Abstract
Aim:
To explore the signalling pathways involved in aldosterone-induced inflammation and fibrosis in rat vascular smooth muscle cells (VSMCs).
Methods:
Using Western blotting and real-time RT-PCR, we investigated the effects of aldosterone on the expression of cyclooxygenase-2 (Cox-2) and IL-6, two important proinflammatory factors, and TGFβ1, a critical profibrotic factor, in VSMCs.
Results:
Aldosterone treatment significantly increased the expression of Cox-2 and IL-6 and activation of p38MAPK and NF-κB. The expression of both Cox-2 and IL-6 could be blocked by the mineralocorticoid receptor (MR) antagonist spironolactone and the p38MAPK inhibitor SB203580. Also, the rapid phosphorylation of p38MAPK could be suppressed by SB203580 but not by spironolactone, implicating in nongenomic effects of aldosterone. Similar to SB203580 and spironolactone, the NF-κB inhibitor α-p-tosyl-L-lysine chloromethyl ketone (TLCK) markedly attenuated expression of Cox-2, indicating that MR, p38MAPK and NF-κB are associated with aldosterone-induced inflammatory responses. Furthermore, aldosterone enhanced expression of TGFβ1 in rat VSMCs. This result may be related to activation of the MR/ERK-Sp1 signalling pathway because PD98059, an ERK1/2 inhibitor, significantly blocked the rapid phosphorylation of ERK1/2 and function of Sp1 and led to reduced expression of TGFβ1. Spironolactone was also shown to significantly inhibit TGFβ1 and Sp1 expression but not ERK1/2 phosphorylation.
Conclusion:
These results suggest that aldosterone-induced inflammatory responses and fibrotic responses may be mediated by the MR/p38MAPK-NF-κB pathways and the MR/ERK-Sp1 pathways in VSMCs, respectively.
Keywords: aldosterone, inflammation, fibrosis, signal transduction, vascular smooth muscle cells, mineralocorticoid receptor, p38MAPK, NF-κB, ERK1/2, Sp1, nongenomic effect
Introduction
It has recently been recognized that aldosterone can exert direct effects on the vasculature, a non-epithelial tissue, and lead to vascular inflammation, fibrosis, remodelling, and finally cardiovascular diseases1. In hypertensive rats, there is evidence that aldosterone-salt treatment caused obvious coronary inflammatory lesions that were characterized by monocyte and macrophage infiltration and increased expression of cyclooxygenase-2 (Cox-2) and osteopontin. The administration of eplerenone, a selective aldosterone blocker, attenuated vascular and myocardial injury and Cox-2 and osteopontin expression2,3. Meanwhile, eplerenone significantly reduced the aortic expression of IL-β1, IL-6, and tumour necrosis factor alpha (TNF-α), and the mineralocorticoid receptor (MR) antagonist spironolactone prevented aortic collagen accumulation induced by aldosterone in spontaneously hypertensive rats4,5. A more recent study using aortic tissues from aldosterone-treated hypertensive rats further revealed that aldosterone increased vascular inflammatory changes, angiotensin II content, and the expression of angiotensin-converting enzyme, vascular proinflammatory genes (osteopontin, MMP-2, ICAM-1, VCAM-1, PDGF-A, VEGF, and PAI-1) and oxidative stress genes (4-hydroxy-2-neonenal, p47phox, p22phox, and gp91phox), the expression of which were all abolished by eplerenone6. These findings suggest that aldosterone plays an important role in regulating inflammation and fibrosis in the vascular system. But so far, the intracellular signalling mechanisms underlying the aldosterone-induced vascular injury have not been completely elucidated.
Several studies have examined the signalling pathways in vascular cells that regulate the inflammatory/profibrotic effects induced by aldosterone. Jaffe et al reported that aldosterone activates the expression of endogenous genes (collagen types I and III, IL-16 and cytotoxic T-lymphocyte-associated protein 4) via functional MRs in human coronary VSMCs7. Callera et al observed that aldosterone rapidly increases the phosphorylation of p38 MAP kinase (p38MAPK) and extracellular signal-regulated kinase (ERK) and significantly increases NADPH oxidase activity and collagen synthesis in VSMCs from both Wistar-Kyoto rats and spontaneously hypertensive rats, all of which are mediated through c-Src-dependent pathways8,9. Also, Ishizawa et al reported that aldosterone stimulates rat VSMC proliferation via the activation of the big MAP kinase 1 and is not inhibited by cycloheximide10. Recently, two studies demonstrated that in mouse VSMCs, aldosterone-induced activation of ERK1/2, c-Jun NH2-terminal protein kinase (JNK) and nuclear factor (NF)-κB depends on the activity of angiotensin type 1a receptors11, and that the proinflammatory phenotype promoted by aldosterone in aged rat VSMCs is mediated by ERK1/2 and epidermal growth factor receptor-dependent pathways12. These data suggest that intracellular signalling pathway(s) that regulate aldosterone-stimulated vascular effects could involve receptors, protein kinases, nuclear factors, oxidant factors, and other unknown factors.
In the present study, we provide new evidence that aldosterone induces the expression of inflammatory factors, Cox-2 and IL-6 through the MR-p38 and NF-κB pathways and induces expression of transforming growth factor-β1 (TGFβ1), a profibrotic factor, through the MR-ERK1/2 and Sp1 pathways in rat VSMCs.
