Abstract
Objectives. We evaluated whether a brief, universal, postnatal nurse home-visiting intervention can be implemented with high penetration and fidelity, prevent emergency health care services, and promote positive parenting by infant age 6 months.
Methods. Durham Connects is a manualized 4- to 7-session program to assess family needs and connect parents with community resources to improve infant health and well-being. All 4777 resident births in Durham, North Carolina, between July 1, 2009, and December 31, 2010, were randomly assigned to intervention and control conditions. A random, representative subset of 549 families received blinded interviews for impact evaluation.
Results. Of all families, 80% initiated participation; adherence was 84%. Hospital records indicated that Durham Connects infants had 59% fewer infant emergency medical care episodes than did control infants. Durham Connects mothers reported fewer infant emergency care episodes and more community connections, more positive parenting behaviors, participation in higher quality out-of-home child care, and lower rates of anxiety than control mothers. Blinded observers reported higher quality home environments for Durham Connects than for control families.
Conclusions. A brief universal home-visiting program implemented with high penetration and fidelity can lower costly emergency medical care and improve family outcomes.
The Maternal, Infant, and Early Childhood Home Visiting Program of the federal Patient Protection and Affordable Care Act of 2010 provides $1.5 billion for postnatal home-visiting programs to improve outcomes in the “reduction of emergency department visits.”1(p218) Because it is intended as an evidence-based public health policy, most of the funds support programs for demographically high-risk subgroups that have demonstrated efficacy in small randomized controlled trials.2–4 A meta-analysis5 of impact studies revealed empirical support for home visiting as a vehicle to reach proximal goals of providing emotional support for parents after birth, improving parenting behavior, and connecting families with individualized community resources to achieve distal impact on reducing emergency medical care. Although these programs are promising, no home-visiting program has ever scaled up successfully to demonstrate population impact on public health, despite the Institute of Medicine mandate to move from basic science to efficacy trials to effectiveness trials to population dissemination.6 To our knowledge, we describe the first-ever randomized controlled trial of a brief, postpartum universal nurse home-visiting program at the population level.
Scaling up for population impact encounters at least 4 challenges. First, home-visiting programs are rarely designed or evaluated for universal reach during a randomized controlled trial (e.g., Nurse-Family Parnership2 limits itself to demographically high-risk, primiparous mothers who voluntarily enroll in the 2nd trimester, a group that accounts for less than half of all maltreatment cases). Second, as programs scale up, penetration and retention often decline (e.g., 40% of targeted groups never enroll,7 and participant dropout after enrollment is 50%–67%8). Third, when a program is scaled up,9 quality and fidelity typically degrade as much as 50%. Finally, programs presume sufficient community capacity to meet families’ needs during a scaled-up dissemination. Impact depends on the home visitor’s ability to find community resources for a family.10 If a program is implemented during a small randomized controlled trial, the family gains a competitive advantage over nontreated families in accessing fixed-sum resources, but when brought to scale, families’ needs might exceed community capacity to provide services, lowering net impact on child outcomes. The Maternal, Infant, and Early Childhood Home Visiting Program legislation recognizes the importance of community capacity by requiring that programs address “improvements in the coordination of referrals for, and the provision of, other community resources and supports for eligible families.”1(p219) These referrals should be based on an individualized assessment of the family. To our knowledge, no program has systematically attempted to improve community capacity.
We report the development, implementation, and impact evaluation of a brief postnatal nurse home-visiting program called Durham Connects that was delivered universally in a mid-sized community with a high rate of poverty. We hypothesized that Durham Connects would achieve its aims to (1) reach most birthing families in the population, with high fidelity of implementation at reasonable cost; (2) improve the family’s connections to individually matched ongoing community resources based on assessed risk and need; (3) improve parenting and family functioning; and (4) improve infant public health outcomes cost beneficially. We report evaluation of aims 1 and 2 through implementation findings and cost analyses and evaluation of aims 3 and 4 through random assignment of all births over an 18-month enrollment period and in-home interviews with a random, representative subsample of families with infants aged 6 months.
METHODS
From July 1, 2009, through December 31, 2010, all 4777 residential births in Durham County, North Carolina, from the 2 hospitals serving the community (1 community hospital and 1 academic tertiary care hospital) were randomly assigned according to birth date, with families of infants with even birth dates assigned to receive Durham Connects and families of infants with odd birth dates assigned to receive services as usual. We evaluated implementation for all 2327 even birth-date families.
We selected a random subsample of the 4777 families to evaluate impact 6 months after infant birth. Sample size was based on statistical power analyses. Following Cohen11 and using G*Power software (version 3.1; Institute for Experimental Psychology, Heinrich Heine University Dusseldorf, Germany),12 we performed power analyses that, estimating at least .80 power and a significance level of .05, indicated that a sample of 549 was sufficient to detect hypothesized effects: an effect size of .21 for continuous variables and a 9% difference for dichotomous variables. We used a computer algorithm with publicly available birth records to randomly select 1 infant per birth date across the enrollment period. These families were contacted when the infant was aged 6 months to participate in an institutional review board–approved study of infant development. Interviewers were blind to intervention status, and families were blind to any relation between the interview and Durham Connects. Nonconsenting families were replaced by a randomly selected same-ethnicity family with an infant of the same birth date. We initially selected 682 families, of whom 549 (80.5%) participated, 1 per birth date across the enrollment period. Eighteen families were subsequently determined to be ineligible because of hospital discharge record errors (e.g., incorrect child birth date), resulting in a final selection sample of 664 families, of whom 531 (80.0%) participated.
