Abstract
Objectives. We used a geographic information system and cluster analyses to determine locations in need of enhanced Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) Program services.
Methods. We linked documented births in the 2010 California Birth Statistical Master File with the 2010 data from the WIC Integrated Statewide Information System. Analyses focused on the density of pregnant women who were eligible for but not receiving WIC services in California’s 7049 census tracts. We used incremental spatial autocorrelation and hot spot analyses to identify clusters of WIC-eligible nonparticipants.
Results. We detected clusters of census tracts with higher-than-expected densities, compared with the state mean density of WIC-eligible nonparticipants, in 21 of 58 (36.2%) California counties (P < .05). In subsequent county-level analyses, we located neighborhood-level clusters of higher-than-expected densities of eligible nonparticipants in Sacramento, San Francisco, Fresno, and Los Angeles Counties (P < .05).
Conclusions. Hot spot analyses provided a rigorous and objective approach to determine the locations of statistically significant clusters of WIC-eligible nonparticipants. Results helped inform WIC program and funding decisions, including the opening of new WIC centers, and offered a novel approach for targeting public health services.
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), a federally funded nutrition and health program, was established as a pilot program in 1972.1 WIC provides nutrition education, referrals, breastfeeding support, and nutritious supplemental food for low- to moderate-income families with nutritionally at-risk pregnant and breastfeeding women, infants, and children up to the 5th birthday.1,2 With an annual federal budget of $6.2 billion, the WIC program serves nearly 9 million participants each month through 1900 local agencies in state public health departments, Indian tribal organizations, and US territories.1,2 Additionally, the WIC Overseas Program provides services to Americans and dependents living overseas at US military bases. Nearly 30% of pregnant women participate in the WIC program nationally each year.2 In 2010, the WIC program served 62.6% of all who were eligible. WIC served 84.8% of eligible infants, 80.6% of eligible postpartum women (both breastfeeding and nonbreastfeeding), and 52.4% of eligible children aged 1 to 4 years.3 In California, WIC agencies provide services to nearly 1.45 million women, infants, and children each month at more than 625 sites statewide with an annual budget of approximately $1.2 billion.4
Research focused on the prenatal benefits of the WIC program has not produced consistent conclusions.5 Some research has indicated that WIC participation is associated with improved birth outcomes6 and that provision of WIC services to pregnant women reduced low birth weights (< 2500 g) and very low birth weights (< 1500 g) by 30% and 54%, respectively, with substantial reductions in first-year medical costs for US infants.7 Moreover, prenatal WIC participation was found to reduce racial disparities in infant mortality rates. For example, the infant mortality rate for African Americans was significantly lower for WIC participants than for non–WIC participants.8 However, other studies have indicated that prenatal participation in WIC had minimal effects on adverse birth outcomes.9,10
Not all women and children who are eligible to receive WIC services actually participate in the program.11 In 2007, only 59% of the total eligible US population participated in the program.12 Research has demonstrated that significantly higher rates of enrollment were observed for women who received prenatal care at health department– and community-sponsored clinics compared with hospital clinics and private physician offices.13 The number of prenatal visits was found to be positively associated with WIC participation rates among pregnant women,13 and the number of prenatal visits was found to improve birth outcomes. Previous participation in the WIC program was positively associated with early prenatal enrollment in WIC.14
Spatial analytical methods and geographic information systems (GISs) have increasingly been used in public health, epidemiology, and nutrition research.15–17 Nutrition researchers have begun to recognize the importance of GIS and spatial analysis, particularly as they relate to measuring the role of the built environment18 and the food environment.19 GIS and nonstatistical (i.e., descriptive) mapping techniques have recently been used to explore disparities in access to fresh produce in low-income neighborhoods.20 We are unaware of any studies, however, that have used statistically based spatial analyses to assess WIC-eligible women who were not participating in WIC services.
Hot spot analysis is a statistically based method to assess geographic clustering. Specifically, hot spot analysis is used to pinpoint locations of statistically significant high- and low-value clusters of a phenomenon of interest by evaluating each feature (e.g., census tract) within the context of neighboring features and against all features in the dataset.21 A feature with a high value may be a statistically significant hot spot if it is also surrounded by other features with high values, as opposed to simply being a data outlier. The local mean for a feature and its neighbors is compared proportionally with the global mean of all features (e.g., all census tracts in a state). When the observed local mean is much different than the global mean and that difference is too large to be the result of random chance, a statistically significant z score results and a hot spot cluster is detected.22 Recent studies using this technique have explored factors associated with West Nile virus incidence,23 tuberculosis transmission,24 patterns of sexually transmitted diseases,25 locations of health care services,26 and community-level overweight and obesity.27
The purpose of our study was to identify the macro- and microlevel geographic regions of California that contain clusters of WIC-eligible nonparticipants. Findings were intended to provide the California WIC Program with an evidence base for funds allocation, to inform program decisions for a subset of counties and subcounty areas, and to strategically target specific populations and areas for WIC service enhancements (i.e., opening of new WIC centers).