Materials and methods
Materials
Aldosterone, spironolactone, α-p-tosyl-L-lysine chloromethyl ketone (TLCK), and dimethylsulfoxide (DMSO) were purchased from Sigma-Aldrich Corporation (St Louis, MO, USA); SB203580 (SB) and PD98059 (PD) were from Calbiochem (Darmstadt, Germany). A stock solution of each compound was dissolved in DMSO, aliquoted and stored at -20 °C. Mouse anti-Cox-2, mouse anti-phospho-p38MAPK, mouse anti-p38MAPK, mouse anti-NF-κB p65, rabbit anti-phospho-ERK1/2, rabbit anti-ERK1/2, rabbit anti-Sp1, rabbit anti-actin, biotinylated secondary antibodies, and HRP-conjugated streptavidin, were all obtained from Santa Cruz (Santa Cruz, CA, USA).
Cell culture
Rat VSMCs were maintained in 75-cm2 tissue culture flasks in DMEM containing 10% fetal bovine serum, 100 IU/mL penicillin, and 100 IU/mL streptomycin at 37 °C with 95% air and 5% carbon dioxide. The cells were grown to 75% confluence and treated with vehicle or aldosterone at serial concentrations from 10−9 to 10−6 mol/L for the times indicated. Twenty four hours before the treatment, the medium was replaced with medium containing 0.4% serum. For the inhibitor studies, SB at 2×10−5 mol/L, PD at 5×10−5 mol/L, TLCK at 10−4 mol/L, or spironolactone at 5×10−5 mol/L was added to the culture medium 1 h prior to the addition of aldosterone.
Western blot analyses of Cox-2, p38MAPK, and ERK1/2 proteins
At the end of the treatment, the cells were washed with ice-cold PBS twice and lysed with 80–100 μL of the following buffer: Tris-HCl [50 mmol/L (pH 8.0)], NaCl (150 mmol/L), SDS (0.1%), PMSF (100 μg/mL), aprotinin (1 μg/mL), Nonidet P-40 (1%). The lysates were frozen with liquid nitrogen and then thawed in water at 37 °C three times, and centrifuged at 15 000×g for 10 min. The protein concentration of the supernatant was determined by the Lowry method using bovine serum albumin as the standard. The proteins (20–40 μg) were separated by SDS-PAGE on an 8% separating gel and 5% stacking gel for Cox-2 or 10% separating gels for p38 and ERK1/2, blotted onto PDVF membranes, incubated in a blocking buffer (5% non-fat, dried milk and 0.05% Tween-20 in PBS), and then incubated with the primary antibodies (at a 1:1000 dilution), biotinylated secondary antibodies (1:2000 dilution), and HRP-conjugated streptavidin (1:2000 dilution). The protein bands were visualized with enhanced chemiluminescence (ECL, Beijing Pulilai Company, Beijing, China) according to the manufacturer's instructions.
Western blot analysis of NF-κB and Sp1 proteins
Two steps were taken to extract the NF-κB and Sp1 proteins from the cytoplasm and nucleoplasm, respectively. After being washed with ice-cold PBS, the cells were lysed with 150 μL of buffer A, which consists of HEPES [10 mmol/L (pH 7.9)], KCl (10 mmol/L), and EDTA (0.1 mmol/L). Just before use, PMSF (0.5 mmol/L), DTT (1 mmol/L), and 1 μL of protease inhibitors (including leupeptin, aprotinin, and pepstatin) (10 μg/mL) were added, incubated for 10 min at room temperature, then scraped and centrifuged at 15 000×g for 3 min. The supernatant (cytoplasmic fraction) was collected, aliquoted and stored at -86 °C. The pellet was resuspended with 150 μL of buffer B: HEPES [20 mmol/L, (pH 7.9)], NaCl (0.4 mol/L), EDTA (1 mmol/L), and glycerol (10%). Before use, PMSF (0.5 mmol/L), DTT (1 mmol/L), and 1 μL of each protease inhibitor (leupeptin, aprotinin, and pepstatin, 10 μg/mL) was added to buffer B. The resuspended solution was shaken vigorously at 4 °C for 2 h then centrifuged at 15 000×g for 5 min. The supernatant (nucleoplasmic fraction) was collected, aliquoted and stored at -86 °C.
The protein concentrations of the cytoplasmic and nucleoplasmic extracts were quantitated. The proteins were electrophoresed on 10% separating gels and analysed by the same methods described above.
Densitometric analysis
The density of the bands on the Western blots was quantified by scanning densitometry (LAS-3000 Fujifilm and Kodak Digital Science 1D software) and expressed as the normalized values to actin.
