Abstract
Globally, health worker shortages continue to plague developing countries. Community health workers are increasingly being promoted to extend primary health care to underserved populations. Since 2004, Healthy Child Uganda (HCU) has trained volunteer community health workers in child health promotion in rural southwest Uganda. This study analyses the retention and motivation of volunteer community health workers trained by HCU. It presents retention rates over a 5-year period and provides insight into volunteer motivation. The findings are based on a 2010 retrospective review of the community health worker registry and the results of a survey on selection and motivation. The survey was comprised of qualitative and quantitative questions and verbally administered to a convenience sample of project participants. Between February 2004 and July 2009, HCU trained 404 community health workers (69% female) in 175 villages. Volunteers had an average age of 36.7 years, 4.9 children and some primary school education. Ninety-six per cent of volunteer community health workers were retained after 1 year (389/404), 91% after 2 years (386/404) and 86% after 5 years (101/117). Of the 54 ‘dropouts’, main reasons cited for discontinuation included ‘too busy’ (12), moved (11), business/employment (8), death (6) and separation/divorce (6). Of 58 questionnaire respondents, most (87%) reported having been selected at an inclusive community meeting. Pair-wise ranking was used to assess the importance of seven ‘motivational factors’ among respondents. Those highest ranked were ‘improved child health’, ‘education/training’ and ‘being asked for advice/assistance by peers’, while the modest ‘transport allowance’ ranked lowest. Our findings suggest that in our rural, African setting, volunteer community health workers can be retained over the medium term. Community health worker programmes should invest in community involvement in selection, quality training, supportive supervision and incentives, which may promote improved retention.
Keywords: Community health worker, retention, motivation, volunteer
KEY MESSAGES.
In a rural African setting, volunteer community health workers can be retained over the medium term.
Within our setting and programme, community health worker motivation stems primarily from perceived improvements in health outcomes, training opportunities and being a valued asset in the community rather than from financial incentives.
Introduction
Globally, health worker shortages represent a serious constraint for health systems. ‘Task-shifting’ and mobilization of community health workers are increasingly being promoted to extend primary health care to underserved populations in resource-poor settings (WHO et al. 2008; East, Central and Southern Health Community 2010; Nabudere et al. 2010; Fulton et al. 2011; Dambisya and Matinhure 2012). Community health workers are a cadre of local community members who receive short training to conduct health education and sometimes treat illness; they may or may not be remunerated (Lehmann 2007). The use of community health workers holds tremendous potential to extend access to very basic health care in Sub-Saharan Africa where the population is mainly rural, health indicators are poor, and health worker shortages and financing constraints are immense. Evidence for community health worker effectiveness in improving child health is growing. Extensive community health worker programmes are being scaled-up throughout Sub-Saharan Africa (Canadian International Development Agency 2010), including in Uganda where the Ministry of Health has begun rolling out its national village health team strategy (Nsungwa-Sabiiti et al. 2004; Nsabagasani et al. 2007; Uganda Ministry of Health et al. 2010).
The challenge of motivating, and in turn, retaining community health workers is of paramount importance as poor motivation and high drop-out rates can impact programme effectiveness, cost and sustainability (Khan et al. 1998; Bhattacharyya et al. 2001; Shrestha 2003; Standing and Chowdhury 2008; Rahman et al. 2010; World Health Organization and Global Health Workforce Alliance 2010). Some authors suggest attrition is higher, especially in large-scale programmes, when workers are not paid (Gilson et al. 1989; Walt et al. 1989; Bhattacharyya et al. 2001; Lehmann 2007), while others question the ethics of using volunteer labour in very poor communities (Maes et al. 2010). However, volunteerism in developing countries remains poorly understood (Dingle 2001). While the World Health Organization is encouraging greater financial remuneration of community health workers as a means of improving motivation and retention (WHO et al. 2008; World Health Organization and Global Health Workforce Alliance 2010), the resources required, even for minimal remuneration, may not be available in resource-constrained countries.
