Abstract
Objectives. We determined whether participation in Healthy Babies Healthy Start (HBHS), a maternal health program emphasizing racial equity and delivering services through case management home visitation, was associated with improved birth outcomes for Black women relative to White women.
Methods. We used a matched-comparison posttest-only design in which we selected the comparison group using propensity score matching. Study data were generated through secondary analysis of Michigan state- and Kalamazoo County–level birth certificate records for 2008 to 2010. We completed statistical analyses, stratified by race, using a repeated-measures generalized linear model.
Results. Despite their smoking rate being double that of their matched counterparts, Black HBHS participants delivered higher birth-weight infants than did Black nonparticipants (P = .05). White HBHS participants had significantly more prenatal care than did White nonparticipants, but they had similar birth outcomes (P = .7 for birth weight; P = .55 for gestation).
Conclusions. HBHS participation is associated with increased birth weights among Black women but not among White women, suggesting differential program gains for Black women.
Over the past several decades, as overall infant mortality has declined in the United States, the gap between Blacks and Whites has remained significant, with Black infants dying at 2.2 times the rate of White infants (11.6 and 5.2 infant deaths/1000 live births, respectively).1–3 In addition to congenital malformations, the leading proximal causes of infant mortality are preterm delivery, low birth weight, and sudden unexplained infant death.4 Less is known about the distal steps in this pathway (e.g., what causes preterm delivery, low birth weight, and sudden unexplained infant death), but the weight of evidence has pointed to nonclinical determinants: sociopolitical inequities that lead to chronic stress and poorer health among Blacks,5–7 coupled with discrimination in delivery of health care services and underutilization of health care resources by Blacks.8–11 Moreover, perceived racism has been implicated in maladaptive coping behaviors that add to perinatal risk, including smoking, unhealthy eating, and lack of exercise.12–15 Finally, poverty, which brings its own social inequities, is more prevalent among Blacks.16,17 In sum, substantial evidence exists that stress affects health and birth outcomes through multiple biopsychosocial pathways and that the stress associated with racism contributes to the Black–White disparity in birth outcomes.
Growing evidence of the scope and nature of racial disparities led the Institute of Medicine to call for comprehensive, multipronged approaches targeting patients, providers, and health care systems to increase access and quality of care and to improve the cultural competency of health systems at the community level.18 Healthy Start, initiated in 1991, is one of the first national programs to adopt racial disparity reduction as one of its primary goals.19,20 The Healthy Start intervention strategies are multilevel: providing home visitation services to high-risk women, educating providers and the wider community on perinatal health–related issues, and identifying institutional barriers and promoting cross-systems collaboration to improve the existing health infrastructure.19 Recognizing that health disparities vary widely from community to community,10 Healthy Start promotes grassroots, community-based program development.19 The Kalamazoo, Michigan, Healthy Babies Healthy Start (HBHS) program has developed a case management approach to home visitation. With the goal of facilitating communication and strengthening ties between community residents and health care institutions, HBHS hires community residents as case managers and places them in perinatal clinic settings. The Kalamazoo HBHS case managers are paraprofessionals trained in a social work framework for service provision. Case management is supported by HBHS health educators who use multiple strategies, including conducting classes for case-managed participants and community members and coordinating the HBHS consortium to foster problem-solving dialogue among case-managed participants, community members, agency representatives, and health care providers.
Using a grassroots approach means that HBHS case managers attempt to meet women where they are in terms of their health-related knowledge, behaviors, and needs and escort them through the remainder of the pregnancy while providing support, information, and improved access to various clinical and community resources.19 On the basis of current reasoning regarding racial disparities18 and the potential benefits of case management, if poor Black women are more disenfranchised than poor White women within the existing health care structure, this approach should offer differential benefit to Black women. The purpose of this study was to determine whether HBHS participation was differentially associated with improved birth outcomes for Black women compared with White women, as indicated by gestational age and birth weight. We expected that study findings would provide important information on the potential value of community-based, multipronged approaches that inform efforts to improve birth outcomes for Black women and infants.
METHODS
The study was quasi-experimental, with a matched-comparison posttest-only design. The intervention was participation in the HBHS program during pregnancy, and we selected the comparison group using propensity score matching. Study data were generated through secondary analysis of state- and county-level birth certificate administrative records, spanning the years 2008 to 2010.
Study Population and Sample
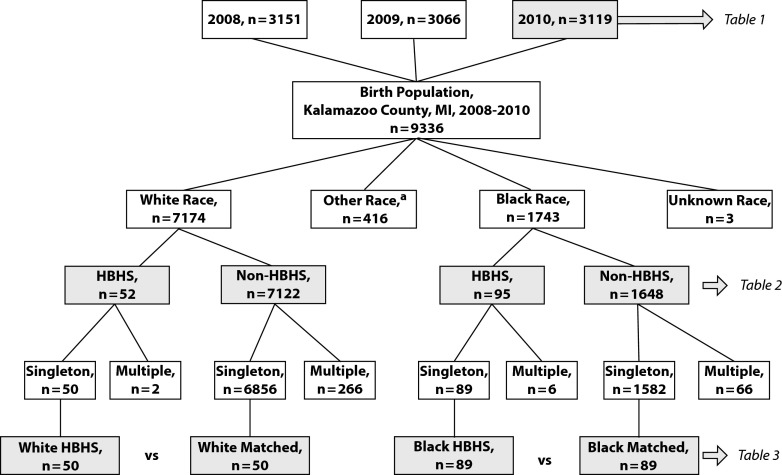
As shown in Figure 1, the study sampling frame was the population of 9336 women who were residents of Kalamazoo County when they gave birth during the years 2008 to 2010. We further stratified the study sample into 2 racial categories, Black and White. We based racial categorization on the bridged race variable found in the birth records,21 which originated from women’s self-report of race on their infant’s birth certificate. Within the birth records data set, Hispanic ethnicity is an independent variable that crosses all racial categories. The HBHS intervention group consisted of women enrolled in HBHS case management during pregnancy and at the time of delivery. One hundred forty-seven women met these criteria: 95 Black and 52 White. As illustrated in Figure 1, eligibility criteria for the final comparison sample groups was a single-gestation delivery.
FIGURE 1—
Flowchart of study population and stratified samples: Kalamazoo County, MI; 2008–2010.
Note. HBHS = Healthy Babies Healthy Start.
aOther race was defined as American Indian, Asian, Pacific Islander, or Other.
Propensity score matching can be an effective technique for minimizing self-selection treatment bias in observational studies such as ours.22 We completed the following set of matching procedures separately for each of the 2 racial categories.
