Abstract
Objectives
To measure changes in prevalence and predictors of home smoking bans (HSB) among smokers in four European countries after the implementation of national smoke-free legislation.
Design
Two waves of the International Tobacco Control (ITC) Policy Evaluation Project Europe Surveys, which is a prospective panel study. Pre- and post-legislation data was used from Ireland, France, Germany, and the Netherlands. Two pre-legislation waves from UK were used as control.
Participants
4,634 respondents from the intervention countries and 1,080 from the control country completed both baseline and follow-up, and were included in the present analyses.
Methods
Multiple logistic regression models to identify predictors of having or of adopting a total HSB, and Generalised Estimating Equation (GEE) models to compare patterns of change after implementation of smoke-free legislation to a control country without such legislation.
Results
Most smokers had at least partial smoking restrictions in their home, but the proportions varied significantly between countries. After implementation of national smoke-free legislation, the proportion of smokers with a total HSB increased significantly in all four countries. Among continuing smokers the number of cigarettes smoked per day either remained stable or decreased significantly. Multiple logistic regression models indicated that having a young child in the household and supporting smoking bans in bars were important correlates of having a pre-legislation HSB. Prospective predictors of imposing a HSB between survey waves were planning to quit smoking, supporting a total smoking ban in bars, and the birth of a child. GEE models indicated that the change in total HSB in the intervention countries was greater than in the control country.
Conclusions
The findings suggest that smoke-free legislation does not lead to more smoking in smokers’ homes. On the contrary, our findings demonstrate that smoke-free legislation may stimulate smokers to establish total smoking bans in their homes.
Keywords: impact of smoke-free legislation, home smoking restrictions, secondhand smoke, prospective study
INTRODUCTION
For children, exposure to secondhand smoke (SHS) is an important health risk. SHS impairs their respiratory system and can cause severe and chronic diseases such as asthma and bronchitis.[1, 2] Especially in early childhood, the home environment is usually the main source of exposure to SHS.[3] But while workplace and public smoking bans have been proven to be successful in reducing exposure to SHS in public areas,[4] private homes cannot be directly targeted by measures such as smoke-free legislation. They might nevertheless be indirectly affected.
Two competing hypotheses regarding possible influences of public smoking bans on smoking at home have been put forward.[5] According to the displacement hypothesis or “last refuge model”, smoking bans in public places would lead to more smoking in the home and hence to increased SHS exposure of non-smoking family members and children. Under this hypothesis, an increase in SHS-related diseases would be expected as an unintended detrimental consequence of smoke-free legislation. The social diffusion hypothesis, in contrast, suggests that more restrictive rules regarding smoking in public places would increase the likelihood of householders imposing voluntary home smoking restrictions.
Whereas two empirical studies from the US and from Hong Kong support the displacement hypothesis,[6, 7] recent studies from Scotland, Wales, Ireland, and New Zealand evaluating the effects of smoke-free legislation found no increase in exposure to SHS in non-smoking family members and children due to displacement of smoking into the private home, and no increase of smoking at home.[3, 8-16] Of these studies, only two are based on longitudinal data.[9, 12]
The recent implementation of pertinent legislation in several European countries provides an unprecedented opportunity to examine this topic in a broader European setting in order to allow better informed decisions by policymakers. Unique prospective data from the Europe Surveys of the International Tobacco Control (ITC) Policy Evaluation Project were analysed, based on representative surveys in Ireland, France, Germany, and the Netherlands conducted shortly before and after the implementation of smoke-free legislation. We examined the numbers of cigarettes smoked at home, and prevalence and predictors of home smoking bans (HSB) before and after implementation of smoke-free legislation. Additionally, the pattern of change in the rate of HSB in these countries was compared to pre-legislation data from the United Kingdom (UK) as a control country.
METHODS
Study design and study participants
The ITC Europe Surveys are part of the ITC Project (www.itcproject.org), which is committed to evaluating the psychosocial and behavioural effects of tobacco control policies throughout the world. All ITC surveys are based on the same conceptual framework and methods and use standardised survey questionnaires.[17, 18]
The ITC Europe Surveys are conducted with probability samples of smokers aged 18 years and older, with smokers being defined as having smoked at least 100 cigarettes in their lifetime and currently smoking at least once per month. In Ireland, France and Germany, respondents were recruited and questioned using random digit dialling (RDD) and computer-assisted telephone interviews (CATI) only. In the Netherlands, the sample consisted of a small RDD CATI sample and a larger computer-assisted web interview sample (CAWI). The CAWI sample was drawn from a large probability-based database with potential respondents who had been recruited by phone or mail and who had indicated their willingness to participate in research on a regular basis. Whereas the two Dutch samples showed small differences in socio-demographics and smoking behaviour,[19] there were no significant differences with regard to HSB prevalence at pre-legislation (χ2=4.46, p=0.11) or post-legislation (χ2=1.77, p=0.41); the samples were thus pooled for the analyses.
