Abstract
Objectives. We identified individual and contextual factors associated with referral and enrollment in home visiting among at-risk, first-time mothers.
Methods. We retrospectively studied referral and enrollment in a regional home visiting program from 2007 to 2009 in Hamilton County, Ohio. Using linked vital statistics and census tract data, we obtained individual and community measures on first-time mothers meeting eligibility criteria for home visiting (low income, unmarried, or age < 18 years). Generalized linear modeling was performed to determine factors associated with relative risk (RR) of (1) referral to home visiting among eligible mothers and (2) enrollment after referral.
Results. Of 8187 first-time mothers eligible for home visiting, 2775 were referred and 1543 were enrolled. Among referred women, high school completion (RR = 1.10) and any college (RR = 1.17) compared with no high school completion were associated with increased enrollment, and enrollment was less likely for those living in communities with higher socioeconomic deprivation (RR = 0.71; P < .05).
Conclusions. Barriers to enrollment in home visiting persisted at multiple ecological levels. Ongoing evaluation of enrollment in at-risk populations is critical as home visiting programs are implemented and expanded.
The magnitude of problems faced by at-risk women and children in the United States is sobering. As of 2010, nearly one quarter of households with children are headed by single mothers; for children of these families, the poverty rate exceeds 44%.1,2 Low maternal socioeconomic status heightens risk for many adverse outcomes, including preterm birth, developmental delay, and child abuse.3–6 Home visiting, defined as a voluntary service delivered in a family’s home, is one strategy to improve outcomes through care coordination, education, and social support for at-risk child-bearing women and their children.7–9 Several national models of home visiting, including Nurse Family Partnership (NFP) and Healthy Families America (HFA), have developed specific program curricula and protocols; qualifications of home visitors range from nurses to social workers to paraprofessionals.10 Recently, a dedicated investment of federal funding for home visiting was made available through the Patient Protection and Affordable Care Act (PPACA), with the intention of promoting and expanding this intervention.11
However, not all women eligible for services enroll in home visiting. Previous research evaluating acceptability of home visiting to at-risk families has demonstrated the importance of maternal factors, including trust, functional status, and parenting confidence.12–17 Additional studies have described the association of age, race, education, and mental health history on retention or engagement among program participants.18–20 Although many such studies have used qualitative methods to evaluate detailed individual-level measures, further research is needed to understand their affects on uptake of home visiting at a population level. A population-based approach to home visiting research adds value to the existing literature by defining and evaluating the denominator of women at-risk and who are eligible for services, thereby informing program planning and outcomes evaluation.
Compared with individual factors, the role of contextual or community factors in influencing engagement in home visiting is less well understood. The importance of such factors is reflected in profound geographic disparities in maternal–child outcomes, including preterm birth.21,22 A population-based approach incorporating both individual and contextual factors may inform a more comprehensive theory of enrollment in home visiting, offering additional insights into potential interventions at different levels within an ecological framework. At a proximal level, individual interaction with surrounding family, neighbors, and peers may influence participation and engagement, whereas at an organizational level, availability and access to services may also be important.23 Finally, at a community level, factors such as poverty and crime may affect program participation through deterioration of trust, community relationships, and resources.24
For our study, we utilized an ecological framework to evaluate individual and contextual factors associated with referral to and enrollment in home visiting among a regional population of eligible, at-risk, first-time mothers. Greater insight into factors associated with enrollment in this intensive prevention program might inform targeted efforts to reach and engage the women most likely to benefit from home visiting and might be critical to interpreting the impact of home visiting on maternal–child health outcomes, including preterm birth.
METHODS
This retrospective, population-based cohort study evaluated factors associated with referral to and enrollment in home visiting among first-time mothers eligible to receive this service.
Patient Population and Setting
We evaluated countywide enrollment in Every Child Succeeds (ECS), a community-based regional home visiting program serving greater Cincinnati, Ohio. Hamilton County represents the most populated region of southwestern Ohio serviced by ECS, with 7 agencies covering home visiting services for effectively the entire county.
ECS agencies in Hamilton County use the HFA model of home visiting, emphasizing early prevention during pregnancy, education in child development and health, parenting skills, and maternal economic self-sufficiency. Home visitors seek to make weekly or biweekly home visits during pregnancy and through the first year after birth, lasting approximately 60 to 90 minutes in length. Women eligible for this program must be first-time mothers and have at least 1 of 4 risk characteristics: unmarried, low income (up to 300% of poverty level, receipt of Medicaid, or reported concerns about finances), younger than 18 years, or suboptimal prenatal care.
Referrals to home visiting may be self-initiated or may occur through prenatal clinics, birth hospitals, pediatric practices, and other community sources. For each referral, the central ECS office assigns an agency based on geographic catchment areas for each agency. Because of a high volume of referrals in Hamilton County, women may remain on a waiting list after referral for up to 8 weeks before enrollment, which involves an assessment visit with complete screening for program eligibility and the first home visit.