Durham Connects Program
In response to the challenges we have noted, Durham Connects was designed for population-level implementation from the outset. It was piloted for 3 years with iterative improvement before testing by a randomized controlled trial. We learned that, to be implemented at scale with high fidelity, a program must be short term, inexpensive, community owned, and aligned with community service providers. To reach a high proportion of families and to have population impact, a program must be delivered universally so that families do not perceive that participation stigmatizes them as poor or risky and to maximize community acceptance. However, it must also use funds efficiently. Durham Connects engages every family but rapidly triages and concentrates resources on families with assessed higher needs. Durham Connects begins with a recruitment session at the birthing hospital; continues with home visits to provide brief intervention, assess longer-term needs, and connect a family with community resources to provide ongoing support; and concludes with a follow-up session 1 month later. Letters from the program also connect families to maternal and infant health care providers for ongoing support.
Durham Connects was implemented jointly by the Durham County Health Department and Duke University. It is a highly structured program (manual available by request from K. A. D.) that consists of 4 to 7 scripted intervention contacts, beginning with consent during a birthing hospital visit when a staff member communicates the importance of community support for parenting, 1 to 3 nurse home visits when the infant is aged between 3 and 12 weeks, 1 to 2 nurse contacts with a community service provider, and a staff member telephone or home follow-up 1 month later.
During the first home visit, the nurse’s tasks are to engage the mother and father (when possible), use a high-inference approach to assessing family risks on 12 factors related to child well-being, provide brief educational interventions organized as 20 teaching moments, offer extended education in areas specific to assessed parent needs (e.g., lactation, crying, baby blues), and facilitate connections to community resources relevant to assessed family needs.
To evaluate a family’s unique risks, the nurse assessed and scored health and psychosocial risk in each of 12 empirically derived areas in 4 domains known to predict child well-being: (1) parenting and child care (child care plans, parent–infant relationship, and management of infant crying); (2) family violence and safety (material supports, family violence, and past maltreatment); (3) parent mental health and well-being (depression and anxiety, substance abuse, and emotional support); and (4) health care (parent health, infant health, and health care plan). The nurse scored and responded to risk separately in each area on a 4-point scale. A family with a score of 1 (low risk) in a particular area received no subsequent intervention. A family with a score of 2 (moderate risk) received short-term nurse-delivered intervention on that particular topic over 1 to 3 sessions. A family with a score of 3 (high risk) received a connection or referral to community resources tailored to address the particular risk. The nurse and intervention support staff members not only made a referral, they also followed up to make sure that each connection endured, requiring a possible additional 1 to 2 contacts. A family with a score of 4 (imminent risk) received emergency intervention. A final session 4 weeks after the nurse had completed the case ascertained whether the community connection continued, whether further problem solving was needed, and whether the family was satisfied.
Two community advisory boards monitored rates of family needs and experiences with services over time to improve community service capacity. Agencies signed a memorandum of agreement to follow a preventive system of care,13 requiring collaboration across agencies, family-centered service delivery, and building a continuum of care.
We estimated the per-family cost of the intervention from budget allocations that included salaries and benefits of intervention staff members and supervisors, local travel reimbursements, and office and supply costs. It does not include in-kind and reallocated time from community agencies. Intervention cost was estimated at $700 per birth.
Intervention Quality Control
The intervention program was manualized and delivered consistently across families. Adherence to protocol as specified in the manual was assessed by having an independent expert accompany the nurse or listen to an audiotape of a home visit for 116 randomly selected families (7% of the total of 1594 families). From a list of necessary program elements, the expert checked adherence (or not) to each model element. The expert also scored risk for each of the 12 domains.
Dependent Variables at Age 6 Months
We reviewed hospital records and conducted interviews with the participating representative sample of 531 mothers. Instruments can be found at http://sites.duke.edu/psid/interviews. Interviewers were not told whether a family participated in Durham Connects, and families were not told of any relation between the interview and the Durham Connects program. Interviews took place in mothers’ homes at prearranged times for compensation of $50.
Health care domain.
We obtained administrative records from the 2 hospitals at which all resident births occurred after mother consent. For each infant, we tallied the number of emergency department (ED) visits since initial hospital release and the number of overnights in the hospital for non–birth-related medical care. ED visits were counted as the number of unique visits to the ED; hospital overnights were tallied as the number of nights the infant spent in the hospital. The sum of these 2 figures constituted the primary outcome variable, the total number of emergency medical care episodes.