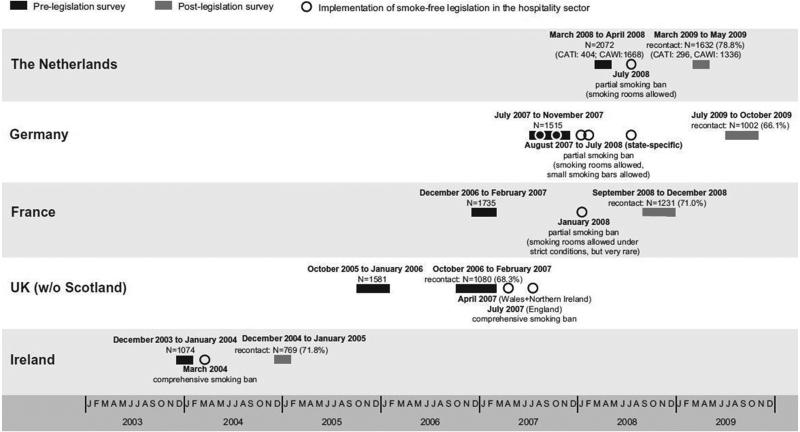
Respondents were first interviewed before implementation of the national smoke-free legislation (pre-legislation surveys). The fieldwork of the post-legislation measurements started about 8 months after implementation of the hospitality sector smoke-free legislation in Ireland, France and the Netherlands (figure 1). As the starting date of the smoke-free legislation in Germany varied from state to state, the time gap between introduction of the state legislation and post-legislation survey varied from 12 to 23 months.
Figure 1.
Fieldwork periods, sample sizes and follow-up rates of ITC surveys, and implementation dates and characterization of smoke-free legislation
The analyses presented here were based on the longitudinal samples, i.e. only on those respondents who had been surveyed both pre- and post-legislation. Of 6,393 smokers interviewed pre-legislation, 4,634 (72.5%) could be followed up after the implementation of the smoke-free legislation. Country-specific follow-up rates varied between 66 and 79 percent (figure 1). For some analyses, sample sizes were smaller due to missing values for some covariates.
In order to address the question of causality, we employed a quasi-experimental design in additional analyses. We chose UK as a control country, the only other European country in the ITC Project and the only one for which several pre-legislation waves are available. In the UK, Scotland introduced a comprehensive smoking ban in March 2006, Wales and Northern Ireland followed in April 2007, and England enacted its ban in July 2007. In order to have a pre-legislation observation period as comparable as possible to the pre- to post-legislation period in the other countries, we used waves 4 (October 2005 – January 2006) and 5 (October 2006 – February 2007) of the ITC UK survey, but excluded Scotland from the analyses, because they implemented their smoke-free legislation between these two waves. From 1,581 smoking non-Scotland respondents of ITC UK wave 4, 1,080 could be followed up at wave 5 and were used for the analyses (follow-up rate: 68.3%).
In order to assess the potential effect of attrition bias, non-responder analyses were conducted by estimating logistic regression models with the full baseline samples, and with being lost to follow-up as dependent variable, and with home smoking restrictions and all covariates as independent variables. In the intervention countries, these analyses yielded higher odds of being lost to follow-up in younger age groups (age 18-24 versus age 55+: OR=1.79, 95%-CI=1.43-2.24; age 25-39 versus age 55+: OR=1.54, 95%-CI=1.26-1.88) and lower odds in married respondents (OR=0.68, 95%-CI: 0.60-0.78). In the control country UK, younger age groups also had comparably higher odds of being lost to follow-up (age 18-24 versus age 55+: OR=2.39, 95%-CI=1.41-4.03; age 25-39 versus age 55+: OR=1.46, 95%-CI=1.02-2.10). Additionally, higher odds were found among UK respondents with children aged 6 to 12 (OR=1.48, 95%-CI=1.05-2.07) and with children aged 13 to 17 (OR=1.74, 95%-CI=1.21-2.50), compared to respondents without children in the household. Furthermore, country-specific non-responder analyses showed that French respondents with home smoking restrictions pre-legislation were less likely to be lost to follow-up (total HSB versus no restrictions: OR=0.56, 95%-CI=0.38-0.81; partial restrictions versus no restrictions: OR=0.57, 95%-CI=0.42-0.77).
Measures and outcomes
The study included relevant socio-demographic variables, such as gender, age, marital status, education and the age of children living in the household. A binary variable referring to the birth of a child between the two survey waves was derived by using pre- and post-legislation information about the age of children living in the respondent's household. Because the Irish survey did not ask about children in the household at the first post-legislation survey, this item of information was derived from the second post-legislation survey (fieldwork period: February – March 2006, i.e. 14 months after the first post-legislation survey).
Smoking-related questions of particular relevance to the present analyses were cigarette consumption, the Heaviness of Smoking Index (HSI),[20] intention to quit smoking, and support for a bar smoking ban. The amount of cigarettes smoked at home was obtained with asking “When you are spending an evening at home, about how many cigarettes do you smoke inside your home during the evening?”, and was used as a continuous variable. Unfortunately, this measure was not available for Ireland and UK. The frequency of bar visits was used to assess to what extent respondents would be affected by the smoke-free policy. Awareness of the harm of SHS was measured by reported agreement with the statement “Cigarette smoke is dangerous to non-smokers”. For Ireland, the comparably phrased statement “Your cigarette smoke is dangerous to those around you” was used.
The rules for smoking at home were assessed by asking, “Which of the following statements best describes smoking inside your home (inside the home, not on the balcony or terrace)?” Response choices in France, Germany and the Netherlands were: “Smoking is allowed anywhere inside your home”, “Smoking is allowed in some rooms inside your home”, “Smoking is never allowed anywhere inside your home”, and “Smoking is not allowed inside your home except under special circumstances”. In Ireland and the UK the response choices were slightly different: “Smoking is allowed anywhere inside your home”, “Smoking is never allowed anywhere inside your home”, and “Something in between”. For the bivariate analyses these statements were translated into three categories: total home smoking ban (HSB), partial restrictions, and no restrictions. For the multivariate analyses on having or adopting a HSB, a binary variable was constructed. The statement “Smoking is never allowed anywhere inside your home” qualified as having a HSB. Those respondents reporting having partial or no home smoking restrictions were regarded as having no HSB.