Data Sources
Vital statistics data were obtained from the Ohio Department of Health, representing births to mothers listing Hamilton County as their county of residence. For 2007 to 2009, 34 994 mothers who delivered a live birth were represented by the data set. Using fields available within vital records, we identified first-time mothers by the recorded measure of interpregnancy interval (“777” for all primiparous women). We then assigned eligibility status for home visiting (yes or no) among first-time mothers based on having at least 1 of 3 risk characteristics: single marital status, younger than 18 years, and low-income status. Because household income is not collected in vital records, enrollment in the Special Supplemental Nutritional Program for Women, Infants, Children (WIC) or Medicaid served as proxy measures for low-income status. Although inadequate prenatal care is 1 of the eligibility criteria for ECS participation, prenatal care use was not reliably documented in vital statistics, with missing data for approximately 50% of the study sample. However, of the 4 eligibility criteria defined by ECS, inadequate prenatal care was the least used, with only an estimated 5% of participants enrolled based on this risk factor absent of other criteria (ECS referral coordinators, personal communication, October 22, 2012).
We used vital statistics to construct additional maternal variables, including demographic characteristics, pregnancy-related health conditions, and infant outcomes. In addition to indicator variables for specific conditions, we also generated a composite variable for complications of pregnancy, including documentation of any of the following: premature rupture of membranes, chorioamnionitis, fetal intolerance of labor, meconium-stained amniotic fluid, use of forceps or vacuum instrumentation, or unplanned maternal surgery.
Using census tract data from vital statistics, we assigned 1 of 7 primary geographic catchment areas by agency to all women in the sample. We also linked census tracts to 5-year estimates from the 2009 American Community Survey (ACS) to provide aggregate sociodemographic measures for each woman’s area of residence. Area-level measures were selected on the basis of theoretical relevance for a range of maternal–child health outcomes and based on previous empirical research.25 Measures included housing characteristics and area-level percent usage of public benefits, such as food stamps and cash public assistance. We also calculated the Townsend Index of Socioeconomic Deprivation (TSI), a census-based index of area-level deprivation and disadvantage based on 4 variables: (1) unemployment as a percentage of those 16 years and older who are economically active, (2) percentage of households without access to a car, (3) percentage of all households renting, and (4) percentage of households with “crowded housing” (i.e., number of residents exceeding number of household rooms).26 The utility of the TSI was demonstrated in previous studies of health outcomes, and was calculated as a sum of the 4 standardized scores for these variables.27–29 The higher the TSI, the more deprived and disadvantaged an area was thought to be.
Finally, this data set was linked to program referral and enrollment data, available through a web-based data entry system, using common data fields and patient identifiers.
Statistical Analysis
Bivariate analyses using the χ2 or t test were used to identify factors associated with referral and enrollment to home visiting among eligible, first-time mothers. A composite risk score of 1, 2, or 3 was assigned based on number of eligibility criteria (single, < 18 years of age, and low income).
Individual-, agency-, and community-level factors deemed to be either empirically or statistically important (P < .25)30 were considered and tested in multiple regression analyses of the 2 outcomes: referral among eligible women and enrollment among those referred. Interaction terms between all factors (i.e., maternal age and race) were added and tested for statistical significance; after adjustment for multiple testing, none were retained. To derive parsimonious models, predictor variables affecting less than 10% of the sample (i.e., hypertension, Hispanic ethnicity) were omitted from the model; effects of omission were then tested using likelihood ratios. Multicollinearity was also assessed, with variance inflation factors for all retained variables less than 10. Because both referral and enrollment were not rare (occurring in more than 10% of women), we used generalized linear models with a log link and binomial distribution to produce an unbiased estimate of the adjusted relative risk (RR).31,32 All models adjusted for clustering using robust standard errors for cluster-correlated data by census tract, which provided a sufficient number of clusters to minimize over-rejection of the null hypothesis.33–35 Analyses were performed using STATA 11.0 (STATA Corp, College Station, TX).
Sensitivity and Spatial Analyses
Although the previously described multivariable model for the enrollment outcome adjusted for whether referral occurred prenatally or after birth, we assumed that certain predictors (i.e., pregnancy and infant complications) might affect the model differently depending on whether enrollment decisions were being made before or after birth. We therefore conducted separate multivariable analyses of enrollment stratified by timing of referral prenatally or after birth. Overall effect sizes for covariates included in the full, final model were similar, and these data are therefore not shown.
We used geospatial methods to further explore the extent to which differences in enrollment status were attributable to geographic location.21 Addresses for all eligible women referred to home visiting over the study timeframe were assigned a latitude and longitude using ArcGIS 10.1 (ESRI, Redlands, CA). Spatial filtering techniques were used within ArcGIS 10.1 through the Spatial Analyst Extension; specifically, the point density and divide tools were utilized.36,37 Point density output cell size was set to 250 feet with a radius of 3000 feet. Within each cell, a numerator of women referred to home visiting but not enrolled was divided by a denominator of all women referred to home visiting to create a rate. To minimize artificial variation because of small numbers, cells containing less than 10 referrals were concealed.