To begin with, we compared HBHS enrollees with nonenrollees on demographic and prepregnancy characteristics, including Hispanic ethnicity, whether adolescent or not, marital status, insurance status, educational level, obstetric history, chronic disease status, body mass index (BMI; defined as weight in kilograms divided by the square of height in meters), and whether prenatal care was initiated in the first trimester. We then entered characteristics that were statistically different at the P ≤ .05 level into a logistic regression model. The regression produced a propensity score variable whose values represented each individual’s probability of participating in HBHS on the basis of the model predictors. The 2 models generating propensity scores for Black and White women were the same, except that the model for White women included Hispanic ethnicity; thus, women in the White comparison group had the same prevalence of Hispanic ethnicity as women in the White HBHS group. Because of the large sample sizes of non-HBHS participants (n = 7122 White nonparticipants and n = 1648 Black nonparticipants), we found an exact match for each of the 147 HBHS participants (i.e., they had the same propensity score). When multiple matches were available, we selected the non-HBHS comparison match randomly.
Setting
Kalamazoo County, the setting for this study, has a history of high Black infant mortality rate (18.7/1000 live births among Black women from 2006–2010) and high racial disparity (Black to White infant mortality rate ratio of 3.5 from 2006–2010).23 The racial disparity in infant mortality in this community is substantially higher than that in the state of Michigan (2.7) and the nation (2.2).24 The high Black infant mortality rates and high Black–White disparity were the impetus for initiating the Healthy Start program in 1997.
Kalamazoo Healthy Babies Healthy Start
Kalamazoo HBHS case management services are offered to any pregnant woman residing within a targeted 3 zip-code area who is in her first or second trimester. Participants typically have household incomes below the federal poverty level, as defined by the US Department of Health and Human Services within each program year.25 Because most participants are recruited in obstetric clinics, the vast majority of them (90.0%) are enrolled after their first prenatal care appointment. Enrolled participants have monthly face-to-face contact with case managers, undergo comprehensive biopsychosocial assessments, are referred to community resources as needed, receive education and counseling on maternal and infant health issues, and receive ongoing support in accessing prenatal care. Case managers develop care plans tailored to the individual, in concert with the participant and her provider. As part of the health care team, HBHS case managers participate in weekly case review meetings, work with providers to achieve health care goals, and have access to medical records for tracking progress.
Measures
With the exception of HBHS participation, all measures were contained within the birth records administrative data set. The 2 outcome measures in this study were gestational age and birth weight, the leading predictors of infant mortality in Kalamazoo County. Gestational age was a continuous, interval-level variable, with number of weeks as the unit of analysis. Birth weight was also a continuous, interval-level variable, with grams as the unit of analysis. Because multiple operationalizations of birth outcomes have been shown to reflect different dimensions of perinatal health,26,27 birth outcomes were measured by indicator (gestational age and birth weight) and by scale (continuous and dichotomous): premature (< 37 weeks gestation) or not and low birth weight (< 2500 g) or not. The primary study predictor was a dichotomous variable representing HBHS program participation. HBHS participants were identified within the birth records data set by matching their name, date of birth, and date of delivery (obtained from HBHS administrative records) to the birth certificate database.
Covariates included demographics (adolescent or not, Hispanic ethnicity, marital status, insurance status, level of education), obstetric history (paragravida, prior poor birth outcomes), prepregnancy health conditions (hypertension, diabetes, BMI), prenatal health conditions (gestational hypertension, gestational diabetes, prenatal weight gain), prenatal health care (prenatal care in first trimester, Kessner Index of prenatal care), and prenatal health behavior risks (prenatal smoking, prenatal alcohol use). These variables were dichotomous, with 3 exceptions: The Kessner Index variable (with 3 levels, inadequate, intermediate, and adequate)28 is a measure of prenatal care that incorporates whether care was initiated in the first trimester and adjusts for the timing and quantity of visits throughout pregnancy. Maternal prepregnancy BMI was categorized as underweight, normal weight, overweight, and obese, according to the World Health Organization classification criteria.29 Finally, the prenatal weight gain variable had 3 categories, not enough, adequate, and too much, and was calculated using Institute of Medicine guidelines, which take into account prepregnancy BMI and gestational age at delivery.30
Analysis
We calculated frequencies summarizing Kalamazoo County and Michigan birth characteristics. For analytical purposes, we divided covariates into those unrelated to HBHS participation, such as marital status and prepregnancy diabetes, and those potentially influenced by HBHS participation, such as prenatal weight gain and adequacy of prenatal care. After stratifying for race, we conducted statistical comparisons between HBHS participants and all nonparticipants regarding unrelated covariates using the Pearson χ2 test. We used the Fisher exact test when cell counts were expected to drop below 5. HBHS-related covariates were compared between participants and their matched non-HBHS counterparts, stratified by race, using the McNemar nonparametric statistical test for related samples. We performed a statistical test of differences in birth outcomes between participants and their non-HBHS matches using repeated-measures generalized linear model testing. We conducted all tests with 2-tailed significance and set significance levels at P ≤ .05. All data analyses were completed using SPSS version 19.0 (IBM, Armonk, NY).
RESULTS
As seen in Table 1, the maternal health and infant birth profile of Kalamazoo County represents that of the state as well as the nation. The racial distribution, adolescent pregnancy rate, marriage rate, health indicators, and birth outcomes are typical, as are the socioeconomic indicators of insurance status and educational level. The only areas in which Kalamazoo County stands out are its smaller Hispanic population (5.9% compared with 23.6% nationally) and a gestational diabetes rate that is twice as high as that of either the state or the nation (10.6% in Kalamazoo vs 4.4% in Michigan and 5.1% nationally).