Mothers independently reported their infant’s number of emergency medical visits to any hospital, urgent care center, or physician in the past 3 months. Mothers also reported the infant’s number of overnights in any hospital for non–birth-related medical care in the past 3 months. We coded these variables in the same manner as the corresponding variables on the basis of administrative records. Finally, we calculated the total number of mother-reported emergency medical care episodes by summing these 2 variables. Mother reports included care at any facility, so these scores might validly differ from the scores obtained from the 2 major hospitals.
Mothers also reported the date of the most recent well-baby primary care visit. We recoded responses as 0 (more than 1 month ago) or 1 (within the past month).
Community connections.
Following prompting regarding major resources, mothers were asked to name all of the community resources that they had used in the past 3 months, including professional, paraprofessional, and informal resources, which was the primary measure of the program’s proximal goal to improve community connections.
Parenting and child care domain.
Mothers completed standard reliable and valid questionnaires assessing their parenting behaviors and knowledge, including the Mother-Child Neglect Scale,14 the Parent-Child Conflict Tactics Scales,15 the Knowledge of Infant Development Inventory (D. L. MacPhee, unpublished manuscript and manual, 1981), the Parenting Sense of Competence Scale,16 and the Survey of New Parents.17 We scored the following 5 variables: positive parenting behaviors (7 items, e.g., “comforted infant”), negative parenting behaviors (10 items, e.g., “shouted at infant”), knowledge of infant development (10 items, e.g., “6-month-olds know what ‘No’ means”), parenting sense of competence (17 items, e.g., “being a parent makes me tense and anxious”), and father–infant relationship quality (whether the biological father was involved with the infant; 10 items, e.g., “hugs or shows physical affection toward child”).
Trained in-home interviewers, blinded to intervention status, completed the 18-item Responsivity and Acceptance subscales of the Infant–Toddler Home Observation for Measurement of the Environment,18 providing an independent rating of mother parenting quality.
Mothers completed a brief questionnaire19 on nonparental child care use (no vs yes) and, if the infant had been placed in regulated child care, the child care center’s star rating (based on North Carolina’s 5-star rating system).
Family and home safety domain.
Blinded interviewers completed the Duke Endowment Child Abuse Prevention Initiative Neighborhood Survey,20 a 5-item rating of overall home environment quality (e.g., “The home is safe, clean, and free from hazards”). Mothers currently in a relationship completed the 20-item Conflict Tactics Scale,21 leading to a partner relationship conflict score.
Parent well-being domain.
Mothers completed the 10-item Edinburgh Postnatal Depression Scale,22 indicating possible clinical depression (cutpoint = 10); the 7-item brief Generalized Anxiety Disorder–7 questionnaire,23 indicating possible clinical anxiety (cutpoint = 5); and the 8-item CAGE and CAGE-AID questionnaires,24 indicating possible substance use problems (cutpoint = 1) in the past 3 months.
Statistical Analysis
We conducted analyses using SAS version 9.2 software (SAS Institute, Cary, NC) with a 2-tailed intent-to-treat design that included all randomly assigned interviewed families without regard to intervention adherence. Probability levels of less than .05 were called significant. We used ordinary least squares regression models and multinomial logistic regression models to estimate the impact of random assignment to Durham Connects on continuous and categorical outcomes, respectively. We used Poisson regression models for count variables with skewed distributions.25 Models included covariates of family Medicaid status (0 = no, 1 = yes) at birth and at age 6 months, mother race/ethnicity (0 = nonminority, 1 = minority), single-parent household status (0 = no, 1 = yes), and any birth complications (0 = no, 1 = yes), including maternal health conditions affecting the fetus or newborn, birthing events affecting the fetus or newborn, infant injuries resulting from birth trauma, and fetal or infant distress. We calculated intervention effect sizes as
 |
RESULTS
We compared the 664 computer-selected families with the full population on 13 variables available from hospital birth records (Table 1 for group means). These families significantly (P < .05) differed from the population on only 1 variable, infant gender (selected families were more likely to have male infants). Next, we compared the 531 participating families with the full population on the same 13 variables and found only 1 significant difference (interviewed families were more likely to be insured by Medicaid or to be uninsured). Interview participation rates did not differ between intervention (81%) and control (79%) families. Finally, we tested whether intervention and control groups differed on the 13 variables and found only 1 significant difference (infants in the control condition were more likely to have had birth complications). We included gender, Medicaid status, and birth complications as covariates in subsequent analyses.
