Although many children with Attention Deficit Hyperactivity Disorder (ADHD) experience motor difficulties, little is known about motor development in these patients (1-3). Potential factors underlying motor problems in ADHD are a lack of physical skill due to lack of experience, poor social skills leading to less opportunities to engage in free play and sports, inability to regulate play and sports, an impaired sense of time, lack of motivation and problems with timing, fundamental to motor coordination (4). Possible aetiologic factors include genes which may be shared between ADHD and motor problems (5,6).
In childhood and adolescence the fundamental motor skill level of individuals is related to the extent of their habitual physical activity, and, vice versa, their physical activity level is positively related to their actual motor competence (7). Perceived motor competence or individual motor self-perception is the degree to which people perceive themselves as being athletic and good at sports and athletic activities (8,9). The way in which people perceive their own motor competence may become more positive if the person is also interested in that specific domain. Therefore the assumption is justified that perceived motor competence, the interest in the motor domain and motor performance are positively related. This assumption also is the philosophy behind Harter's Self-Perception Profile for Children (SPPC (10). It supports a relationship between self-perception, self-esteem and global self-worth on measures of scholastic competence, athletic ability, physical appearance, social acceptance and behavioral conduct, with athletic skills and physical appearance contributing significantly to the self-worth of typically developing children.
Children with motor difficulties like Developmental Coordination Disorder (DCD), not accompanied by ADHD, tend to show lower perceived motor competence. These children generally are realistic about their physical abilities (4,11,12). Children with Attention Deficit Hyperactivity Disorder (ADHD) experience comorbid DCD in 30% to 50% of cases (1;13;14). Little is known about the motor self-perception in this group of children. In studies of general self-perception in children with ADHD, some found lowered self-perception whereas others found no differences compared to controls (e.g.15). Barber and colleagues compared self-perception of children with and without ADHD. The ADHD group scored significantly lower on an overall score and on the behavioral conduct subscale compared to children without ADHD. However, on the athletic competence subscale, the ADHD children did not differ from their non-ADHD-affected peers. Not all studies however used a criterion or an actual measure of performance as the basis for comparing objectively measured and self-perceived competence. In studies in which an actual level of performance was known, inflated self-perception was found. The children with ADHD tended to overestimate themselves in scholastic, social and behavioral domains, relative to a teacher-rated criterion (16;17).
In summary, the literature on self-perception in ADHD is inconclusive, and little is known about the motor domain. The main goal of this study was to explore the relationship between actual motor performance level and perceived motor competence in children with ADHD, their unaffected siblings and healthy controls. Healthy controls were included next to non-ADHD-affected siblings to be able to make a comparison regarding self-perception, to be sure that familial factors in self-perception did not bias the results.
Method
Participants
A total of 103 children (mean age 10 years; SD 1.9 years) participated in the study. Local ethics review boards in The Netherlands approved the study. Parents provided written informed consent for their children less than 12 years old; children aged 12 and older gave written informed consent themselves, in addition to their parents.
Participants with ADHD and their siblings were recruited from a sample of families who participated in the International Multi-centre ADHD Genetics (IMAGE) project (18;19). These families have at least two biological children participating in the study, at least one of them suffering from ADHD (probands). Thirty-two families randomly chosen were approached to participate by their physician. Twenty-five of these families participated. The families had 33 children with ADHD, as well as 19 unaffected siblings participating. The control children (n = 51) were recruited from two elementary schools in Drenthe, The Netherlands, and were unrelated. Children with IQ<70 were excluded from the study. None of the children suffered from known genetic syndromes (Down, Turner, Fragile-X), brain injuries, autism, epilepsy or a physical disability.
Materials
ADHD measures
Screening questionnaires (parent and teacher Conners' long version rating scales and parent and teacher Strengths and Difficulties Questionnaires (SDQ) (20,21)) were used to screen children for ADHD symptoms. T-scores ≥ 63 on the Conners ADHD-subscales (L for inattention, M for hyperactive-impulsive and N for total scores) and scores > 90th percentile on the SDQ-hyperactivity scale were considered as clinical. Children who scored in the clinical range were subsequently invited for a complete diagnostic procedure. During a hospital visit, a semi-structured, standardized, investigator-based interview, the Parental Account of Children's Symptoms (PACS) (22) was administered. The PACS covers DSM-IV symptoms of ADHD, conduct disorder, oppositional defiant disorder, anxiety, mood, and other internalizing disorders. The section on autistic behavior traits was administered, if a clinical score (raw score ≥ 15) was obtained on the Social Communication Questionnaire (23). A standardized algorithm was applied to the PACS to derive each of the 18 DSM-IV ADHD symptoms, providing operational definitions for each behavioral symptom. These were combined with items that were scored 2 (‘pretty much true’) or 3 (‘very much true’) on the teacher-rated Conners ADHD subscales (L, M and N) to generate the total number of hyperactive-impulsive and inattentive symptoms of the DSM-IV symptom list. Situational pervasiveness was defined as at least one symptom occurring within two or more different situations as indicated by the parents in the PACS interview, as well as the teachers' Conners questionnaire. The procedure used to establish the ADHD diagnosis in this study is described in more detail elsewhere (18,19). To rule out ADHD in the control children teachers were asked to fill out the Conners questionnaire (Conners Teachers' Long Version). A scaled score of <63 was used as a cut-off for control children.