TABLE 1—
Comparison of Kalamazoo County, State of Michigan, and National Selected Maternal and Child Characteristics: 2010
| Variable | 2010 Kalamazoo County Births (n = 4734), % | 2010 Michigan Births (n = 114 717), % | 2010 National Births (n = 3 999 386), % |
| Maternal characteristics | |||
| Race | |||
| White | 82.2 | 74.2 | 76.7 |
| Black | 13.9 | 19.3 | 15.9 |
| Asian | 2.0 | 3.2 | 1.7 |
| Native American | 0.2 | 0.7 | 6.2 |
| Other | 1.8 | 2.6 | … |
| Hispanic ethnicity | |||
| Yes | 5.9 | 7.1 | 23.6 |
| No | 94.1 | 92.9 | 75.7 |
| Age, y | |||
| < 20 | 9.1 | 9.5 | 9.3 |
| ≥ 20 | 90.9 | 90.5 | 90.7 |
| Marital status | |||
| Unmarried | 37.9 | 39.4 | 40.8 |
| Married | 62.1 | 60.6 | 59.2 |
| Health insurance | |||
| Private | 51.9 | 54.3 | NA |
| Public, Medicaid | 48.1 | 45.7 | NA |
| Education | |||
| Not HS graduate | 11.5 | 15.5 | NA |
| HS graduate | 88.5 | 84.5 | NA |
| Paragravida | |||
| First pregnancy | 29.9 | 32.7 | NA |
| Previous pregnancies | 70.1 | 67.3 | NA |
| Previous poor outcomea | |||
| Yes | 1.5 | 2.0 | NA |
| No | 98.5 | 98.0 | NA |
| Prepregnancy diabetes or hypertension | |||
| Yes | 1.7 | 2.0 | NA |
| No | 98.3 | 98.0 | NA |
| Gestational diabetes or hypertension | |||
| Yes | 17.3 | 9.1 | 9.4 |
| No | 82.7 | 90.9 | 90.6 |
| BMI category | |||
| Under (< 18.5) | 3.5 | 3.5 | NA |
| Normal (18.5–24.9) | 42.8 | 44.5 | NA |
| Overweight (25.0–29.9) | 26.1 | 25.9 | NA |
| Obese (≥ 30.0) | 27.6 | 25.9 | NA |
| Prenatal smoking | |||
| Yes | 18.3 | 20.8 | NA |
| No | 81.6 | 78.2 | NA |
| Prenatal alcohol use | |||
| Yes | 2.3 | 0.4 | NA |
| No | 97.7 | 99.6 | NA |
| Kessner Index of prenatal care | |||
| Inadequate | 7.1 | 8.3 | NA |
| Intermediate | 28.5 | 21.4 | NA |
| Adequate | 64.0 | 68.1 | NA |
| Child characteristics | |||
| Birth weight | |||
| Low (< 2500 g) | 9.8 | 8.4 | 8.1 |
| Adequate (≥ 2500 g) | 90.2 | 91.6 | 91.9 |
| Gestation | |||
| Premature (< 37 wk) | 11.5 | 10.2 | 12.0 |
| Full term (≥ 37 wk) | 88.5 | 89.8 | 88.0 |
Preenrollment Maternal Characteristics Not Influenced by HBHS
Over the 3-year study period, 9336 women delivered live infants while residing in Kalamazoo County. Of these, 1743 self-reported their race as Black on their infant’s birth record form and 7174 reported their race as White. The race-stratified comparison groups shown in Table 2 demonstrate the disproportionate program participation of Black women relative to their representation in the larger population; they made up 65% of the HBHS sample (95/147 HBHS participants) yet only 18.7% of the total population for the same time period (1743 of the total population of 9336).
TABLE 2—
Preenrollment Characteristics of HBHS Participants and Nonparticipants, Stratified by Race: Kalamazoo County, MI; 2008–2010
| Black |
White |
|||||
| Variable | HBHS (n = 95), No. (%) | Non-HBHS (n = 1648), No. (%) | P | HBHS (n = 52), No. (%) | Non-HBHS (n = 7122), No. (%) | P |
| Hispanic ethnicitya | .62 | < .001 | ||||
| Yes | 0 | 19 (1.2) | 16 (30.8) | 389 (5.5) | ||
| No | 95 (100.0) | 1628 (98.8) | 36 (69.2) | 6732 (94.5) | ||
| Missing values | 1 | 1 | ||||
| Age, y | < .001 | < .001 | ||||
| < 20 | 40 (42.1) | 362 (22.0) | 13 (25.0) | 476 (6.7) | ||
| ≥ 20 | 55 (57.9) | 1286 (78.0) | 39 (75.0) | 6646 (93.3) | ||
| Married | .002 | < .001 | ||||
| Yes | 6 (6.3) | 317 (19.2) | 16 (30.8) | 4821 (67.7) | ||
| No | 89 (93.7) | 1331 (80.8) | 36 (69.2) | 2301 (32.3) | ||
| Insurancea | < .001 | < .001 | ||||
| Private | 1 (1.1) | 274 (16.6) | 1 (1.9) | 4412 (62.0) | ||
| Public | 93 (98.9) | 1372 (83.4) | 51 (98.1) | 2701 (38.0) | ||
| Missing values | 1 | 2 | 9 | |||
| Educationa | < .001 | < .001 | ||||
| Not HS graduate | 49 (51.6) | 416 (25.2) | 22 (42.3) | 658 (9.2) | ||
| HS graduate | 46 (48.4) | 1232 (74.8) | 30 (57.7) | 6462 (90.8) | ||
| Missing values | 2 | |||||
| Paragravida | .181 | .445 | ||||
| Yes | 32 (33.7) | 451 (27.4) | 19 (36.5) | 2250 (31.6) | ||
| No | 63 (66.3) | 1197 (72.6) | 33 (63.5) | 4872 (68.4) | ||
| Previous poor outcomea | .556 | .427 | ||||
| Yes | 8 (12.8) | 124 (10.4) | 3 (9.1) | 284 (5.8) | ||
| No | 55 (87.3) | 1072 (89.6) | 30 (90.9) | 4585 (94.2) | ||
| Missing values | 1 | 3 | ||||
| Prepregnancy diabetes or hypertension | .716 | .573 | ||||
| Yes | 2 (2.1) | 33 (2.0) | 1 (1.9) | 115 (1.6) | ||
| No | 93 (97.9) | 1615 (98.0) | 51 (98.1) | 7007 (98.4) | ||
| BMI categorya | .381 | .373 | ||||
| Under (< 18.5 kg/m2) | 4 (4.3) | 68 (4.1) | 2 (3.9) | 244 (3.4) | ||
| Normal (18.5–24.9 kg/m2) | 41 (43.6) | 591 (36.1) | 30 (58.8) | 3336 (46.9) | ||
| Overweight (25.0–29.9 kg/m2) | 17 (18.1) | 407 (24.8) | 10 (19.6) | 1834 (25.8) | ||
| Obese (≥ 30.0 kg/m2) | 32 (34.0) | 573 (35.0) | 9 (17.6) | 1693 (23.8) | ||
| Missing values | 1 | 9 | 1 | 15 | ||
| Initiated prenatal care in first trimestera | .414 | .277 | ||||
| Yes | 64 (67.4) | 1038 (63.2) | 44 (86.3) | 5687 (80.2) | ||
| No | 31 (32.6) | 604 (36.8) | 7 (13.7) | 1405 (19.8) | ||
| Missing values | 6 | 1 | 30 | |||
Note. BMI = body mass index; HBHS = Healthy Babies Healthy Start; HS = high school.
