Abstract
Background
Census predictions for Florida suggest a threefold increase in the population 65 or older within 20 years. We predict resource utilization for this age group.
Methods
Using the Florida Agency for Healthcare Administration admission dataset we evaluated the effect of age on length of stay, hospital charges and discharge disposition while adjusting for clinical and demographic factors. Using U.S. Census Bureau data and burn incidence rates from this dataset we estimated future resource utilization.
Results
Elderly patients were discharged to home less often and were discharged to short term general hospitals, intermediate care facilities and skilled nursing facilities more often than the other age groups (p < 0.05). They also required home health care and IV medications significantly more often (p <0.05). Their length of stay was longer and total hospital charges were greater (p < 0.05) after adjusting for gender, race, Charleson comorbidity index, payer, TBSA burned and burn center treatment.
Conclusions
Our data show an age dependent increase in the utilization of post-hospitalization resources, LOS and total charges for elderly burn patients.
Introduction
Following World War II and extending into the 1960's, the United States observed a dramatic increase in its birth rates, often referred to as the “Baby Boom.” This generation of Americans was the product of birth rates well over 3.5 million live births per year for a period of close to 20 years. This population wave is now approaching the 65 and over age group.1 Burn injuries are among the top twenty causes of non-fatal injuries in the geriatric population.2 The care of burn patients is a resource intensive team approach at burn centers across the United States. Combining the population age shift with frequent burn injury and resource intensive treatment suggests an increasing demand on these medical resources.
Medical resource usage is often measured by patient length of stay and total hospital charges. These measurements along with mortality figures account for the most common outcome measures in current research.3,4,5,6,7,8,9,10 In 1980, Curreri et al published an analysis of survival and hospitalization time which identified increasing mortality and length of stay with age. They also used this data to predict burn bed needs for a known or predicted population of regional burn victims.3 By 1990, Saffle published on improvements in the survival of elderly burn patients. And in 2006, Pomahac evaluated patients 80 years of age or older and found improved survival in this group of burn victims.10 Even with these improvements, elderly burn patients are reported to have higher mortality and worse outcomes despite advances in burn care.11, 12, 13, 14 While the most expensive setting in medical care is the acute hospitalization, there are additional factors which add to the costs of treating burn patients. A patient's discharge disposition highlights this. Patients may be sent home, to skilled nursing facilities or rehabilitation centers.
Pham described this as discharge to non-independent status.11 Other patients may require home health care and outpatient occupational and physical therapy. Data on the discharge disposition of patients is collected in the Agency for Health Care Administration admission dataset in the State of Florida. The goal of this study was to determine the potential required resource utilization of the elderly population in light of the ageing “Baby Boom” generation in the State of Florida.
Materials and Methods
Study Design
This is a retrospective cohort study using data from the Agency for Health Care Administration (AHCA) in Florida. With this data, we evaluated inpatient hospital admissions for patients with a diagnosis of burn injury. The Florida Agency for Health Care Administration database was analyzed from 1997 through the third quarter of 2010 for outcomes after burn injury. The primary outcomes were hospital charges and length of stay, while the secondary outcome was discharge disposition
Database and Study Population
We identified 34,908 patients who were admitted with a diagnosis of burn injury using the ICD-9 diagnosis codes of 940 through 949 excluding 947 (internal burns secondary to ingestion of a caustic substance.) We further excluded those patients who expired. Subsequently we refined this group into those patients who had a 948 code for total body surface area burned. The Charlson co-morbidity Index was calculated for this dataset to adjust for co-morbid conditions in these patients. This study was performed with institutional IRB approval.
The Charlson co-morbidity index was introduced in 1987 by M.E. Charlson and colleagues. It is a weighted index which takes into account the number and seriousness of co-morbid diseases.15 This method of classifying co-morbidity has been validated in several patient populations including intensive care unit (ICU) admissions and several surgical procedures. It has been adapted for use with ICD-9 databases. 16It is one of the most extensively studied co-morbidity indices, and has predictive validity with several outcome measures such as mortality, disability, readmissions, and length of stay. 17This allows our age groups to be compared while adjusting for the effect of co-morbid conditions on the outcome.