Despite the ongoing debate on financial remuneration, retention rates and incentives in volunteer and non-volunteer programmes have not been well documented (Bhattacharyya et al. 2001; Lehmann 2007; Nkonki et al. 2011). Recently though, some countries with large community health worker programmes have begun to undertake systematic reviews (Sunkutu and Nampanya-Serpell 2009). While it is difficult to assess programmes by comparing numbers alone, retention rates—in those studies that have published results—have varied greatly from 23 to 97% (Nkonki et al. 2011). Published rates include 66% community health worker retention after 11 months in an HIV/AIDS home care programme in western Kenya (Olang’o et al. 2010); 43% in a government programme in Kalabo District, Zambia (Stekelenburg et al. 2003); 97% in a volunteer programme managed by BRAC (formerly Bangladesh Rural Advancement Committee) during the 1990s (Standing and Chowdhury 2008), but only 55% over 3 years in a different maternal and newborn health trial in the Sylhet District of Bangladesh that paid comparatively high salaries (Rahman et al. 2010); ∼70% over 9 months among unpaid volunteers in Sine Saloum, Senegal and ∼50% over 2 years in a national volunteer community health worker programme in Niger (Parlato and Favin 1982). Understanding the apparently large variance in retention across programmes is constrained by the limited number of studies that document retention data in general and the virtual absence of studies that present data disaggregated by attrition type (i.e. resignation, relocation and termination) (Nkonki 2011) or systematically track retention against different packages of incentives (Bhattacharyya 2001).
The main objectives of this study are to (1) examine retention data in detail (including rates and reasons for attrition) for volunteer community health workers trained by Healthy Child Uganda (HCU) and (2) assess factors related to community health worker selection and motivation. HCU was established in 2004 as a Ugandan–Canadian university partnership aiming to promote child health in rural southwestern Uganda through education and training of volunteer community health workers. A recent 3-year impact evaluation of HCU demonstrated significant reductions in reported child deaths, as well as decreases in malaria, diarrhoea and underweight status of children (Brenner et al. 2011).
Methods
Study setting and population
From 2004 to 2009, HCU trained 404 volunteer community health workers (279 females, 69%) to conduct child health promotion in Mbarara and Bushenyi Districts in southwest Uganda. The project reached 175 villages in 18 parishes, covering a total population of 95 000 people. Villages are clustered together into administrative groupings known as ‘parishes’. An average village has a population of 450, of whom ∼20% are under 5 years of age. Most communities are remote, with poor access to health care and very poor baseline child health indicators (Uganda Ministry of Health et al. 2010).
Intervention
Community health workers were selected and trained in two main cohorts: Phase I (February–March 2004) was initiated in 6 parishes (57 villages); Phase II (March 2006–January 2008) involved 12 additional parishes (118 villages). Each community health worker served on average 25 households and 45 children under 5 years of age.
Selection
Community health worker selection is intended to encourage broad community participation. Community leaders organized village meetings where project representatives provided a clear description of community health worker volunteer roles and expectations. Building on suggested criteria (at least one female, possess voluntary spirit and be parents of young children), community members subsequently developed their own criteria and determined the process for selecting individuals to be trained.
Training and supervision
Government health staff trained by HCU led 5-day introductory training workshops and subsequent 2-day annual refresher workshops on basic child health promotion, prevention and assessment of sick children, as well as community facilitation and counselling skills. Health centre trainers met teams of community health workers monthly for reporting and refresher training.
Community activities
Community health workers registered children, conducted home visits and health education sessions, assessed ill children and mobilized communities for health outreach activities such as national immunization days.
Incentives
Community health workers were not paid a salary, but received various forms of financial and non-financial incentives such as:
Financial incentives: transport stipends to attend monthly meetings and 2–5 day-long annual training workshops (Canadian ∼$1.50 per day).
Material incentives: job aids (t-shirt, pen, folder, manual), token gifts (calendar, photo, soap, Christmas food packages) and small prizes during training.
Recognition awards: certificates and awards for various competitions (i.e. community health worker of the month, drama group presentations).
Social networking opportunities: exchange visits (i.e. between community health worker groups), inter-village health promotion competitions, annual holiday party and engagement with local council.
Income-generating opportunities: community health worker-initiated income-generating activities and savings/loans groups; HCU-supported training for specific income-generating activities (i.e. handicrafts, small business management).
A detailed description of the HCU intervention and its impact can be found in our report, The HCU Community-Owned Resource Persons Model 2010 (Healthy Child Uganda 2010), available at www.healthychilduganda.org/resources.
Study design
In November 2008, HCU undertook a study to examine community health worker retention over the course of the project and elicit factors supporting retention and motivation of its volunteers. Study approval was obtained from the Mbarara University of Science and Technology Institutional Ethical Review Committee in Uganda and the Carleton University Research Ethics Committee in Canada. All survey participants provided informed written consent.