Real-time quantitative reverse-transcription polymerase chain reaction analyses of IL-6 and TGFβ1 mRNA levels
The total RNA from rat VSMCs was extracted according to the TRIzol reagent protocol (Invitrogen). Two micrograms of total RNA was reverse transcribed in a MyCycler (BioRad) in a 25-μL reaction volume containing 1 μL Moloney murine leukemia virus reverse transcriptase (5 IU/mL), 0.5 μL RNAsin (40 IU/mL), 2.5 μL deoxynucleotide triphosphate (10 mmol/L), 5 μL 5×PCR buffer, 2.5 μL Oligo dT (0.5 μg/μL), and diethylpyrocarbonate-water added to the final volume. The resulting cDNA was amplified and quantified by real-time RT-PCR (PRISM-7000, ABI) in a 10-μL reaction volume containing 1 μL cDNA (RT product), 5 μL 2×mixture, 0.2 μL of the sense primer (20 pmol/L), 0.2 μL of the antisense primer (20 pmol/L), 0.2 μL 50× SYBR Green I (Invitrogen), and 3.4 μL double distilled water. The primers and reaction conditions were as follows: IL-6, sense 5′-AGGAACGAAAGTCAACTCCATCTG-3′ antisense 5′-GGCAGTGGCTGTCAACAACATC-3, product size 111 bp; β-actin, sense 5′-CAGCGGAACCGCTCATTGCCAATGG-3′, antisense 5′-TCACCCACACTGTGCCATCTACG-3′, product size, 360 bp; TGFβ1, sense 5′-GCTAATGGTGGACCGCAACAAC-3′, antisense 5′-CACTGCTTCCCGAATGTCTGAC-3′, product size, 122 bp; GAPDH, sense 5′-TGGAGTCTACTGGCGTCTTCAC-3′, antisense 5′-ATGAGCCCTTCCACGATGC-3′, product size, 238 bp; reaction conditions: activation of enzymes at 50 °C for 5 min, one cycle of denaturation at 95 °C for 5 min; 42 cycles of denaturation at 95 °C for 15 s, primer annealing at 60 °C for 31 s, primer extension at 72 °C for 30 s; then dissociation curves at 95 °C for 0 min, 65 °C for 15 s, and 4 °C for 1 min. The IL-6 and TGFβ1 mRNA levels were normalized to the β-actin and GAPDH mRNA amounts, respectively. The results are expressed as the fold of control.
Statistical analysis
All values are expressed as the mean±SD. The data were analysed using the Student's t test. A P<0.05 was accepted as statistically significant.
Results
Aldosterone induces the expression of Cox-2 protein and IL-6 mRNA in VSMCs
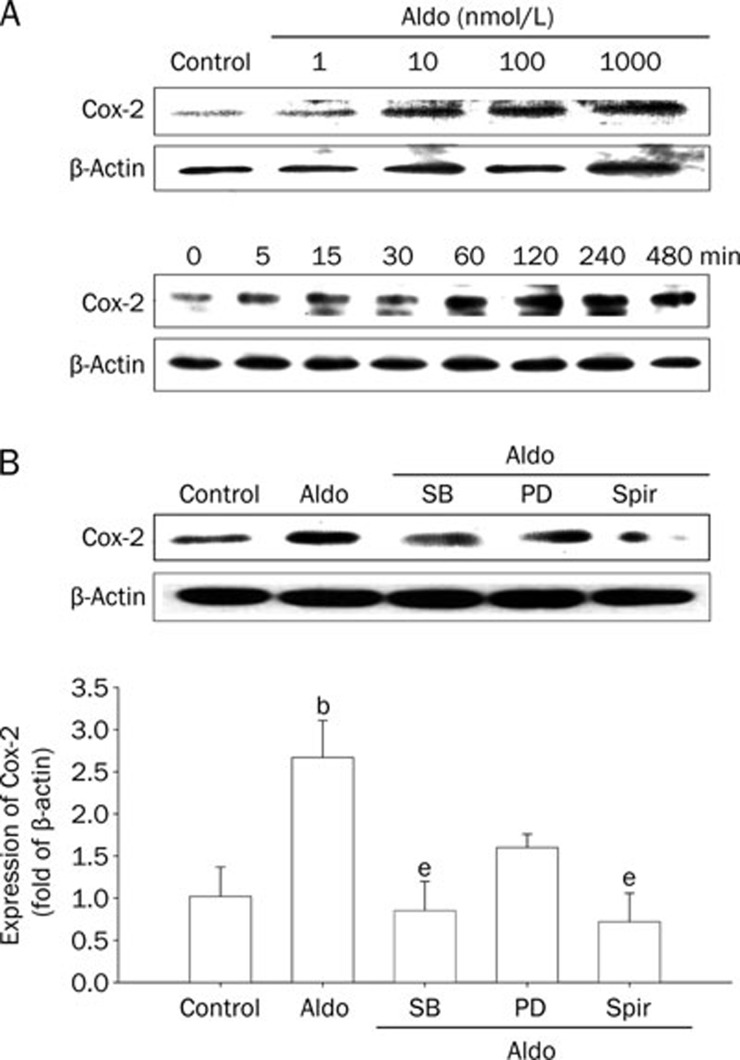
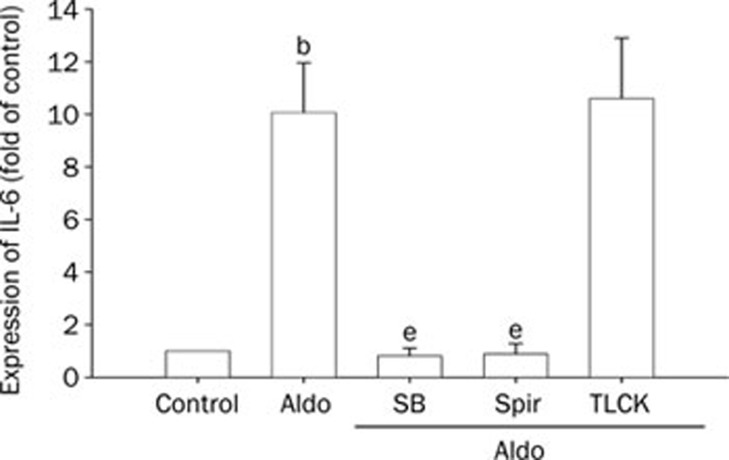
In rat VSMCs, aldosterone induced the expression of Cox-2 protein in a concentration- and time-dependent manner, from 1 to 1000 nmol/L and 30 min to 2 or 4 h, respectively (Figure 1A). Aldosterone treatment also significantly enhanced IL-6 mRNA levels by 10-fold over the control group (Figure 2). These activities were blocked by the MR antagonist spironolactone and the p38MAPK inhibitor SB203580, but not by the ERK1/2 inhibitor PD98059, although PD98059 did reduce the levels to a certain extent (Figure 1B and 2). TLCK had no inhibitory effects on IL-6 mRNA expression. These data suggest that aldosterone potentially elicits vascular inflammatory responses through the MR and protein kinase system.