Statistical Analysis
Differences between cohorts in length of stay and total hospital charges were evaluated by regression analysis. Multivariate regression was used to adjust and match for non modifiable factors that had the potential of confounding or biasing the outcome of interest. Confounders were considered in the multivariate analysis if it was reasonable to assume (Gestalt) or if there was published data to show that these variables had an independent effect on the exposure (risk factor) and outcome of interest. Prior to regression analysis, multicollinearity was measured between the adjusted or confounding variables. Multicollinearity was evaluated prior to regression analysis by examining the correlation coefficient among confounders. If the correlation coefficient was greater than 0.8, only one of the confounders was used in the multivariate analysis.18 None of the confounders in this study exhibited collinearity with each other. In the final multivariate regression, gender, race, payer, Charlson co-morbidity index, total body surface area burned, and burn center admission were treated as confounders. Analysis of variance was used to evaluate significant differences in demographics, burn center admission, payer and discharge status between age groups. We used census predictions for the population of Florida and burn incidence rates from the AHCA hospital admission dataset to calculate future resource needs of our State. This incidence rate was calculated by number of persons admitted to Florida burn centers per 1,000 person years. SAS version [9.2] of the SAS System for [Windows] Copyright @ 2002-2008 by SAS Institute Inc., Cary, NC, USA was used during our statistical evaluation of the dataset.
Results
There were 34,908 records over 14 years with a diagnosis of burn injury on admission to a hospital in the State of Florida. Of those patients, 17,827 had an ICD-9 948 code describing burn size recorded and had survived through discharge from the hospital. We evaluated the age groups 0-17(pediatric), 18-64(adult), and > or = 65(elderly) years of age. There were 4,982 patients in group 0-17, 11,051 in group 18-64 and 1,794 in group > or = 65 years of age. The patients' gender and race are listed in table I. Analysis of variance (ANOVA) was used to evaluate for differences in gender and race. Burn sizes for each age group are reported in figure 1 they were separated by admission to burn centers and other hospitals. The mean burn size of elderly patients was lower than that for the adult and pediatric age groups, while the mean burn size admitted to burn units was larger than that admitted to other hospitals in all age groups. Burn center admission, payer category, length of stay and total charges are reported in table II. Our elderly cohort (> or = 65 years) was less likely to be treated at a burn center compared to the adult and pediatric cohorts (p<0.05). Approximately 43% of the elderly patients were treated in a burn center, while at least 71% of the adult and pediatric age groups were treated at burn centers. When reviewing the insurance coverage of this cohort of patients, we noted that approximately 83 percent of the elderly age group was covered by Medicare services. The adult age group had a wider spread of payer sources with 18.4 percent being covered by workers compensation and 17% self pay or uninsured.
Table I.
Demographic data of the 17,827 patients with 948 codes recorded who survived through discharge.
| Child (0∼17 years) N=4,982 | Adult (18∼64years) N=11,051 | Old (65+ years) N=1,794 | P-value | |
|---|---|---|---|---|
| Gender | ||||
| Male | 3,177 (63.8%) | 8,190 (74.1%) | 971 (54.1%) | < 0.0001 |
| Female | 1,805 (36.2%) | 2,860 (25.9%) | 823 (45.9%) | < 0.0001 |
| Unknown | 0 | 1 (0.01%) | 0 | |
| Race | ||||
| American Indian | 4 (0.08%) | 23 (0.2%) | 2 (0.1%) | 0.15 |
| Asian | 22 (0.4%) | 64 (0.6%) | 13 (0.7%) | 0.33 |
| Black | 1,534 (30.8%) | 2,155 (19.5%) | 277 (15.4%) | < 0.0001 |
| White | 2,281 (45.8%) | 6,061 (54.9%) | 1,149 (64.1%) | < 0.0001 |
| White Hispanic | 869 (17.4%) | 2,316 (21.0%) | 294 (16.4%) | < 0.0001 |
| Black Hispanic | 29 (0.6%) | 99 (0.9%) | 12 (0.7%) | 0.10 |
| Other | 205 (4.1%) | 261 (2.4%) | 35 (2.0%) | < 0.0001 |
| No Response | 38 (0.8%) | 72 (0.7%) | 12 (0.7%) | 0.73 |
Figure 1.