METHODS
We linked data from the California Birth Statistical Master File (BSMF) for all women with a live birth in 2010 (n = 503 722) with program data from the California WIC Integrated Statewide Information System (WIC-ISIS).4 The BSMF consists of variables documented on the birth certificate by hospital staff. WIC-ISIS data are entered by WIC staff during each participant visit. We linked WIC-ISIS records to the BSMF data on a combination of mother’s name and date of birth, infant’s name and date of birth, date of last prior live birth, father’s name, and address (city and zip code). To account for data quality issues, we took a broad query from WIC-ISIS that included all women who delivered or had an expected delivery date from November 2009 through February 2011, including all prenatal records for women who had a documented live birth in WIC-ISIS, as well as those who had a miscarriage, abortion, or stillbirth or who were lost to follow-up (outcome unknown). After accounting for duplicate records and excluding non-California residents from the BSMF, the final study population consisted of 501 907 California resident women with a live birth in 2010, of whom 279 288 (55.6%) had a prenatal record in WIC-ISIS. Of the remaining 222 619 women without a prenatal record in WIC-ISIS, 30 697 were deemed eligible for WIC services, based on their receipt of Medi-Cal benefits (i.e., Medicaid for California residents), which paid for prenatal care, labor and delivery, or both, as documented on the birth certificate. Thus, our final analytical sample included these 30 697 WIC-eligible nonparticipants.
Outcome Variable of Interest
Our outcome of interest for hot spot analysis was the density per square mile of WIC-eligible nonparticipants. Women were categorized as WIC participants if they had a prenatal record in WIC-ISIS. To obtain the density of WIC-eligible nonparticipants at the census tract level, we first calculated the area per California census tract in ArcGIS version 10.1 (Esri, Redlands, CA) and then divided the number of WIC-eligible nonparticipants in a census tract by that census tract’s square mile area.
Analyses
Geocoding.
The BSMF was geocoded before linkage to WIC-ISIS. We geocoded residential addresses for mothers who gave birth in 2010 using the browser-based geocoder available through the California Environmental Health Investigations Branch (http://www.ehib.org/toollist.jsp). During the geocoding process, we compared each address with reference data for streets and addresses across California and ultimately assigned each a latitude and longitude to create a point on a map (similar to placing a pin on a map). We attained a 98% geocoding match rate (i.e., addresses matched a reference address in the geocoder). We then conducted a “point in polygon join” (i.e., reverse geocoding) within the GIS to assign a census tract number to each geocoded address point. We used census tract boundaries for 2000 because 2010 boundaries were not available until well after we completed our data linkage, reverse geocoding, and spatial analyses.
Descriptive mapping.
We used descriptive GIS mapping techniques to assess the spatial distribution of WIC-eligible nonparticipants at the state, county, and subcounty levels. We explored the distribution of WIC-eligible nonparticipant counts, percentages of women who were WIC-eligible nonparticipants of all WIC-eligible women, and densities with thematic maps and corresponding data tables. These maps provided preliminary indications of the spatial distribution of WIC-eligible nonparticipants. In such thematic maps, however, it was not possible to reliably determine definitive patterns across the 7049 census tracts in the state. We conducted spatial analyses that invoked a number of statistical tests in our next phase of analysis to determine the location of statistically significant clusters of high densities of WIC-eligible nonparticipants.
Spatial analysis.
We used a series of spatial analytical techniques to find clusters of WIC-eligible nonparticipants on the macro- (i.e., state) and microlevels (county).
Step 1—Analysis of Variation in California Census Tract Areas
In California, census tracts range in size from 0.02 to 7992.4 square miles, with a mean area of 22.4 square miles (SD = 173.79). This variation can cause analytic challenges in 2 ways. First, in descriptive mapping, one is visually biased by the bigger-sized tracts even though the measured outcome may be just as pronounced (or more so) in smaller tracts (census tracts are relatively homogeneous in population size and demographic makeup). Second, it is difficult to develop an appropriate neighborhood (local mean) size (i.e., spatial scale) with large variation in areas. To understand the degree of size variation in California’s 7049 census tracts, we calculated the square mile area of all census tracts in the state. We considered census tracts that possessed a square mile area greater than 1.5 standard deviations above the state mean census tract area outliers (n = 118) and temporarily removed them from the dataset. In addition, we also removed small census tracts that had been adjacent to the removed ones (and appeared as “islands”; n = 11). This allowed us to begin to control for variability in census tract size in the next step of the analysis, considering census tracts of homogeneous geographic sizes.