Figure 1.
The expression of cyclooxyenase 2 (Cox-2) in rat vascular smooth muscle cells (VSMCs) induced by aldosterone (Aldo). (A) Upper panel, the concentration-dependent increase in Cox-2 expression induced by Aldo for 4 h. Lower panel, the time-related increase in Cox-2 expression induced by Aldo (0.1 μmol/L) for the indicated times. (B) The effects of different inhibitors on Cox-2 expression induced by Aldo. The cells were pretreated with SB203580 (SB, 20 μmol/L), PD98059 (PD, 50 μmol/L), and spironolactone (Spir, 50 μmol/L) for 1 h, then stimulated by Aldo (0.1 μmol/L) for 4 h. The cell lysates were analysed by Western blotting with specific antibodies. Mean±SD. n=3. bP<0.05 vs control. eP<0.05 vs Aldo.
Figure 2.
The expression of IL-6 in VSMCs induced by aldosterone (Aldo). The cells were pretreated with SB203580 (SB, 20 μmol/L), spironolactone (Spir, 50 μmol/L) and TLCK (100 μmol/L) for 1 h, then stimulated with Aldo (0.1 μmol/L) for 7 h. The cell lysates were analysed by real time RT-PCR. Mean±SD. n=3. bP<0.05 vs control. eP<0.05 vs Aldo.
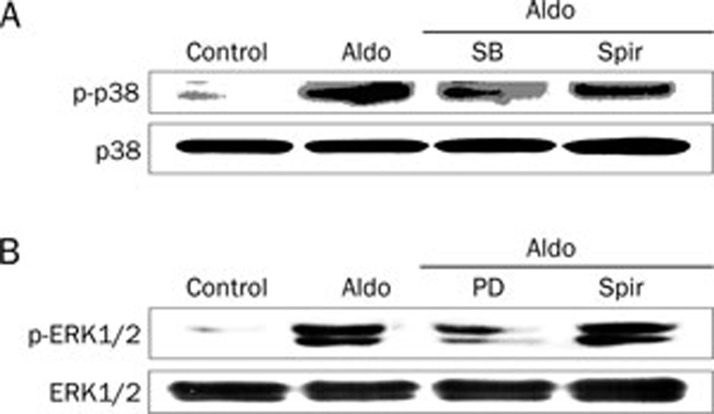
Aldosterone increases the phosphorylation of p38MAPK
SB203580 could significantly down-regulate the expression of Cox-2 and IL-6, implying that p38MAPK is involved in the inflammatory responses induced by aldosterone. Incubation of cultured VSMCs with aldosterone for 15 or 30 min markedly enhanced the phosphorylation of p38MAPK, which was obviously suppressed by SB203580 but not spironolactone (Figure 3A), suggesting that MAPKs are involved in the signal transduction of direct vascular effects (nongenomic effects) induced by aldosterone.
Figure 3.
Aldosterone (Aldo) stimulates the phosphorylation of p38MAPK (A) and ERK1/2 (B) in VSMCs. The cells were pretreated with SB203580 (SB, 20 μmol/L), PD98059 (PD, 50 μmol/L), and spironolactone (Spir, 50 μmol/L) for 1 h, then stimulated with Aldo (0.1 μmol/L) for 30 min. The cell lysates were analysed by Western blotting with specific antibodies.
Aldosterone stimulates NF-κB p65 expression
The role of the proinflammatory transcription factor NF-κB in the inflammatory responses induced by aldosterone was investigated. After the administration of aldosterone to VSMCs for 4 h, both the cytoplasmic and nucleoplasmic extracts were prepared, and the amount of NF-κB p65 protein was determined by Western blot analysis. As shown in Figure 4, the expression of p65 was almost undetectable in the cytoplasm but was expressed 6.7-fold over the control in the nucleoplasm, even after aldosterone stimulation, indicating that NF-κB mediates the inflammatory responses of aldosterone.
