, 11)
more frequent patient- and center-initiated treatment dropout (12).
Overall, the long-term prognosis of the dependence disorder is poorer (13).
Focused on patients with borderline personality disorder and comorbid substance dependence disorders
The behavior of these patients is characterized by greater impulsivity compared with patients diagnosed with only one of the two disorders. Clinically, this manifests as a preference for short-term rewards and the reduced ability to work towards mid- or long-term rewards (11, 14). The findings regarding an aggravation of BPD symptoms with comorbid dependence disorders are inconsistent (15– 17). Even though the frequency of substance-related disorders in BPD patients decreases over the years (18), addiction is found to be a factor associated with a more unfavorable diagnosis in patients initially diagnosed with both BPD and dependence disorder, as remissions, defined as a drop below the minimum number of criteria required for the diagnosis of BPD according to DSM, occur less frequently: Remissions in BPD patients without comorbid addiction were four times more likely to occur within a period of six years compared with patients with such comorbidity (hazard ratio [HR] 4.01; p<0.0001); dependency disorders constituted a significantly worse prognostic factor for the course of BPD compared with, for example, comorbid post-traumatic stress disorder (PTSD) ([HR] 2.72, p<0.001), other anxiety (HR 1.93, p<0.001) or mood disorders (HR 1.97, p<0.001) (18).
Etiology and phenomenology of substance use in BPD patients
Substance use is caused by multiple factors. BPD patients often use dependence-producing substances in an attempt to mitigate emotions perceived as overwhelmingly negative or to replace these by a pleasant state, such as feeling intoxicated (self-medication hypothesis). Apart from that, the use of addictive substances can also be triggered by factors related to the social environment, such as peer pressure. The patterns of use show the same diversity as in the general population. Substances are frequently taken with the intention to produce a state similar to dissociation. Thus, the frequency of use can follow an episodic through to a dependent pattern of use (19).
Treatment of borderline personality disorder and comorbid substance dependence
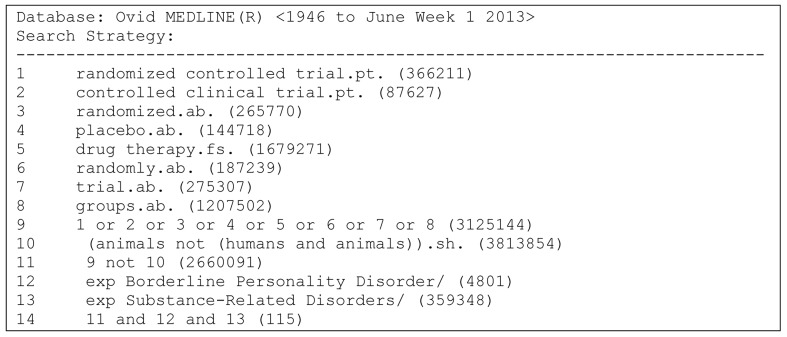
In the following, an overview of the specific treatment options for BPD patients with comorbid dependence disorder will be provided which is based on current Cochrane Collaboration reviews (20, 21) and a complementary recent search of the literature for randomized controlled trials (RCTs) in Medline (Figure). To estimate treatment effects, standardized mean differences (SMDs) and risk ratios (RRs) were calculated for continuous and categorical data, respectively.
Figure.
Search strategy for identifying relevant randomized controlled trials (Cochrane Highly Sensitive Search Strategy for identifying random ized trials in MEDLINE, sensitivity-maximizing version [2008 revision], Ovid format)
Treatment
Psychopharmacotherapy
Since in patients with BPD comorbid dependence disorders are typically regarded as an exclusion criterion for pharmacotherapy studies (21), the available evidence is limited to one randomized controlled treatment trial (RCT) on alcohol-dependent patients with BPD. This study compared 254 alcohol-dependent patients with
comorbid BPD
comorbid anti-social personality disorder or
none of the two personality disorders.
