Birth outcomes are improving in the United States. Following a plateau from 2000 through 2005, the US infant mortality rate (IMR) declined 12% from 2006 through 2011, with the greatest decline seen among non-Hispanic Black women (16%).1 Similarly, preterm birthrate also declined by 10% from 2006 through 2012.2
But now is not the time to declare mission accomplished. The United States still ranks near the bottom among developed nations in infant mortality and other birth outcomes.1 Furthermore, significant racial/ethnic and socioeconomic disparities persist. For example, despite recent improvements, African Americans have 2.3 times the IMR as non-Hispanic Whites.3
On June 14, 2012, Health and Human Services Secretary Kathleen Sebelius called for the first national strategy to address infant mortality.4 The Secretary’s Advisory Committee on Infant Mortality was charged with developing recommendations for the national strategy. The Committee consists of members who represent diverse backgrounds and perspectives: public and private; federal, state, and local; and providers, consumers, and families.5 The Committee also brings together, as ex officio members, various federal agencies that are working to address infant mortality. The Committee delivered its recommendations to the Secretary earlier this year,6 which we summarize in this editorial.
THE LIFE COURSE PERSPECTIVE
The Committee used the life course perspective as a guiding framework for the development of its recommendations. The life course perspective views life not as disconnected stages but as an integrated continuum.7 It recognizes that each stage of life is influenced by all the life stages that precede it, and it, in turn, influences all the life stages that follow it. With respect to birth outcomes, it provides a longitudinal account of the interplay of biological, behavioral, psychological, social, and environmental factors in producing birth outcomes. It conceptualizes birth outcomes as the product of not only the nine months of pregnancy but of the entire life course of the mother from before her own conception and leading up to the pregnancy. Disparities in birth outcomes, therefore, are the consequences of not only differential exposures during pregnancy but of differential health trajectories across the life span.7
The life course perspective suggests a need for a paradigm shift in our national strategy to address infant mortality.8 It calls for an expanded approach to improve birth outcomes in the United States, one that emphasizes not only risk reduction during pregnancy but also health promotion and optimization before and between pregnancies and, indeed, across the life course. The approach needs to be both clinical and population-based, addressing individual factors as well as social determinants of health.
TOWARD A NATIONAL STRATEGY ON INFANT MORTALITY
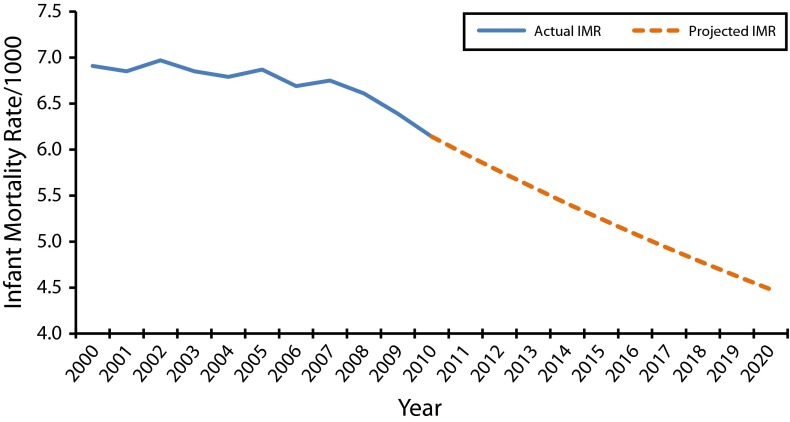
Recognizing that we have already neared the Healthy People 2020 target for IMR of 6.0 infant deaths per 1000 live births, the Committee called for a stretch goal—the nation should aim to reduce IMR to 5.5 infant deaths per 1000 live births by 2015 and to 4.5 by 2020 (Figure 1).
FIGURE 1—
Trend in US infant mortality rate (IMR): actual and projected to 2020.
Note. The projected IMR is based on 2007–2010 average annual trend (–3.1%).
The Committee identified six strategic priorities for the national strategy, encompassing both “low-hanging fruits” as well as life course and intergenerational investments to address infant mortality.