Statistical analyses
Percentages reported for country-specific estimates of home smoking restrictions and arithmetic means of cigarette consumption were weighted by age and sex to each country's resident smoking population of the year of the respective survey. To assess whether changes in home smoking restrictions were due to smoking cessation between survey waves, the percentages were also reported for continuing smokers. McNemar-Bowker-tests of symmetry were used to test for changes in prevalence of home smoking restrictions. Paired t-tests were used to test for changes in mean cigarette consumption.
In order to identify factors associated with the presence or adoption of HSB in smokers, multiple logistic regression models were computed. For predictors of a HSB at the time of the pre-legislation survey, reporting a HSB at this survey was the dependent variable. For predictors of adopting a HSB, reporting a HSB at the post-legislation survey was the dependent variable, while the sample was restricted to those who had not implemented a HSB at the pre-legislation survey. Except for “newborn child”, all predictor variables refer to the pre-legislation measurement.
To test whether patterns of changes in HSB prevalence from pre- to post-legislation in the four countries examined differed from the control country (UK) in a comparable period of time, Generalised Estimating Equations (GEE) models [21, 22] predicting the presence of a HSB (binomial distribution; logit link function; exchangeable correlation structure) were computed separately for Ireland, France, Germany, and the Netherlands, each time including UK as control. The models were adjusted for socio-demographic time-invariant covariates reported at baseline (age, gender, education, country) as well as for socio-demographic time-varying covariates reported at each measurement (wave, age of youngest child in the household, marital status). The inclusion of country x wave-interaction allowed us to test whether the change in the presence of HSB over time significantly differed from the change in the UK as the no-legislation control country.
The statistical package SAS 9.2 was used for all analyses.
RESULTS
Prevalence of home smoking restrictions
Most smokers had at least partial smoking restrictions in their home at the pre-legislation survey (table 1). The proportion of smokers with no home smoking restrictions was lowest in Germany and in France; and both countries accordingly also had the highest proportion of smokers with a total HSB. By the post-legislation measurement, there was an increase in the proportion of total HSB in all four countries among the baseline smokers and a decrease in the proportion with no smoking restrictions. The relative increases of total HSB were 22 % in the control country UK. In the intervention countries, it was 25 % in Ireland, 17 % in France, 38 % in Germany, and 28 % in the Netherlands. The changes in the proportions followed a similar pattern in the intervention countries when analysing only continuing smokers, albeit with somewhat smaller relative increases, suggesting that these changes were not merely a surrogate for smoking cessation occurring between the survey waves. The changes in proportions between the time points were statistically significant (p<0.05) in each country when analysing all baseline smokers, and in all countries but UK after restriction to continuing smokers. For UK, this suggests that the observed changes in home smoking restrictions in the overall sample mainly occurred among smokers who quit between the survey waves.
Table 1.
Home smoking restrictions and smoking behaviour among smokers, pre-legislation (pre-law) and post-legislation (post-law) (in %)
| Intervention countries | Control country | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ireland | France | Germany | Netherlands | UK | |||||||
| Pre-law | Post-law | Pre-law | Post-law | Pre-law | Post-law | Pre-law | Post-law | Pre-law 1 | Pre-law 2 | ||
| Home smoking restrictions among baseline smokers | N | 767 | 1,231 | 1,000 | 1,627 | 1,077 | |||||
| % total home smoking ban (HSB) | 17.0 | 21.3 | 24.1 | 28.2 | 29.7 | 40.9 | 14.6 | 18.7 | 24.0 | 29.3 | |
| % partial restrictions | 49.4 | 50.3 | 61.5 | 60.3 | 55.7 | 47.8 | 59.5 | 60.8 | 50.8 | 48.9 | |
| % no restrictions | 33.6 | 28.4 | 14.4 | 11.6 | 14.6 | 11.3 | 25.9 | 20.5 | 25.2 | 21.8 | |
| P-value** | 0.003 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
| Home smoking restrictions among continuing smokers | N | 597 | 1,067 | 875 | 1,443 | 907 | |||||
| % total home smoking ban (HSB) | 14.6 | 16.1 | 23.0 | 25.6 | 27.7 | 38.2 | 14.2 | 17.1 | 23.4 | 25.4 | |
| % partial restrictions | 47.2 | 51.0 | 61.6 | 62.0 | 56.3 | 49.6 | 59.5 | 61.0 | 51.3 | 50.5 | |
| % no restrictions | 38.2 | 32.9 | 15.4 | 12.4 | 16.1 | 12.2 | 26.3 | 22.0 | 25.3 | 24.0 | |
| P-value** | 0.031 | 0.003 | <0.0 | 01 | <0.001 | 0.201 | |||||
| Cigarettes smoked per day at home among continuing smokers with no HSB at both measurements | N | -* | 580 | 444 | 1,105 | -* | |||||
| Arithmetic mean | -* | -* | 5.6 | 5.5 | 6. 6 | 6. 0 | 6.4 | 5.9 | -* | -* | |
| P-value*** | -* | 0.469 | <0.001 | <0.001 | -* | ||||||
| Cigarettes smoked per day among continuing smokers | N | 594 | 1,067 | 871 | 1,428 | 907 | |||||
| Arithmetic mean | 19.3 | 18.0 | 12.6 | 12.5 | 15.5 | 14.7 | 15.6 | 15.2 | 17.8 | 16.2 | |
| P-value*** | <0.001 | 0.777 | <0.001 | 0.005 | 0.121 | ||||||
Question was not asked in the Irish and UK surveys.