RESULTS
Of 34 994 mothers in Hamilton County in 2007 to 2009, we identified 8187 first-time mothers eligible for home visiting based on vital statistics data. Figure 1 depicts that 2734 women (33%) were referred to home visiting, and of these, 1543 women (56%) eventually enrolled (with 716 enrolling prenatally and 827 enrolling after birth of the infant). Residences for eligible women spanned 226 census tracts, providing a wide range of area-level measures, including percentage of residents below poverty (< 1%–79%), percentage using food stamps (0%–60%), percentage of residential buildings with more than 10 housing units (0%–98%), and TSI scores (−4.9 to 9.2).
FIGURE 1—
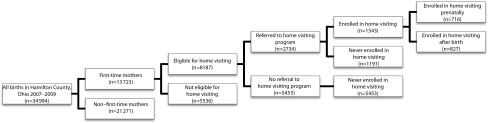
Determination of study population based on eligibility, referral, and enrollment status: Hamilton County, OH, 2007–2009.
Referral to Home Visiting
As shown in Table 1, several factors were significantly associated with referral status among those eligible for home visiting, including African American race (65.8% vs 42.2% among those not referred), and lack of a high school degree (50.7% vs 24.1% among those not referred). Compared with eligible women who were not referred, referred women lived in communities with a higher percentage use of food stamps (18.5% vs 12.2%) and higher mean TSI values.
TABLE 1—
Individual and Community Characteristics of Women Eligible for Home Visiting by Referral and Enrollment Status: Ohio Department of Health, Hamilton County, OH, 2007–2009
| Among Total Eligible Population (n = 8187) |
Among Women Referred to Home Visiting (n = 2734) |
|||||
| Characteristic | Not Referred (n = 5453) | Referred (n = 2734) | P | Not Enrolled (n = 1191) | Enrolled (n = 1543) | P |
| No. of risk criteria,a % | ||||||
| 1 | 33.4 | 10.3 | < .001 | 10.4 | 10.2 | .81 |
| 2 | 60.2 | 65.8 | < .001 | 65.1 | 66.3 | .48 |
| 3 | 6.4 | 24.0 | < .001 | 24.5 | 23.5 | .56 |
| Age, y, mean | 22.7 | 20.0 | < .001 | 19.8 | 20.1 | .12 |
| Race/ethnicity, % | ||||||
| White | 55.8 | 33.1 | < .001 | 33.0 | 33.1 | .95 |
| African American | 42.2 | 65.8 | < .001 | 66.2 | 65.6 | .78 |
| Native American/Alaska Native | 0.2 | 0.3 | .3 | 0.3 | 0.3 | .96 |
| Asian | 1.8 | 0.8 | < .001 | 0.5 | 1.0 | .15 |
| Hispanic | 5.2 | 7.8 | < .001 | 8.9 | 7.0 | .08 |
| Maternal education, % | ||||||
| No high school degree | 24.1 | 50.7 | < .001 | 54.5 | 47.8 | .002 |
| High school degree | 29.4 | 28.0 | .18 | 26.7 | 29.0 | .15 |
| Any college | 46.5 | 21.3 | < .001 | 18.8 | 23.2 | .002 |
| Previous loss, % | 9.6 | 9.3 | .61 | 8.6 | 9.8 | .23 |
| History of sexually transmitted infection, % | 9.9 | 14.4 | < .001 | 13.9 | 14.8 | .55 |
| Diabetes, % | 4.9 | 3.8 | .03 | 3.6 | 3.9 | .7 |
| Smoker, % | 30.3 | 26.0 | < .001 | 25.5 | 26.4 | .63 |
| Hypertension, % | 5.9 | 5.6 | .51 | 5.2 | 5.8 | .44 |
| Pregnancy complication,b % | 34.1 | 24.8 | < .001 | 27.7 | 34.3 | < .001 |
| Residents in area receiving food stamps, mean % | 12.2 | 18.5 | < .001 | 18.3 | 19.8 | .9 |
| Residential buildings in area with > 10 housing units, mean % | 17.0 | 19.1 | < .001 | 18.5 | 18.6 | .1 |
| Townsend Index score,c % | ||||||
| < −3 | 5.3 | 2.4 | < .001 | 2.1 | 2.6 | .39 |
| Between −3 and 0 | 40.9 | 26.1 | < .001 | 25.6 | 26.3 | .72 |
| Between > 0 and 3 | 33.9 | 33.1 | .84 | 32.7 | 33.3 | .78 |
| Between > 3 and 5 | 10.9 | 18.6 | < .001 | 18.4 | 18.6 | .91 |
| > 5 | 9.0 | 19.7 | < .001 | 21.2 | 19.2 | .13 |
Note. P values are based on univariable regression adjusted for clustering at the level of census tract.
Risk criteria: single marital status, age < 18 y, low income status based on Medicaid enrollment, or Special Supplemental Nutrition Program for Women, Infants, Children enrollment.
Includes any diagnosis of premature rupture of membranes, chorioamnionitis, fetal distress, meconium-stained amniotic fluid, or unplanned maternal surgery as indicated on the vital statistics record.
Calculated as a sum of the standardized scores for 4 census tract-level variables: (1) percentage unemployed, (2) percentage of households without access to a car, (3) percentage of all households renting, and (4) percentage of households with crowded housing. Higher Townsend Index scores reflect higher levels of deprivation and social disadvantage.