Figure 4.
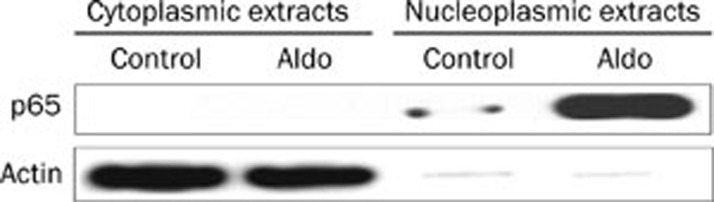
The expression of NF-κB p65 in the cytoplasmic and nucleoplasmic extracts from rat VSMCs induced by aldosterone (Aldo). The cells were stimulated by Aldo for 4 h. The cytoplasmic and nucleoplasmic extracts were separated by SDS-PAGE and were analysed by Western blotting with specific antibodies.
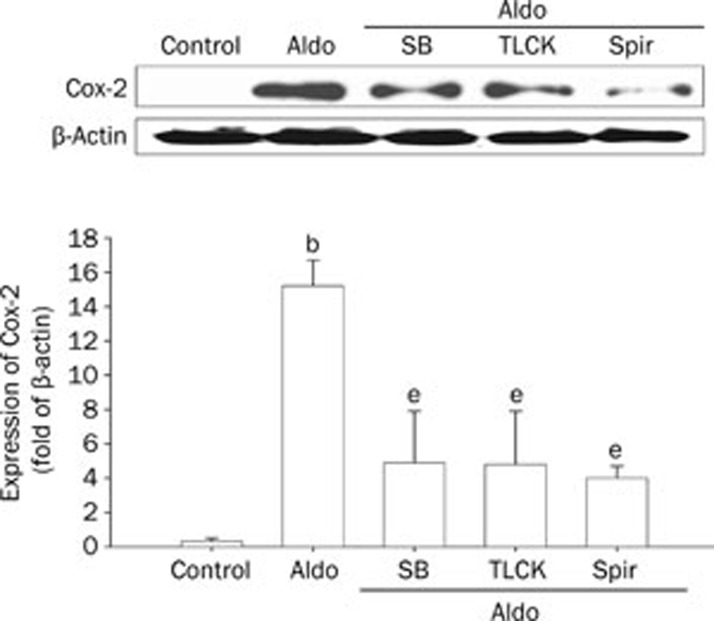
Inhibition of NF-κB and p38MAPK activities stimulated by aldosterone
Further studies revealed that pretreating cells with TLCK, a serine proteinase inhibitor of NF-κΒ, could significantly block Cox-2 protein expression induced by aldosterone in cultured VEMCs. Similar results were obtained using the p38MAPK inhibitor SB203580 and the MR receptor blocker spironolactone (Figure 5). The results suggest that aldosterone-induced inflammatory effects could be mediated through a MR-p38MAPK-NF-κΒ pathway.
Figure 5.
The inhibition of p38MAPK and NF-κB activities stimulated by aldosterone (Aldo) in rat VSMCs. The cells were pretreated with SB203580 (SB, 20 μmol/L), TLCK (100 μmol/L), and spironolactone (Spir, 50 μmol/L) for 1 h, then stimulated with Aldo (0.1 μmol/L) for 4 h. The cell lysates were analysed by Western blotting with specific antibodies. Mean±SD. n=3. bP<0.05 vs control. eP<0.05 vs Aldo.
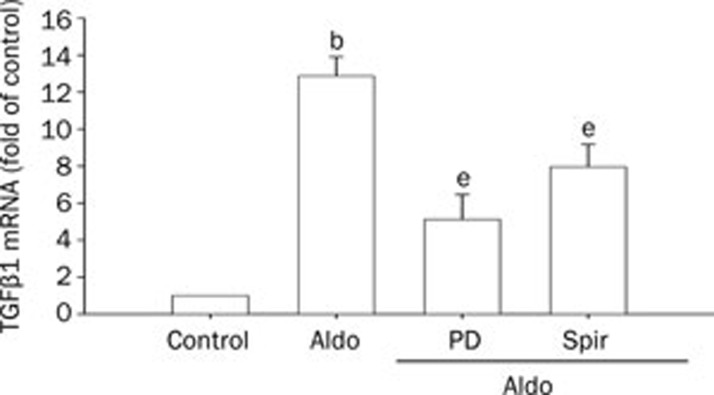
Aldosterone induces the expression of TGFβ1 mRNA
Aldosterone-stimulated inflammation probably results in fibrosis in vascular tissues. Thus, the mRNA expression of the profibrotic molecule TGFβ1 in rat VSMCs was investigated using quantitative real-time RT-PCR. As shown in Figure 6, aldosterone treatment increased the levels of TGFβ1 mRNA. This effect was significantly reduced by the ERK1/2 inhibitor PD98059 and the MR receptor antagonist spironolactone, suggesting that ERKs and MR have a role in the profibrotic effects of aldosterone.
Figure 6.