Community health worker registry
Basic demographic information (name, gender, village and training dates) for all community health workers trained by HCU between February 2004 and July 2009 was entered in an MS Excel database and updated at least quarterly. Deaths, resignations (including self-reported reason for resignation) and new replacements were recorded. Periodically, additional community health worker demographic data including age, level of education and number of children were collected and recorded in the registry.
Community health worker survey
Two separate Questionnaires (A and B) were constructed de novo in English to address selection and motivation concepts. Questionnaire A collected both quantitative and qualitative data and applied a participatory rural appraisal technique called ‘pair-wise ranking’ (Russell 1997) to compare a series of potential motivating factors. The results of an earlier brainstorming exercise (involving six groups and 92 community health workers) were used to identify the motivational factors. Questionnaire B consisted of open-ended questions to elicit more in-depth responses to those given in Questionnaire A. Both questionnaires were translated into the local dialect, back translated and piloted with four community health workers from non-study parishes for clarity. No major revisions were required.
A stratified sampling frame was designed to survey community health workers from half (9 of 18) of the parishes where HCU operates. The nine participating parishes were selected based on the date of their next scheduled community health worker meeting (convenience sample). From these nine parishes, the names of 25% of active community health workers were drawn randomly in advance. Any pre-selected participant(s) not present on the day of the survey was replaced through a second random draw conducted on site. The number of community health workers in each parish varies according to the population size of each parish. Time and resource constraints limited a larger sample size.
Questionnaire A was initially conducted in six parishes (46 respondents). Preliminary analysis revealed a strong consensus among respondents, suggesting data saturation. The survey was then modified (Questionnaire B) to elicit more in-depth information and build on responses from Questionnaire A. Twelve respondents (from the remaining three study parishes) completed Questionnaire B. This sampling process is summarized in Figure 1.
Figure 1.
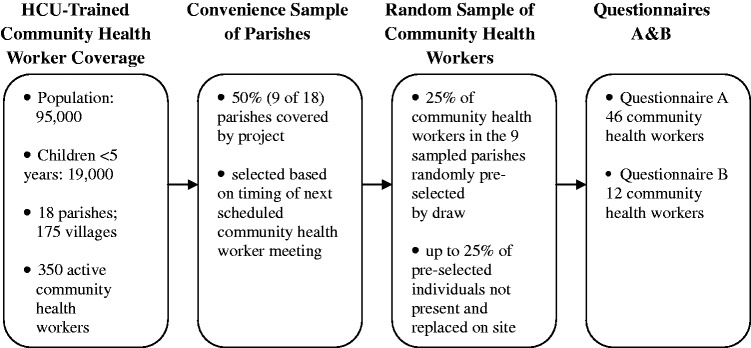
Sampling methods.
Surveys were constructed de novo in English, translated into local dialect, back translated for accuracy, then verbally administered in the local dialect by research assistants who did not have a role in HCU programming. Interviews were conducted on an individual basis to avoid peer and group influence on individual responses.
Data analysis
Using 2009 data from the registry (the most recent data available at the time of the study), descriptive statistics for community health worker demographics and retention were calculated using means and frequencies for numerical data and proportions for categorical data. The retention analysis considered aggregated results for the duration of the project, as well as disaggregated results by training date (Phases I and II). For the survey, descriptive statistics were used to calculate proportions for quantitative questions. Final pair-wise ranking scores were calculated by averaging the score for each motivator across all respondents. For closed-ended, multiple-choice questions, deductive coding was used to calculate frequency. Open-ended answers were grouped thematically and multiple-coded manually by the lead researcher.
Results
Community health worker demographics
Between February 2004 and July 2009, HCU trained 404 community health workers in 175 villages (279 females, 69%). Demographic data were collected from 302 community health workers from December 2009. Community health workers ranged in age from 20 to 73 years with an average age of 36.7 years (Figure 2). Ninety-eight per cent of community health workers had at least one child, with an average of 4.9 children. All community health workers had completed at least primary school grade 3: 30% completed primary 3–6; 33% completed primary 7 and 38% had gone beyond primary school. Male community health workers reported a higher average level of education (secondary school level 1) than did women (primary school level 7), [t (3.23) P < 0.05].
Figure 2.
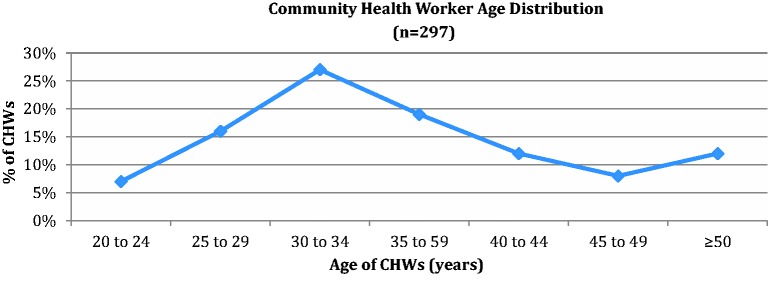
Community health worker age distribution.