Table 2 depicts that after adjustment for all covariates and clustering by census tract, maternal characteristics remained significantly associated with an increased likelihood of referral, including African American race (RR = 1.42; 95% confidence interval [CI] = 1.32, 1.53). At a systems level, residence by individual home visiting agency catchment area was also significantly associated with differences in likelihood of referral. At the community level, higher TSI scores were significantly associated with increased likelihood of referral compared with communities scoring in the lowest range (< −3).
TABLE 2—
Multivariable Regression of Individual-, Agency-, and Community-Level Factors With Referral to and Enrollment in Home Visiting: Ohio Department of Health, Hamilton, OH, 2007–2009
| Variable | RR of Referral (95% CI) | RR of Enrollment (95% CI) |
| No. of risk criteriaa | ||
| 1 (Ref) | 1.00 | 1.00 |
| 2 | 1.87** (1.60, 2.18) | 1.05 (0.94, 1.17) |
| 3 | 2.43** (2.07, 2.85) | 1.13 (0.98, 1.30) |
| Race/ethnicity | ||
| White (Ref) | 1.00 | 1.00 |
| African American | 1.42** (1.32, 1.53) | 1.02 (0.93, 1.11) |
| Native American/Alaska Native | 1.92* (1.21, 3.04) | 1.04 (0.55, 1.94) |
| Asian | 0.99 (0.71, 1.38) | 1.27 (0.97, 1.67) |
| Maternal education | ||
| No high school degree (Ref) | 1.00 | 1.00 |
| High school degree | 0.80** (0.73, 0.88) | 1.10* (1.00, 1.21) |
| Any college | 0.55** (0.49, 0.61) | 1.17** (1.07, 1.28) |
| History of sexually transmitted infection | 1.05 (0.99, 1.11) | 1.03 (0.93, 1.14) |
| Smoker | 1.02 (0.94, 1.11) | 1.00 (0.92, 1.08) |
| Pregnancy complicationb | 0.89** (0.84, 0.94) | 1.14** (1.07, 1.22) |
| Prenatal referral | … | 1.61** (1.51, 1.71) |
| Home visiting agency catchment area | ||
| A (Ref) | 1.00 | 1.00 |
| B | 0.88 (0.76, 1.01) | 0.71** (0.59, 0.85) |
| C | 0.82* (0.74, 0.91) | 0.87* (0.78, 0.97) |
| D | 0.82* (0.74, 0.92) | 0.92 (0.81, 1.04) |
| E | 0.97 (0.84, 1.11) | 1.19* (1.04, 1.36) |
| F | 0.98 (0.89, 1.08) | 0.99 (0.88, 1.10) |
| G | 0.89* (0.82, 0.98) | 0.90* (0.81, 1.00) |
| Residents in area receiving food stamps,c % | 1.00* (1.00, 1.01) | 1.01** (1.00, 1.02) |
| Majority of residential buildings in area have > 10 housing units | 1.04 (0.93, 1.17) | 1.27** (1.15, 1.39) |
| Townsend Index scored | ||
| < −3 (Ref) | 1.00 | 1.00 |
| Between −3 and 0 | 1.21* (1.02, 1.43) | 1.02 (0.80, 1.30) |
| Between > 0 and 3 | 1.26* (1.05, 1.50) | 0.95 (0.75, 1.22) |
| Between > 3 and 5 | 1.39* (1.15, 1.68) | 0.85 (0.65, 1.12) |
| > 5 | 1.32* (1.05, 1.65) | 0.71* (0.52, 0.97) |
Note. CI = confidence interval; RR = relative risk. The multivariable model adjusts for cluster-correlated data at level of census tract. The first column represents the full sample of women eligible for home visiting (n = 8187); the second column represents subset of women who were referred to the program (n = 2734).
Risk criteria: single marital status, age < 18 years, low-income status based on Medicaid enrollment, or Special Supplemental Nutrition Program for Women, Infants, Children enrollment.
Includes any diagnosis of premature rupture of membranes, chorioamnionitis, fetal distress, meconium-stained amniotic fluid, or unplanned maternal surgery as indicated on the vital statistics record.
Coefficients represent RR associated with a 5% increase in area-level usage of food stamps.
Calculated as a sum of the standardized scores for 4 census tract-level variables: (1) percentage unemployed; (2) percentage of households without access to a car; (3) percentage of all households renting; and 4) percentage of households with crowded housing. Higher Townsend Index scores reflect higher levels of deprivation and social disadvantage.
*P < .05; **P < .001.
Enrollment in Home Visiting
Bivariate comparisons of maternal and community characteristics with enrollment status among the 2734 women referred for home visiting are also depicted in Table 1. Among maternal factors, lack of a high school degree (54.5% vs 47.8%) and pregnancy complications (34.3% vs 27.7%) differed significantly between women who enrolled in the program and those who did not. In bivariate analysis, there was no significant difference in the distribution of TSI scores between enrolled and nonenrolled women.