Step 2—Determination of Spatial Scale, Part A
We began to determine the appropriate spatial scale for remaining California census tracts (n = 6920). Because our hot spot analysis examined each census tract in the context of its neighbors, we needed to develop an analytic sphere of influence around each census tract. We therefore calculated the average and maximum distance it would take to get from the geocentroid of each census tract to the geocentroid of its nearest 2 neighbors, deciding a priori that 3 neighboring census tracts with high or low WIC-eligible nonparticipant densities would constitute a cluster.
Step 3—Determination of Spatial Scale (the Moran I ), Part B
To inform allocation of resources in the most focused area possible, we were interested in using the smallest possible distance (analytic sphere of influence) at which clustering of WIC-eligible nonparticipants was most intense, if clustering existed at all. If geographic analysis was to be useful, our outcome of interest (WIC-eligible nonparticipants per square mile) needed to exhibit spatial autocorrelation (based on Tobler’s first law of geography, which states that everything is related to everything else, but nearby things are more related than things that are far away28) to ensure that we found the shortest distance for which clustering (spatial autocorrelation) was intense. A common statistical measure of the degree to which a set of spatial features and their associated data values tended to be clustered or dispersed is the Moran I.21
We performed the Moran I test at multiple distances using the results from step 2. Our shortest distance tested was two thirds of the maximum distance it would take to reach the 2 nearest neighboring census tracts. Our experience has shown that using the actual maximum distance is often too conservative when trying to find the distance of most intense clustering at local geographic scales, because it is possible that all island census tracts were not removed or that larger census tracts continued to inflate the result of the distance-to-2-neighbors calculation. Subsequent Moran I tests were done incrementally, using half of the average distance to 2 neighbors found in step 2. Testing continued until the resulting z score peaked and was statistically significant (P < .05). The distance at that peak point (see Figure A, available as a supplement to the online version of this article at http://www.ajph.org) represented the smallest distance at which clustering of WIC-eligible nonparticipants was most intense and therefore represented an appropriate scale of analysis for subsequent hot spot analyses (step 5).
Step 4—Accounting for the Larger Polygons
Once we determined the distance that was the exemplar sphere of influence, or distance band, for the hot spot analysis, we next accounted for the large and island census tracts that had previously been left out of the analysis. To do this, we created a definition file called a spatial weights matrix that represented the spatial structure of our data and quantified the spatial relationships that existed among the features in the dataset. The structure of the matrix was an N × N table where N was the number of features in the dataset. Every feature in the dataset had 1 row and 1 column. We chose a binary strategy to quantify the relationships among data features in our dataset so that in the matrix a feature either was a neighbor (1) or was not (0). In this case, we included a feature as a neighbor if it was within the distance band calculated in step 3 or, for the previously excluded features, if it was 1 of the 2 nearest neighbors. With this strategy, every feature in the dataset was guaranteed 2 neighbors even if those neighbors did not fall within the local distance band parameter.
Step 5—Hot Spot Analysis
Finally, we conducted hot spot analyses to determine the locations of statistically significant clusters of census tracts with higher densities of WIC-eligible nonparticipants than would be expected given the mean density of WIC-eligible nonparticipants in the dataset.
We first conducted this 5-step geoprocessing approach to analyze the density of WIC-eligible nonparticipants for all 7049 census tracts in California to detect counties with clusters of WIC need relative to the state mean. Once we determined significant hot spot clusters and identified priority counties, we repeated the 5-step geoprocessing approach to identify more local clusters of census tracts relative to means of those priority counties.
RESULTS
Our results consist of 2 main components: (1) the step-by-step results that led to each subsequent stage in the hot spot analysis, drawing attention to the reproducibility and objectivity of the hot spot methodology, and (2) the locations in which we found hot or cold spots for WIC-eligible nonparticipants.