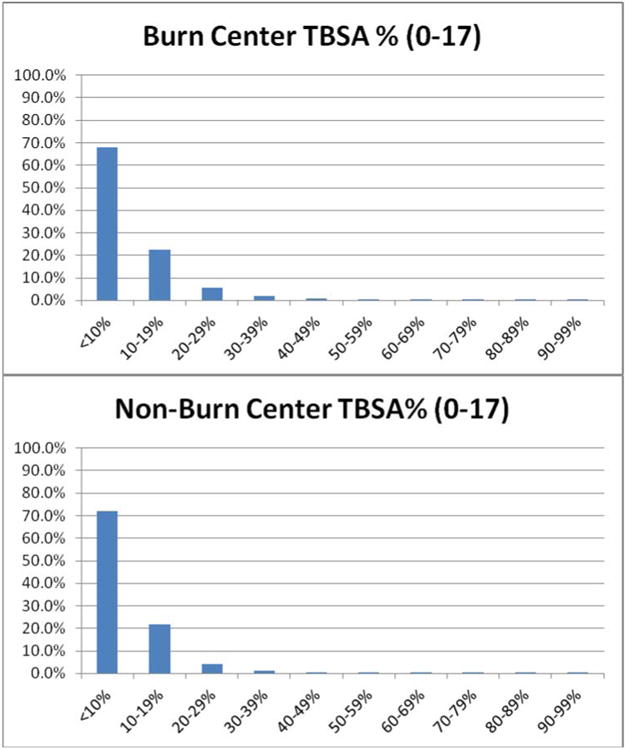
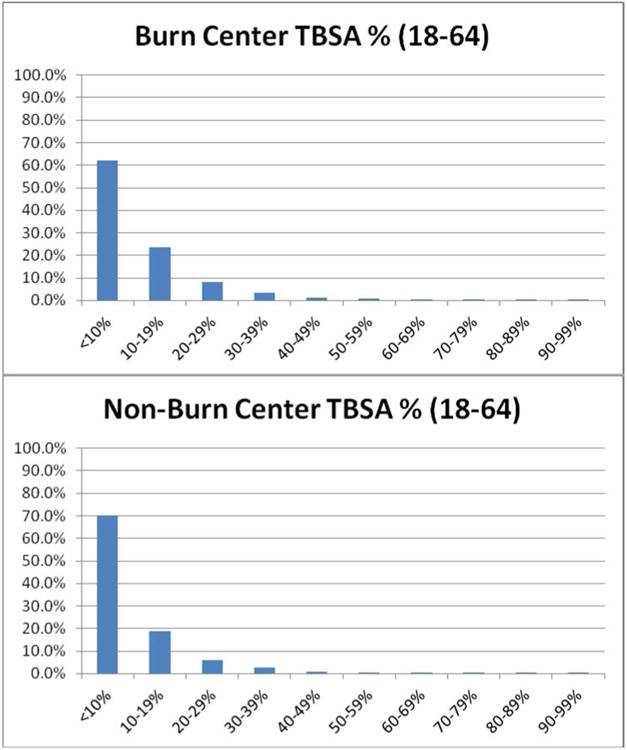
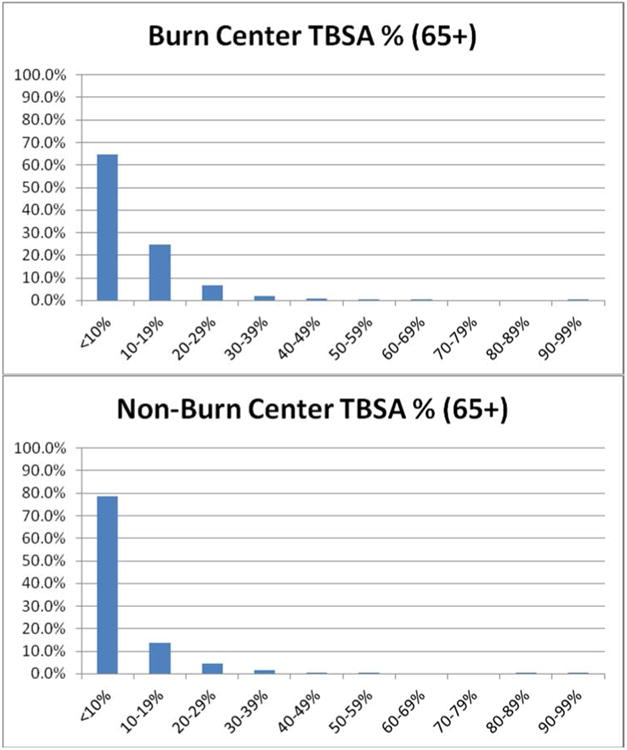
Frequency of burn sizes (TBSA) seen at burn centers and non-burn centers divided by age group.