Aldosterone (Aldo) induces the expression of TGFβ1 mRNA in rat VSMCs. The cells were pretreated with PD98059 (PD, 50 μmol/L) or spironolactone (Spir, 50 μmol/L) for 1 h, then stimulated with Aldo (0.1 μmol/L) for 7 h. The cell lysates were analysed by real time RT-PCR. Mean±SD. n=3. bP<0.05 vs control. eP<0.05 vs Aldo.
Aldosterone increases the phosphorylation of ERK1/2
Incubation of cultured VSMCs with aldosterone for 15 or 30 min markedly increased not only the phosphorylation of p38MAPK but also ERK1/2. The phosphorylation of ERK1/2 was strongly blocked by PD98059, while spironolactone had no effect (Figure 3B), implying it was rapid, nongenomic effects of aldosterone. These data further demonstrate that MAPKs have a role in the proinflammatory and profibrotic effects of aldosterone.
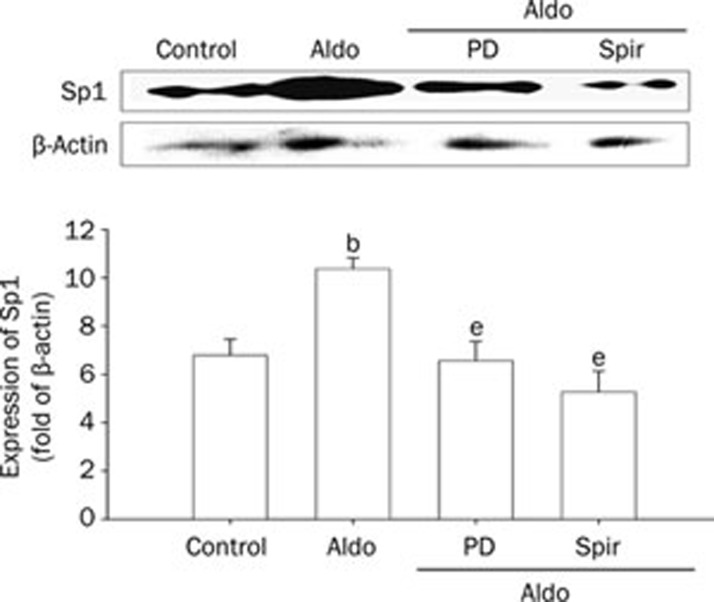
Aldosterone stimulates Sp1 expression in the nucleoplasm
The role of Sp1, a nuclear transcription factor, in profibrotic responses induced by aldosterone was also studied. As shown in Figure 7, aldosterone significantly increased Sp1 expression in the nucleoplasm, and this effect was blocked by PD98059 and spironolactone, which is similar to their effect on inhibiting TGFβ1 expression (Figure 6). These results indicate that the profibrotic effects of aldosterone could be associated with the MR-ERKs-Sp1 pathway.
Figure 7.
Aldosterone (Aldo) stimulates Sp1 protein expression in rat VCMCs. The cells were pretreated with PD98059 (PD, 50 μmol/L), and spironolactone (Spir, 50 μmol/L) for 1 h, then stimulated with Aldo (0.1 μmol/L) for 30 min. Nucleoplasmic extracts were separated by SDS-PAGE and analysed by Western blotting with specific antibodies. Mean±SD. n=3. bP<0.05 vs control. eP<0.05 vs Aldo.
Discussion
In this study, we showed that aldosterone stimulation caused inflammatory responses in rat VSMCs and resulted in the enhanced expression of the inflammatory factors Cox-2 and IL-6. This effect was attenuated by the MR antagonist spironolactone (Figures 1 and 2). These results are consistent with previous reports demonstrating that aldosterone treatment in uninephrectomized rats elevated the levels of Cox-2 mRNA and coronary inflammatory lesions; these vascular inflammatory responses were reduced by the aldosterone blocker eplerenone2,3. The results indicated that the MR was part of the signalling pathway involved in the inflammatory responses induced by aldosterone. Further studies in our laboratory have demonstrated that aldosterone has two different effects: (1) phosphorylation of p38MAPK (rapid, nongenomic effect), which was suppressed by SB203580 but not by spironolactone (Figure 3), implying that the MR does not mediate this effect; (2) activation and nuclear translocation of NF-κB p65 (delayed genomic effect; Figure 4). In VSMCs, the activation of both p38MAPK and NF-κB might result in the production of chemokines and inflammatory cytokines1,13. Indeed, we observed a significant increase in the expression of Cox-2 and IL-6 (Figure 5). Furthermore, in spontaneously hypertensive rats, aldosterone up-regulated NF-κB p50 expression and down-regulated IκB mRNA expression. This effect was accompanied by the enhanced expression of cytokines (such as IL-1β, IL-6, and TNF-α)4. Similarly, in VSMCs from both Wistar-Kyoto rats and spontaneously hypertensive rats, aldosterone-induced phosphorylation of the protein tyrosine kinase c-Src, results in the amplification of NAD(P)H-mediated generation of reactive oxygen species (ROS) and leads to the activation of ROS-sensitive transcription factors, such as NF-κB and activation protein-1 (AP-1), recruitment of inflammatory cells and elaboration of inducible NO synthase (iNOS), and, consequently, vascular damage8,9,10. Therefore, protein kinases (p38MAPK, Src) and transcription factors (NF-κB, AP-1) are two elements of the signalling pathway that mediate the inflammatory responses of aldosterone. Recent studies using siRNA in mouse VSMCs revealed that the activation of NF-κB requires not only the MR but also the AT1 receptor11. The data from this study demonstrated that the aldosterone-induced expression of inflammatory factors (Cox-2) could be significantly reduced by the MR blocker spironolactone, the p38 MAPK inhibitor SB203580, and the NF-κB inhibitor TLCK (Figure 5), indicating that the MR-p38MAPK-NF-κB signalling pathway mediates the inflammatory responses induced by aldosterone. In this signalling pathway, the activation of p38MAPK may not require the MR because spironolactone did not inhibit phosphorylation of p38 MAPK (Figure 3). This result may be due to the direct, nongenomic effects of aldosterone, which may facilitate classical MR-mediated effects1.