Community health worker retention
The study analysed the retention of community health workers using data from the project registry. As of July 2009 (18–64 months after training owing to staggered start dates), 350 (87%) of all community health workers were still active. Fifty-four community health workers (13%) had resigned with no statistically significant difference between genders [χ2(1) = 1.84, P > 0.05 (Table 1)]. In the Phase I cohort (117 individuals trained during January–March 2004), the 5-year retention rate was 86.3%. However, once reasons unlikely to be related to poor motivation—changed village of residency, death, schooling and health problems—were excluded, the 5-year community health worker retention for the Phase 1 cohort was close to 95%. Almost all (173/175) villages had at least one active worker for every month during the 5-year period.
Table 1.
Community health worker retention by training date (n = 404)
| Period | Number trained | Number resigned | Number died | Retention |
|---|---|---|---|---|
| Phase I:February–March 2004 | 117 | 13 | 3 | 86% |
| Phase II:March 2006–January 2008 | 287 | 35 | 3 | 87% |
| Phases I and II:February 2004–July 2009 | 404 | 48 | 6 | 87% |
Length of time until resignation or death
For the 54 community health workers who were no longer active, the average length of time from initial training until resignation or death was 20 months with a range of 1–60 months (Figure 3). Of the total 404 community health workers trained between 2004 and 2009, 389 were still active 1 year (12 months) after initial training (96.2% retention). By 2 years post-initial training, 36 community health workers had died or resigned, leaving 91% retained.
Figure 3.
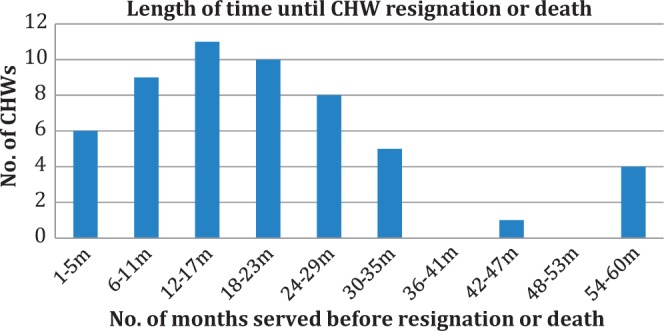
Community health worker attrition (n = 54).
In summary
96% (389/404) of CHWs were active for at least 1 year.
91% (368/404) of CHWs were active for at least 2 years.
86% (101/117) of CHWs were active for 5 years.
Reasons for community health worker attrition
The most common self-reported reasons for dropout were due to being too busy, moving to another village or needing to focus on business or other paid activities (Table 2). Six community health workers died, while another six resigned due to divorce. In cases of divorce, the woman typically returns to her parents’ village.
Table 2.
Self-reported reasons for community health worker attrition (n = 54)
| Reason | Total | Women | Men |
|---|---|---|---|
| Too busy | 12 | 5 | 7 |
| Moved from village | 11 | 9 | 2 |
| Business/employment | 8 | 3 | 5 |
| Died | 6 | 1 | 5 |
| Separation/divorce | 6 | 6 | 0 |
| Health/family issues | 4 | 4 | 0 |
| Opposed by husband | 3 | 3 | 0 |
| Unknown | 2 | 1 | 1 |
| Fired | 1 | 0 | 1 |
| Further studies | 1 | 1 | 0 |
| Total | 54 | 33 | 21 |
Participation in the questionnaire studies
In total, 58 community health workers participated in the verbally administered survey, representing 17% of all 350 community health workers active at the time. Forty-six completed Questionnaire A and 12 completed Questionnaire B. In each of the nine parishes, one or two of the pre-selected community health workers did not attend their scheduled monthly meeting; reasons for non-attendance were not documented. No community health workers at the meeting refused to participate in the survey.
The demographics of those participating in the survey were similar to the overall group in terms of age (mean age, 36 years) and gender (67% female), but the average level of education was slightly higher with 48% having at least some secondary school education.
Community health worker selection
In Questionnaire A, most (87%) respondents reported having been chosen through a community ‘election’. The remainder was selected either by the local council or by the local women’s council without wider input from the community. Of those ‘elected’, 89% recalled at least half of the community being present. Eighty-seven per cent estimated that women comprised at least half of those in attendance at the election.