The studies investigated the efficacy of
placebo
50 mg naltrexone (an opioid antagonist)
50 mg naltrexone plus 250 mg disulfiram or
250 mg disulfiram plus placebo for addiction-related and general psychiatric symptoms.
The results were:
Pharmacological relapse prevention in patients with alcohol dependency and comorbid BPD was equally effective as in patients with alcohol dependency without comorbid BPD.
Pharmacotherapy with disulfiram or naltrexone reduced craving to the same extent as the intake of placebo.
In addition, no drug was superior to the others (22). There are no studies on other addictive substances available.
Note to clinicians: Patients with alcohol dependence and comorbid BPD benefit to the same extent from pharmacotherapy as patients with dependence disorder without comorbid BPD. Consequently, pharmacological relapse prevention should always be offered to patients with BPD and alcohol dependence, with continued administration if successful (10).
Psychotherapy
Data on the efficacy of psychological therapies are somewhat more robust (20). Presently available from comorbid patient populations are RCTs and manuals on Dialectical Behavior Therapy for Substance Use Disorders (DBT-SUD) (23– 26), a version of dialectical behavior therapy specifically developed for comorbid patients, on dynamic deconstructive psychotherapy (DDP) (27– 30), a psychodynamic approach, and on schema therapy for addiction (Dual Focus Schema Therapy, DFST) (31– 34).
Dialectical Behavior Therapy for Substance Use Disorders (DBT-SUD)—DTB-SUD is a behavioral therapy which, because of its transparency and specifically developed educational concept, is easier to learn than any other method currently available for this patient group. It takes a solution-focused approach and teaches these patients to assume personal responsibility.
Fundamental principles: 1. Simultaneous treatment of both disorders: Patients with BPD frequently use addictive substances to control tensions and emotions, in the same way they use self-harm, for example. Would only the self-harm behavior be addressed, an increased use of additive substances would probably occur, and vice versa (shifting of symptoms). For this reason, it is recommended to simultaneously treat the dependence disorder and BPD.
2. Patient attachment: A key principle is the systematic use of attachment strategies. These strategies foster regular participation even of patients who find it very difficult to do so.
3. Dialectical abstinence: The principle of dialectical abstinence enables the therapist to keep the focus on what is possible for the individual patient instead of demanding radical changes in their consumption behavior. Abstinence is the ultimate goal of the treatment which is to be achieved step-by-step along the therapeutic path. Therefore, vital skills are trained before the substance is withdrawn to ensure that during early abstinence, in the event of a crisis patients can resort to skills they have already learnt.
4. Skills training: Learning a battery of specific skills to cope with addictive behavior.
Implementation: DBT-SUD consists of:
weekly individual therapy (the psychotherapy processes are worked upon and the further therapeutic steps are planned and coordinated),
weekly educative group therapy for skills training,
visiting self-help groups and addiction counseling facilities,
telephone coaching for patients, and
supervision for therapists.
Key to the therapy’s efficacy are the lived eight basic assumptions of DBT for therapists and the targeted use of the six distinct validation strategies stated for DBT-SUD.
Efficacy: So far, DBT has been evaluated in two RCTs (Table 1) in which significant improvements of the level of general functioning and addiction-related problems were found. The findings regarding treatment compliance are contradictory. The available data indicate that patients from the DBT-SUD group make more use of group therapy compared with patients from the control group. In addition, it was found that DBT patients provided more plausible information about their actual substance intake, showing a higher correlation with objective urine sample data (Table 1).