The p-value refers to McNemar-Bowker-tests of symmetry.
The p-value refers to paired t-tests.
Changes in smoking at home
In order to test whether displacement took place among continuing smokers, we also tested for changes in cigarette consumption (table 1). Among continuing smokers with no HSB at both time points, the average number of cigarettes smoked at home decreased significantly in Germany (0.60, 0.31-0.88) and the Netherlands (0.52, 0.34-0.69). Cigarette consumption per day decreased significantly (p<0.05) in Ireland (mean decrease in cigarettes: 1.29, 95% CI: 0.67-1.91), Germany (0.79, 0.45-1.13) and the Netherlands (0.39, 0.12-0.65)).
Predictors of home smoking bans
Smokers who were male, younger, or married were more likely to report having a HSB at the pre-legislation survey (table 2), and also smokers supporting a bar smoking ban, and those strongly agreeing that cigarette smoke is dangerous to others were more likely to report having a HSB. The presence of young children in the household was a strong predictor of HSB with a pronounced dose-response relationship with age of child: the younger the child, the greater the likelihood of having a HSB. Heaviness of smoking was inversely related to having a HSB. At pre-legislation, HSBs were significantly less likely among smokers from France, the Netherlands and Ireland than among smokers from Germany.
Table 2.
Correlates of having a home-smoking ban (HSB) at the pre-legislation survey and prospective predictors of adopting a HSB between the pre- and post-legislation survey, multiple logistic regression analyses
| Predictor variable* | Stratum | Having a HSB at the pre-legislation survey among baseline smokers | Adopting a HSB between pre- and post-legislation survey among baseline smokers with no HSB at baseline | Adopting a HSB between pre- and post-legislation among continuing smokers with no HSB at baseline | |||
|---|---|---|---|---|---|---|---|
| N=4461, events=929 | N=3528, events=446 | N=3072, events=322 | |||||
| Events % | Predictors Adjusted OR (95% CI) | Events % | Predictors Adjusted OR (95% CI) | Events % | Predictors Adjusted OR (95% CI) | ||
| Gender | Male | 24.5 | 1.78 (1.51-2.10) | 15.3 | 1.66 (1.34-2.05) | 12.7 | 1.60 (1.25-2.05) |
| Female | 17.4 | 1 | 10.4 | 1 | 8.6 | 1 | |
| Age | 18-24 | 27.4 | 2.90 (2.08-4.03) | 14.1 | 1.47 (0.96-2.25) | 11.9 | 1.83 (1.11-3.02) |
| 25-39 | 26.7 | 1.74 (1.30-2.31) | 16.8 | 1.57 (1.11-2.21) | 14.3 | 1.79 (1.19-2.71) | |
| 40-54 | 17.5 | 1.26 (0.96-1.66) | 10.2 | 0.95 (0.69-1.31) | 8.7 | 1.11 (0.76-1.63) | |
| 55+ | 12.8 | 1 | 10.5 | 1 | 7.7 | 1 | |
| Education | Low | 17.5 | 0.97 (0.78-1.21) | 11.3 | 1.04 (0.77-1.39) | 8.7 | 0.88 (0.63-1.25) |
| Moderate | 22.2 | 1.03 (0.84-1.26) | 12.9 | 1.07 (0.81-1.41) | 11.1 | 1.02 (0.74-1.39) | |
| High | 24.1 | 1 | 14.6 | 1 | 12.8 | 1 | |
| Marital status | Married | 22.9 | 1.43 (1.19-1.73) | 13.3 | 1.38 (1.08-1.77) | 11.3 | 1.53 (1.14-2.03) |
| Not married | 19.0 | 1 | 12.1 | 1 | 9.9 | 1 | |
| Age of youngest child in household | <1 | 46.8 | 3.92 (2.54-6.07) | 19.0 | 0.99 (0.47-2.05) | 16.0 | 1.00 (0.43-2.30) |
| 1-5 | 39.4 | 3.06 (2.38-3.93) | 17.5 | 1.11 (0.76-1.61) | 16.7 | 1.39 (0.91-2.12) | |
| 6-12 | 25.2 | 1.77 (1.39-2.25) | 13.4 | 1.05 (0.76-1.46) | 11.5 | 1.11 (0.76-1.62) | |
| 13-17 | 17.9 | 1.12 (0.84-1.49) | 11.1 | 1.01 (0.70-1.47) | 9.5 | 1.07 (0.70-1.64) | |
| No children<18 | 16.0 | 1 | 12.0 | 1 | 9.5 | 1 | |
| Newborn child | Newborn child | - | - | 51.6 | 6.60 (3.83-11.37) | 46.9 | 6.72 (3.63-12.45) |
| No newborn child | - | - | 11.9 | 1 | 9.9 | 1 | |
| Heaviness of smoking** | Index | 0.72 (0.68-0.76) | 0.86 (0.80-0.92) | 0.87 (0.80-0.95) | |||
| Intention to quit | Within 1 month | 23.2 | 1.24 (0.96-1.61) | 16.9 | 1.56 (1.12-2.16) | 13.8 | 1.67 (1.12-2.50) |
| Within 6 months | 22.1 | 1.00 (0.82-1.22) | 16.8 | 1.49 (1.16-1.91) | 13.9 | 1.50 (1.13-2.01) | |
| Not within 6 months/no intention | 20.0 | 1 | 10.7 | 1 | 9.1 | 1 | |
| Support of bar smoking ban | Support of a full ban | 32.4 | 2.12 (1.63-2.76) | 21.8 | 2.28 (1.60-3.26) | 17.9 | 2.34 (1.54-3.56) |
| Support of a partial ban | 19.7 | 1.18 (0.98-1.42) | 12.4 | 1.39 (1.08-1.79) | 10.5 | 1.48 (1.10-1.99) | |
| Against ban | 18.6 | 1 | 10.2 | 1 | 8.4 | 1 | |
| Frequency of bar visits | At least once a week | 20.5 | 0.95 (0.78-1.17) | 13.4 | 1.09 (0.84-1.43) | 10.8 | 1.17 (0.85-1.60) |
| Monthly | 22.5 | 0.95 (0.78-1.17) | 15.0 | 1.21 (0.93-1.59) | 13.6 | 1.44 (1.06-1.96) | |
| Rarely or never | 20.0 | 1 | 10.6 | 1 | 8.3 | 1 | |