It is known that aldosterone induces fibrosis in rat heart and blood vessels14, and spironolactone prevents aortic collagen accumulation in spontaneously hypertensive rats5,15. These data imply that the MR is involved in vascular fibrosis, but the underlying, detailed molecular mechanism has not been completely elucidated. In the present study, we observed the effects of aldosterone on the profibrotic molecule TGFβ1 in rat VMSCs. Our data show that the incubation of VSMCs with aldosterone significantly increased the expression of TGFβ1 mRNA, which was then inhibited by spironolactone and PD98059 (Figure 5), implying that ERK1/2 is also involved in vascular fibrosis. Similar results were reported by Kobayashi et al14 in Dahl salt-sensitive hypertensive rats. In that study, treating the animals with eplerenone significantly decreased the phosphorylation of protein kinase C (PKC)βII, c-Src, ERK1/2, and p70S6 kinase (p70S6K), as well as the expression of TGFβ1 and type I collagen mRNA and protein, which suggests that aldosterone-induced profibrotic effects could be mediated through the PKCβII-c-Src (upstream regulator)-ERK1/2-p70S6K (downstream effector) pathway. Furthermore, studies by Callera et al8,9 in VSMCs from spontaneously hypertensive rats demonstrated that aldosterone stimulation could enhance the phosphorylation of c-Src and MAPKs, and the incorporation of 3H]-proline, a marker of collagen synthesis, and stimulatory effects of aldosterone on collagen synthesis was inhibited by PP2 (c-Src inhibitor) and SB212190 (p38MAPK inhibitor), confirming that the vascular profibrotic actions of aldosterone could be mediated through the c-Src/MAPK signalling pathways. Additionally, it was reported that the epidermal growth factor receptor (EGFR) could be involved in mediating the profibrotic responses of aldosterone because the EGFR is involved in the development of fibrosis and vascular dysfunction16,17, and aldosterone-induced stimulation of ERK1/2 in VSMCs is dependent on the EGFR18. In this study, our data also show that aldosterone could induce rapid phosphorylation of ERK1/2 in rat VSMCs, which was suppressed by PD98059 but not spironolactone, implying that aldosterone has nongenomic effects (Figure 3). Moreover, spironolactone and PD98059 inhibited the enhanced expression of TGFβ1 mRNA and Sp1 protein, suggesting that the MR-ERKs-Sp1 pathway could mediate aldosterone-activated profibrotic responses in rat VSMCs.
Taken together, our studies provide new evidence on the proinflammatory and profibrotic effects of aldosterone (including genomic and nongenomic effects) that are mediated through the MR-MAPKs (ERK1/2, p38MAPK), transcription factors (Sp1, NF-κB) signalling pathways. Regulating the aldosterone-induced effects through these factors will potentially reduce vascular remodelling and damage. This effect could be beneficial and effective in the treatment of cardiovascular diseases.
Author contribution
Zhuo-wei HU directed the research; Chuan-jiang ZHU conducted the research and wrote and revised the manuscript; Qing-qing WANG, Jun-lan ZHOU, and Han-zhi LIU assisted with the experiments; Fang HUA and Hong-zheng YANG gave some technical support for the research.
Acknowledgments
This work was supported by National Natural Science Foundation of China (No 30472025).