TABLE 1—
Preintervention Sample Characteristics for Population and Selected Evaluation Subsample Groups: Durham County, NC; July 1, 2009–December 31, 2010
| RCT Population vs Selected and Interviewed Evaluation Subsamples |
Interviewed Intervention vs Control Evaluation Subsamples |
||||
| Variable | RCT Population (n = 4777), Mean | Selected Evaluation Subsample (n = 664), Mean (P) | Interviewed Evaluation Subsamplea (n = 531), Mean (P) | Participating Intervention Subsampleb (n = 260), Mean | Participating Control Subsamplec (n = 271), Mean (P) |
| Low birth weight, % | 10.0 | 9.1 (.5) | 8.9 (.45) | 7.8 | 10.0 (.39) |
| Gestation < 37 wk, % | 8.2 | 6.7 (.17) | 6.3 (.12) | 4.7 | 7.8 (.15) |
| Any birth complications, % | 7.4 | 5.8 (.13) | 6.1 (.26) | 3.9 | 8.1 (.04) |
| Cesarean delivery, % | 30.6 | 31.6 (.59) | 31.8 (.56) | 32.3 | 31.4 (.82) |
| Multiple births, % | 2.1 | 2.1 (.92) | 2.6 (.37) | 3.5 | 1.9 (.25) |
| Adolescent mother, % | 9.4 | 9.2 (.86) | 9.4 (.99) | 9.2 | 9.6 (.89) |
| Medicaid/no insurance, % | 60.8 | 63.1 (.26) | 65.5 (.04) | 63.3 | 67.5 (.31) |
| Maternal age, y | 28.5 | 28.5 (.84) | 28.3 (.58) | 28.2 | 28.4 (.66) |
| Maternal race/ethnicity, % | |||||
| White, non-Hispanic | 29.7 | 29.2 (.8) | 26.6 (.13) | 28.5 | 24.7 (.33) |
| Black, non-Hispanic | 36.7 | 38.0 (.54) | 39.4 (.23) | 36.5 | 42.1 (.19) |
| Hispanic | 22.6 | 23.2 (.71) | 24.7 (.27) | 25.0 | 24.4 (.86) |
| Other | 11.1 | 9.6 (.27) | 9.4 (.25) | 10.0 | 9.9 (.65) |
| Infant female, % | 49.8 | 54.7 (.01) | 53.5 (.11) | 50.8 | 56.1 (.22) |
Note. RCT = randomized controlled trial. The selected evaluation and interviewed evaluation subsamples are compared with the RCT population and the participating control subsample is compared with the participating intervention subsample.
80.0% of the selected subsample participated.
81.3% of the selected subsample participated.
78.8% of the selected subsample participated.
Implementation
Penetration (program completion rate).
Of the 2327 even-birth-date families, 1863 (80.0%) consented and participated in the first intervention session. Of those 1863 families, 1596 (85.8%) completed the entire program (net completion = 69%). Of the 1596 participating families, 40% (n = 638) were White, 37% (n = 591) were Black, and 23% (n = 367) were other or multiracial; 26% (n = 415) reported Hispanic ethnicity. Sixty-two percent (n = 990) received Medicaid or had no health insurance; 44% (n = 709) were married.
Fidelity (adherence to protocol).
Observer-rated adherence to the manual was 84% (5267 of 6304 program elements checked), which is judged to be high. Interrater agreement on scoring of risk yielded a mean κ coefficient across nurses of 0.69 and across the 12 risk factors of 0.68 (coefficients > 0.60 are considered substantial26).
Risk assessment, intervention, and family consumer satisfaction.
Of 1596 families, 50 (3.1%) stopped assessment because of family choice. Of the 1546 assessed families, 15 (1%) scored 4 at least once, indicating the need for immediate emergency intervention; 681 (44%) scored 3 (but not 4) at least once, indicating serious risk best served by referral to a community agency provider; 757 (49%) received a 2 (but not a 3 or 4) at least once, indicating mild to moderate risk that was addressed by brief nurse intervention during home visits; and 93 (6%) received the lowest need score (1) in all 12 domains.
Nurses implemented a mean of 13.8 teachings (of 20 possible) with each family. Nonimplementation occurred because of nurse judgment that a teaching was unnecessary, time constraints, or neglect. During follow-up contacts, families reported that a successful connection had been established with the community service provider for 60% (1009/1671) of referrals, and community services had already been received for 39% (651/1671) of the total. Families reported the following aspects to be helpful (vs not helpful): materials provided by the nurse (diapers, thermometer, books, and so on; 99%; 820/832); discussion with the nurse about the mother’s needs (98%; 812/830); and nurse teachings (95%; 792/830). Almost every mother indicated that she would recommend the visit to another new mother (99%; 818/828).
Impact Evaluation
Infant health care.
Group means for all variables are found in Table 2, and regression analyses are summarized in Table 3. In multivariate Poisson regression models using administrative records, random assignment to Durham Connects (Durham Connects families) was significantly associated with a mean of 0.91 fewer overall emergency medical care episodes than the control group (95% confidence interval [CI] = −1.13, −0.69; P < .001; effect size = 0.26). Inspection of the group distributions indicated that Durham Connects and control families did not differ in the proportions who had no emergency care episodes (0.742 vs 0.723, respectively), but groups did differ in the proportions having 2 or more episodes (0.096 vs 0.151, respectively) and 3 or more episodes (0.031 vs 0.085, respectively).