Table 2 depicts that after adjustment for all covariates and clustering at the level of the census tract, both a high school degree (RR = 1.10; 95% CI = 1.00, 1.21) and any college education (RR = 1.17; 95% CI = 1.07, 1.29) were associated with increased enrollment compared with women without a high school degree. Prenatal referral compared with referral after birth was associated with a 1.61 RR of enrollment (95% CI = 1.51, 1.71), and the composite variable for pregnancy-related complications was associated with a 1.14 RR of enrollment (95% CI = 1.07, 1.22). At a systems level, individual agency catchment area was associated with differences in likelihood of enrollment. At a community level, areas where a majority of residences were multiunit housing were associated with a significantly higher likelihood of enrollment (RR = 1.27; 95% CI = 1.15, 1.39). Compared with communities scoring in the lowest TSI range, those with TSI scores greater than 5 were associated with a significantly lower likelihood of enrollment (RR = 0.71; 95% CI = 0.52, 0.97). When we transformed data for the TSI variable into standardized proportions using marginal standardization, the proportion enrolled among women with lowest TSI scores was 60% compared with 44% of women with TSI scores greater than 5 (P = .03).
Spatial Analysis
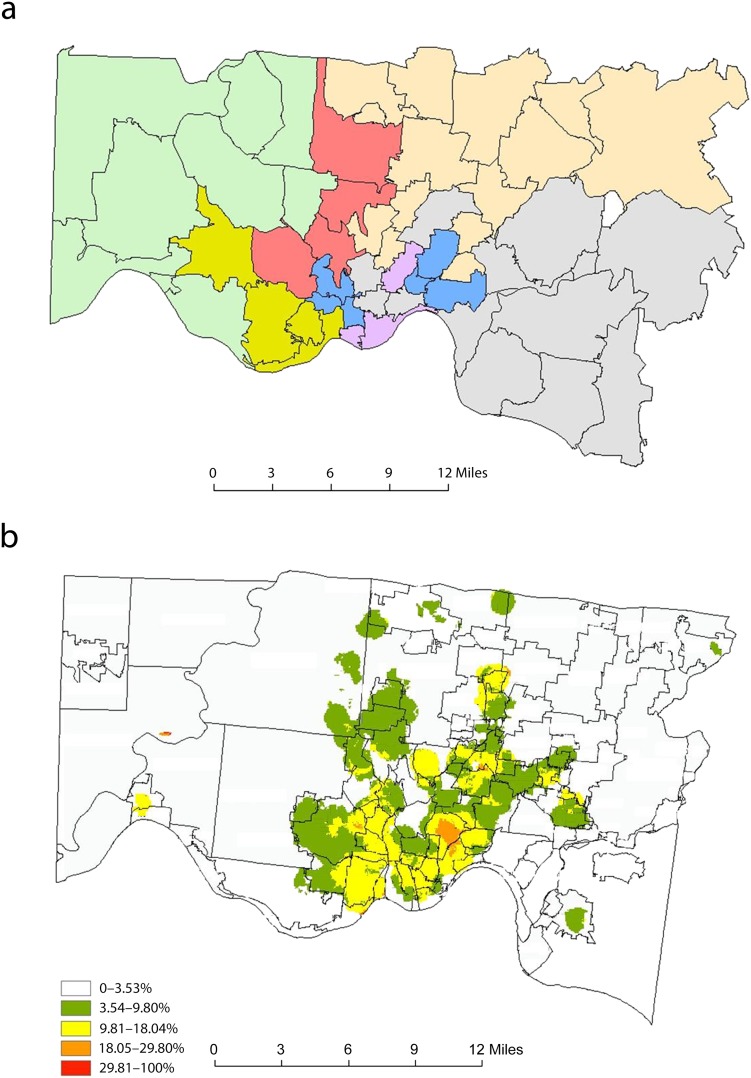
Figure 2 depicts a heat gradient for nonenrollment among mothers referred to home visiting in Hamilton County during the study timeframe. Geographic cells in the periphery were masked to suppress variation attributable to small sample sizes. This smoothed intensity estimation demonstrates geographic areas of lower and higher concentrations of nonenrollment. Two warm spots (Avondale and Whitewater Township) revealed areas with a relatively high percentage of women who were referred to home visiting but did not enroll. These areas are demographically distinct—Avondale is urban and predominantly African American and Whitewater Township is more rural and almost entirely White—however, both areas have poverty rates in excess of 33%.
FIGURE 2—
Maps of (a) agency catchment areas and (b) nonenrollment: Hamilton County, OH, 2007–2009.
Note. Panel a depicts primary geographic catchment areas for each home visiting agency, defined by color blocks; delineated borders represent zip code boundaries. Panel b depicts heat gradient for nonenrollment among mothers referred to home visiting; delineated borders represent neighborhood boundaries. Smoothed intensity estimation demonstrates geographic areas of lower and higher concentrations of nonenrollment. Geographic cells in the periphery are masked to suppress variation attributable to small sample sizes.