| Cigarette smoke is dangerous to others (SHS awareness) | Strongly agree | 26.9 | 1.62 (1.23-2.14) | 15.7 | 2.10 (1.42-3.10) | 13.2 | 1.73 (1.11-2.67) |
| Agree | 19.0 | 1.16 (0.89-1.50) | 13,5 | 1.89 (1.31-2.72) | 10.9 | 1.58 (1.05-2.38) | |
| Don't agree | 12.4 | 1 | 5.8 | 1 | 5.3 | 1 | |
| Country | Netherlands | 16.2 | 0.44 (0.35-0.55) | 8.8 | 0.42 (0.31-0.57) | 7.3 | 0.39 (0.27-0.55) |
| France | 24.2 | 0.43 (0.34-0.55) | 13.9 | 0.46 (0.34-0.63) | 11.9 | 0.45 (0.32-0.64) | |
| Ireland | 13.2 | 0.31 (0.23-0.42) | 12.1 | 0.47 (0.33-0.68) | 8.7 | 0.40 (0.26-0.64) | |
| Germany | 30.2 | 1 | 18.9 | 1 | 16.5 | 1 | |
All independent variables except for “newborn child” refer to baseline. Models included all variables in the table together.
The index ranges from 0 to 6, with higher values indicating higher addiction/heavier smoking.
The prospective predictors of having adopted a HSB at the post-legislation survey (in subjects who did not have a HSB pre-legislation) were generally similar to the predictors of having a HSB at the pre-legislation survey (table 2). Exceptions were the increased odds of newly adopting a HSB at the post-legislation survey among smokers who had reported at the pre-legislation survey an intention to quit within 1 or 6 months. Although the age of the youngest child at baseline was not related to the adoption of a HSB, the birth of a child between waves was a strong predictor.
When the analysis of newly adopting a HSB was restricted to continuing smokers in order to rule out HSB adoption purely being a consequence of smoking cessation, the patterns were generally the same (table 2). However, in this model only, smokers visiting bars on a monthly basis were significantly more likely to adopt a HSB than those rarely visiting bars.
Pattern of change over time and in comparison to control country
Table 3 summarizes the results of the GEE models comparing the intervention countries with the control country, separately for baseline smokers and for continuing smokers. The results for baseline smokers indicate that there was a significant increase in HSB prevalence from baseline to follow-up in all countries, i.e. in countries which introduced smoke-free legislation in the meantime as well as in the control country (UK). The increase was smaller in the control country compared to each of the four intervention countries. Nevertheless, the wave x country-interaction was only significant in the model comparing Germany to UK, indicating that the HSB prevalence increased to a significantly greater extent than it did in the control country.
Table 3.
Results of GEE models estimating the change in HSB prevalence for baseline smokers and for continuing smokersa
| Presence of HSB among baseline smokers | Presence of HSB among continuing smokers | ||
|---|---|---|---|
| Pattern of change | OR (95% CI) | OR (95% CI) | |
| Ireland vs. UK | follow-up vs. baseline | ||
| Ireland | 1.53 (1.24-1.90) | 1.26 (0.97-1.65) | |
| UK | 1.29 (1.11-1.50) | 1.07 (0.91-1.26) | |
| Ireland × wave-interaction | 1.19 (0.92-1.54) | 1.16 (0.86-1.61) | |
| France vs. UK | follow-up vs. baseline | ||
| France | 1.53 (1.32-1.78) | 1.40 (1.18-1.66) | |
| UK | 1.29 (1.11-1.49) | 1.07 (0.91-1.26) | |
| France × wave-interaction | 1.17 (0.96-1.47) | 1.31 (1.04-1.66) | |
| Germany vs. UK | follow-up vs. baseline | ||
| Germany | 1.61 (1.42-1.81) | 1.55 (1.37-1.76) | |
| UK | 1.29 (1.11-1.50) | 1.07 (0.91-1.26) | |
| Germany × wave-interaction | 1.25 (1.03-1.51) | 1.45 (1.17-1.79) | |
| Netherlands vs. UK | follow-up vs. baseline | ||
| Netherlands | 1.34 (1.20-1.51) | 1.22 (1.08-1.38) | |
| UK | 1.29 (1.11-1.50) | 1.07 (0.90-1.26) | |
| Netherlands × wave-interaction | 1.05 (0.86-1.27) | 1.15 (0.93-1.42) |
Models adjusted for socio-demographic time-invariant covariates (age, gender, education, country) and for time-varying covariates (age of youngest child in the household, marital status, wave), and included country × wave-interaction terms. The odds ratios reported for each country estimate the change in HSB prevalence odds between the two waves. The interaction odds ratios are the ratios of these estimates and were used to assess if the change in the respective intervention country was statistically significantly different from the change in the no-legislation control country (UK w/o Scotland). In this table, an interaction OR > 1 indicates that the change was greater in the intervention country compared to the control country.