Respondents described methods used to select the community health workers in their village: each side of the village chose one community health worker; interested individuals self-nominated themselves and were confirmed by community members; nominations from peers that were confirmed by consensus or by vote. Voting was often carried out by show of hands or by standing behind the candidate of choice. Community health workers almost universally (94%) reported that community election was the most desirable means of selecting candidates for the post. Community selection was preferred because community members have intimate knowledge of who would be most suitable (67%) and communities should have the ‘right’ to select their own representative (28%).
Community health worker motivation
Community health workers were asked to compare seven motivators using a pair-wise ranking tool (Table 3). As seven factors were presented, the highest possible score was 6, indicating that the respondent ranked that motivator above all others. The top 3 rankings were as follows: 1. ‘Improved child health in your village’; 2. ‘Education and training’ and 3. ‘Community members ask you for health advice or assistance’. The transport allowance ranked the lowest.
Table 3.
Motivating factors using pair-wise ranking (n = 46)
| Motivators | Ranking* (max score: 6) |
|---|---|
| Improved child health in village | 5.72 |
| Education and training | 4.50 |
| Community members ask me for health advice or assistance | 4.22 |
| Friendship with other community health workers | 2.39 |
| Income-generating projects and cash rounds | 2.02 |
| Respect by people in community | 1.39 |
| Monthly transport stipend (CAD ∼$1.50) | 0.43 |
*The maximum ranking score is 6; the minimum is 0.
The responses to the open-ended questions in Questionnaire B reinforce the outcomes of the ranking exercise:
Improved child health
When asked ‘Why do you volunteer?’ respondents explained that the training increased their awareness of how they could take action to improve the health of children in their community (11/12) and in their own families (4/12): ‘I realised I will benefit personally as well as my neighbours in a way that diseases would be fought and our children would grow healthy, strong, and have a right future as opposed to how it was before’. Respondents gave concrete examples of how their families and others in their villages had adopted new health practices and observed improved child health. ‘In our village child mortality was very high, but after we got involved through the project, it has now decreased very much. Almost every home if not all have vegetable gardens. This has improved greatly the health of our children. The neighbouring village which is not part of Healthy Child Uganda … their children die almost daily’.
Seventy-six per cent of respondents reported that since initial training, the number of hours they dedicate to carrying out volunteer, community health worker-related activities have increased.
Education and training
Furthermore, half of all respondents (6/12) cited refresher training/learning opportunities as something they ‘like about being a community health worker’: ‘The re-fresher courses they give us keep opening our eyes./ … I realized knowing these things could greatly change my family and the whole community at large’.
Requests for advice/assistance
Surveyed community health workers indicated that they gained pride and respect when village members consult them: ‘… people learn from me; they come to me for advice and I feel proud and useful in my community. I am even appointed to represent them elsewhere’. Though respect was not rated as highly as some of the other motivators in the ranking exercise, it emerged more clearly in the open-ended responses.
Discussion
Critics have flagged low retention as a serious weakness of community health worker programmes. However, poor retention does not have to be the rule. Our study is one of few to report medium-term retention from East Africa and present a detailed, disaggregated analysis of retention data for volunteers. The study provides insight into reasons for attrition, differentiating those which may be motivation-related from those due to other factors (death, illness, relocation and family problems). An impressively high retention rate was demonstrated (>85%) even after 5 years. Although many programmes do struggle to retain community health workers (Walt et al. 1989; Bhattacharyya et al. 2001; Olang’o et al. 2010), our findings alongside other successful examples—such as the low 3% dropout reported by the BRAC programme in Bangladesh (Standing and Chowdhury 2008)—suggest that high community health worker retention can be achieved.
Moreover, the high retention in HCU-trained community health workers challenges the assertion that non-financial incentives are insufficient to retain community health workers (Walt et al. 1989; WHO et al. 2008), since HCU does not provide significant salaries. Debate in the literature provides competing views on whether non-financial motivators such as ‘a sense of achievement' and ‘recognition’ are more important than salary in low income countries (Chandler et al. 2010; Glenton et al. 2010). Our study, based on the HCU context found that volunteer community health worker motivation stems primarily from perceived improvements in health outcomes, training opportunities and being a valued asset in the community.