DISCUSSION
Several review studies of home visiting yielded inconsistent evidence of the association between participation in home visiting and improvements in pregnancy outcomes, including preterm birth.38,39 A clearer delineation of who was more likely to enroll in this intensive, prevention program was critical to understanding the impact of home visiting at a population level.40 On one hand, families who did not enroll might have had adequate resources, and therefore, did not need home visiting. On the other hand, lack of enrollment might reflect factors such as low health literacy, social isolation, discrimination, and low self-efficacy. This study evaluated referral to and enrollment in home visiting among eligible women using a population-based ecological approach. Results demonstrated that referral was more likely among those with lower education and in women living in communities with higher levels of social deprivation. However, once women were referred to home visiting, enrollment was paradoxically less likely for those with lower education and higher community levels of social deprivation. This suggested that despite appropriate referrals among the target, eligible population, there was lack of engagement among women at highest risk who were perhaps most in need of home visiting.
Previous work demonstrated that mothers intending to use home visiting were different from those who did not, and that intention was a key predictor of participation.15 Qualitative interviews of women refusing enrollment elicited themes, including perceived misgivings about home visiting, and lack of trust.14 The issue of vulnerability might be reflected in our findings that, among referred women, enrollment was more likely among those with pregnancy-related complications. Young age and lower education were also previously associated with refusal of home visiting.12 Additional studies explored maternal characteristics associated with duration or intensity of participation after enrollment, demonstrating that sustained engagement was associated with higher support needs.18–20 In context of our present findings, this suggested that women who agreed to enroll in home visiting might appropriately self-select into high and low users of services based on individual needs.
However, few previous studies evaluated the role of contextual factors in home visiting enrollment. McGuigan et al.24 previously demonstrated the independent effect of community violence on program retention after enrollment; the authors surmised that violence might erode engagement in home visiting through heightened stress, distrust, fear, and social isolation. Our study expanded this approach by exploring multilevel barriers to enrollment within an ecological framework. At a systems level, we demonstrated that residence by individual agency catchment area was associated with differences in likelihood of referral and enrollment, potentially reflecting variation in volume and wait list times, follow-up for hard-to-reach families, or engagement within the surrounding community, which might be different for larger versus smaller geographic catchment areas. Additionally, residence in areas with primarily multiunit housing were associated with increased likelihood of enrollment after referral, potentially indicating the importance of social interaction or peer networks for program acceptability. Finally at a community level, high level of deprivation (measured by the TSI) was independently associated with lower likelihood of using available support services despite being appropriately referred. The overall effect of contextual factors was represented by the heat map of nonenrollment for the county. Although the 2 “warm” neighborhoods were demographically distinct, both areas were affected by high rates of poverty. Such geographic clustering provided visual evidence of real-world barriers that might transcend individual factors in affecting program engagement.
Findings had several implications for providers targeting at-risk, maternal–child populations. First, results demonstrated the value of linking population and program data for the purpose of evaluating program reach and identifying characteristics of those in the target population that were difficult to engage. This underscored the potential utility of enhanced data systems containing participant information across provider agencies, such as WIC, home visiting programs, and prenatal clinics, to improve tracking of women at highest risk of loss to follow-up. Secondly, the association between prenatal referral to home visiting and higher likelihood of enrollment indicated the need for strong partnerships and coordination with prenatal care providers—particularly those with outreach in underserved communities. Third, results suggested the need for a multifaceted approach to engaging difficult-to-access populations, including strategies that leverage the cultural knowledge and social networks of lay health workers and community champions who live in the community they serve. Lastly, the paradoxical association of risk factors with enrollment compared with referral might be important not only for home visiting but also for other community-based services, from preschool readiness programs to jobs training programs. A similar study of early intervention participants, for example, demonstrated that although children referred to early intervention were at higher socioeconomic risk than the general population, there was a disproportionate loss of socially at-risk children during enrollment.41 At a systems level, maternal–child service providers within a range of settings might require more standardized approaches to mitigating loss to follow-up, while also acknowledging potential selection bias of participants when conducting program evaluations.
Limitations
Results of this observational analysis were subject to important limitations, most notably the issue of unmeasured confounding. Data were limited to what was available in vital records, which might have led to underestimates or overestimates and potentially contributed to misclassification bias. At the individual level, we were unable to measure intention to enroll and psychosocial factors such as stress level or social support. At a systems level, we did not measure characteristics of referring providers, the setting in which referral was made, or the process of enrollment itself (i.e., period of time on the waiting list). Such factors are likely to be important within an ecologic framework, and they may provide opportunities for logistical interventions to address barriers to enrollment.
Conclusions
Home visiting is one important intervention to mitigate risk for adverse maternal–child health outcomes through care coordination, education, and emotional support. Our findings suggested that among eligible women referred to home visiting, barriers to enrollment persisted at both individual and contextual levels. As states and communities implement and expand home visiting, ongoing evaluation is critical to ensuring that programs reach and engage families most in need of services.
Acknowledgments
N. K. Goyal was supported by the Buildling Interdisciplinary Research Careers in Women's Health (BIRCWH) K12 program, cofunded by the Office of Research on Women’s Health and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD; award number 5K12HD051953-07). R. T. Ammerman was supported by the National Institute of Mental Health (grant R01MH087499).