TABLE 2—
Descriptive Statistics for Evaluation Outcomes at Infant Age 6 Months (n = 531): Durham County, NC, July 1, 2009–December 31, 2010
| Variable | Intervention (n = 260), Mean ±SD or % | Control (n = 271), Mean ±SD or % |
| Infant health—hospital records | ||
| No. of total emergency medical care episodesa | 0.43 ±0.99 | 1.05 ±3.86 |
| No. of emergency department visits | 0.32 ±0.66 | 0.39 ±0.82 |
| No. of overnights in hospital (n = 514) | 0.10 ±0.63 | 0.66 ±3.81 |
| Infant health—parent report | ||
| No. of total emergency medical care episodesb | 0.89 ±1.24 | 1.37 ±3.43 |
| No. of emergency medical visitsc | 0.82 ±1.12 | 0.98 ±1.57 |
| No. of overnights in hospital | 0.08 ±0.48 | 0.40 ±2.77 |
| Community support | ||
| No. of community connections | 5.02 ±2.67 | 4.31 ±2.36 |
| Parenting and child care | ||
| Mother positive parenting behaviors | 4.12 ±0.44 | 4.01 ±0.43 |
| Mother negative parenting behaviors | 0.32 ±0.38 | 0.33 ±0.41 |
| Mother knowledge of infant development | 0.75 ±0.19 | 0.77 ±0.17 |
| Mother sense of parenting competence | 4.62 ±0.51 | 4.63 ±0.53 |
| Observer-rated mother parenting quality (n = 419) | 15.14 ±1.50 | 14.76 ±1.81 |
| Father–infant relationship quality (n = 524) | 2.09 ±0.74 | 1.92 ±0.87 |
| Proportion using nonparental child care | 45.77 | 53.14 |
| Out-of-home child care quality rating (n = 83) | 4.61 ±0.55 | 3.98 ±0.92 |
| Family safety | ||
| Observer-rated home environment (n = 499) | 4.83 ±1.48 | 4.50 ±1.52 |
| Partner relationship conflictd (n = 426) | −4.65 ±1.64 | −4.65 ±1.69 |
| Parent mental health | ||
| Mother possible clinical depression disorder | 7.69 | 11.81 |
| Mother possible anxiety disorder | 21.15 | 29.52 |
| Mother possible substance use problems (n = 530) | 4.63 | 6.27 |
| Most recent well-baby visit within past mo | 69.62 | 67.16 |
No. of total emergency medical care episodes (hospital records) = (no. of emergency department visits + no. of hospital ovesrnights).
No. of total emergency medical care episodes (parent report) = (no. of emergency medical visits + no. of hospital overnights).
No. of emergency medical visits = (no. of emergency pediatric visits + no. of emergency department visits).
Marital relationship = (total relationship conflict − total relationship negotiation).
TABLE 3—
Regression Models Testing Impact of Random Assignment to Durham Connects on Infant Health, Community Connections, and Family Behavior and Well-Being (n = 531): Durham County, NC, July 1, 2009–December 31, 2010
| Model |
|||
| Variable | B (95% CI) | OR (95% CI) | P |
| Infant health—hospital records | |||
| No, of total emergency medical care episodesab | −0.91 (−1.13, −0.69) | < .001 | |
| No. of emergency department visitsa | −0.14 (−0.43, 0.15) | .36 | |
| No. of overnights in hospitala (n = 514) | −1.91 (−2.31, −1.50) | < .001 | |
| Infant health—parent report | |||
| No. of total emergency medical care episodesac | −0.40 (−0.57, −0.24) | < .001 | |
| No. of emergency medical visitsad | −0.17 (−0.35, 0.02) | .07 | |
| No. of overnights in hospitala | −1.60 (−2.09, −1.11) | < .001 | |
| Total no. of community connectionse | 0.86 (0.51, 1.21) | < .001 | |
| Parenting and child care | |||
| Mother positive parenting behaviorse | 0.10 (0.03, 0.17) | < .01 | |
| Mother negative parenting behaviorse | −0.02 (−0.09, 0.05) | .59 | |
| Mother knowledge of infant developmente | −0.02 (−0.050, 0.004) | .1 | |
| Mother sense of parenting competencee | −0.01 (−0.10, 0.08) | .83 | |
| Observer-rated mother parenting qualitye (n = 419) | 0.25 (−0.03, 0.54) | .08 | |
| Father–infant relationship qualitye (n = 524) | 0.11 (−0.01, 0.24) | .08 | |
| Proportion using nonparental child caref | 0.75 (0.53, 1.07) | .11 | |
| Out-of-home child care quality ratinge (n = 83) | 0.66 (0.30, 1.02) | < .001 | |
| Family safety | |||
| Observer-rated home environmente (n = 499) | 0.21 (0.01, 0.40) | < .05 | |
| Partner relationship conflicteg (n = 426) | 0.01 (−0.30, 0.32) | .95 | |
| Parent mental health | |||
| Mother possible clinical depression disorderf | 0.69 (0.38, 1.27) | .23 | |
| Mother possible anxiety disorderf | 0.65 (0.43, 0.97) | < .05 | |
| Mother possible substance use problemsf (n = 530) | 0.80 (0.36, 1.77) | .58 | |
| Most recent well-baby visit within past mof | 1.12 (0.78, 1.63) | .54 | |
Note. CI = confidence interval; OR = odds ratio. All models include Medicaid–no insurance status at birth, any birth complications, infant gender, Medicaid status at infant age 6 mo, minority race/ethnicity status, and single-parent status at infant age 6 mo as covariates.