Descriptive Maps
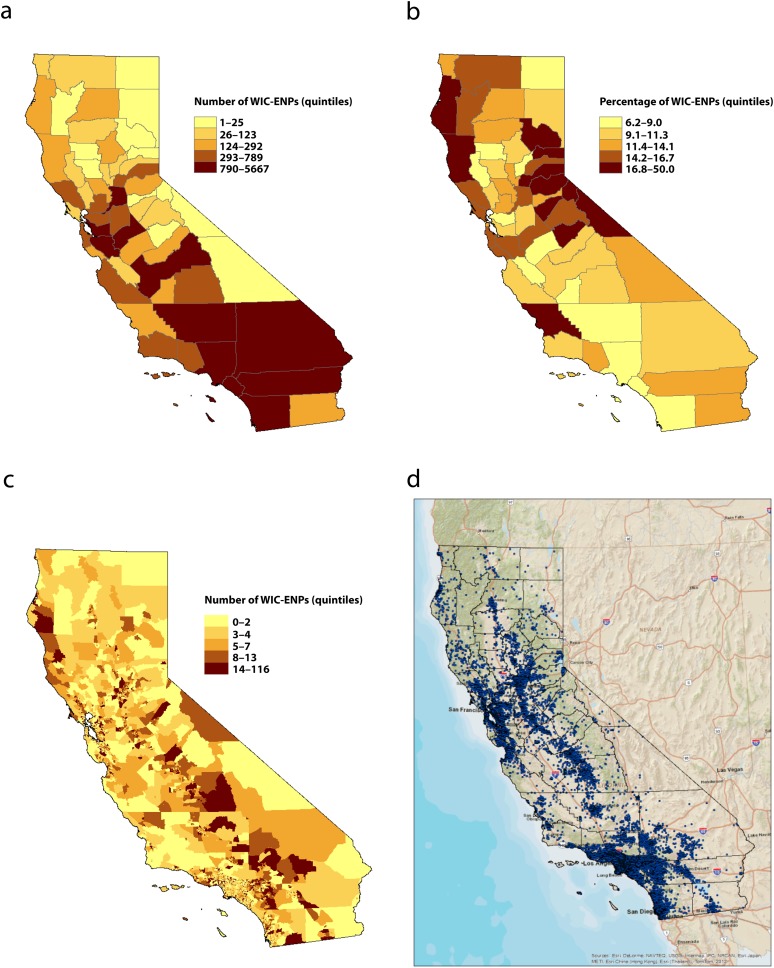
Descriptive thematic maps portray the number, percentage, and density of WIC-eligible nonparticipants across California by counties and census tracts (Figure 1). Counts and percentages were categorized by quintiles. These maps indicated that counties in the Bay Area, the Central Valley, and the Los Angeles County Basin possessed large counts and densities of WIC-eligible nonparticipants (Figure 1a, 1c, 1d) and provided initial information about the burden of unmet WIC service needs. Figure 1b portrayed the percentage of WIC-eligible women who were eligible nonparticipants, providing initial indications of WIC service coverage.
FIGURE 1—
Thematic maps of Special Supplemental Nutrition Program for Women, Infants and Children–eligible nonparticipants by (a) number at the county level, (b) percentage at the county level, (c) number at the census tract level, and (d) dot density at the census tract level: California, 2010.
Note. ENPs = eligible nonparticipants; WIC = Women, Infants, and Children.
Incremental Spatial Autocorrelation
The distance at which clustering of WIC-eligible nonparticipants was greatest, when considering all 7049 California census tracts, was 26 kilometers (16.2 miles; z score = 37.3; P < .001). The distance in county-specific analyses varied by county: Sacramento (distance = 5 km; z score = 9.1; P < .001 [see Figure A]), San Francisco (distance = 1.1 km; z score = 3.2; P = .001), Los Angeles (distance = 11 km; z score = 39.4; P < .001), and Fresno (distance = 9 km; z score = 10.6; P < .001).