We hypothesize that a number of HCU programme design factors may have helped promote community health worker retention and served to motivate volunteers, most of which have previously been cited as retention promoting: an inclusive, community-centred approach to selection (Bhattacharyya et al. 2001; Lehmann 2007); recruitment of individuals with a sense of community spirit and social responsibility (Glenton et al. 2010); frequent, participatory training sessions (Gilson et al. 1989; Biggs-Jarrel 1992; Bailey and Coombs 1996; Bhattacharyya et al. 2001; Lehmann 2007; Standing and Chowdhury 2008) and regular and supportive supervision from health centre staff (Curtale et al. 1995; Bhattacharyya et al. 2001; Haines et al. 2007). Furthermore, the study findings suggest our programme focus on ‘child health’ and subsequent notable child health improvements in intervention areas—documented and attributed to the community health worker intervention (Brenner 2011)—were key motivators for volunteers, whose activities, in turn, further improved the health of children in their communities.
We believe that HCU’s process for selecting community health workers may have played a key role in recruiting candidates who have a strong likelihood of staying on the job. The selection process emphasized clear communication of volunteer roles and expectations, promoted broad community attendance and community input into selection criteria and encouraged community selection of their own representatives. Perhaps community members are best positioned to select those individuals who have a demonstrated track record of volunteer spirit and commitment to the community. Furthermore, community-led selection may also help select individuals whose demographic profile (i.e. age, gender, marriage status and education) will most likely lead to longevity in that community and on the job (Bhattacharyya et al. 2001). Finally, those volunteers selected by their own peers may experience the most accountability and responsibility towards their own communities. Evidence from the literature and this study suggest that a transparent, participatory community selection process is a worthwhile investment for community health worker programmes of all sizes.
In addition, HCU’s use of interactive learning pedagogy and emphasis on community development and facilitation skills combined with regular contact and training by supervisors likely served as retention promoting, non-financial motivators. Other key HCU programme elements not cited in the literature but which may have played a role in promoting retention include the role of a ‘uniting cause’ (in our case child health) and organization of community health workers into teams. Both of these create a platform for peer support and an opportunity to be a ‘champion for change’.
We acknowledge important limitations of this study. Surveying only community health workers in attendance at monthly meetings may over represent more ‘motivated’ volunteers. Additionally, community health workers may have responded so as to satisfy interviewers, including underrating the significance of the small transport allowance. Our motivation and selection questionnaires lacked input from supervisors, those who had dropped out, and community members served by community health workers—all of which may have highlighted different perspectives on selection and motivation. Although we consider HCU community health workers to be ‘volunteers’, they did receive a very modest transport allowance to attend monthly meetings (∼CAN $1.50) which may have acted as a financial incentive. Of reassurance, these allowances were discontinued completely 1 year after conducting this survey, without substantial impact on meeting attendance, reporting or retention during the following 12 months.
As countries and donors increasingly invest in large-scale community health worker programmes, more studies examining retention and motivation across various programme designs are needed. While HCU has demonstrated positive results, more evaluation is needed to assess whether high retention is possible within larger programmes, such as the roll-out of Uganda’s Village Health Teams and other country-level programmes. Ensuring quality of selection, non-financial incentives, supervision and refresher training may be more challenging as programme size increases. Future studies should explore how different ‘packages’ of incentives may impact motivation and retention, how retention varies over time (included the longer term) and how often and through what mechanism community health workers should be replaced or re-affirmed. Further investigation is also needed to better understand how assigned tasks (such as medicine distribution), responsibilities and workload impact retention and motivation.
Conclusion
Our study demonstrates that under the right conditions it is possible to retain volunteer community health workers over the medium term (i.e. 5 years) in a rural, sub-Saharan Africa context where financing is extremely limited. Community health worker programmes should not be viewed simplistically as a quick fix, but as one component of a broader primary health care approach involving diverse human resources for health.
Community health worker programmes require investment in high-quality selection, training, supportive supervision, incentives and evaluation. Policy-makers and programmers should consider the following among key elements in designing and implementing community health worker programmes: community involvement in community health worker selection, recurrent training, incentives, peer and supervisory support, and focus on specific, easily understood, high priority health issues.
Narrowly debating the merits of paid vs unpaid community health workers may not be the most productive way forward. Rather, researching incentive and behavioural models could strengthen understanding of motivation and retention, and support the implementation of more effective, sustainable programmes. This will be particularly important as we move into the post-2015, post-MDG era where the dialogue on how to achieve sustainable health gains and address continuing shortages of human resources for health is of increasing importance.