Table 1. Randomized controlled trials evaluating the efficacy of dialectical behavior therapy in patients with borderline personality disorder and substance use disorder (DBT-SUD).
| Patient population | Interventions | Duration (months) | Findings: BPD problems | Findings: Addiction problems | ||
|---|---|---|---|---|---|---|
| DBT-SUD | ||||||
| Linehan et al. 1999 (24) |
N = 28 female patients with BPD + addiction: multiple substances (74%), cocaine (58%), alcohol (52%), opioids (21%), cannabis (14%), methamphetamine (11%) |
DBT-SUD | TAU | 12 | improvement of general level of functioning, SMD 1.78 Fewer dropouts, RR 0.51 |
more abstinence days, SMD 0.81, ES 1.03 more negative urine samples, SMD 0.31,ES 0.75 |
| Linehan et al. 2002 (25) |
N = 23 female patients with BPD + opioid dependence |
DBT-SUD | CVT+ 12ST | 12 | tendency towards more dropouts or not starting treatment for DBT (3 out of 11), none in CVT + 12ST group in DBT patients more frequent participation in groups (SMD 1.07) and individual therapy (SMD 1.61), marginally reduced participation in individual therapy (SMD −0.05) |
fewer positive urine samples with DBT (opiate: SMD –0.63, other drugs: SMD −0.21) |
BPD, borderline personality disorder; CVT+12ST, controls: Comprehensive Validation Therapy + 12-step program of Narcotics Anonymous; DBT-SUD, Dialectical Behavior Therapy for Substance Use Disorders (DBT-SUD); ES, effect sizes; RR, risk ratio; SMD, standardized mean difference; SHB, self-harm behavior; TAU, treatment-as-usual; bold: significant effects (95% confidence interval)
Note for clinicians: It is advantageous to start the treatment program when patients are not in a state of severe crisis and do not use large amounts of substances, since learning new skills to regulate their emotions and addictions requires an increased learning ability of the affected individuals. It is possible to search treatment spaces in Germany using, for example, the contact form of the DBT umbrella association: www.dachverband-dbt.de. (References: 23–25, manual in 26).
Dynamic Deconstructive Psychotherapy (DDP)— DDP is one of the depth-psychological methods.
Fundamental principles: DDP combines elements of neuroscience, object relations theory, and Derrida’s deconstruction philosophy. The treatment of BPD symptoms and the dependence disorder is provided at the same time.
Implementation: Treatment is provided in four phases over a period of 12 months in weekly individual therapy sessions.
In phase 1, the focus is on establishing therapeutic alliance. Patients learn to identify and verbalize emotional experiences. In phase 2, the affected individuals analyze their interpersonal emotional experiences and become aware of their polarizing evaluations. In phase 3 and 4, patients learn to become aware of their subjective interpretation and make their judgments closer to reality. In phase 4, the patients learn to distance themselves from idealizing phantasies.
Efficacy: Currently, one study on DDP is available (Table 2), showing moderately positive, but not statistically significant effects on symptoms of both BPD and addiction. The dropout rate was lower for DDP (Table 2).
Table 2. Randomized controlled trials evaluating the efficacy of dynamic deconstructive psychotherapy (DDP) in patients with borderline personality disorder and addiction.
| Patient population | Interventions | Duration (months) | Findings: BPD problems | Findings: Addiction problems | ||
|---|---|---|---|---|---|---|
| DDP | ||||||
| Gregory et al. 2008 (27) |
N = 30 male (20%) and female patients (80%) with BPD + alcohol dependence |
DDP | TAU | 12 | BPD severity SMD −0.44 patient with SHB RR 0.89 dissociative symptoms SMD 0.25 depressed mood SMD −0.52 dropout rate RR 0.83 |
Patients with alcohol use RR 0.80 |
BPD, borderline personality disorder; DDP, Dynamic Deconstructive Psychotherapy; SMD, standardized mean difference; RR, risk ratio; TAU, treatment-as-usual; SHB, self-harm behavior.
Note for clinicians: DDP is almost unknown in Germany; a central search tool for treatment spaces is not available. (References: 27–29, manual in 30).