Improve Women’s Health Before Pregnancy
For more than two decades, prenatal care was our nation’s answer to the problem of infant mortality. In the late 1980s through the 1990s, federal and state efforts to expand Medicaid coverage for pregnant women led to significant increases in prenatal care utilization, but not in significant improvements in birth outcomes. This is not to take anything away from prenatal care. It’s necessary, but not sufficient.9,10
There is now growing recognition that to improve US birth outcomes, we need to start by improving the health of girls and women before pregnancy.11 Since 2005, Centers for Disease Control and Prevention has led a national movement to promote preconception health and health care in the United States.12 But the game changer this time is the Affordable Care Act. Starting in August 2012 with the implementation of the clinical preventives services for women, millions of women gained access to health care even when not pregnant (including coverage for preconception and interconception care without copay), services that provide an extraordinary opportunity to improve women’s health not only during pregnancy but before, between, and beyond pregnancy and across their life course.13,14
Improve Quality and Safety of Maternal and Neonatal Care
An example of a low-hanging fruit for improving birth outcomes is to reduce early elective deliveries. Compared with infants born after 39 completed weeks of gestation, infants delivered after 37 weeks but before 39 weeks have significantly greater risks of mortality and morbidities15,16 and account for an estimated $1 billion in increased hospital costs annually.17 Efforts in recent years to educate patients and providers, implement rapid-cycle quality improvement processes, or institute a hard-stop policy at the hospital or payer level have been shown to be effective in curbing early elective deliveries.15,18,19 A recent study of a rapid-cycle process improvement program in 26 hospitals resulted in significant reduction in elective scheduled early-term deliveries, from 28% to less than 5% in 12 months.19 Several national initiatives are now under way such as the Healthy Babies Are Worth the Wait Campaign (March of Dimes),20 Healthy Babies Initiative (Association of State and Territorial Health Officials [ASTHO]),21 Strong Start Initiative (Center for Medicare and Medicaid Innovation [CMMI]),22 and Collaborative Improvement and Innovation Network (Health Resources and Services Administration [HRSA]).23 There are many other low-hanging fruits whereby better care can lead to better outcomes and lower costs, such as the Maternal Safety Bundle (Society for Maternal–Fetal Medicine, American Congress of Obstetricians and Gynecologists [SMFM-ACOG])24 to reduce morbidities from thromboembolism, hemorrhage, and preeclampsia on the maternal side, and appropriate use of 17P (a Food and Drug Administration–approved progesterone medicine for use by pregnant women with a previous preterm delivery), screening for asymptomatic bacteriuria or group B streptococcus, or reducing central-line–associated bloodstream infections in newborns on the neonatal side.
A central tenet of quality-improvement science is that quality improvement is not about making individuals work harder; it is about making the system work smarter.25 Presently our so-called perinatal health system is highly fragmented, and the key to making that system work smarter is integration—vertical, horizontal, and longitudinal. Vertical integration refers to appropriate levels of care. For very low birth weight and very preterm infants, birth outside of a level III hospital is significantly associated with increased likelihood of neonatal or predischarge death,26 and yet nearly one in four such infants are born outside of a level III hospital.27 (Level III hospitals provide perinatal services outlined for all levels of care, as well as diagnosis and treatment of high-risk pregnancy and neonatal problems.) The American Academy of Pediatrics recently updated its policy statement regarding levels of neonatal care, to state that facilities that provide hospital care for newborn infants should be classified on the basis of functional capabilities and that these facilities should be organized within a regionalized system of perinatal care.28 Horizontal integration refers to service coordination and systems integration across multiple sectors. The State of North Carolina developed a statewide network of pregnancy medical homes, and CMMI, through its Strong Start Initiative, is testing a similar model of maternity care home to enhance the quality of prenatal care.22 Longitudinal integration refers to the continuum of comprehensive women’s health care, from preconception through prenatal to postpartum and interconception care and across the life course. The State of Georgia is using its Medicaid 1115 waiver to provide interconception care to high-risk women whose pregnancy-related Medicaid would have otherwise terminated at 60 days postpartum, and the Committee calls for CMMI to expands its initiative to expand beyond prenatal care to test innovative models of preconception and interconception care.
Focus on Primary Prevention
While much of prenatal care currently focuses on secondary and tertiary prevention, the Committee identified five areas where there are highly effective evidence-based strategies for reducing infant mortality through primary prevention: smoking cessation, breastfeeding, family planning, immunization, and safe sleep. Despite the success of the back-to-sleep campaign, still one in four US infants and nearly 40% of non-Hispanic Black infants are not placed on their back to sleep.29 Furthermore, infant deaths caused by accidental suffocation and strangulation in bed and other sudden unexplained infant deaths are on the rise. The Eunice Kennedy Shriver National Institute of Child Health and Human Development and its partners have now broadened their safe sleep campaign to include three key messages: back-to-sleep for every sleep, room-sharing without bed-sharing, and keep soft objects and loose bedding out of the crib.30 The Committee recommends exploration of new platforms, such as group prenatal care model,31 and new technologies, such as the use of short messaging service and social media, to deliver health messaging on prevention and promotion to a new generation of mothers and families.