Other contributors
We thank the many community health workers, trainers, health centre staff, community members and leaders whose input shaped the HCU model and who participated in the study including HCU staff (Erin Kiley and Patricia Tushemereirwe), academic advisors (Valerie Percival and Chantal Blouin), research assistants (Priscilla Tusiime, Doreen Ainembabzi and Mutoni Ramulah), analysis (Andrea Wilson, Carolyn Pim and Tanya Beran) and editing advice (Noni MacDonald).
Funding
This study was funded by the Association of Universities and Colleges of Canada (AUCC) through its Students for Development program. The AUCC played no role in the study design, data collection, analysis, or report writing. We are also grateful for support which has enabled community health worker training and programming since 2004 from the Canadian International Development Agency, Healthy Generations Foundation, Buy-A-Net, Mayfield Rotary Club and the University of Calgary Annual Giving Program.
References
- Bailey J, Coombs D. Effectiveness of an Indonesian model for rapid training of Guatemalan health workers in diarrhea case management. Journal of Community Health. 1996;21:269–76. doi: 10.1007/BF01794877. [DOI] [PubMed] [Google Scholar]
- Bhattacharyya K, Winch P, Leban K, Tien M. Community Health Worker Incentives and Disincentives: How They Affect Motivation, Retention and Sustainability. 2001. Published by the Basic Support for Institutionalizing Child Survival Project (BASICS II) for the United States Agency for International Development. Arlington, Virginia. [Google Scholar]
- Biggs-Jarrel P. Village health volunteers: key issues facing agencies in Malawi. Malawi Medical Journal. 1992;8:68–69. [Google Scholar]
- Brenner J, Kabakyenga J, Kyomuhangi T, et al. Can volunteer community health workers decrease child morbidity and mortality in southwestern Uganda? An impact evaluation. PLoS ONE. 2011;12:e27997. doi: 10.1371/journal.pone.0027997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian International Development Agency. Canada’s Contribution to the Global Effort to Reach the Millennium Development Goals. Her Majesty the Queen in Right of Canada. 2010. [Google Scholar]
- Chandler C, Chonya S, Mtei F, Reyburn H, Whitty C. Motivation, money and respect: a mixed-method study of Tanzanian non-physician clinicians. Social Science and Medicine. 2009;68:2078–2088. doi: 10.1016/j.socscimed.2009.03.007. [DOI] [PubMed] [Google Scholar]
- Curtale F, Siwakoti B, Lagrosa C, Laraja M, Guerra R. Improving skills and utilization of community health volunteers in Nepal. Social Science and Medicine. 1995;40:1117–25. doi: 10.1016/0277-9536(94)00172-p. [DOI] [PubMed] [Google Scholar]
- Dambisya YM, Matinhure S. Policy and programmatic implications of task shifting in Uganda: a case study. BMC Health Services Research. 2012;12:61. doi: 10.1186/1472-6963-12-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dingle A, editor. Measuring Volunteering: A Practical Toolkit. Washington, DC: Independent Sector and United Nations Volunteers (UNW); 2001. [Google Scholar]
- East, Central and Southern Health Community (ECSA-HC) Task Shifting in Uganda: Case Study. Washington, DC: Futures Group, Health Policy Initiative, Task Order 1; 2010. [Google Scholar]
- Fulton B, Scheffler R, Sparkes S, et al. Health workforce skill mix and task shifting in low income countries: a review of recent evidence. Human Resources for Health. 2011;9:1. doi: 10.1186/1478-4491-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilson L, Walt G, Kris H, et al. National community health worker programs: how can they be strengthened? Journal of Public Health Policy. 1989;10:518–32. [PubMed] [Google Scholar]
- Glenton C, Scheel I, Pradhan S, et al. The female community health volunteer programme in Nepal: Decision makers’ perceptions of volunteerism, payment and other incentives. Social Science and Medicine. 2010;70:1920–7. doi: 10.1016/j.socscimed.2010.02.034. [DOI] [PubMed] [Google Scholar]
- Haines A, Sanders D, Lehmann U, et al. Achieving child survival goals: potential contribution of community health workers. Lancet. 2007;369:2121–31. doi: 10.1016/S0140-6736(07)60325-0. [DOI] [PubMed] [Google Scholar]
- Healthy Child Uganda. Healthy Child Uganda Community Owned Resource Persons Model. 2010. www.healthychilduganda.org/resources, accessed 23 April 2013. [Google Scholar]