Dual Focus Schema Therapy (DFST)—Schema therapy makes use of depth psychological and behavioral therapy elements. The term “maladaptive schema” refers to unfavorable cognitive, emotional and behavioral reflexes shaped by memories, feelings, thoughts, and behavioral patterns. Such schemas are activated by key stimuli in typical situations, guiding behavior even where they are, directly or indirectly, detrimental to the affected individual.
Fundamental principles: Here again, the treatment of BPD symptoms and the dependence disorder is provided at the same time. DFST postulates:
that failed attempts to satisfy important basic needs may lead to the development of maladaptive schemas and harmful coping strategies in young people.
the existence of 18 distinct maladaptive schemas, each of which can be assigned to 1 of 5 overarching clusters. The patient–therapist team aims at initially identifying and inhibiting these schemas, followed by perceiving the underlying basic needs and satisfying them in an adequate manner.
the subclassifications of personality disorders have no bearing on the work with schema therapy. Based on this approach, DFST logically interprets substance use as a maladaptive strategy for coping with moods or conflicts.
Implementation: Treatment with DFST combines personality-related with pragmatic addiction-specific strategies. These include, besides relapse prevention training, skills training with regard to interpersonal relationships, emotion regulation, stimulus control, and coping with craving, as well as methods to change schemas and coping strategies. The implementation takes place in individual therapy and skills training sessions.
Efficacy: Presently, 3 RCTs on DFST are available in which DFST is compared with general (31) and personalized (33) drug counseling and an Alcoholics Anonymous 12-step program modified for opioid dependent patients (32), respectively. All studies showed (uniformly across all groups) very high dropout rates of about 60%, which certainly needs to be interpreted against the background of each treatment setting (homeless drop-in center, forensic hospital). Consequently, there is little point in undertaking quantitative group comparisons between these studies. Table 3 provides a solely narrative overview; however, these findings should be interpreted with great caution (Table 3).
Table 3. Randomized controlled trials evaluating the efficacy of dual focus schema therapy (DFST) in patients with borderline personality disorder and addiction.
| Patient population | Interventions | Duration (months) | Findings: BPD problems | Findings: Addiction problems | ||
|---|---|---|---|---|---|---|
| DFST | ||||||
| Ball et al. 2005 (31) |
N = 52 homeless men (94%) and women (6%) with predominately combined PD (Cluster A: 88%, Cluster B: 74%, Cluster C: 85%; 51% with BPD) + substance abuse or dependence: alcohol (50%), cocaine (23%), heroine (14%), cannabis (14%) | DFST | Drug counseling | 6 | very high dropout rate in both groups (60%), thus no quantitative analyses reported and not sufficient raw data available for reanalysis of effect sizes | |
| Ball 2007 (32) |
N = 30 men (50%) and women (50%) with predominately combined PD + opioid dependence; most frequent PD: antisocial (63%), BPD (57%) | DFST | 12 FT | 6 | not sufficient raw data available for reanalysis of effect sizes; the authors report the following: | |
| stronger therapeutic alliances in DFST group, better mood improvement with 12FT | more rapid decreases in substance use in the DFST group | |||||
| WARNING: Proportion of dropouts unclear | ||||||
| Ball et al. 2011 (33) |
N = 105 men (79%) and women (21%) with PD (54% paranoid, 50% antisocial PD, 30% BPD) in in-patient forensic setting + history of substance abuse/dependence | DFST | Drug counseling | 6 | high dropout rate (overall 58%); not sufficient raw data available for reanalysis of effect sizes; the authors report the following: | |
| less reduction in general burden and dysphoria with DFST | corresponding data were not collected | |||||
BPD, borderline personality disorder;
12 FT, 12-Step Facilitation Therapy in line with the 12-step program of the National Institute on Alcohol Abuse and Alcoholism (NIAAA);
DFST, Dual Focus Schema Therapy; TAU, treatment-as-usual; PD personality disorder
Note for clinicians: To search for treatment spaces for DFST in Germany, the following website is available: www.verhaltenstherapie.de (31– 33).