In the models restricted to continuing smokers, the increase of HSB over time was significant in Germany, France, and the Netherlands, but not in Ireland nor in the control country. In Germany and France, the increase of HSB over time was statistically significantly greater than in the control country (as measured by the country x wave-interaction).
DISCUSSION
This large prospective dataset with pre- and post-smoke-free legislation observations from four European countries provided us with a uniquely comprehensive opportunity to assess effects of smoke-free legislation on home smoking in Europe. No evidence of displacement of smoking into the home after the implementation of national smoke-free legislation could be found. In all four countries, irrespective of the smoke-free legislation being comprehensive or allowing exceptions, the proportions of smokers having no or only partial home smoking restrictions either remained stable or even decreased, whereas the proportions of smokers with total home smoking bans increased. Among continuing smokers, the average number of cigarettes smoked per day decreased in three of the four countries examined, and there also was no rise in the average number of cigarettes smoked at home.
Regarding causality, it is important to assess whether the smoke-free legislation itself facilitated the adoption of home smoking bans, as the growth in the prevalence of home smoking bans could also be the manifestation of secular trends. GEE analyses comparing the patterns of change in the four countries which implemented smoke-free legislation with a control country without smoke-free legislation at both time-points (UK) yielded some evidence that the increase in HSB prevalence could at least be partially attributable to the smoke-free legislation. Especially for continuing smokers the results indicated a significant (or borderline significant) increase in HSB among continuing smokers in Ireland, Germany, France, and the Netherlands, while there was no significant increase in HSB in the UK. Although the difference in patterns of change was significant only in the models comparing Germany to UK and France to UK, this is an important finding as it suggests the possibility of a causal link between the implementation of a national smoke-free legislation and imposition of individual home smoking restrictions among continuing smokers.
Furthermore, we found that positive attitudes towards smoking bans in bars were a significant prospective predictor of having adopted a HSB between pre- and post-legislation survey waves. This supports the social diffusion hypothesis and is suggestive of a causal relationship between smoking-related norms and attitudes and the adoption of a HSB. It is also known that the introduction of public smoking bans usually leads to an increase in support for such measures.[15, 23, 24] Given the positive association between policy support and HSB observed in the present study, the prevalence of HSB may be expected to increase further in the future.
We also found that male, younger, married smokers, smokers with a young (or with a newborn) child in the household and smokers with a high awareness of the dangerous potential of SHS were more likely to have or to adopt a HSB. The gender effect could be an effect of household composition, which we could not control for as this variable was not recorded in all country surveys. Borland et al. reported that in their analyses, household composition accounted for the gender effect as male smokers were more likely to live in a home with non-smokers.[5] Previous cross-sectional studies,[25-27] and a study analyzing ITC survey data from Australia, Canada, United Kingdom, and United States,[5] already showed that having a young child is one of the most important correlates of home smoking restrictions. In addition to this, our study found that also the birth of a child is a strong prospective predictor of adopting a HSB.
Some limitations need to be considered when interpreting our results. Due to different implementation dates of the national smoke-free legislation, the four country surveys were conducted in different years. The follow-up time and the time between implementation of the smoking ban and the post-legislation survey also varied between the countries, which probably affects the comparability of the relative increases in HSB prevalence. Such effects might explain why the comprehensiveness of the legislation seems to be unrelated to the extent of the policy effect in terms of an increase in HSB prevalence. In particular, that the relative increases in HSB prevalence is strongest in Germany could be partly due to the longer time between pre- and post-legislation measurements compared to the other countries, whereas the lower prevalence of home smoking restrictions in Ireland could partly be attributed to the surveys having been conducted about four years earlier than in the other countries. However, as additional single-country analyses of predictors of HSB yielded similar and consistent results (data not shown), it is unlikely that country differences in the study design would have distorted the findings from the multivariate analyses.
Between 21 and 34 percent of respondents were lost to attrition between pre- and post-legislation surveys. The non-responder analysis suggests only limited potential bias in the estimates of the multivariate analyses. The lower odds of being lost to follow-up among French respondents with pre-legislation home smoking restrictions might however lead to overestimated prevalence estimates for France.
UK (without Scotland) was chosen as a control country to give an estimate for the secular trend in HSB, and comparable baseline HSB prevalence implied that it was an appropriate choice for this purpose. In line with the diffusion hypothesis, it is nevertheless possible that the publicity around the plans for the enactment of the smoke-free legislation in UK has led to a steeper increase than would have been expected with the secular trend alone, which might have resulted in an overestimation of the secular trend. However, a similar effect could have led to a pre-legislation increase in the intervention countries already before the pre-legislation measurements, which might have resulted in an underestimation of the policy effect in these countries. It thus appears quite possible that such effects might have lead to our estimates being altogether conservative.