We would like to acknowledge the participation and support of the United Way of Greater Cincinnati, Kentucky HANDS, and Ohio Help Me Grow. In addition, we thank Robert Kahn, MD, for his critical review of the article.
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver NICHD, the National Institute of Mental Health, or the National Institutes of Health.
Human Participant Protection
This study was approved by the Ohio Department of Health and Cincinnati Children’s Hospital Medical Center institutional review boards. A waiver of consent for the use of human participant data was obtained.
References
- 1. US Census Bureau. Families and living arrangements; Table FM-1: families by presence of own children under 18: 1950 to present. Available at: http://www.census.gov/hhes/families/data/families.html. Accessed September 26, 2012.
- 2. US Census Bureau. Detailed poverty tables, POV03: people in families with related children under 18 by family structure, age, and sex, iterated by income-to-poverty ratio and race: 2009. Available at: http://www.census.gov/hhes/www/cpstables/032010/pov/new03_100_01.htm. Accessed September 26, 2012.
- 3.Slykerman RF, Thompson JM, Clark PM et al. Determinants of developmental delay in infants aged 12 months. Paediatr Perinat Epidemiol. 2007;21(2):121–128. doi: 10.1111/j.1365-3016.2007.00796.x. [DOI] [PubMed] [Google Scholar]
- 4.Singh GK, Kogan MD. Persistent socioeconomic disparities in infant, neonatal, and postneonatal mortality rates in the United States, 1969-2001. Pediatrics. 2007;119(4):e928–e939. doi: 10.1542/peds.2005-2181. [DOI] [PubMed] [Google Scholar]
- 5.Kotch JB, Browne DC, Dufort V, Winsor J. Predicting child maltreatment in the first 4 years of life from characteristics assessed in the neonatal period. Child Abuse Negl. 1999;23(4):305–319. doi: 10.1016/s0145-2134(99)00003-4. [DOI] [PubMed] [Google Scholar]
- 6.Behrman R, Butler A. Institute of Medicine (US) Committee on Understanding Premature Birth and Assuring Healthy Outcomes. Preterm Birth: Causes, Consequences, and Prevention. Washington, DC: National Academies Press; 2006. [PubMed] [Google Scholar]
- 7.Council on Child and Adolescent Health. The role of home-visitation programs in improving health outcomes for children and families. American Academy of Pediatrics. Pediatrics. 1998;101(3 Pt 1):486–489. doi: 10.1542/peds.101.3.486. [DOI] [PubMed] [Google Scholar]
- 8.Kitzman H, Olds DL, Henderson CR, Jr et al. Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing. A randomized controlled trial. JAMA. 1997;278(8):644–652. [PubMed] [Google Scholar]
- 9.Sweet MA, Appelbaum MI. Is home visiting an effective strategy? A meta-analytic review of home visiting programs for families with young children. Child Dev. 2004;75(5):1435–1456. doi: 10.1111/j.1467-8624.2004.00750.x. [DOI] [PubMed] [Google Scholar]
- 10. US Department of Health and Human Services. Home visiting evidence of effectiveness. Available at: http://homvee.acf.hhs.gov. Accessed January 31, 2013.
- 11. Health Resources and Services Administration. Maternal, infant, and early childhood home visiting program. 2010. Available at: http://mchb.hrsa.gov/programs/homevisiting/index.html. Accessed September 30, 2011.
- 12.Murray L, Woolgar M, Murray J, Cooper P. Self-exclusion from health care in women at high risk for postpartum depression. J Public Health Med. 2003;25(2):131–137. doi: 10.1093/pubmed/fdg028. [DOI] [PubMed] [Google Scholar]
- 13.Ireys HT, DeVet KA, Chernoff R. Who joins a preventive intervention? How risk status predicts enrollment. J Community Psychol. 2001;29(4):417–427. [Google Scholar]
- 14.Barlow J, Kirkpatrick S, Stewart-Brown S, Davis H. Hard-to-reach or out-of-reach? Reasons why women refuse to take part in early interventions. Child Soc. 2005;19(3):199–210. [Google Scholar]
- 15.McCurdy K, Daro D, Anisfeld E et al. Understanding maternal intentions to engage in home visiting programs. Child Youth Serv Rev. 2006;28(10):1195–1212. doi: 10.1016/j.childyouth.2005.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Duggan A, Windham A, McFarlane E et al. Hawaii’s healthy start program of home visiting for at-risk families: evaluation of family identification, family engagement, and service delivery. Pediatrics. 2000;105(1 Pt 3):250–259. [PubMed] [Google Scholar]
- 17.Tandon SD, Parillo K, Mercer C, Keefer M, Duggan AK. Engagement in paraprofessional home visitation: families’ reasons for enrollment and program response to identified reasons. Womens Health Issues. 2008;18(2):118–129. doi: 10.1016/j.whi.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 18.Navaie-Waliser M, Martin SL, Campbell MK et al. Factors predicting completion of a home visitation program by high-risk pregnant women: the North Carolina Maternal Outreach Worker Program. Am J Public Health. 2000;90(1):121–124. doi: 10.2105/ajph.90.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Daro D, McCurdy K, Falconnier L, Stojanovic D. Sustaining new parents in home visitation services: key participant and program factors. Child Abuse Negl. 2003;27(10):1101–1125. doi: 10.1016/j.chiabu.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 20.Ammerman RT, Stevens J, Putnam FW et al. Predictors of early engagement in home visitation. J Fam Violence. 2006;21(2):105–115. [Google Scholar]