Table II.
Burn center admission, insurance status, length of stay and total charges compared using ANOVA. The p-value less than 0.0001 suggests a significant difference between at least two of the age groups.
| Child (0∼17 years) N=4,982 | Adult (18∼64years) N=11,051 | Old (65+ years) N=1,794 | P-values | |
|---|---|---|---|---|
| Burn Center | ||||
| Yes | 3,576 (71.8%) | 7,851 (71.0%) | 781 (43.5%) | < 0.0001 |
| No | 1,406 (28.2%) | 3,200 (29.0%) | 1,013 (56.5%) | < 0.0001 |
| Payer Category | Child (0∼17 years) N=4,982 | Adult (18∼64years) N=11,051 | Old (65+ years) N=1,794 | P-values |
| Medicare | 9 (0.2%) | 824 (7.5%) | 1,508 (84.1%) | <0.0001 |
| Medicaid | 2,824 (56.7%) | 1,449 (13.1%) | 43 (2.4%) | <0.0001 |
| Commercial | 1,522 (30.6%) | 3,110 (28.1%) | 146 (8.1%) | <0.0001 |
| Worker's Compensation | 25 (0.5%) | 1,812 (16.4%) | 41 (2.3%) | <0.0001 |
| Government | 103 (2.1%) | 713 (6.5%) | 146 (8.1%) | <0.0001 |
| Self Pay | 499 (10.0%) | 3,143 (28.4%) | 36 (2.0%) | <0.0001 |
| Length of Stay | 6.3 | 9.4 | 9.3 | <0.0001 |
| Total Charges | $ 23,200 | $ 54,071 | $ 49,826 | <0.0001 |
The median length of stay (LOS) and charges for each age group are recorded in table II. In addition we compared LOS and total hospital charges between groups using linear regression and adjusting for gender, race, Charlson co-morbidity index, payer, TBSA burned and burn center treatment. The crude linear regression of LOS and age group was not significant. When adjusting for the parameters described above we found the elderly patients to have a longer LOS (p < 0.05). We performed a similar comparison for total hospital charges and found that the crude regression was not statistically significant while the adjusted regression showed that the elderly patients had higher charges than the other age groups (p < 0.05). For disposition, elderly patients were more likely to be discharged to short term general hospitals, intermediate care facilities, and skilled nursing facilities compared to the adult and pediatric age groups (p < 0.05) as shown in table III. We also noted a larger percentage of the elderly population was discharged to inpatient rehabilitation facilities (p < 0.05). Elderly patients were also more likely to be sent home with home health care nursing and IV medications (p < 0.05). In addition to that we noted that the elderly patients were more likely to be discharged into hospice care, or a hospice medical facility (p < 0.05).
Table III.
Discharge status of each age group compared using ANOVA.