We relied solely on self-reported information in this study, and our findings may be subject to social desirability bias. A study using data from a large household survey furthermore found inconsistencies in reports about strict HSB especially in multi-person households with smokers.[28] Recording more detailed information about the household composition and its members and biochemical validation would be an asset for any future study.
Regardless of the limitations outlined above, this study is characterised by several strengths. The surveys were based on large national probability samples from four European countries using standardised survey questions and a prospective study design. They were conducted at pre- and post-smoke-free legislation time-points and thus exploited a historically unique situation. The prospective design, with replications across four countries, and with explicit analytic comparisons with a country in which smoke-free legislation had not yet been implemented, offers greater opportunities to examine alternatives to causality than cross-sectional studies. The greater internal validity accompanying the prospective design has been noted as a distinct advantage in evaluating the impact of tobacco control policies.[29] Our findings also were consistent with results from ITC studies conducted elsewhere,[5] which suggests a broad generalisability of the findings for Western industrial nations.
Future research should be aimed at elucidating the mechanisms of how public smoking bans influence household smoking rules. Our study and some previous evidence support the social diffusion hypothesis, but the precise interrelations between smoke-free legislation, smoking-related norms and imposing household smoking bans have yet to be clarified. Additional ITC survey waves will provide an important resource in this regard.
Opponents of workplace or public smoking bans have argued that these policies – albeit intended to protect non-smokers from tobacco smoke – could lead to displacement of smoking into the home and hence even increase the SHS exposure of non-smoking family members and, most importantly, children. On the contrary, our findings strongly support the premise that smoke-free legislation does not lead to more smoking in smokers’ homes. The data suggest rather that smoke-free legislation may stimulate smokers to establish total smoking bans in their homes. Policymakers in Europe and around the world thus do not need to fear an increase in SHS exposure among children as an unintended detrimental consequence of smoke-free legislation. In fact, converging evidence supports the notion that smoke-free legislation will lead to further benefits in reducing the harms of SHS beyond the limits of the legislation.
What this paper adds:
– The recent implementation of smoke-free legislation in several European countries provided the unique opportunity to examine the impact of public smoking bans on home smoking bans in a broader European setting.
– After implementation of national smoke-free legislation, the share of smokers with a total home smoking ban (HSB) increased significantly in all four countries examined. The pattern of change in HSB prevalence after implementation of smoke-free legislation among baseline smokers in Germany and among continuing smokers in Germany and France differed significantly from the pattern of change in UK which served as a control country without smoke-free legislation.
– This comprehensive study on the effects of smoke-free legislation on smoking in the home demonstrates that such legislation may stimulate smokers to establish total smoking bans in their homes.
Acknowledgements
Several members of the ITC Project team at the University of Waterloo have assisted in all stages of conducting the ITC Europe surveys, which we gratefully acknowledge. In particular, we thank Lorraine Craig, Project Manager of the ITC Europe surveys and the Data Management Core of the ITC Project, both at the University of Waterloo, Canada. We also thank Ann McNeill at the University of Nottingham for helpful comments, and for granting the permission to use ITC UK data in this study.
Funding
ITC Ireland: U.S. National Cancer Institute (R01 CA90955), Glaxo Smith Kline, Flight Attendants’ Medical Research Institute, Pfizer (Ireland) and Cancer Research UK. ITC France: French Institute for Health Promotion and Health Education (INPES), French National Cancer Institute (INCa), French Monitoring Centre for Drugs and Drug Addiction (OFDT). ITC Netherlands: The Netherlands Organisation for Health Research and Development (ZonMw). ITC Germany: German Ministry of Health, German Cancer Research Center, Dieter-Mennekes-Umweltstiftung. ITC UK: U.S. National Cancer Institute (RO1 CA100362 and P50 CA111236), Canadian Institutes of Health Research (57897), Cancer Research UK (C312/A6465). Survey development, management, and data management, ITC Project, University of Waterloo: U.S. National Cancer Institute (P50 CA111236; P01 CA138389); Canadian Institutes of Health Research (57897; 79551); Ontario Institute of Cancer Research. UM was financially supported by Klaus Tschira Foundation gGmbH. GTF was supported by a Senior Investigator Award from the Ontario Institute for Cancer Research and a Prevention Scientist Award from the Canadian Cancer Society Research Institute.
Footnotes
Contributions
UM planned the paper, carried out the statistical analyses, interpreted the data, and drafted the manuscript. She is the guarantor of the paper. LPB substantially contributed to the conception of the paper, to the interpretation of the data, and to drafting the paper. GEN, SA, and BvdP substantially contributed to the conception of the paper and to the interpretation of the data. RG, MW, GTF, HB, and MP-L advised on the design of the study and substantially contributed to the interpretation of the data. In addition, all co-authors revised drafts critically for important intellectual content, and all authors reviewed and approved of the final manuscript.
Competing interests
All authors declare having no conflicts of interest.