Address Social Determinants
The Committee recognizes that there are important social determinants operating across the life course, which are the root cause of disparities in birth outcomes. Addressing these social determinants will require working outside the health care domain. The Committee calls for greater support for more place-based initiatives working across multiple sectors—health care, education, economic and community development. Addressing these social determinants will also require working at the policy level, and the Committee recommends inclusion of antipoverty programs, such as Temporary Assistance for Needy Families, as part of the national strategy to address infant mortality.
Currently, HRSA is redesigning its Healthy Start program,32 the largest federal program dedicated to addressing infant mortality in our nation—with six major aims:
improve perinatal health outcomes not only for its clients but for the entire communities it serves (if it is to be truly place-based);
improve women’s health before pregnancy, with a focus on preconception health promotion and reproductive life planning;
promote quality services, with a focus on quality improvement, care coordination and systems integration, and linkage to medical home;
strengthen family resilience, with a focus on strengthening fatherhood and parenting, addressing toxic stress, and supporting trauma-informed care;
achieve collective impact, with a focus on its role in the community as a “backbone” organization working across multiple sectors to support a common agenda, develop shared measurement systems, coordinating mutually reinforcing activities, and facilitating continuous communication33; and
increase accountability.
And if it is better aligned with other early childhood investments, such as the Maternal, Infant, and Early Childhood Home Visiting program; Early Head Start; Head Start; universal preschool; and Women, Infants, and Children, along with other place-based initiatives such as Promise Neighborhood, Choice Neighborhood, and Project Launch, Healthy Start can become a first rung in the ladder of opportunity that will set disadvantaged children and families on a different life course trajectory. From a life course perspective, this type of intergenerational investment is what it will take to stop the transmission of social inequality across generations and to close the infant mortality gap in our nation.
Support Surveillance and Research
The Committee calls for greater investments in adequate data, monitoring, and surveillance systems, focusing on standardizing vital statistics and measurements, improving state capacity for data linkages (e.g., linking Medicaid claims data to vital statistics), and supporting rapid-cycle quality improvement processes with real-time data.
The Committee recognizes the need for more research, but not for more of the same. We need the three Ts: transformative research to help us better understand the developmental origins of social inequality (not only how social inequality gets under the skin but how social inequality gets inside the womb and how social inequality gets transmitted across generations through epigenetic and other mechanisms),34,35 transdisciplinary research that brings researchers out of their disciplinary siloes around a shared conceptual framework,36 and translational research (not only from bench to bedside but more importantly from bedside to curbside and from curbside to policy) that will help accelerate translation of research to practice and policy in addressing disparities in infant mortality.
Maximize Collaboration
We are not going to win this fight against infant mortality by working in siloes. The Committee calls attention to the need to maximize the potential of interagency, public–private and multidisciplinary collaboration. A good example of such collaboration is HRSA’s Collaborative Improvement and Innovation Network, which has accelerated collaborative improvement and innovation across the 13 Southern states by bringing together public and private partners at the federal, state, and local levels in a learning system, complete with shared workspace and a real-time data dashboard, to implement rapid cycles of change to reduce early elective deliveries and promote smoking cessation, safe sleep, perinatal regionalization, and interconception care.23 In 2014 HRSA is planning to scale up the Collaborative Improvement and Innovation Network nationwide.