Conclusion
Only few data are available on the efficacy of pharmacotherapy or psychotherapy in this patient population. Recommendations for longer-term pharmacotherapy are limited to the standard addiction medicine approaches and the treatment of emotion regulation disorders. First steps towards a systematic treatment using psychotherapy have been taken; however, further therapy research based on randomized controlled trials with larger patient populations is needed. It would, in particular, be desirable that independent groups of researchers evaluate the various methods. Despite the very limited data presently available, it should be recommended to use DBT-SUD, DDP or DFST, at least as methods of psychotherapy. All available studies report positive developments for symptoms of both BPD and addiction with treatment over time, but it is currently not possible to postulate that a certain therapy should be preferred over others because of its superiority. Likewise, the absence of solid evidence (compare DFST) should not be misinterpreted as proof of their lack of efficacy.
All 3 approaches have in common:
the therapists’ consistently positive attitude of appreciation,
the therapists’ high levels of expertise in the treatment of BPD and dependence disorders,
the separate offering of skills training and sociotherapy, and
the simultaneous treatment of both disorders.
Therapists offering one of the three methods discussed above can achieve better treatment outcomes as these psychotherapies have a systematic treatment approach for which special scientific and supervisory expertise is at hand.
Footnotes
Conflict of interest statement
Prof. Bermpohl has received reimbursements for congress participation fees from Lilly.
Prof. Lieb, Dr. Kienast and Ms. Stoffers declare that no conflict of interest exists.
References
- 1.Trull TJ, Jahng S, Tomko RL, Wood PK, Sher KJ. Revised NESARC personality disorder diagnoses: gender, prevalence, and comorbidity with substance dependence disorders. J Pers Disord. 2010;24:412–426. doi: 10.1521/pedi.2010.24.4.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tomko RL, Trull TJ, Wood PK, Sher KJ. Characteristics of borderline personality disorder in a community sample: Comorbidity, treatment utilization, and general functioning. J Pers Disord. 2013 doi: 10.1521/pedi_2012_26_093. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Skodol AE, Bender DS. Why are women diagnosed borderline more than men? Psychiatr Q. 2003;74:349–360. doi: 10.1023/a:1026087410516. [DOI] [PubMed] [Google Scholar]
- 4.Barth J. Subgruppendifferenzierung bei Patienten mit Borderline-Persönlichkeitsstörung unter Berücksichtigung von dimensionaler Persönlichkeitsausprägung, Komorbiditäten und Symptomausprägung. Dissertation Ruprecht-Karls-Universität Heidelberg, Medizinische Fakultät Mannheim. 2007 [Google Scholar]
- 5.Zanarini MC, Frankenburg FR, Dubo ED, et al. Axis I comorbidity of borderline personality disorder. Am J Psychiatry. 1998;155:1733–1739. doi: 10.1176/ajp.155.12.1733. [DOI] [PubMed] [Google Scholar]
- 6.Zikos E, Gill KJ, Charney DA. Personality disorders among alcoholic outpatients: prevalence and course in treatment. Can J Psychiatry. 2010;55:65–73. doi: 10.1177/070674371005500202. [DOI] [PubMed] [Google Scholar]
- 7.Morgenstern J, Langenbucher J, Labouvie E, Miller KJ. The comorbidity of alcoholism and personality disorders in a clinical population: prevalence rates and relation to alcohol typology variables. J Abnorm Psychol. 1997;106:74–84. doi: 10.1037//0021-843x.106.1.74. [DOI] [PubMed] [Google Scholar]