- 21.South AP, Jones DE, Hall ES et al. Spatial analysis of preterm birth demonstrates opportunities for targeted intervention. Matern Child Health J. 2012;16(2):470–478. doi: 10.1007/s10995-011-0748-2. [DOI] [PubMed] [Google Scholar]
- 22.Kramer MR, Hogue CR. Place matters: variation in the black/white very preterm birth rate across US metropolitan areas, 2002-2004. Public Health Rep. 2008;123(5):576–585. doi: 10.1177/003335490812300507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McLaren L, Hawe P. Ecological perspectives in health research. J Epidemiol Community Health. 2005;59(1):6–14. doi: 10.1136/jech.2003.018044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McGuigan WM, Katzev AR, Pratt CC. Multi-level determinants of retention in a home-visiting child abuse prevention program. Child Abuse Negl. 2003;27(4):363–380. doi: 10.1016/s0145-2134(03)00024-3. [DOI] [PubMed] [Google Scholar]
- 25.Krieger N, Chen JT, Waterman PD et al. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: The Public Health Disparities Geocoding Project (US) J Epidemiol Community Health. 2003;57(3):186–199. doi: 10.1136/jech.57.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Townsend P, Phillimore P, Beattie A. Health and Deprivation. Inequality and the North. London, England: Croom Helm Ltd; 1988. [Google Scholar]
- 27.Young GS, Fox MA, Trush M et al. Differential exposure to hazardous air pollution in the United States: a multilevel analysis of urbanization and neighborhood socioeconomic deprivation. Int J Environ Res Public Health. 2012;9(6):2204–2225. doi: 10.3390/ijerph9062204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burr ML, Verrall C, Kaur B. Social deprivation and asthma. Respir Med. 1997;91(10):603–608. doi: 10.1016/s0954-6111(97)90006-8. [DOI] [PubMed] [Google Scholar]
- 29.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures–the Public Health Disparities Geocoding Project. Am J Public Health. 2003;93(10):1655–1671. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sun GW, Shook TL, Kay GL. Inappropriate use of bivariable analysis to screen risk factors for use in multivariable analysis. J Clin Epidemiol. 1996;49(8):907–916. doi: 10.1016/0895-4356(96)00025-x. [DOI] [PubMed] [Google Scholar]
- 31.McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157(10):940–943. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- 32.Robbins AS, Chao SY, Fonseca VP. What’s the relative risk? A method to directly estimate risk ratios in cohort studies of common outcomes. Ann Epidemiol. 2002;12(7):452–454. doi: 10.1016/s1047-2797(01)00278-2. [DOI] [PubMed] [Google Scholar]
- 33.Cameron AC, Gelbach JB, Miller DL. Bootstrap-based improvements for inference with clustered errors. Rev Econ Stat. 2008;90(3):414–427. [Google Scholar]
- 34.Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56(2):645–646. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- 35.Rogers WH. Regression standard errors in clustered samples. Stata Tech Bull. 1993;13:19–23. [Google Scholar]
- 36.Rushton G, Krishnamurthy R, Krishnamurti D, Lolonis P, Song H. The spatial relationship between infant mortality and birth defect rates in a US city. Stat Med. 1996;15(17-18):1907–1919. doi: 10.1002/(sici)1097-0258(19960930)15:18<1907::aid-sim402>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 37.Rushton G, Lolonis P. Exploratory spatial analysis of birth defect rates in an urban population. Stat Med. 1996;15(7-9):717–726. doi: 10.1002/(sici)1097-0258(19960415)15:7/9<717::aid-sim243>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 38.Issel LM, Forrestal SG, Slaughter J, Wiencrot A, Handler A. A review of prenatal home-visiting effectiveness for improving birth outcomes. J Obstet Gynecol Neonatal Nurs. 2011;40(2):157–165. doi: 10.1111/j.1552-6909.2011.01219.x. [DOI] [PubMed] [Google Scholar]
- 39.McNaughton DB. Nurse home visits to maternal-child clients: a review of intervention research. Public Health Nurs. 2004;21(3):207–219. doi: 10.1111/j.0737-1209.2004.021303.x. [DOI] [PubMed] [Google Scholar]
- 40.Stein RE, Bauman LJ, Ireys HT. Who enrolls in prevention trials? Discordance in perception of risk by professionals and participants. Am J Community Psychol. 1991;19(4):603–617. doi: 10.1007/BF00937994. [DOI] [PubMed] [Google Scholar]
- 41.Clements KM, Barfield WD, Kotelchuck M, Wilber N. Maternal socio-economic and race/ethnic characteristics associated with early intervention participation. Matern Child Health J. 2008;12(6):708–717. doi: 10.1007/s10995-007-0291-3. [DOI] [PubMed] [Google Scholar]