Model estimated using Poisson regression.
No. of total emergency medical care episodes (hospital records) = (no. of emergency department visits + no. of hospital overnights).
No. of total emergency medical care episodes (parent report) = (no. of emergency medical visits + no. of hospital overnights).
No. of emergency medical visits = (no. of emergency pediatric visits + no. of emergency department visits).
Model estimated using ordinary least squares regression.
Model estimated using logistic regression.
Marital relationship conflict = (total relationship conflict − total relationship negotiation).
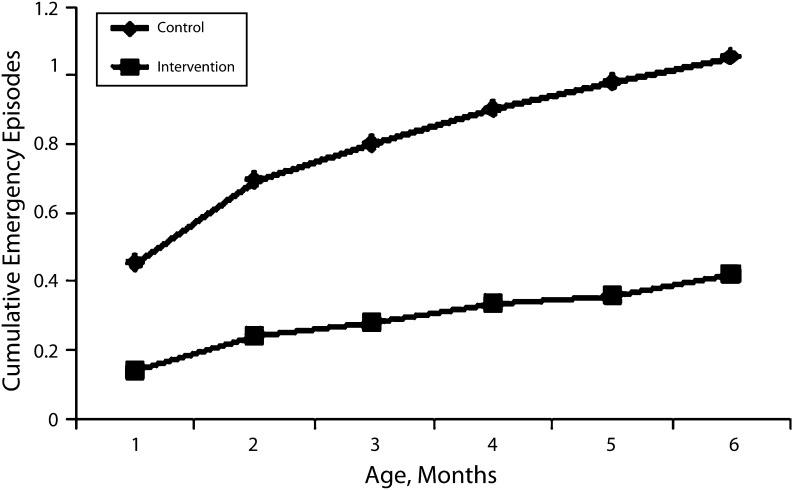
Analysis of the timing of emergency care episodes as depicted in Figure 1 indicated that Durham Connects and control families differed beginning in the first month after intervention, and the difference kept increasing with each advancing month of age, indicating both an immediate and a deferred impact of intervention. Administrative records also indicated that Durham Connects families had a mean of 0.14 fewer ED visits (95% CI = −0.43, 0.15) and a mean of 1.91 fewer overnights in the hospital (95% CI = −2.31, −1.50; P < .001; effect size = 0.25).
FIGURE 1—
Mean cumulative number of emergency care episodes across the first 6 months of life, by intervention group: Durham County, NC, July 1, 2009–December 31, 2010.
In multivariate Poisson regression models, random assignment to Durham Connects was also associated with a mean of 0.40 fewer mother-reported overall emergency medical care episodes (95% CI = −0.57, −0.24; P < .001; effect size = 0.21). Inspection of group distributions indicated that Durham Connects and control families did not differ in the proportions reporting no emergency care episodes (0.499 vs 0.513, respectively), but they did differ in the proportions reporting more than 1 episode (0.212 vs 0.251, respectively) and in the proportions reporting more than 2 episodes (0.088 vs 0.129, respectively). Durham Connects families reported a mean of 0.17 fewer emergency medical outpatient visits (95% CI = −0.35, 0.02; P = .07) and a mean of 1.60 fewer overnights in the hospital (95% CI = −2.09, −1.11; P < .001; effect size = 0.20). Families did not differ in the time since the last well-baby pediatric visit.
Community connections.
Multivariate ordinary least squares regression models revealed that Durham Connects families accessed 0.86 more community resources than did control families (95% CI = 0.51, 1.21; P < .001; effect size = 0.28).
Parenting and child care.
Durham Connects mothers reported more positive parenting behaviors than did control mothers (B = 0.10; 95% CI = 0.03, 0.17; P < .01; effect size = 0.25); we found no significant differences in negative parenting behaviors, knowledge of infant development, sense of parenting competence, father–infant relationship quality, or blinded in-home observer ratings of parenting quality.
We found no group difference for the likelihood of placing an infant in out-of-home child care but, contingent on receipt of out-of-home child care, the quality of that care was higher for Durham Connects families than for the control families (B = 0.66; 95% CI = 0.30, 1.02; P < .001; effect size = 0.86).
Family safety.
Blinded in-home observers rated the home environment quality as significantly higher for Durham Connects families than for control families (B = 0.21; 95% CI = 0.01, 0.40; P < .05; effect size = 0.22). No difference was reported for the partner relationship conflict score.
Maternal mental health.
Multinomial logistic regression models revealed that Durham Connects mothers were less likely to report possible clinical anxiety (odds ratio = 0.65; 95% CI = 0.43, 0.97; P < .05; 29.5% for control and 21.2% for DC mothers). They were not less likely than control mothers to report possible depression (11.8% for control mothers and 7.7% for Durham Connects mothers) or substance use problems (6.3% for control mothers and 4.6% for Durham Connects mothers).
Benefit–cost analysis.