- 8.Preuss UW, Koller G, Barnow S, Eikmeier M, Soyka M. Suicidal behavior in alcohol-dependent subjects: the role of personality disorders. Alcohol Clin Exp Res. 2006;30:866–877. doi: 10.1111/j.1530-0277.2006.00073.x. [DOI] [PubMed] [Google Scholar]
- 9.Powell G, Peveler R. Nature and prevalence of personality disorders amongst patients receiving treatment for alcohol dependence. Journal of Mental Health. 1996;5:305–314. [Google Scholar]
- 10.Verheul R, Van den Brink W, Hartgers C. Personality disorders predict relapse in alcoholic patients. Addict Behav. 1998;23:869–882. doi: 10.1016/s0306-4603(98)00065-3. [DOI] [PubMed] [Google Scholar]
- 11.Wilson ST, Fertuck EA, Kwitel A, Stanley MC, Stanley B. Impulsivity, suicidality and alcohol use disorders in adolescents and young adults with borderline personality disorder. Int J Adolesc Med Health. 2006;18:189–196. doi: 10.1515/ijamh.2006.18.1.189. [DOI] [PubMed] [Google Scholar]
- 12.Tull MT, Gratz KL. The impact of borderline personality disorder on residential substance abuse treatment dropout among men. Drug Alcohol Depend. 2012;121:97–102. doi: 10.1016/j.drugalcdep.2011.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krampe H, Wagner T, Stawicki S, et al. Personality disorder and chronicity of addiction as independent outcome predictors in alcoholism treatment. Psychiatr Serv. 2006;57:708–712. doi: 10.1176/ps.2006.57.5.708. [DOI] [PubMed] [Google Scholar]
- 14.Coffey SF, Schumacher JA, Baschnagel JS, Hawk LW, Holloman G. Impulsivity and risk-taking in borderline personality disorder with and without substance use disorders. Personal Disord. 2011;2:128–141. doi: 10.1037/a0020574. [DOI] [PubMed] [Google Scholar]
- 15.Lee HJ, Bagge CL, Schumacher JA, Coffey SF. Does comorbid substance use disorder exacerbate borderline personality features? A comparison of borderline personality disorder individuals with vs. without current substance dependence. Personal Disord. 2010;1:239–249. doi: 10.1037/a0017647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van den Bosch LM, Verheul R, Van den Brink W. Substance abuse in borderline personality disorder: clinical and etiological correlates. J Pers Disord. 2001;15:416–424. doi: 10.1521/pedi.15.5.416.19201. [DOI] [PubMed] [Google Scholar]
- 17.Ross S, Dermatis H, Levounis P, Galanter M. A comparison between dually diagnosed inpatients with and without Axis II comorbidity and the relationship to treatment outcome. Am J Drug Alcohol Abuse. 2003;29:263–279. doi: 10.1081/ada-120020511. [DOI] [PubMed] [Google Scholar]
- 18.Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Axis I comorbidity in patients with borderline personality disorder: 6-year follow-up and prediction of time to remission. Am J Psychiatry. 2004;161:2108–2114. doi: 10.1176/appi.ajp.161.11.2108. [DOI] [PubMed] [Google Scholar]
- 19.McMain S, Sayrs JHR, Dimeff L, Linehan MM. Dialectical Behavior Therapy in Clinical Practice. Dialectical behavior therapy for individuals with borderline personality disorder and substance dependence. In: Dimeff L, Koerner K, editors. New York: The Guilford Press; 2007. pp. 145–173. [Google Scholar]