References
- 1.Cheraghi M, Salvi S. Environmental tobacco smoke (ETS) and respiratory health in children. Eur J Pediatr. 2009;168:897–905. doi: 10.1007/s00431-009-0967-3. [DOI] [PubMed] [Google Scholar]
- 2.Royal College of Physicians . Passive smoking and children: a report by the Tobacco Advisory Group of the Royal College of Physicians. Royal College of Physicians; London: 2010. [Google Scholar]
- 3.Akhtar PC, et al. Smoking restrictions in the home and secondhand smoke exposure among primary schoolchildren before and after introduction of the Scottish smoke-free legislation. Tob Control. 2009;18:409–15. doi: 10.1136/tc.2009.030627. [DOI] [PubMed] [Google Scholar]
- 4.Callinan JE, et al. Legislative smoking bans for reducing secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst Rev. 2010;4:CD005992. doi: 10.1002/14651858.CD005992.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Borland R, et al. Determinants and consequences of smoke-free homes: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(Suppl 3):iii42–50. doi: 10.1136/tc.2005.012492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adda J, Cornaglia F. The effect of bans and taxes on passive smoking. Am Econ J Appl Econ. 2010;2:1–32. [Google Scholar]
- 7.Ho SY, et al. Comprehensive smoke-free legislation and displacement of smoking into the homes of young children in Hong Kong. Tob Control. 2010;19:129–33. doi: 10.1136/tc.2009.032003. [DOI] [PubMed] [Google Scholar]
- 8.Akhtar PC, et al. Changes in child exposure to environmental tobacco smoke (CHETS) study after implementation of smoke-free legislation in Scotland: national cross sectional survey. Br Med J. 2007;335:545. doi: 10.1136/bmj.39311.550197.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fong GT, et al. Reductions in tobacco smoke pollution and increases in support for smoke-free public places following the implementation of comprehensive smoke-free workplace legislation in the Republic of Ireland: findings from the ITC Ireland/UK Survey. Tob Control. 2006;15(Suppl 3):iii51–8. doi: 10.1136/tc.2005.013649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haw SJ, Gruer L. Changes in exposure of adult non-smokers to secondhand smoke after implementation of smoke-free legislation in Scotland: national cross sectional survey. Br Med J. 2007;335(7619):549. doi: 10.1136/bmj.39315.670208.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holliday JC, Moore GF, Moore LA. Changes in child exposure to secondhand smoke after implementation of smoke-free legislation in Wales: a repeated cross-sectional study. BMC Public Health. 2009;9:430. doi: 10.1186/1471-2458-9-430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hyland A, et al. Does smoke-free Ireland have more smoking inside the home and less in pubs than the United Kingdom? Findings from the international tobacco control policy evaluation project. Eur J Public Health. 2008;18:63–5. doi: 10.1093/eurpub/ckm054. [DOI] [PubMed] [Google Scholar]
- 13.Hyland A, et al. The impact of smokefree legislation in Scotland: results from the Scottish ITC: Scotland/UK longitudinal surveys. Eur J Public Health. 2009;19:198–205. doi: 10.1093/eurpub/ckn141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jarvis MJ, et al. Impact of smoke-free legislation on children's exposure to secondhand smoke: cotinine data from the Health Survey for England. Tob Control. 2011 doi: 10.1136/tc.2010.041608. [DOI] [PubMed] [Google Scholar]
- 15.Edwards R, et al. After the smoke has cleared: evaluation of the impact of a new national smoke-free law in New Zealand. Tob Control. 2008;17:e2. doi: 10.1136/tc.2007.020347. [DOI] [PubMed] [Google Scholar]
- 16.Edwards R, et al. Beneficial impacts of a national smokefree environments law on an indigenous population: a multifaceted evaluation. Int J Equity Health. 2009;8:12. doi: 10.1186/1475-9276-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fong GT, et al. The conceptual framework of the International Tobacco Control (ITC) Policy Evaluation Project. Tob Control. 2006;15(Suppl 3):iii3–11. doi: 10.1136/tc.2005.015438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thompson ME, et al. Methods of the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(Suppl 3):iii12–8. doi: 10.1136/tc.2005.013870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nagelhout GE, et al. Is web interviewing a good alternative to telephone interviewing? Findings from the international tobacco control (ITC) Netherlands survey. BMC Public Health. 2010;10:351. doi: 10.1186/1471-2458-10-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heatherton TF, et al. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict. 1989;84:791–9. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- 21.Hanley JA, et al. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157:364–75. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- 22.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30. [PubMed] [Google Scholar]
- 23.Rayens MK, et al. Public opinion and smoke-free laws. Policy Polit Nurs Pract. 2007;8:262–70. doi: 10.1177/1527154407312736. [DOI] [PubMed] [Google Scholar]
- 24.Tang H, et al. Changes of attitudes and patronage behaviors in response to a smoke-free bar law. Am J Public Health. 2003;93:611–7. doi: 10.2105/ajph.93.4.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Borland R, et al. Trends in environmental tobacco smoke restrictions in the home in Victoria, Australia. Tob Control. 1999;8:266–71. doi: 10.1136/tc.8.3.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ouedraogo E, et al. Factors associated with the adoption of a smoking ban in Quebec households. Chronic Dis Can. 2009;29:128–35. [PubMed] [Google Scholar]
- 27.Pizacani BA, et al. Household smoking bans: which households have them and do they work? Prev Med. 2003;36:99–107. doi: 10.1006/pmed.2002.1123. [DOI] [PubMed] [Google Scholar]
- 28.Mumford EA, Levy DT, Romano EO. Home smoking restrictions. Problems in classification. Am J Prev Med. 2004;27:126–31. doi: 10.1016/j.amepre.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 29.International Agency for Research on Cancer . IARC Handbooks of cancer prevention, Vol. 12: Methods for evaluating tobacco control policies. World Health Organization, International Agency for Research on Cancer; Lyon: 2009. [Google Scholar]