| Discharge Status | Child | Adult (Reference) | Old |
|---|---|---|---|
| Home | 87.2% ** | 67.6% | 36.1% ** |
| Short Term General Hospital | 2.4% | 2.0% | 3.4% ** |
| Skilled Nursing Facility | 0.3% | 2.1% | 21.2% ** |
| Intermediate Care Facility | 0.4% | 0.5% | 1.7% ** |
| Other Institution | 2.1% | 3.1% | 4.9% |
| Home Health Care | 8.1% ** | 22.1% | 28.4% ** |
| Left Against Medical Advice | 0.3% ** | 1.2% | 1.2% |
| Discharged on IV Medications | 0.2% | 0.3% | 0.9% ** |
| Hospice- Home | 0.3% | 0.3% | 1.7% ** |
| Hospice- Medical Facility | 0% | 0.2% | 1.2% * |
| Inpatient Rehabilitation Facility | 0.8% * | 2.4% | 5.0% ** |
| Medicare Long Term Care Facility | 0% | 0.6% | 2.0% |
| Psychiatric Hospital | 0% | 0.8% | 0% |
Significantly different at p=0.05;
Significantly different at p=0.01;
To extrapolate admission volume of age specific burn injury for the future, we combined data from the State of Florida AHCA and the U.S. Census Bureau. We calculated the incident rate of burn injury in the state of Florida, using population data from the year 2000 as reference. Data from the U.S. Census Bureau provided the projected population growth. This information is shown in figure 2. By 2030, the total hospital admissions for burn patients 65 or older will surpass that of the patients in the 45 to 64 year old age group. With the discharge disposition percentages from our 14 year cohort, we could expect to have on the order of 300 referrals for home health care services, 222 transfers to skilled nursing facilities, 43 transfers to short term general hospitals and 22 referrals to intermediate care facilities in 2030 from the 65 or older age group. This compares to 100, 74, 14 and 7 in the year 2000. This represents close to three times as many patients requiring services in each of these areas per year.
Figure 2.
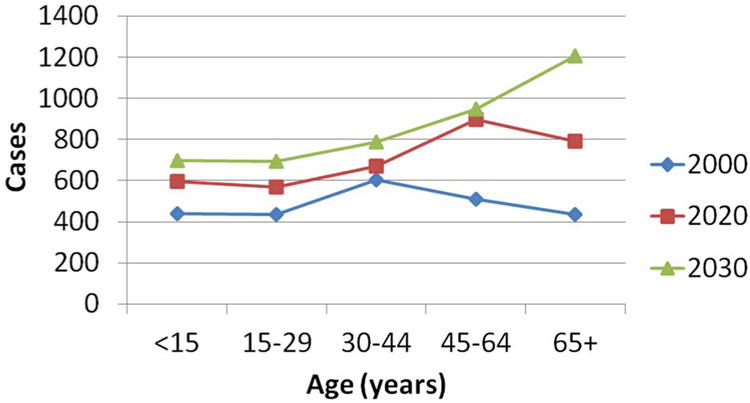
Graph showing the trend of increasing population in the State and the relative increase in the population of patients 65+. (Projected number of burn cases evaluated in Florida Trauma Centers by age based on calculated 2000 incidence rate.)
Discussion
A wave of elderly patients created by the baby boom is now approaching the 65+ age group. This group of patients will likely suffer burn injuries at rates similar to the recent past. With population predictions provided by the Census Bureau, we are able to create a forecast of burn injuries, their dispositions and their resource utilization. Using information gained from the AHCA dataset we have identified a pattern which points to greater discharge needs for the elderly patient in comparison to the younger cohorts. Combining these sources, we noted a dramatic three fold increased need for home health care services, skilled nursing facilities, and short term general hospitals for elderly burn patients on discharge after injury. Based on these findings burn centers and other facilities in the state will need to plan for the increased volume of elderly patients in need of additional care at these facilities over the next ten to twenty years.
Saffle noted that the chances of survival after burn injury have steadily improved over the past 50 years.12, 13 Wibbenmeyer et. al. and others have reported that there have been limited improvements in survival for the elderly population despite the overall survival improvements.14, 15, 20, 21, 22 This highlights geriatric burn injury as a specific area for improvement. Given the rapid approach of this increased demographic; there is an urgent need to address the resource requirements of this age group.