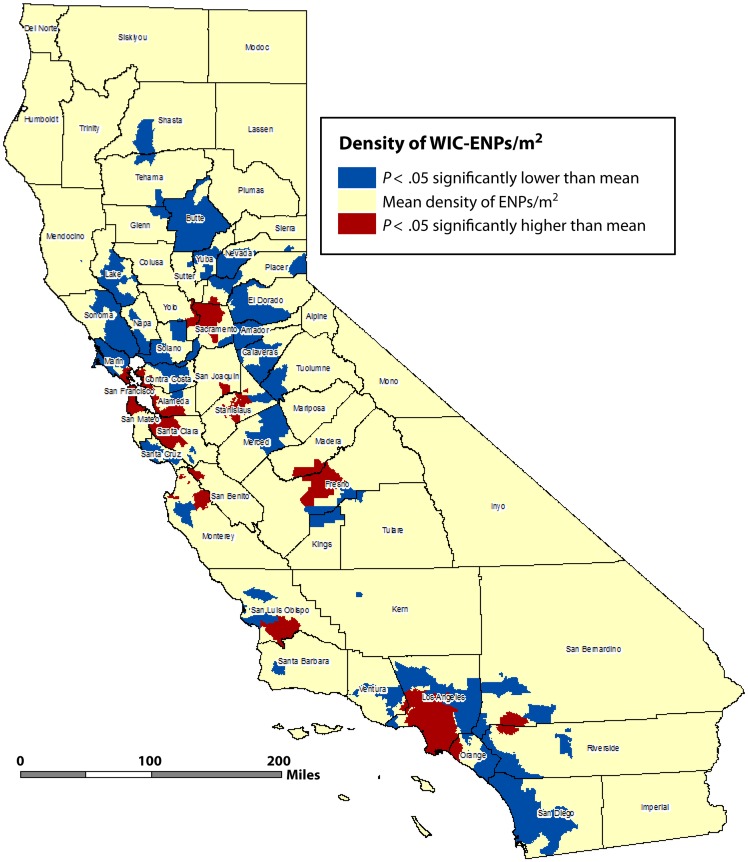
Hot Spot Cluster Analysis
Results from hot spot analyses at the census tract level portray a detailed picture of the statistically significant clusters of WIC-eligible nonparticipants (Figure 2). Red census tracts denoted hot spot clusters with significantly higher densities of WIC-eligible nonparticipants than the mean density of eligible nonparticipants for all census tracts (P < .05). Yellow tracts represented census tracts that had densities of WIC-eligible nonparticipants that were not statistically different from the mean density of WIC-eligible nonparticipants in the state. Blue census tracts denoted cold spots, or lower densities of WIC-eligible nonparticipants, that were significant at the P < .05 level.
FIGURE 2—
Clusters of Special Supplemental Nutrition Program for Women, Infants and Children ENPs: California, 2010.
Note. ENPs = eligible nonparticipants; WIC = Women, Infants, and Children. Analyses based on density of Women, Infants and Children–ENPs per square mile per census tract (n = 7049). Hot spots (red) represent clusters of census tracts with densities of ENPs that were significantly higher than mean densities of ENPs for the state (P < .05). Cold spots (blue) represent clusters of census tracts with densities of ENPs that were significantly lower than mean densities of ENPs for census tracts throughout the state (P < .05). Yellow areas represent census tracts with densities of ENPs that were not significantly different than the mean density for all census tracts in the state. Distance band = 26 kilometers (16.2 miles). Projected coordinate system: NAD83, CA Teale Albers.
In statewide analyses (58 counties), we found statistically significant hot spot clusters of census tracts with high densities of WIC-eligible nonparticipants in 21 counties: 7 counties in the Central Valley (Sacramento, Yolo, Placer, San Joaquin, Stanislaus, Madera, Fresno), 6 counties in the San Francisco Bay Area (Marin, San Francisco, Contra Costa, Alameda, San Mateo, Santa Clara), 3 Central Coast counties (San Benito, Monterey, San Luis Obispo), and 5 Southern California counties (Ventura, Los Angeles, Orange, San Bernardino, Riverside; P < .05). Significant cold spot clusters (blue shading), with low densities of WIC-eligible nonparticipants, existed in 37 counties, with notable clusters in the more rural regions of the state.