References
- Gilbert KC, Brown NJ. Aldosterone and inflammation. Curr Opin Endocrinol Diabetes Obes. 2010;17:199–204. doi: 10.1097/med.0b013e3283391989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocha R, Rudolph AE, Frierdich GE, Nachowiak DA, Kekec BK, Blomme EA, et al. Aldosterone induces a vascular inflammatory phenotype in the rat heart. Am J Physiol Heart Circ Physiol. 2002;283:H1802-10. doi: 10.1152/ajpheart.01096.2001. [DOI] [PubMed] [Google Scholar]
- Rocha R, Martin-Berger CL, Yang P, Scherrer R, Delyani J, McMahon E. Selective aldosterone blockade prevents angiotensin II/salt-induced vascular inflammation in the rat heart. Endocrinology. 2002;143:482–836. doi: 10.1210/en.2002-220120. [DOI] [PubMed] [Google Scholar]
- Sanz-Rosa D, Cediel E, de las Heras N, Miana M, Balfagon G, Lahera V, et al. Participation of aldosterone in the vascular inflammatory response of spontaneously hypertensive rats: role of the NFkappaB/IkappaB system. J Hypertens. 2005;23:116–772. doi: 10.1097/01.hjh.0000170379.08214.5a. [DOI] [PubMed] [Google Scholar]
- Benets A, Lacolley P, Safar ME. Prevention of aortic fibrosis by spironolactone in spontaneously hypertension rats. Arteriosclerosis. 1997;17:1152–6. doi: 10.1161/01.atv.17.6.1152. [DOI] [PubMed] [Google Scholar]
- Hirono Y, Yoshimoto T, Suzuki N, Sugiyama T, Sakurada M, Takai S, et al. Angiotensin II receptor type 1-mediated vascular oxidative stress and proinflammatory gene expression in aldosterone-induced hypertension: the possible role of local rennin-angiotensin system. Endocrinology. 2007;148:1688–96. doi: 10.1210/en.2006-1157. [DOI] [PubMed] [Google Scholar]
- Jaffe IZ, Mendelsohn ME. Angiotensin II and aldosterone regulate gene transcription via functional mineralocorticoid receptors in human coronary artery smooth muscle cells. Circ Res. 2005;96:643–50. doi: 10.1161/01.RES.0000159937.05502.d1. [DOI] [PubMed] [Google Scholar]
- Callera GE, Touyz RM, Tostes RC, Yogi A, He Y, Malkinson S, et al. Aldosteone activates vascular p38MAP kinase and NADPH oxidase via c-Src. Hypertension. 2005;45:773–9. doi: 10.1161/01.HYP.0000154365.30593.d3. [DOI] [PubMed] [Google Scholar]
- Callera GE, Montezano AC, Yogi A, Tostes RC, He Y, Schiffrin EL, et al. c-Src-dependent nongenomic signaling responses to aldosterone are increased in vascular myocytes from spontaneously hypertensive rats. Hypertension. 2005;46:1032–8. doi: 10.1161/01.HYP.0000176588.51027.35. [DOI] [PubMed] [Google Scholar]
- Ishizawa K, Izawa Y, Ito H, Miki C, Miyata K, Fujita Y, et al. Aldosterone stimulates vascular smooth muscle cell proliferation via big mitogen-activated protein kinase 1 activation. Hypertension. 2005;46:1046–52. doi: 10.1161/01.HYP.0000172622.51973.f5. [DOI] [PubMed] [Google Scholar]
- Lemarié CA, Simeone SM, Nikonova A, Ebrahimian T, Deschênes ME, Coffman TM, et al. Aldosterone-induced activation of signaling pathways requires activity of angiotensin type 1a receptors. Circ Res. 2009;105:852–9. doi: 10.1161/CIRCRESAHA.109.196576. [DOI] [PubMed] [Google Scholar]
- Krug AW, Allenhöfer L, Monticone R, Spinetti G, Gekle M, Wang M.et al. Elevated mineralocorticoid receptor activity in aged rat vascular smooth muscle cells promotes a proinflammatory phenotype via extracellular signal-regulated kinase 1/2 mitogen-activated protein kinase and epidermal growth factor receptor-dependent pathways Hypertension 2010551476–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukundan L, Milhorn DM, Matta B, Suttles J. CD40-mediated activation of vascular smooth muscle cell chemokine production through a Src-initiated, MAPK-dependent pathway. Cell Signal. 2004;16:375–84. doi: 10.1016/j.cellsig.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Kobayashi N, Yoshida K, Nakano S, Ohno T, Honda T, Tsubokou Y, et al. Cardioprotective mechanisms of eplerenone on cardiac performance and remodeling in failing rat hearts. Hypertension. 2006;47:671–9. doi: 10.1161/01.HYP.0000203148.42892.7a. [DOI] [PubMed] [Google Scholar]
- Park JB, Schiffrin EL. Cardiac and vascular fibrosis and hypertrophy in aldosterone-infused rats: role of endothelin-1. Am J Hypertens. 2002;15:164–9. doi: 10.1016/s0895-7061(01)02291-9. [DOI] [PubMed] [Google Scholar]
- Grossmann C, Krug AW, Freudinger R, Mildenberger S, Voelker K, Gekle M. Aldosterone-induced EGFR expression: interaction between the human mineralocorticoid receptor and the human EGFR promoter. Am J Physiol Endocrinol Metab. 2007;292:E1790–800. doi: 10.1152/ajpendo.00708.2006. [DOI] [PubMed] [Google Scholar]
- Flamant M, Tharaux PL, Placier S, Henrion D, Coffman T, Chatziantoniou C, et al. Epidermal growth factor receptor trans-activation mediates the tonic and fibrogenic effects of endothelin in the aortic wall of transgenic mice. FASEB J. 2003;17:327–9. doi: 10.1096/fj.02-0115fje. [DOI] [PubMed] [Google Scholar]
- Mazak I, Fiebeler A, Muller DN, Park JK, Shagdarsuren E, Lindschau C, et al. Aldosterone potentiates angiotensin II-induced signaling in vascular smooth muscle cells. Circulation. 2004;109:2792–800. doi: 10.1161/01.CIR.0000131860.80444.AB. [DOI] [PubMed] [Google Scholar]