Percentages are based on nonmissing data only. For Black participants, no. of previous pregnancies = 63 for HBHS and 1197 for non-HBHS; for White participants, no. of previous pregnancies = 33 for HBHS and 4872 for non-HBHS.
Among Black women delivering babies during the study period, those who enrolled in HBHS were significantly more likely than other Black women to be adolescent, unmarried, on Medicaid insurance, and either currently in high school or to have dropped out of high school. Among White women, HBHS participants were 6 times more likely to be Hispanic. Just as with Black HBHS participants, White participants, compared with their nonparticipant White counterparts, were more likely to be adolescent, unmarried, on Medicaid insurance, and without a high school degree. Within each racial category, the differences we have noted constituted the factors on which participants were matched.
Regardless of race, participants and nonparticipants had similar health histories, both obstetric history (being primagravida and having had a prior pregnancy that resulted in stillbirth, low birth weight, or intrauterine growth retardation) and general health (having diabetes or hypertension before the current pregnancy and prepregnancy BMI). They also had comparable rates of prenatal care initiation in the first trimester.
Although not the focus of this article, it is notable that Black women in the study were characterized by significantly higher risk factors than White women. They were more likely to be adolescent (19.6% and 7.2%, respectively; P < .001), single (79.1% and 30.2%, respectively; P < .001), without a high school diploma (25.1% and 12.4%, respectively; P < .001), on Medicaid (57.4% and 42.4%, respectively; P < .001), and obese (33.9% and 24.8%, respectively; P < .001).
Matched Comparisons of Health Care, Health Behaviors, and Birth Outcomes
Table 3 illustrates the effectiveness of the matching procedure. As noted previously, we developed the comparison groups for Black and White HBHS participants using nearly the same set of factors (adolescence, marital status, insurance status, and high school graduation), except that the White group was also matched on Hispanic ethnicity. Even though we used the same variables, the importance of matching each racial group separately is clear: Black and White HBHS participants had different configurations of these variables, and each configuration was precisely matched in their respective comparison group. Note that we eliminated 6 Black HBHS births and 2 White HBHS births before matching to remove multiple-gestation pregnancies and their subsequent effect on prenatal health indicators and birth outcomes.
TABLE 3—
Matched Comparison of HBHS Participants and Nonparticipants on Health Access, Health Behaviors, and Birth Outcomes, Stratified by Race, for Singleton Gestations Only: Kalamazoo County, MI; 2008–2010
| Black, Matched |
White, Matched |
|||||
| Variable | HBHS (n = 89), No. (%) or Mean | Non-HBHS (n = 89), No. (%) or Mean | P | HBHS (n = 50), No. (%) or Mean | Non-HBHS (n = 50), No. (%) or Mean | P |
| Maternal factors used in propensity score match | ||||||
| Age | > .999 | > .999 | ||||
| < 20 y | 38 (42.7) | 38 (42.7) | 13 (26.0) | 13 (26.0) | ||
| ≥ 20 y | 51 (57.3) | 51 (57.3) | 37 (74.0) | 37 (74.0) | ||
| Married | > .999 | > .999 | ||||
| Yes | 4 (4.5) | 4 (4.5) | 16 (32.0) | 16 (32.0) | ||
| No | 85 (95.5) | 89 (95.5) | 34 (68.0) | 34 (68.0) | ||
| Health insurancea | > .999 | > .999 | ||||
| Private | 1 (1.1) | 1 (1.1) | 1 (2.0) | 1 (2.0) | ||
| Public | 87 (98.9) | 88 (98.9) | 49 (98.0) | 49 (98.0) | ||
| Missing values | 1 | |||||
| Education | > .999 | > .999 | ||||
| Not HS graduate | 45 (50.6) | 45 (50.6) | 22 (44.0) | 22 (44.0) | ||
| HS graduate | 44 (49.4) | 44 (49.4) | 28 (56.0) | 28 (56.0) | ||
| Hispanic ethnicity | NA | NA | > .999 | |||
| Yes | 16 (32.0) | 16 (32.0) | ||||
| No | 34 (68.0) | 34 (68.0) | ||||
| Prenatal health indicators | ||||||
| Gestational diabetes or hypertension | .791 | > .999 | ||||
| Yes | 9 (10.1) | 7 (7.9) | 11 (22.0) | 10 (20.0) | ||
| No | 80 (89.9) | 82 (92.1) | 39 (78.0) | 40 (80.0) | ||
| Sexually transmitted infection, prenatala | .377 | > .999 | ||||
| Yes | 20 (22.7) | 14 (16.1) | 6 (12.2) | 6 (12.0) | ||
| No | 68 (77.3) | 73 (83.9) | 43 (87.8) | 44 (88.0) | ||
| Missing values | 1 | 2 | 1 | |||
| Prenatal smoking | .01 | .424 | ||||
| Yes | 37 (41.6) | 20 (22.5) | 17 (34.0) | 13 (26.0) | ||
| No | 52 (58.4) | 69 (77.5) | 33 (66.0) | 37 (74.0) | ||
| Prenatal alcohol use | .688 | > .999 | ||||
| Yes | 4 (4.5) | 2 (2.2) | 1 (2.0) | 2 (4.0) | ||
| No | 85 (95.5) | 87 (97.8) | 49 (98.0) | 48 (96.0) | ||
| Prenatal weight gaina | ||||||
| Too little | 12 (13.5) | 22 (25.0) | .1 | 8 (17.4) | 7 (14.6) | > .999 |
| Adequate | 21 (23.6) | 22 (25.0) | .85 | 14 (30.4) | 12 (25.0) | .629 |
| Too much | 51 (57.3) | 44 (50.0) | .291 | 24 (52.2) | 29 (60.4) | .503 |
| Missing values | 5 | 1 | 4 | 2 | ||
| Kessner Index of prenatal carea | ||||||
| Inadequate | 8 (9.0) | 17 (19.1) | .078 | 0 | 6 (12.0) | .031 |
| Intermediate | 34 (38.2) | 36 (40.4) | .877 | 16 (32.7) | 19 (38.0) | .629 |
| Adequate | 47 (52.8) | 36 (40.4) | .136 | 33 (67.3) | 25 (50.0) | .064 |
| Missing values | 1 | |||||
| Intent to breastfeeda | .635 | .556 | ||||
| Yes | 43 (48.9) | 39 (43.8) | 33 (66.0) | 28 (57.1) | ||
| No | 45 (51.1) | 50 (56.2) | 17 (34.0) | 21 (42.9) | ||
| Missing values | 1 | 1 | ||||
| Birth outcomes | ||||||
| Birth weight, g | 3111 | 2918 | .05 | 3199 | 3243 | .701 |
| Birth weight category | ||||||
| Low (< 2500 g) | 9 (10.1) | 18 (20.2) | .108 | 7 (14.0) | 4 (8.0) | .453 |
| Adequate | 80 (89.9) | 71 (79.8) | 43 (86.0) | 46 (92.0) | ||
| Gestation, wk | 38.7 | 38.1 | .26 | 39.2 | 39.6 | .547 |
| Gestation category | > .999 | > .999 | ||||
| Premature (< 37 wk) | 15 (16.9) | 16 (18.0) | 4 (8.0) | 5 (10.0) | ||
| Full term (≥ 37 wk) | 74 (83.1) | 73 (82.0) | 46 (92.0) | 45 (90.0) | ||
Note. HBHS = Healthy Babies Healthy Start; HS = high school; NA = not applicable.