- 20.Stoffers JM, Völlm BA, Rücker G, Timmer A, Huband N, Lieb K. Psychological therapies for people with borderline personality disorder. Cochrane Database Syst Rev. 2012;8 doi: 10.1002/14651858.CD005652.pub2. CD005652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stoffers J, Völlm BA, Rücker G, Timmer A, Huband N, Lieb K. Pharmacological interventions for borderline personality disorder. Cochrane Database Syst Rev. 2010;6 doi: 10.1002/14651858.CD005653.pub2. CD005653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ralevski E, Ball S, Nich C, Limoncelli D, Petrakis I. The impact of personality disorders on alcohol-use outcomes in a pharmacotherapy trial for alcohol dependence and comorbid Axis I disorders. Am J Addict. 2007;16:443–449. doi: 10.1080/10550490701643336. [DOI] [PubMed] [Google Scholar]
- 23.Mayer-Bruns F, Lieb K, Dannegger E, Jacob GA. Dialektisch Behaviorale Therapie in der stationären Alkoholentwöhnung. Nervenarzt. 2005;76:339–343. doi: 10.1007/s00115-004-1860-y. [DOI] [PubMed] [Google Scholar]
- 24.Linehan MM, Schmidt H, 3rd, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. Am J Addict. 1999;8:279–292. doi: 10.1080/105504999305686. [DOI] [PubMed] [Google Scholar]
- 25.Linehan MM, Dimeff LA, Reynolds SK, et al. Dialectical behavior therapy versus comprehensive validation therapy plus 12-step for the treatment of opioid dependent women meeting criteria for borderline personality disorder. Drug Alcohol Depend. 2002;671:3–26. doi: 10.1016/s0376-8716(02)00011-x. [DOI] [PubMed] [Google Scholar]
- 26.Kienast T. Modul Umgang mit Sucht. In: Bohus M, Wolf-Arehult M, editors. Interaktives Skillstraining für Borderline Patienten. 2nd edition. Stuttgart: Schattauer Verlag; 2013. pp. 347–383. [Google Scholar]
- 27.Gregory RJ, Chlebowski S, Kang D, et al. A controlled trial for psychodynamic psychotherapy for co-ocurring borderline personality disorder and alcohol use disorder. Psychotherapy (Chic) 2008;45:28–41. doi: 10.1037/0033-3204.45.1.28. [DOI] [PubMed] [Google Scholar]
- 28.Gregory RJ, Remen AL, Soderberg M, et al. A Controlled Trial of Psychodynamic Psychotherapy for Co-Occurring Borderline Personality Disorder and Alcohol Use Disorder: Six-Month Outcome. J Am Psychoanal Assoc. 2009;57:199–204. doi: 10.1177/00030651090570011006. [DOI] [PubMed] [Google Scholar]
- 29.Gregory RJ, DeLucia-Deranja E, Mogle JA. Dynamic deconstructive psychotherapy versus optimized community care for borderline personality disorder co-occurring with alcohol use disorders: a 30-month follow-up. J Nerv Ment Dis. 2010;198:292–298. doi: 10.1097/NMD.0b013e3181d6172d. [DOI] [PubMed] [Google Scholar]
- 30.Gregory RJ. Remediation for Treatment-Resistant Borderline Personality Disorder: manual of Dynamic Deconstructive Psychotherapy. www.upstate.edu/psych/education/psychotherapy/pdf/ddp_manual.pdf. (last accessed on 20 February 2014) [Google Scholar]
- 31.Ball SA, Cobb-Richardson P, Connolly AJ, Bujosa CT, O’Neall TW. Substance abuse and personality disorders in homeless drop-in center clients: symptom severity and psychotherapy retention in a randomized clinical trial. Compr Psychiatry. 2005;46:371–379. doi: 10.1016/j.comppsych.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 32.Ball SA. Comparing individual therapies for personality disordered opioid dependent patients. J Pers Disord. 2007;21:305–321. doi: 10.1521/pedi.2007.21.3.305. [DOI] [PubMed] [Google Scholar]
- 33.Ball SA, Maccarelli LM, LaPaglia DM, Ostrowski MJ. Randomized trial of dual-focused vs. single-focused individual therapy for personality disorders and substance dependence. J Nerv Ment Dis. 2011;199:319–328. doi: 10.1097/NMD.0b013e3182174e6f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ball SA. Manualized treatment for substance abusers with personality disorders: dual focus schema therapy. Addict Behav. 1998;23:883–891. doi: 10.1016/s0306-4603(98)00067-7. [DOI] [PubMed] [Google Scholar]