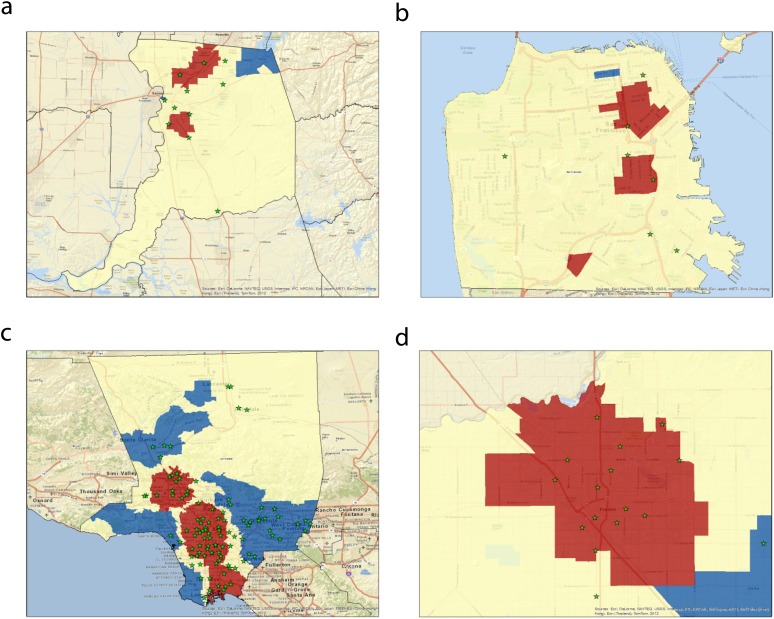
The San Francisco Bay Area, Los Angeles County, and the Central Valley, which encompassed large hot spots and a large number of WIC-eligible nonparticipants, merited closer attention. County-specific hot spot analyses revealed neighborhood-level clusters of census tracts with high densities of WIC-eligible nonparticipants, primarily in urban areas of the counties (Figure 3). We found local hot spot clusters of census tracts with high densities of WIC-eligible nonparticipants in the Downtown and North Highlands neighborhoods of Sacramento; the Tenderloin, Civic Center, South of Market, and Mission neighborhoods in San Francisco; the Downtown, Reseda, and Long Beach areas in Los Angeles; and the Central Valley.
FIGURE 3—
County-specific hot spot maps for Special Supplemental Nutrition Program for Women, Infants and Children ENPs in (a) Sacramento, (b) San Francisco, (c) Los Angeles, (d) and Fresno: California, 2010.
Note. Hot spots (red) represent clusters of census tracts with densities of eligible nonparticipants (ENPs) that were significantly higher than mean densities of ENPs for the county (P < .05). Cold spots (blue) represent clusters of census tracts with densities of ENPs that were significantly lower than mean densities of ENPs for census tracts throughout the county (P < .05). Yellow areas represent census tracts with densities of ENPs that were not significantly different than the mean density for all census tracts in the county. Existing WIC Centers are represented by green stars. Projected coordinate system: NAD 83, CA Teale Albers.
DISCUSSION
GIS and spatial analyses have experienced considerable growth and popularity in public health in recent decades. The growing role of space and geography in understanding health issues and applying interventions underscores the fact that the field of spatial epidemiology, with ever improving hardware and software tools, is greatly needed.
In California, we used data visualization techniques with a GIS and conducted systematic and complex spatial analyses to determine the location of statistically significant clusters of census tracts with high densities of WIC-eligible nonparticipants in 2010. We used a 5-step geoprocessing approach, culminating in cluster-detecting hot spot analyses, which allowed us to first determine the California counties with greatest unmet need for WIC services. Then, in 4 counties, we performed local hot spot analyses to determine the opportunity neighborhoods with regard to clusters of WIC-eligible nonparticipants.
We detected clusters of WIC-eligible nonparticipants in the San Francisco Bay Area, along the Central Pacific Coast, in the Central Valley, and in the Los Angeles Basin. These clusters of high eligible nonparticipant densities appeared to parallel areas of high population density and large densities of families living in poverty (data not shown). County-level hot spot analyses in Sacramento, San Francisco, Fresno, and Los Angeles highlighted locations in which WIC directors could consider enhancing WIC services and outreach by increasing staffing, service hours, or the number of WIC sites available on the local level. Conversely, statistically significant cold spots highlighted regions in which expanded WIC services may not have been needed and in which WIC may have been adequately serving those communities’ needs.
The results of our spatial and statistical analyses have been presented to WIC directors, WIC staff, health care providers, and stakeholder groups through GIS maps, interactive online map presentations, and reports. The results have been used to guide resource allocation decisions, target outreach efforts, and help guide public health policy and program enhancement decisions. In Sacramento County, for instance, 1 local WIC agency used results from Sacramento hot spot cluster analyses, in concert with local data, to guide the opening of 2 new WIC centers.
Our study has several limitations. We focused on the location of residence at the time of birth in 2010 and, as a result, cluster analyses may not represent the reality of counties, cities, and local regions today. In our experience, however, we have not seen large changes in WIC service needs from one year to the next between 2008, 2009, and 2010, and our current findings are likely to represent needs for WIC services for the years immediately preceding and following 2010. Moreover, our methodology is highly reproducible and can be used annually to track change and improvements in programmatic services. Although our hot spot analyses allow us to determine locations in which WIC services may need to be modified to meet increasing or decreasing service needs, hot spot analyses do not allow us to determine the factors that are associated with such clusters of need. Multivariate logistic regression and spatial regression methods are needed to determine such associations and will be considered in subsequent analyses.