- Khan S, Chowdhury A, Karim F, Barua M. Training and retaining Shasthyo Shebika: reasons for turnover of community health workers in Bangladesh. Health Care Supervisor. 1998;17:37–47. [PubMed] [Google Scholar]
- Lehmann U. Community Health Workers: What Do We Know about Them? The State of the Evidence on Programmes, Activities, Costs and Impact on Health Outcomes of Using Community Health Workers. Geneva: World Health Organization; 2007. [Google Scholar]
- Maes K, Kohrt B, Closser S. Culture, status and context in community health worker pay: Pitfalls and opportunities for policy research. A commentary on Glenton et al. (2010) Social Science and Medicine. 2010;71:1375–8. doi: 10.1016/j.socscimed.2010.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabudere H, Assimwe D, Mijumbi R. An Evidence-based Policy Brief: Task Shifting to Optimise the Roles of Health Workers to Improve the Delivery of Maternal and Child Healthcare. Regional East African Community Health (REACH) Policy Initiative; 2010. [Google Scholar]
- Nkonki L, Cliff J, Sanders D. Lay health worker attrition: important but often ignored. Bulletin of the World Health Organization. 2011;89:853–928. doi: 10.2471/BLT.11.087825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nsabagasani X, Nsungwa-Sabiiti J, Källander K, et al. Home-based management of fever in rural Uganda: community perceptions and provider opinions. Malaria Journal. 2007;6:11. doi: 10.1186/1475-2875-6-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nsungwa-Sabiiti J, Peterson S, Pariyo G, et al. Local fever illness classifications: implications for home management of malaria strategies. Tropical Medicine and International Health. 2004;9:1191–9. doi: 10.1111/j.1365-3156.2004.01319.x. [DOI] [PubMed] [Google Scholar]
- Olang’o C, Nyamongo I, Aagaard-Hansen J. Staff attrition among community health workers in home-based care programmes for people living with HIV and AIDS in western Kenya. Health Policy. 2010;97:232–7. doi: 10.1016/j.healthpol.2010.05.004. [DOI] [PubMed] [Google Scholar]
- Parlato M, Favin M. Primary Health Care. Progress and Problems: An Analysis of 52 AID Assisted Projects. Washington, DC: American Public Health Association; 1982. [Google Scholar]
- Rahman SM, Ali NA, Jennings L, et al. Factors affecting recruitment and retention of community health workers in a newborn care intervention in Bangladesh. Human Resources for Health. 2010;8:12. doi: 10.1186/1478-4491-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell T. PLA Notes. London: International Institute for Environment and Development; 1997. [Google Scholar]
- Shrestha S. A conceptual model for empowerment of the female community health volunteers in Nepal. Education for Health. 2003;16:318–27. doi: 10.1080/1357628031000701607668. [DOI] [PubMed] [Google Scholar]
- Standing H, Chowdhury AMR. Producing effective knowledge agents in a pluralistic environment: what future for community health workers? Social Science and Medicine. 2008;66:2096–107. doi: 10.1016/j.socscimed.2008.01.046. [DOI] [PubMed] [Google Scholar]
- Stekelenburg J, Simasiku SK, Wolffers I. Poor performance of community health workers in Kalabo District, Zambia. Health Policy. 2003;65:109–18. doi: 10.1016/s0168-8510(02)00207-5. [DOI] [PubMed] [Google Scholar]
- Sunkutu K, Nampanya-Serpell N. Searching for Common Ground on Incentive Packages for Community Workers and Volunteers in Zambia: A Review of Issues and Recommendations. Zambia: The National HIV/AIDS STI, TB Council; 2009. [Google Scholar]
- Uganda Ministry of Health, WHO, UNICEF. Integrated Community Case Management of Childhood Malaria, Pneumonia and Diarrhoea: Implementation Guidelines. Kampala: Ugandan Ministry of Health; 2010. [Google Scholar]
- Walt G, Perera M, Heggenhougen K. Are large-scale volunteer community health worker programmes feasible? The case of Sri Lanka. Social Science and Medicine. 1989;29:599–608. doi: 10.1016/0277-9536(89)90179-2. [DOI] [PubMed] [Google Scholar]
- WHO, PEPFAR, UNAIDS. Task Shifting: Rational Redistribution of Tasks among Health Workforce Teams: Global Recommendations and Guidelines. Geneva: World Health Organization; 2008. [Google Scholar]
- World Health Organization, Global Health Workforce Alliance. Global Experience of Community Health Workers for Delivery of Health-Related Millenium Development Goals: A Systematic Review, Country Case Studies, and Recommendations for Integration into National Health Systems. 2010. [Google Scholar]