Percentages are based on nonmissing data only.
Compared with their own matched nonparticipant comparison group, Black HBHS participants were similar on most of the measured prenatal health indicators shown in Table 3 (gestational diabetes and hypertension, sexually transmitted infection, prenatal alcohol consumption, intent to breastfeed). The only statistically significant difference was that Black HBHS participants were nearly twice as likely to smoke prenatally as their matched group (41.6% Black HBHS participants vs 22.5% Black matched nonparticipants; P = .01). Two additional factors, prenatal care and prenatal weight gain, were trending toward significance (i.e., their P values did not meet criteria for statistical significance but, at P ≤ .1, approached significance). Compared with their matched counterparts, fewer Black participants had inadequate prenatal care (9.0% HBHS vs 19.1% comparison; P = .078), and fewer gained inadequate weight (13.5% HBHS vs 25.0% comparison; P = .1).
Comparisons between White HBHS women and the White nonparticipants matched to them revealed similarity on several of the same measures (gestational diabetes and hypertension, sexually transmitted infection, prenatal alcohol consumption, intention to breastfeed) as well as dissimilarity on prenatal care. As with their Black counterparts, the White participant group was less likely to have inadequate prenatal care (0% HBHS vs 12.0% comparison; P = .031), with the between-groups difference reaching statistical significance. Unlike Black participants and their comparisons, however, White participants and their comparisons did not have different rates of prenatal smoking (34.0% White HBHS participants vs 26.0% White matched nonparticipants; P = .424).
Black HBHS participants had statistically significant higher birth weights, averaging nearly 200 g more than their matched comparison group. When categorized into low birth weight groups (above and below the 2500-g threshold), the difference between Black HBHS participants and their comparison group (10.1% and 20.2% in the low birth weight category, respectively) did not reach statistical significance (P = .108). We found no difference between Black participants and matched nonparticipants regarding gestational age or premature birth.
In a multivariate regression analysis combining all 4 matched groups, we found a significant main effect for race for birth weight (White mean = 3221 g, Black mean 3015 g; b = −324.87; P = .006) and gestation (White mean = 39.4 weeks, Black mean 38.4 weeks; b = −1.45; P = .015) and nonsignificant effects for HBHS participation (birth weight, P = .738; and gestation, P = .639) as well as for the HBHS × race interaction (birth weight, P = .154; and gestation, P = .283).
DISCUSSION
Study results showing significantly improved birth weight for infants of Black HBHS participants but not for infants of White participants suggest that HBHS case management may be differentially beneficial for Black women. After matching and analyzing data for Black and White participants separately to isolate racially variable predictors, we found that Black HBHS participants, despite a rate of prenatal smoking nearly double that of Black nonparticipants (a leading risk factor for poor birth outcomes),31 delivered infants of significantly higher birth weight than Black nonparticipants, whereas White HBHS participants’ birth outcomes were similar to those of their matched White counterparts. The strong negative effect associated with Black race and birth outcomes, seen in the regression models combining the 4 matched groups, highlights the value of a race-stratified analytical approach to detect potential program effects. It also reveals the force of the trend that such a program is working to reverse.
In this study, indicators pointing to possible improvements in amount of prenatal care and prenatal weight gain among Black participants compared with Black nonparticipants (both factors trending toward statistical significance) may be clues to the mechanisms through which HBHS could be having an impact. Prenatal care has certainly been found to be strongly associated with improved birth outcomes, especially among Black women.32,33 Increasing the quantity of prenatal care, however, although a positive contributor, is not sufficient in and of itself to increase birth weight or gestational age to the point of eliminating disparities.34 The inconsistent role of prenatal care in birth outcomes in this study bears this out: The significant increase in birth weight among Black participants’ infants was preceded by a moderate, not-quite-significant increase in prenatal care visits, whereas the significant increase in prenatal care among White participants was not followed by better birth outcomes. Alternatively, perhaps the modest improvement in optimal prenatal weight gain among Black HBHS women exerts an inordinate influence on the health of their pregnancies. Certainly, previous studies of this same population have found that prenatal weight gain is a leading predictor of birth outcomes35 and that weight, in general, has been tied to levels of perceived discrimination.13,36 Moreover, existing evidence has revealed that patterns of maternal nutrition and attitudes toward weight gain are deeply embedded within personal habits and cultural norms,37,38 making them modifiable in the individualized, culturally sensitive approach of HBHS.