Using findings on emergency medical care, we estimated costs using published rates that indicate a local average of $423 per emergency outpatient visit and $3722 per hospital night.27 Using the group means of hospital records reported in Table 2 and these dollar costs, one can apply a standard formula for the ratio of the costs of an intervention to the benefits that accrue28 as follows:
 |
in which BCRDC is the benefit–cost ratio that accrues from random assignment to the Durham Connects program, OCOBD is the output cost for each odd-birth-date infant measured as the average per-infant cost for emergency medical care at age 6 months, OCEBD is the output cost for each even birth-date infant measured as the average per-infant cost for emergency medical care at age 6 months, ICEBD is the average per-infant cost of the Durham Connects program ($700), and ICOBD is the average marginal cost of programs for control infants ($0). We obtained average costs of emergency medical care of $2621 for control infants ($165 in outpatient and $2456 in overnight costs) and $507 for Durham Connects infants ($135 in outpatient and $372 in overnight costs) and a benefit–cost ratio of $3.02, meaning that every $1 spent on the Durham Connects program saved $3.02 by infant age 6 months in costs for hospital emergency care. For a community the size of Durham with an average of 3187 resident births per year and a Durham Connects intervention cost of $700 per birth, a community annual investment of $2 230 900 in the Durham Connects program would yield a community-wide emergency health care cost savings of $6 737 318 in the first 6 months of life.
DISCUSSION
The Durham Connects program offers a novel, feasible, and effective public health policy for families of newborn infants. It combines a top-down commitment by community agencies to align services according to a preventive system of care model with an individually administered, brief nurse home-visiting program that aims to reach every family. This approach solves the paradox of being universal but also tailored to individual family needs by triaging families into community services on the basis of brief individualized assessments. Findings indicate that when this program is implemented at scale, it is successful in penetrating most of the community with high fidelity and high consumer satisfaction at an affordable cost ($700 per birth).
To our knowledge, we report the first known randomized controlled trial of universal infant home visiting implemented with an entire population of families. Impact findings based on hospital records (independently validated by parent reports) indicate that random assignment to the Durham Connects program at birth has a dramatic positive impact on reducing infant emergency health care outcomes. The impact begins immediately after the intervention and more than doubles in size by age 6 months.
Other findings support positive impact in other domains. The program was effective in its proximal goal of improving a family’s connections to community resources. The program also improved family well-being, specifically positive parenting behavior, the quality of father involvement, the quality of out-of-home child care, family safety, and maternal mental health. The program’s logic model had asserted that improving connections to community resources would improve family well-being, which in turn would lead to less emergency health care utilization. Future articles will examine whether this mediation pattern held.
Effect sizes for emergency care are in the modest range, but they are similar to those of longer and more expensive targeted home-visiting programs2–4 that have proven cost beneficial, and they are within the range of effect sizes on parenting behavior for programs involving at least 1 postnatal visit, as reported in a meta-analysis.5 The current cost–benefit analysis suggests that the birthing hospital could recoup program costs 3 times over by age 6 months. Given new Affordable Care Act–mandated penalties to hospitals when patients are rehospitalized prematurely, the cost–benefit ratio for the hospital should improve in future implementations.
Findings are limited by the implementation of Durham Connects in just 1 community. Findings are also limited to the infant’s first 6 months of life. Future studies will follow up on these findings by extending cost analysis further into the infants’ lives and more broadly to other domains to see whether even larger savings accrue across development or costs are simply deferred or shifted. Additional population outcomes will be assessed, including reports to Child Protective Services.
Future analyses will address the moderation of findings across subgroups within the population and the mediation of distal impact on health care services outcomes through proximal impact on community connections and family well-being.
We conclude that a brief, universal, postnatal, nurse home-visiting program can be delivered to most of the population with high fidelity, increase a family’s community connections, and have a positive impact on infant health and well-being. Finally, we conclude that a public policy of universal implementation could be cost beneficial for a community.
Acknowledgments
We thank the Duke Endowment and the Pew Center on the States for financial support. Those organizations approved the design of the study but had no responsibility for the conduct, collection, management, analysis, and interpretation of the data, or the preparation, review, and approval of the article. K. A. D. acknowledges grants from the National Institute on Drug Abuse (K05DA15226 and P30DA023026).
This trial has been registered as the “Durham Connects Evaluation” with ClinicalTrials.gov (NCT01406184, http://www.clinicaltrials.gov).
Note. The views expressed are those of the authors and do not necessarily reflect the views of the Duke Endowment, the Pew Center on the States, or The Pew Charitable Trusts. The authors acknowledge that they have no conflict of interest in this article or the study reported here.
Human Participant Protection
The Duke University institutional review board approved this study before the beginning of data collection.