Finally, our calculation for WIC-eligible nonparticipants in California (n = 30 697) was based on Medi-Cal status (i.e., if women were on Medi-Cal, they were eligible for WIC services). Women may also have been eligible for WIC services if their income was lower than 185% of the federal poverty level, even if they were not receiving Medi-Cal benefits. We estimate that this could have expanded our population of WIC-eligible nonparticipants to approximately 51 300. Data for these larger eligible nonparticipant estimates were not available for our analyses and will be considered for future research.
The federally funded WIC program has been around for nearly 4 decades and, although the program continues to provide important nutrition support and health education to millions of mothers, infants, and children across the country each year, the use of spatial data and complex spatial analyses foster fine-tuned assessments of program coverage and areas of refined service apportionment.
Our 5-step geoprocessing analysis that culminated in hot spot maps provided a rigorous and systematic method to determine the location of statistically significant clusters of WIC-eligible women. Use of these approaches in addition to traditional data visualization techniques (e.g., thematic maps) provides policymakers and program managers with an evidence base for important public health program and funding decisions. Similar analyses can be conducted for other public health programs to help assess the coverage and breadth of services in specified catchment areas that can facilitate targeting of public health services. During good budgetary times, hot spot analyses can point to counties, cities, and local neighborhoods in which services can be enhanced. During less favorable economic times, cold spot clusters can help inform policymakers and program directors to provide services in more efficient ways or relocate services to areas of higher need. Used in concert with statistical modeling approaches and spatial epidemiology, hot spot analyses provide additional tools for researchers, public health practitioners, and policymakers.
Acknowledgments
We thank the California WIC Program through the US Department of Agriculture for funding to conduct this study (universal ID 7CA700CA7).
We thank Catherine Camacho, director for MCAH, Center for Family Health, CDPH, Shabbir Ahmad, Barbara Longo, Michael Curtis, and Charlene Manning for support on this work and Katie Martin, Sibylle Lob, and Archana Minnal for contributions to earlier phases of analysis. We are grateful to Lauren Scott and Lauren Rosenhein Bennett for technical assistance with the hot spot cluster analysis methodology.
Human Participant Protection
This study was reviewed by the Committee for the Protection of Human Subjects, Health and Human Services Agency, State of California, and was deemed exempt.
References
- 1. US Department of Agriculture. Food and Nutrition Service. Women, Infants and Children. Available at: http://www.fns.usda.gov/wic. Accessed September 14, 2011.
- 2.Oliveira VJ, Frazão E. The WIC Program Background, Trends, and Economic Issues. Economic Research Service report no 73. Washington, DC: US Department of Agriculture, Economic Research Service; 2009. [Google Scholar]
- 3.Martinez-Schiferl M, Zedlewski S, Giannarelii L. National and State-Level Estimates of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) Eligibles and Program Reach, 2010. Washington, DC: US Department of Agriculture, Food and Nutrition Service, Office of Research and Analysis; 2013. [Google Scholar]
- 4. California WIC Association. WIC Program at a glance. Available at: http://www.calwic.org. Accessed September 22, 2011.
- 5.Ludwig J, Miller M. Interpreting the WIC debate. J Policy Anal Manage. 2005;24(4):691–701. doi: 10.1002/pam.20133. [DOI] [PubMed] [Google Scholar]
- 6.Bitler MP, Currie J. Does WIC work? The effects of WIC on pregnancy and birth outcomes. J Policy Anal Manage. 2005;24(1):73–91. doi: 10.1002/pam.20070. [DOI] [PubMed] [Google Scholar]
- 7.Avruch S, Cackley AP. Savings achieved by giving WIC benefits to women prenatally. Public Health Rep. 1995;110(1):27–34. [PMC free article] [PubMed] [Google Scholar]
- 8.Khanani I, Elam J, Hearn R, Jones C, Maseru N. The impact of prenatal WIC participation on infant mortality and racial disparities. Am J Public Health. 2010;100(suppl 1):S204–S209. doi: 10.2105/AJPH.2009.168922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Joyce T, Gibson D, Colman S. The changing association between prenatal participation in WIC and birth outcomes in New York City. J Policy Anal Manage. 2005;24(4):661–685. doi: 10.1002/pam.20131. [DOI] [PubMed] [Google Scholar]