A healthy start is foundational to the American Dream. The Committee’s recommendations provide a roadmap for our nation not only to improve birth outcomes but also to begin to restore the American Dream for the next generation. (For a full report of the Committee’s recommendations, please visit the HRSA Web site.6)
References
- 1.MacDorman MF, Hoyert DL, Mathews TJ. NCHS data brief. No. 120. Hyattsville, MD: National Center for Health Statistics; 2013. Recent declines in infant mortality in the United States, 2005–2011. [PubMed] [Google Scholar]
- 2.Hamilton BE, Martin JA, Ventura SJ. National Vital Statistics Reports. 3. Vol. 62. Hyattsville, MD: National Center for Health Statistics; 2013. Births: preliminary data for 2012. [PubMed] [Google Scholar]
- 3.Mathews TJ, MacDorman MF. National Vital Statistics Reports. 8. Vol. 61. Hyattsville, MD: National Centers for Health Statistics; 2013. Infant mortality statistics from the 2009 period linked birth/infant death data set. [PubMed] [Google Scholar]
- 4.Sebelius K. A promise renewed pledge signing. Speech at Child Survival Call to Action. 2012 Available at: http://5thbday.usaid.gov/pages/responsesub/Panel4.pdf. Accessed September 29, 2013. [Google Scholar]
- 5.US Department of Health and Human Services. Secretary’s Advisory Committee on Infant Mortality. Available at: http://www.hrsa.gov/advisorycommittees/mchbadvisory/InfantMortality/index.html. Accessed September 29, 2013. [Google Scholar]
- 6.US Department of Health and Human Services. Secretary’s Advisory Committee on Infant Mortality: recommendations for Department of Health and Human Services (HHS) action and framework for a national strategy. 2013 Available at: http://www.hrsa.gov/advisorycommittees/mchbadvisory/InfantMortality/Correspondence/recommendationsjan2013.pdf. Accessed September 29, 2013. [Google Scholar]
- 7.Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: A life-course perspective. Matern Child Health J. 2003;7(1):13–30. doi: 10.1023/a:1022537516969. [DOI] [PubMed] [Google Scholar]
- 8.Lu MC, Kotelchuck M, Hogan V, Jones L, Wright K, Halfon N. Closing the Black-White gap in birth outcomes: a life-course approach. Ethn Dis. 2010;20(1 suppl 2):62–76. [PMC free article] [PubMed] [Google Scholar]
- 9.Lu MC, Tache V, Alexander G, Kotelchuck M, Halfon N. Preventing LBW: is prenatal care the answer? J Matern Fetal Neonatal Med. 2003;13(6):362–380. doi: 10.1080/jmf.13.6.362.380. [DOI] [PubMed] [Google Scholar]
- 10.Lu MC, Kotelchuck M, Hogan VK, Johnson K, Reyes C. Innovative strategies to reduce disparities in the quality of prenatal care in underresourced settings. Med Care Res Rev. 2010;67(5 suppl):198S–230S. doi: 10.1177/1077558710374324. [DOI] [PubMed] [Google Scholar]
- 11.Lu MC. We can do better: improving perinatal health in America. J Womens Health (Larchmt) 2010;19(3):569–574. doi: 10.1089/jwh.2009.1415. [DOI] [PubMed] [Google Scholar]
- 12.Johnson K, Posner SF, Biermann J et al. Select Panel on Preconception Care. Recommendations to improve preconception health and health care—United States. A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm Rep. 2006;55(RR-6):1–23. [PubMed] [Google Scholar]
- 13.Johnson KA. Women’s health and health reform: implications of the Patient Protection and Affordable Care Act. Curr Opin Obstet Gynecol. 2010;22(6):492–497. doi: 10.1097/GCO.0b013e3283404e31. [DOI] [PubMed] [Google Scholar]
- 14.Gee RE, Brindis CD, Diaz A et al. Recommendations of the IOM clinical preventive services for women committee: implications for obstetricians and gynecologists. Curr Opin Obstet Gynecol. 2011;23(6):471–480. doi: 10.1097/GCO.0b013e32834cdcc6. [DOI] [PubMed] [Google Scholar]
- 15.Oshiro BT, Henry E, Wilson J, Branch DW, Varner MW. Decreasing elective deliveries before 39 weeks of gestation in an integrated health care system. Obstet Gynecol. 2009;113(4):804–811. doi: 10.1097/AOG.0b013e31819b5c8c. [DOI] [PubMed] [Google Scholar]