Many papers highlight LOS, charges and mortality rates in elderly patients as measures of outcome. Elderly patients stayed longer, cost more and had higher mortality rates than their younger counterparts. Our research shows these differences in LOS and charges, while describing statistically significant differences in the discharge disposition of elderly patients. Discharge to home health care services, skilled nursing facilities, and short term general hospitals represent continued losses in function and physical freedom and increased costs to society that may actually represent a potentially more important outcome measure than initial LOS, charges or mortality in terms of total impact on the individual patient and society. In addition to the differences in discharge disposition between age groups there are differences in the raw percent results in discharge disposition in the elderly population admitted to burn centers versus non-burn centers. These differences will be further evaluated using regression analysis techniques and may highlight the benefits of treatment at a burn center for elderly patients with burn injuries. With a set of well-accepted outcome measures for comparison, we can enhance our ability to be prepared for the treatment of our growing elderly population.
It is well accepted and documented that mortality rates for burn injury are higher in elderly patients. We would like to highlight the following; mortality from burn injury is highly dependent on TBSA involved, but the vast majority of burn injuries in this study (> 90%) were less than 20% TBSA across all age groups. In addition we limited this study to those patients that survived their burn injuries. Our findings highlight the morbidity associated with burn injury and its disproportionate effect on elderly burn patients and their discharge disposition. We think that increases in the elderly population combined with the small average size of burn injury will outweigh the effect of the mortality figures noted for the elderly in the current literature. However we did not directly evaluate the resource utilization of those patients that died from their injuries. Given the higher mortality rate from burn injuries in the elderly population this may represent an increased cost per TBSA percent burned. This highlights a limitation in the scope of this study.
Triage of burn patients to burn centers depends upon multiple factors including TBSA burned, burn depth, patient age, co-morbidities and other clinical factors. During our analysis we noted that elderly burn patients were seen or treated at burn centers 43% of the time while pediatric and adult patients were seen at burn centers 73% and 71% of the time respectively. This disparity was striking, and deserves in-depth evaluation. Differences in triage and transfer patterns for patients with burn injuries are most certainly multifactorial. We intend to evaluate our data to identify factors associated with this difference including burn size and severity, insurance status, referral source, admission status, race and gender. Demographic and financial factors may well account for this disparity, while patient requests and geographic location may add another layer to the analysis. Other factors such as physician referral patterns and emergency medical services transportation contracts have all been forwarded as influences in the age disparity of burn patient treatment. With the available data points in this administrative dataset we plan to systematically evaluate whether patients who met the ABA triage transfer criteria for burn center care were appropriately transferred regardless of age.
In this study as with any study utilizing administrative data, the results are highly dependent upon the quality of data collected. We found that there were differences in the proportion of patients recorded with a TBSA ICD-9 code (948.**) in the non-burn and burn centers. This may represent familiarity with the coding and billing aspect of burn care that is limited in non-burn centers. There are also concerns that some coding does not accurately represent the severity of injury in patients seen at non-burn centers. These limitations are concerning, but will improve with continued utilization of the data sets and quality monitoring of the process for collecting the data.
In conclusion, a large number of baby boomers are reaching the age of 65. We have identified increased resource utilization in their post-hospital care from burn injury. Others have suggested that survival from burn injury is improving. Even though the elderly population has not seen the same survival benefits of our improved burn care, burn centers and other hospitals that treat the burned patient will need to prepare for increasing post-hospital resource utilization from the growing elderly population.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Bibliography