- 10.Joyce T, Racine A, Yunzal-Butler C. Reassessing the WIC effect: evidence from the Pregnancy Nutrition Surveillance System. J Policy Anal Manage. 2008;27(2):277–303. doi: 10.1002/pam.20325. [DOI] [PubMed] [Google Scholar]
- 11.Black MM, Cutts DB, Frank DA et al. Special Supplemental Nutrition Program for Women, Infants, and Children participation and infants’ growth and health: a multisite surveillance study. Pediatrics. 2004;114(1):169–176. doi: 10.1542/peds.114.1.169. [DOI] [PubMed] [Google Scholar]
- 12.Harper E, Hirschman J, Mabli J, Nelson S, Hourihan K. WIC Eligibles and Coverage—1994 to 1997: Estimates of the Population of Women, Infants, and Children Eligible for WIC Benefits. Washington, DC: US Department of Agriculture, Food and Nutrition Service; 2009. [Google Scholar]
- 13.Kahler LR, O’Shea RM, Duffy LC, Buck GM. Factors associated with rates of participation in WIC by eligible pregnant women. Public Health Rep. 1992;107(1):60–65. [PMC free article] [PubMed] [Google Scholar]
- 14.Ku L. Factors influencing early prenatal enrollment in the WIC program. Public Health Rep. 1989;104(3):301–306. [PMC free article] [PubMed] [Google Scholar]
- 15.Moore DA, Carpenter TE. Spatial analytical methods and geographic information systems: use in health research and epidemiology. Epidemiol Rev. 1999;21(2):143–161. doi: 10.1093/oxfordjournals.epirev.a017993. [DOI] [PubMed] [Google Scholar]
- 16.Ghirardelli A, Quinn V, Foerster SB. Using geographic information systems and local food store data in California’s low-income neighborhoods to inform community initiatives and resources. Am J Public Health. 2010;100(11):2156–2162. doi: 10.2105/AJPH.2010.192757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson ML. Neighborhood racial composition, neighborhood poverty, and the spatial accessibility of supermarkets in metropolitan Detroit. Am J Public Health. 2005;95(4):660–667. doi: 10.2105/AJPH.2004.042150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thornton LE, Pearce JR, Kavanagh AM. Using geographic information systems (GIS) to assess the role of the built environment in influencing obesity: a glossary. Int J Behav Nutr Phys Act. 2011;8:71. doi: 10.1186/1479-5868-8-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Charreire H, Casey R, Salze P et al. Measuring the food environment using geographical information systems: a methodological review. Public Health Nutr. 2010;13(11):1773–1785. doi: 10.1017/S1368980010000753. [DOI] [PubMed] [Google Scholar]
- 20.Algert SJ, Agrawal A, Lewis DS. Disparities in access to fresh produce in low-income neighborhoods in Los Angeles. Am J Prev Med. 2006;30(5):365–370. doi: 10.1016/j.amepre.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 21.Ord JK, Getis A. Local spatial autocorrelation statistics: distributional issues and an application. Geogr Anal. 1995;27(4):286–306. [Google Scholar]
- 22.Mitchell A. The ESRI Guide to GIS Analysis: Spatial Measurements and Statistics. Vol 2. Redlands, CA: ESRI Press; 2005. [Google Scholar]
- 23.DeGroote JP, Sugumaran R, Brend SM, Tucker BJ, Bartholomay LC. Landscape, demographic, entomological, and climatic associations with human disease incidence of West Nile virus in the state of Iowa, USA. Int J Health Geogr. 2008;7:19. doi: 10.1186/1476-072X-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haase I, Olson S, Behr MA et al. Use of geographic and genotyping tools to characterise tuberculosis transmission in Montreal. Int J Tuberc Lung Dis. 2007;11(6):632–638. [PubMed] [Google Scholar]
- 25.Rusch ML, Brouwer KC, Lozada R, Strathdee SA, Magis-Rodríguez C, Patterson TL. Distribution of sexually transmitted diseases and risk factors by work locations among female sex workers in Tijuana, Mexico. Sex Transm Dis. 2010;37(10):608–614. doi: 10.1097/OLQ.0b013e3181deaa0f. [DOI] [PubMed] [Google Scholar]
- 26.Tsai PJ, Lin ML, Chu CM, Perng CH. Spatial autocorrelation analysis of health care hotspots in Taiwan in 2006. BMC Public Health. 2009;9:464. doi: 10.1186/1471-2458-9-464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Penney TL, Rainham DG, Dummer TJ, Kirk SF. A spatial analysis of community level overweight and obesity. J Hum Nutr Diet. 2013 doi: 10.1111/jhn.12055. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 28.Tobler W. A computer movie simulating urban growth in the Detroit region. Econ Geogr. 1970;46(2):234–240. [Google Scholar]