- 16.Tita AT, Landon MB, Spong CY et al. Eunice Kennedy Shriver NICHD Maternal-Fetal Medicine Units Network. Timing of elective repeat cesarean delivery at term and neonatal outcomes. N Engl J Med. 2009;360(2):111–120. doi: 10.1056/NEJMoa0803267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robinson CJ, Villers MS, Johnson DD, Simpson KN. Timing of elective repeat cesarean delivery at term and neonatal outcomes: a cost analysis. Am J Obstet Gynecol. 2010;202(6):632. doi: 10.1016/j.ajog.2010.03.045. e1–e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Donovan EF, Lannon C, Bailit J et al. A statewide initiative to reduce inappropriate scheduled births at 36(0/7)-38(6/7) weeks’ gestation. Am J Obstet Gynecol. 2010;202(3):243. doi: 10.1016/j.ajog.2010.01.044. e1–e8. [DOI] [PubMed] [Google Scholar]
- 19.Oshiro BT, Kowalewski L, Sappenfield W et al. A multistate quality improvement program to decrease elective deliveries before 39 weeks of gestation. Obstet Gynecol. 2013;121(5):1025–1031. doi: 10.1097/AOG.0b013e31828ca096. [DOI] [PubMed] [Google Scholar]
- 20.March of Dimes. Healthy babies are worth the wait. Available at: http://www.marchofdimes.com/professionals/healthy-babies-are-worth-the-wait.aspx. Accessed September 29, 2013. [PubMed] [Google Scholar]
- 21.Association of State and Territorial Health Officials. ASTHO Healthy Babies Initiative. Available at: http://www.astho.org/healthybabies. Accessed September 29, 2013. [Google Scholar]
- 22.Centers for Medicare and Medicaid Services. Strong Start for Mothers and Newborns Initiative. Available at: http://innovation.cms.gov/initiatives/strong-start. Accessed September 29, 2013. [Google Scholar]
- 23.US Department of Health and Human Services. Collaborative Improvement and Innovation Network to reduce infant mortality. Available at: http://mchb.hrsa.gov/infantmortality/coiin. Accessed September 29, 2013. [Google Scholar]
- 24.Boschert S. Maternal safety blueprint outlined. Ob.Gyn. News. July 17, 2013 Available at: http://www.obgynnews.com/news/top-news/single-article/maternal-safety-blueprint-outlined/80ca51a7604a9320b757557e65c0fe88.html. Accessed September 29, 2013. [Google Scholar]
- 25.Langley GL, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nd ed. San Francisco, CA: Jossey-Bass Publishers; 2009. [Google Scholar]
- 26.Lasswell SM, Barfield WD, Rochat RW, Blackmon L. Perinatal regionalization for very low-birth-weight and very preterm infants: a meta-analysis. JAMA. 2010;304(9):992–1000. doi: 10.1001/jama.2010.1226. [DOI] [PubMed] [Google Scholar]
- 27.Barfield WD, Manning SE, Kroelinger C, Martin JA, Barradas DT. Neonatal intensive-care unit admission of infants with very low birth weight–19 states, 2006. MMWR Morb Mortal Wkly Rep. 2010;59(44):1444–1447. [PubMed] [Google Scholar]
- 28.American Academy of Pediatrics Committee on Fetus and Newborn. Levels of neonatal care. Pediatrics. 2012;130(3):587–597. doi: 10.1542/peds.2012-1999. [DOI] [PubMed] [Google Scholar]
- 29.Task Force on Sudden Infant Death Syndrome. Moon RY SIDS and other sleep-related infant deaths: expansion of recommendations for a safe infant sleeping environment. Pediatrics. 2011;128:e1341–e1367. doi: 10.1542/peds.2011-2285. [DOI] [PubMed] [Google Scholar]
- 30.Eunice Kennedy Shriver National Institute of Child Health and Human Development. Safe to Sleep® public education campaign. Available at: http://www.nichd.nih.gov/SIDS/Pages/sids.aspx. Accessed September 29, 2013. [Google Scholar]
- 31.Rotundo G. Centering pregnancy: the benefits of group prenatal care. Nurs Womens Health. 2011;15(6):508–517. doi: 10.1111/j.1751-486X.2011.01678.x. [DOI] [PubMed] [Google Scholar]
- 32.US Department of Health and Human Services. Healthy Start. doi: 10.3109/15360288.2015.1037530. Available at: http://mchb.hrsa.gov/programs/healthystart. Accessed September 29, 2013. [DOI] [PubMed] [Google Scholar]
- 33.Karnia J, Kramer M. Collective impact. Stanford Social Innovation Review. 2011 Available at: http://www.ssireview.org/articles/entry/collective_impact. Accessed September 29, 2013. [Google Scholar]
- 34.Thayer ZM, Kuzawa CW. Biological memories of past environments: epigenetic pathways to health disparities. Epigenetics. 2011;6(7):798–803. doi: 10.4161/epi.6.7.16222. [DOI] [PubMed] [Google Scholar]
- 35.Loi M, Del Savio L, Stupka E. Social epigenetics and equality of opportunity. Public Health Ethics. 2013;6(2):142–153. doi: 10.1093/phe/pht019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stokols D, Misra S, Moser RP, Hall KL, Taylor BK. The ecology of team science: understanding contextual influences on transdisciplinary collaboration. Am J Prev Med. 2008;35(2 suppl):S96–S115. doi: 10.1016/j.amepre.2008.05.003. [DOI] [PubMed] [Google Scholar]