References
- 1. Patient Protection and Affordable Care Act, Pub. L. No. 111–148, § 3502, 124 Stat. 119, 124 (2010)
- 2.Olds DL, Henderson CR, Chamberlin R, Tatelbaum RT. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics. 1986;78(1):65–78. [PubMed] [Google Scholar]
- 3.Fergusson DM, Grant H, Horwood LJ, Ridder EM. Randomized trial of the Early Start program of home visitation. Pediatrics. 2005;116(6):e803–e809. doi: 10.1542/peds.2005-0948. [DOI] [PubMed] [Google Scholar]
- 4.Armstrong KL, Fraser JA, Dadds MR, Morris J. A randomized, controlled trial of nurse home visiting to vulnerable families with newborns. J Paediatr Child Health. 1999;35(3):237–244. doi: 10.1046/j.1440-1754.1999.00348.x. [DOI] [PubMed] [Google Scholar]
- 5.Kendrick D, Elkan R, Hewitt M et al. Does home visiting improve parenting and the quality of the home environment? A systematic review and meta analysis. Arch Dis Child. 2000;82(6):443–451. doi: 10.1136/adc.82.6.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mrazek PJ, Haggerty RJ. Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research. Washington, DC: Committee on Prevention of Mental Disorders, Institute of Medicine; 1994. [PubMed] [Google Scholar]
- 7.Welsh BC, Sullivan CJ, Olds DL. When early crime prevention goes to scale: a new look at the evidence. Prev Sci. 2010;11(2):115–125. doi: 10.1007/s11121-009-0159-4. [DOI] [PubMed] [Google Scholar]
- 8.Daro D, McCurdy K, Falconnier L, Stojanovic D. Sustaining new parents in home visitation services: key participant and program factors. Child Abuse Negl. 2003;27(10):1101–1125. doi: 10.1016/j.chiabu.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 9.Olds DL, Hill PL, O’Brien R, Moritz P. Taking preventive intervention to scale: the Nurse-Family Partnership. Cognitive Behav Pract. 2003;10(4):278–290. [Google Scholar]
- 10.Olds DL, Eckenrode J, Henderson C . Preventing child abuse and neglect with home visiting by nurses. In: Dodge KA, Coleman DL, editors. Preventing Child Maltreatment: Community Approaches. New York, NY: Guilford Press; 2009. pp. 29–54. [Google Scholar]
- 11.Cohen J. Statistical Power for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 12.Faul F, Erdfelder E, Buchner A, Lang A.-G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 13.Dodge KA, Berlin LJ, Epstein M et al. The Durham Family Initiative: a preventive system of care. Child Welfare. 2004;83(2):109–128. [PMC free article] [PubMed] [Google Scholar]
- 14.Lounds JJ, Borkowski JG, Whitman TL. Reliability and validity of the mother-child neglect scale. Child Maltreat. 2004;9(4):371–381. doi: 10.1177/1077559504269536. [DOI] [PubMed] [Google Scholar]
- 15.Straus MA, Hamby SL, Finkelhor D, Runyan D. The Parent-Child Conflict Tactics Scales (PCCTS), Form A. Durban, NH: Family Research Laboratory, University of New Hampshire; 1995. [Google Scholar]
- 16.Ohan J, Leung D, Johnston C. The Parenting Sense of Competence Scale: evidence of a stable factor structure and validity. Can J Behav Sci. 2000;32(4):251–261. [Google Scholar]
- 17.Center for Research on Child Wellbeing. The Fragile Families and Child Wellbeing Study (Survey of New Parents): Mothers’ Baseline Survey public use version. 2008 Available at: http://www.fragilefamilies.princeton.edu/documentation.asp. Accessed May 23, 2008. [Google Scholar]
- 18.Caldwell BM, Bradley RH. Home Observation for Measurement of the Environment. Little Rock: University of Arkansas at Little Rock; 1984. [Google Scholar]
- 19.Bates JE, Marvinney D, Kelly T, Dodge KA, Bennett DS, Pettit GS. Childcare history and kindergarten adjustment. Developmental Psychol. 1994;30(5):690–700. [Google Scholar]
- 20.Daro D, Dworsky A. Duke Endowment Child Abuse Prevention Initiative Neighborhood Survey: 2004 Baseline Report. Chicago, IL: Chapin Hall, University of Chicago; 2005. [Google Scholar]
- 21.Straus MA, Douglas EM. A short form of the Revised Conflict Tactics Scale, and typologies for severity and mutuality. Violence Vict. 2004;19(5):507–520. doi: 10.1891/vivi.19.5.507.63686. [DOI] [PubMed] [Google Scholar]
- 22.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 23.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 24.Brown RL, Rounds L. Conjoint screening questionnaires for alcohol and drug abuse: criterion validity in a primary care practice. Wis Med J. 1995;94(3):135–140. [PubMed] [Google Scholar]
- 25.Coxe S, West SG, Aiken LS. The analysis of count data: a gentle introduction to Poisson regression and its alternatives. J Pers Assess. 2009;91(2):121–136. doi: 10.1080/00223890802634175. [DOI] [PubMed] [Google Scholar]
- 26.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 27.Paul IM, Phillips TA, Widome MD, Hollenbeak CS. Cost-effectiveness of postnatal home nursing visits for prevention of hospital care for jaundice and dehydration. Pediatrics. 2004;114(4):1015–1022. doi: 10.1542/peds.2003-0766-L. [DOI] [PubMed] [Google Scholar]
- 28.Drummond MF, O’Brien B, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. New York, NY: Oxford University Press; 2001. [Google Scholar]