The fact that Black HBHS participants demonstrated gains in birth weight but not in gestation could reflect differences between the 2 indicators regarding their operationalization or differences in their underlying etiology. Birth weight and gestational age are common perinatal health indicators, used both individually and together.39 Methodologically, birth weight tends to be more accurately and more easily measured, and thus more reliable, than gestational age.26,40 Etiologically, although birth weight and gestational age often overlap, there are important distinctions between them. Birth weight is actually the end result of 2 separate processes, 1 of which is gestational duration and the other of which is fetal growth rate.41 Although much is still unknown about the underlying mechanisms of these 2 processes, studies have suggested that race, consistently and strongly correlated to both, may contribute differently to each, either in the strength of its impact or in its causal role.27,42,43
The ultimate goal of public health programs such as Healthy Start is to eliminate health and psychosocial disparities between Blacks and Whites. However, study findings of markedly poorer preprogram differences illustrate how far we are from achieving this goal. As in communities across the nation, pregnant Black women in the Kalamazoo County are, as a group, younger, poorer, less educated, and in worse health than pregnant White women.44,45 Programs shown to help Black women with these additional burdens tend to have broad and racially specific foci.6,46,47 These programs focus on enhancing individuals’ coping skills (for chronic stress as well as for discrete episodes of racial discrimination),48–51 empowering them through knowledge and access to resources52–54 and specifically targeting institutional disparities in diagnosis, treatment, and medical follow-up.55–59 Programs that exclusively zero in on individual risk factors (such as smoking, substance abuse, depression, or domestic violence), however, have mixed effects on Black birth outcomes.60–65
Although we do not provide definitive information about the pathways linking specific HBHS services to the improved birth weight of Black participants’ infants (especially relative to that of White participants’ infants), the HBHS program integrates characteristics that have in other studies shown promise in improving racial disparities. The home visitation format has been linked to increased self-efficacy, relationship building between community and provider, and improved birth outcomes.66 The multiprovider model advocated by HBHS, combining paraprofessionals and licensed health care providers, can moderate the impact of everyday stress and contribute to personal empowerment.67,68 Along these same lines, using liaison health workers from one’s own culture and community is associated with a shift in perceived locus of health control from external to internal.66 Finally, adopting a social work approach, in which case managers assist women with targeted health information and facilitate linkages to community resources, can mitigate the impact of social class on stress levels.69
Limitations
These findings should be viewed in light of the following study limitations. Study variables were restricted to those contained within the Michigan Department of Community Health’s birth records data set; as a result, we had no direct measures of internal conditions of stress, perceived racism, or personal empowerment, key constructs moderating the effect of race on health. Additionally, several covariates known to be important predictors of birth outcomes, including mental health, family violence, drug abuse, and homelessness, were also missing from the analysis, although somewhat mitigated by the inclusion of several variables (smoking, sexually transmitted infections, education level, insurance level) known to correlate highly with the unmeasured factors.37,70 A direct measure of income was also missing from the analysis; however, we included insurance status as a proxy measure of income. Also, although matching removed the self-selection bias associated with the matched demographic variables, it is possible that HBHS participants may be different in other ways that contribute to their improved birth outcomes. Although the stratified matched-comparison approach controls for significant preprogram differences between participants and nonparticipants, it does preclude examining the degree to which these factors (adolescence, marital status, insurance status, education, and Hispanic ethnicity) may serve as mechanisms for the postenrollment differences in prenatal care, prenatal weight gain, and birth weight). A final limitation of this study is that by focusing on individuals, we did not account for the impact of the institutional structures and cultural climates that may perpetuate discrimination and racism.15
Conclusions
In a community population reflecting the maternal–infant profile of women across the country, our findings confirmed the profound discrepancy in underlying risk factors and resulting infant mortality that currently exists between Black and White women. Using propensity scores to match each HBHS participant with a demographically similar nonparticipant and stratifying the analysis by race, we have shown that HBHS case management is associated with having infants with higher birth weights among Black women, but not among White women. These findings suggest that case management home visitation programs may play a role in reducing racial disparities.
Acknowledgments
This research was funded by Kalamazoo Healthy Babies Healthy Start as part of its local evaluation efforts.
We acknowledge the contributions of Annie Wendt, MPH, Kalamazoo County Health and Community Services epidemiologist, and, for her methodological advice, Amy Curtis, PhD, MPH, Western Michigan University PhD Program in Interdisciplinary Health Sciences. We also recognize the amazing work of case managers and health educators within Kalamazoo Healthy Babies Healthy Start, as well as the strength and courage of the women they serve.
Human Participant Protection
Permission to access data was provided by the Michigan Department of Community Health Vital Records and Health Statistics Section, and institutional review board approval was provided by both Borgess Medical Center and Bronson Methodist Hospital, Kalamazoo, MI.
References
- 1.Martin JA, Hamilton BE, Ventura SJ et al. Births: final data for 2010. Natl Vital Statistics Rep. 2012;61(1):1–71. [PubMed] [Google Scholar]
- 2.Krieger N, Rehkopf DH, Chen JT et al. The fall and rise of US inequities in premature mortality: 1960-2002. PLoS Med. 2008;5(2):e46. doi: 10.1371/journal.pmed.0050046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Orsi JM, Margellos-Anast H, Whitman S. Black-White health disparities in the United States and Chicago: a 15 year progress analysis. Am J Public Health. 2010;100(2):349–356. doi: 10.2105/AJPH.2009.165407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murphy SL, Xu J, Kochanek KD. Deaths: preliminary data for 2010. Natl Vital Stat Rep. 2012;60(4):1–51. [PubMed] [Google Scholar]
- 5.Giurgescu C, McFarlin BI, Lomax J, Craddock C, Albrecht A. Racial discrimination and the Black-White gap in adverse birth outcomes: a review. J Midwifery Womens Health. 2011;56(4):362–370. doi: 10.1111/j.1542-2011.2011.00034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003;7(1):13–30. doi: 10.1023/a:1022537516969. [DOI] [PubMed] [Google Scholar]
- 7.Rosenberg L, Palmer JR, Wise LA, Horton NJ, Corwin MJ. Perceptions of racial discrimination and the risk of preterm birth. Epidemiology. 2002;13(6):646–652. doi: 10.1097/00001648-200211000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Yen IH, Kaplan GA. Neighborhood social environment and risk of death: multilevel evidence from the Alameda County study. Am J Epidemiol. 1999;149(10):898–907. doi: 10.1093/oxfordjournals.aje.a009733. [DOI] [PubMed] [Google Scholar]
- 9.Winkleby M, Cubbin C, Ahn D. Effect of cross-level interaction between individual and neighborhood socioeconomic status on adult mortality rates. Am J Public Health. 2006;96(12):2145–2153. doi: 10.2105/AJPH.2004.060970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kramer MR, Hogue CR. Place matters: variation in the Black/White very preterm birth rate across U.S. metropolitan areas, 2002-2004. Public Health Rep. 2008;123(5):576–585. doi: 10.1177/003335490812300507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mouton CP. Impact of perceived racial discrimination on health screening in Black women. J Health Care Poor Underserved. 2010;21(1):287–300. doi: 10.1353/hpu.0.0273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borrell LN, Jacobs DR, Jr, Williams DR et al. Self-reported racial discrimination and substance use in the coronary artery risk development in adults study. Am J Epidemiol. 2007;166(9):1068–1079. doi: 10.1093/aje/kwm180. [DOI] [PubMed] [Google Scholar]
- 13.Hunte HE, Williams DR. The association between perceived discrimination and obesity in a population-based multiracial and multiethnic adult sample. Am J Public Health. 2009;99(7):1285–1292. doi: 10.2105/AJPH.2007.128090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shariff-Marco S, Klassen AC, Bowie JV. Racial/ethnic differences in self-reported racism and its association with cancer-related health behaviors. Am J Public Health. 2010;100(2):364–374. doi: 10.2105/AJPH.2009.163899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Health Resources and Services Administration, Maternal and Child Health Bureau. Evidence of Trends, Risk Factors, and Intervention Strategies. Washington, DC: US Department of Health and Human Services, Health Resources and Services Administration; 2006. [Google Scholar]
- 16.Dankwa-Mullan I, Rhee KB, Williams K et al. The science of eliminating health disparities: summary and analysis of the NIH summit recommendations. Am J Public Health. 2010;100(suppl 1):S12–S18. doi: 10.2105/AJPH.2010.191619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Williams DR. Race, socioeconomic status, and health: the added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896:173–188. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- 18.Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- 19.Brand A, Walker Klein D, Hargreaves M, Rosenbach M. Intermediate outcomes, strategies, and challenges of eight Healthy Start projects. Matern Child Health J. 2010;14(5):654–665. doi: 10.1007/s10995-008-0421-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenbach M, O’Neil S, Cook B, Trebino L, Walker Klein D. Characteristics, access, utilization, satisfaction, and outcomes of Healthy Start participants in eight sites. Matern Child Health J. 2010;14(5):666–679. doi: 10.1007/s10995-009-0474-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ingram DD, Parker JD, Schenker N et al. United States Census 2000 population with bridged race categories. Vital Health Statistics. 2003;2(135):1–55. [PubMed] [Google Scholar]
- 22.Guo S, Fraser M. Propensity Score Analysis. Los Angeles, CA: Sage Publications; 2010. [Google Scholar]
- 23. Michigan Department of Community Health, Division for Vital Records and Health Data Development. Live birth file and death file, preliminary results [summary data file]. 2012.