- 1.Population Pyramids of Florida. US Census Bureau, Population Division, Interim State Population Projections, 2005 Internet Release Date. 2005 Apr 21; [Google Scholar]
- 2.National Center For Injury Prevention and Control. CDC, NEISS All Injury Program, Consumer Product Safety Commission. 20 leading Causes of Non-fatal Injury, US. 2008 [Google Scholar]
- 3.Curreri PW, Luterman A, Braun D, Shires GT. Burn Injury Analysis of Survival and Hospitalization Time for 937 Patients. Ann Surg. 1980;192(4):472–477. doi: 10.1097/00000658-198010000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anous MM, Heimbach DM. Causes of Death and Predictors in Burned Patients More than 60 Years of Age. The Journal of Trauma. 1986;26(2):135–139. doi: 10.1097/00005373-198602000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Renz BM, Sherman R. The Burn Unit Experience at Grady Memorial Hospital: 844 Cases. J Burn Care Rehabil. 1992;13:426–436. doi: 10.1097/00004630-199207000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Sarahadi S, Kincaid R, McGregor JC, Watson JD. Burns in the Elderly in the South East of Scotland: Review of 176 Patients Treated in the Bangour Burns Unit (1982-91) and Burn Inpatients in the Region 1975-91) J Burns. 1995;21(2):91–95. doi: 10.1016/0305-4179(95)92130-5. [DOI] [PubMed] [Google Scholar]
- 7.O'Keefe GE, Hunt JL, Purdue GF. An Evaluation of Risk Factors for Mortality after Burn Trauma and the Identification of Gender-Dependent Differences in Outcomes. J Am Coll Surg. 2001;192(2):153–160. doi: 10.1016/s1072-7515(00)00785-7. [DOI] [PubMed] [Google Scholar]
- 8.Ho WS, Ying SY, Burd A. Outcome analysis of 286 severely burned patients: retrospective study. Hong Kong Med J. 2002;8(4):235–239. [PubMed] [Google Scholar]
- 9.Rao K, Moiemen NS. Aetiology and Outcome of Burns in the Elderly. J Burns. 2006;32:802–805. doi: 10.1016/j.burns.2006.03.024. [DOI] [PubMed] [Google Scholar]
- 10.Pomahac B, Matros E, Semel M, et al. Predictors of Survival and Length of Stay in Burn Patients Older Than 80 Years of Age: Does Age Really Matter? Journal of Burn Care & Research. 2006;27(3):265–269. doi: 10.1097/01.BCR.0000216795.90646.4E. [DOI] [PubMed] [Google Scholar]
- 11.Pham TN, Kraner CB, Want J, et al. Epidemiology and Outcomes of Older Adults with Burn Injury: An Analysis of the National Burn Repository. Journal of Burn Care & Research. 2009;30(1):30–36. doi: 10.1097/BCR.0b013e3181921efc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saffle JR. Predicting outcomes of burns. N Engl J Med. 1998 Feb 5;338(6):387–8. doi: 10.1056/NEJM199802053380610. [DOI] [PubMed] [Google Scholar]
- 13.Saffle JR, Larson CM, Sullivan J, Shelby J. The Continuing Challenge of Burn Care in the Elderly. Surgery. 1990;108(3):534–543. [PubMed] [Google Scholar]
- 14.Wibbenmeyer LA, Amelon MJ, Morgan LJ, et al. Predicting Survival in an Elderly Burn Patient Population. Burns. 2001;27:583–590. doi: 10.1016/s0305-4179(01)00009-2. [DOI] [PubMed] [Google Scholar]
- 15.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation. J Chron Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 16.Deyo RA, Cherkin DC, Ciol MA. Adapting a Clinical Comorbidity Index for Use with ICD-9-CM Administrative Databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 17.Groot V, Beckerman H, Lankhorst GJ, Bouter LM. How to Measure Comorbidity: a Critical Review of Available Methods. J Clin Epidemiol. 2003;56:221–229. doi: 10.1016/s0895-4356(02)00585-1. [DOI] [PubMed] [Google Scholar]
- 18.Detecting Multicollinearity in Logistic Regression Models: An Extenison of BKW Diagnostic. Joint Statistical Meetings. 2002:1356–1358. [Google Scholar]
- 19.DeMeestre T, Feller I. Mortality in Burned Patients Sixty-One Years of Age and Older. Surgery, Gynecology & Obstetrics. 1968;126:1041–1044. [PubMed] [Google Scholar]
- 20.Merrell SW, Saffle JR, Sullivan JJ, et al. Increased Survival after Major Thermal Injury. The American Journal of Surgery. 1987;154:623–627. doi: 10.1016/0002-9610(87)90229-7. [DOI] [PubMed] [Google Scholar]
- 21.McGwin G, Cross JM, Ford JW, Rue LW. Long-Term Trends in Mortality According to Age among Adult Burn Patients. Journal of Burn Care & Rehabilitation. 2003;24(1):21–25. doi: 10.1097/00004630-200301000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Latenser BA, Miller SF, Palmer B, et al. National Burn Repository 2006: A Ten-Year Review. J Burn Care Res. 2007 Sep-Oct;28(5):635–58. doi: 10.1097/BCR.0B013E31814B25B1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