- 24.Murphy SL, Xu J, Kochanek KD. Deaths: preliminary data for 2010. Natl Vital Stat Rep. 2012;60(4):1–52. [PubMed] [Google Scholar]
- 25.US Department of Health and Human Services. Prior HHS Poverty Guidelines and Federal Register References. Available at: http://aspe.hhs.gov/poverty/figures-fed-reg.cfm. Accessed December 6, 2013.
- 26.Ma S, Finch BK. Birth outcome measures and infant mortality. Popul Res Policy Rev. 2010;29(6):865–891. [Google Scholar]
- 27.Wilcox AJ. On the importance—and the unimportance—of birth weight. Int J Epidemiol. 2001;30(6):1233–1241. doi: 10.1093/ije/30.6.1233. [DOI] [PubMed] [Google Scholar]
- 28.Kessner DM, Singer J, Kalk CE, Schlesinger ER. Infant death: an analysis by maternal risk and health care, vol 1 of Contrasts in health status. Am J Dis Child. 1974;127(6):914. [Google Scholar]
- 29.World Health Organization. WHO Physical Status: The Use and Interpretation of Anthropometry: Report of a WHO Expert Committee. Geneva, Switzerland: World Health Organization; 1995. Technical Report Series 854. [PubMed] [Google Scholar]
- 30.Institute of Medicine. Nutrition During Pregnancy. Washington, DC: National Academy of Sciences; 1990. [Google Scholar]
- 31.Ashdown-Lambert JR. A review of low birth weight: predictors, precursors and morbidity outcomes. J R Soc Promot Health. 2005;125(2):76–83. doi: 10.1177/146642400512500211. [DOI] [PubMed] [Google Scholar]
- 32.Kotelchuck M. The adequacy of prenatal care utilization index: its US distribution and association with low birthweight. Am J Public Health. 1994;84(9):1486–1489. doi: 10.2105/ajph.84.9.1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hardy PJ. Environmental Stressors, Prenatal Care, and Low Birthweight [dissertation] Minneapolis, MN: Capella University; 2011. [Google Scholar]
- 34.Handler A, Kennelly J, Peacock N, editors. Reducing Racial/Ethnic Disparities in Reproductive and Perinatal Outcomes: The Evidence From Population-Based Interventions. New York, NY: Springer; 2010. [Google Scholar]
- 35.Kothari CL, Wendt A, Liggins O, Overton J, Sweezy CL. Assessing maternal risk for fetal-infant mortality: a population-based study to prioritize risk reduction in a Healthy Start community. Matern Child Health J. 2011;15(1):68–76. doi: 10.1007/s10995-009-0561-3. [DOI] [PubMed] [Google Scholar]
- 36.Mays VM, Cochran SD, Barnes NW. Race, race-based discrimination, and health outcomes among African Americans. Annu Rev Psychol. 2007;58:201–225. doi: 10.1146/annurev.psych.57.102904.190212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Olson CM, Strawderman MS. Modifiable behavioral factors in a biopsychosocial model predict inadequate and excessive gestational weight gain. J Am Diet Assoc. 2003;103(1):48–54. doi: 10.1053/jada.2003.50001. [DOI] [PubMed] [Google Scholar]
- 38.Cunningham S, Fahey S, Thompson B. Promoting a Healthy Weight in Women of Reproductive Age: Experiences & Lessons Learned From Eight State/Local Health Department Teams. Sacramento, CA: California Department of Public Health; 2008. [Google Scholar]
- 39.Ma S. A Good Start in Life: Revisiting Racial and Ethnic Disparities in Health Outcomes at and After Birth [dissertation] Santa Monica, CA: Pardee Rand Graduate School; 2007. [Google Scholar]
- 40.Gjessing HK, Skjaerven R, Wilcox AJ. Errors in gestational age: evidence of bleeding early in pregnancy. Am J Public Health. 1999;89(2):213–218. doi: 10.2105/ajph.89.2.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kramer MS. Maternal nutrition, pregnancy outcome and public health policy. CMAJ. 1998;159(6):663–665. [PMC free article] [PubMed] [Google Scholar]
- 42.Kramer MS. Determinants of low birth weight: methodological assessment and meta-analysis. Bull World Health Organ. 1987;65(5):663–737. [PMC free article] [PubMed] [Google Scholar]
- 43.Behrman RE, Butler AS. Preterm Birth: Causes, Consequences and Prevention. Washington, DC: National Academies Press; 2007. [PubMed] [Google Scholar]
- 44.Martinez G, Daniels K, Chandra A. Fertility of men and women aged 15-44 years in the United States: national survey of family growth, 2006-2010. Natl Health Stat Rep. 2012;51:1–28. [PubMed] [Google Scholar]
- 45.Centers for Disease Control and Prevention. Vital signs: teen pregnancy—United States, 1991-2009. MMWR Morb Mortal Wkly Rep. 2011;60(13):414–420. [PubMed] [Google Scholar]
- 46.Brondolo E, Gallo LC, Myers HF. Race, racism and health: disparities, mechanism and interventions. J Behav Med. 2009;32(1):1–8. doi: 10.1007/s10865-008-9190-3. [DOI] [PubMed] [Google Scholar]
- 47.Krieger N. Proximal, distal, and the politics of causation: what’s level got to do with it? Am J Public Health. 2008;98(2):221–230. doi: 10.2105/AJPH.2007.111278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Collins JW, Jr, David RJ, Handler A, Wall S, Andes S. Very low birthweight in African American infants: the role of maternal exposure to interpersonal racial discrimination. Am J Public Health. 2004;94(12):2132–2138. doi: 10.2105/ajph.94.12.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brondolo E, ver Halen NB, Pencille M, Beatty D, Contrada RJ. Coping with racism: a selective review of the literature and a theoretical and methodological critique. J Behav Med. 2009;32(1):64–88. doi: 10.1007/s10865-008-9193-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nuru-Jeter A, Dominguez TP, Hammond WP et al. “It's the skin you're in”: African-American women talk about their experiences of racism. An exploratory study to develop measures of racism for birth outcome studies. Matern Child Health J. 2009;13(1):29–39. doi: 10.1007/s10995-008-0357-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rankin KM, David RJ, Collins JWJ. African American women’s exposure to interpersonal racial discrimination in public settings and preterm birth: the effect of coping behaviors. Ethn Dis. 2011;21(3):370–376. [PubMed] [Google Scholar]
- 52.Pieterse AL. An exploratory investigation of the relationship between racism, racial identity, perceptions of health, and health locus of control among Black American women. J Health Care Poor Underserved. 2010;21(1):334–348. doi: 10.1353/hpu.0.0244. [DOI] [PubMed] [Google Scholar]
- 53.Dahlgren G, Whitehead M. Policies and Strategies to Promote Social Equity in Health. Copenhagen, Denmark: World Health Organization, Regional Office for Europe; 2007. [Google Scholar]
- 54.Anachebe NF. Racial and ethnic disparities in infant and maternal mortality. Ethn Dis. 2006;16(2 suppl 3):S3-71–76. [PubMed] [Google Scholar]
- 55.Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Relationship between quality of care and racial disparities in Medicare health plans. JAMA. 2006;296(16):1998–2004. doi: 10.1001/jama.296.16.1998. [DOI] [PubMed] [Google Scholar]
- 56.Schrag SJ, Arnold KE, Mohle-Boetani JC et al. Prenatal screening for infectious diseases and opportunities for prevention. Obstet Gynecol. 2003;102(4):753–760. doi: 10.1016/s0029-7844(03)00671-9. [DOI] [PubMed] [Google Scholar]
- 57.Kogan MD, Kotelchuck M, Alexander GR, Johnson WE. Racial disparities in reported prenatal care advice from health care providers. Am J Public Health. 1994;84(1):82–88. doi: 10.2105/ajph.84.1.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Anderson KO, Green CR, Payne R. Racial and ethnic disparities in pain: causes and consequences of unequal care. J Pain. 2009;10(12):1187–1204. doi: 10.1016/j.jpain.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 59.O’Neil SS, Lake T, Merrill A, Wilson A, Mann DA, Bartnyska LM. Racial disparities in hospitalizations for ambulatory care-sensitive conditions. Am J Prev Med. 2010;38(4):381–388. doi: 10.1016/j.amepre.2009.12.026. [DOI] [PubMed] [Google Scholar]
- 60.Wells N, Sbrocco T, Hsiao C et al. The impact of nurse case management home visitation on birth outcomes in African-American women. J Natl Med Assoc. 2008;100(5):547–552. doi: 10.1016/s0027-9684(15)31301-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Joseph JG, El-Mohandes AAE, Kiely M et al. Reducing psychosocial and behavioral pregnancy risk factors: results of a randomized clinical trial among high-risk pregnant African American women. Am J Public Health. 2009;99(6):1053–1061. doi: 10.2105/AJPH.2007.131425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Olds DL, Robinson J, O’Brien R et al. Home visiting by paraprofessionals and by nurses: a randomized, controlled trial. Pediatrics. 2002;110(3):486–496. doi: 10.1542/peds.110.3.486. [DOI] [PubMed] [Google Scholar]
- 63.Klerman LV, Ramey SL, Goldenberg RL et al. A randomized trial of augmented prenatal care for multiple-risk, Medicaid-eligible African American women. Am J Public Health. 2001;91(1):105–111. doi: 10.2105/ajph.91.1.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gonzalez-Calvo J, Jackson J, Hansford C, Woodman C, Remington RS. Nursing case management and its role in perinatal risk reduction: development, implementation, and evaluation of a culturally competent model for African American women. Public Health Nurs. 1997;14(4):190–206. doi: 10.1111/j.1525-1446.1997.tb00292.x. [DOI] [PubMed] [Google Scholar]
- 65.Ricketts SA, Murray EK, Schwalberg R. Reducing low birthweight by resolving risks: results from Colorado’s Prenatal Plus program. Am J Public Health. 2005;95(11):1952–1957. doi: 10.2105/AJPH.2004.047068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Berry E, Brady C, Cunningham SD . Federal Healthy Start Initiative: A National Network for Effective Home Visitation and Family Support Services. Washington, DC: National Healthy Start Association; 2010. [Google Scholar]
- 67.Roman LA, Gardiner JC, Lindsay JK et al. Alleviating perinatal depressive symptoms and stress: a nurse-community health worker randomized trial. Arch Womens Ment Health. 2009;12(6):379–391. doi: 10.1007/s00737-009-0083-4. [DOI] [PubMed] [Google Scholar]
- 68.Koger DC. The Influence of a Home Visitation, Parent Education Program on Locus of Control and Parenting Behaviors of Limited Resource Mothers. East Lansing, MI: Michigan State University, Department of Family and Child Ecology; 1999. [Google Scholar]
- 69.Livingood WC, Brady C, Pierce K et al. Impact of pre-conception health care: evaluation of social determinants focused intervention. Matern Child Health J. 2010;14(3):382. doi: 10.1007/s10995-009-0471-4. [DOI] [PubMed] [Google Scholar]
- 70.Beck LF, Morrow B, Lipscomb LE et al. Prevalence of selected maternal behaviors and experiences, Pregnancy Risk Assessment Monitoring System (PRAMS), 1999. MMWR Surveill Summ. 2002;51(2):1–27. [PubMed] [Google Scholar]