Motor performance measures
To test the motor performance level, all children completed the Movement Assessment Battery for Children (MABC) in a second hospital visit (24).The MABC is an age-appropriate standardized and valid motor performance test to measure the motor abilities of a child and is used worldwide to detect motor performance problems in clinical populations (24,25,26). In 1998 the MABC was translated into Dutch and validated for the Dutch population. The Dutch version was used in the current study (27). The MABC includes motor tasks related to functioning in daily life, and the manual provides normative data for children aged 4 to 12 years. The MABC is divided into four age bands. Each band contains 8 motor tasks, suitable for a restricted age group of children: age band I for 4 to 6 years, age band II for 7 to 8 years, age band III for 9 to 10 years, and age band IV for 11 to 12 years. The children older than 12 years (n 11)were tested with age band IV. Each age band is identical in structure and contains eight items, divided into three sections: manual dexterity (3 items), ball skills (2 items), and static and dynamic balance (3 items). There are two sorts of tasks at each item level: time-related (scored in seconds) and error-related (scored by number of ‘good’ attempts). The aim of the test is to assess children's motor performance level; therefore the tester ascertains that the child has understood the task before commencing. The raw score of the best attempt on each item is converted into a scaled score. The way this is done varies from task to task, but is well described in the test manual. Scaled interval scores for each item are provided: 0=good and 5=very poor. Some items are performed by both the preferred and non-preferred hand (or feet); the child's scores for both hands (or feet) are added up and then divided by two. Summing the item scores into three section scores produces a profile of the child's performance. The section score for manual dexterity will vary from 0 to 15, the section score for ball skills from 0 to 10, and that for static and dynamic balance from 0 to 15. These three section scores are then summed again to produce a Total Motor Impairment score, ranging from 0 to 40. High scores on the MABC represent poor performance. The raw scores of the three sections and the raw Total Impairment Score can be converted into age-related percentile scores, with a typical cut-off score of ≤ 15th percentile or ≤ 5th percentile. All participants were classified into three categories according to their MABC Total Impairment Scores: 1. Total Impairment Score >15th percentile: acceptable performance; 2. Total Impairment Score between 5 and 10th percentile: borderline performance; and 3. Total Impairment Score < 5th percentile: motor problems conform DCD. The MABC has acceptable validity and reliability (23).
To test the self-perception of motor competence in children the supplement m-CBSK from the Dutch ‘Competentiebelevingsschaal’ for Children (CBSK) was used (28), a Dutch translation of Harter's SPPC (10). This m-CBSK contains two different questionnaires: a motor self-perception questionnaire and a domain interest questionnaire. The motor self-perception questionnaire (17-items) is designed to measure children's self-perception of their motor performance level. Physical activities are presented to the child and the child has to choose two times in a digitomized format. For example, a child is asked to choose from two alternatives the one that best describes himself such as “some kids are really good swimmers” or “other kids are not so good swimmers”. After choosing one of those two alternatives, he/she has to indicate whether the selected sentence was either “a little bit true for me” or “totally true for me”. The first question in the questionnaire is for practice and four “filter-items” are included to correct for socially desirable answers. These five questions are not calculated in the total score, so the final total score is based on 12 questions, with higher scores indicating higher perception.
The domain interest questionnaire contains 10 items and is designed to measure the interest in five different domains, the ‘motor domain’, ‘cognitive domain’, ‘social domain’, ‘appearance’ and ‘general behavior’. A four-point scale is used to score how important above mentioned domains are for the child. An example for a motor domain question is: “I think being good in sports is” ‘totally not important’(score 1), ‘actually not important’(2), ‘rather important’(3), or really important' (4).
Procedure
The same medical doctor examined all children and performed the ADHD measurements at the start of this study. Medication (methylphenidate in all medicated cases) was stopped one day prior to testing. The same trained investigator, a physical therapist, tested all children included in the study on the MABC. The investigator knew which children were the control children because these children were examined in a gym in their school. The investigator was blind to group status in the ADHD families which were all examined in the hospital (ADHD-proband, ADHD-affected or ADHD-non-affected siblings). The investigator did not have prior information about the motor capacities of the children. All children were tested in a quiet room. All children completed the motor self-perception and domain interest questionnaires before the MABC test. The investigator gave an oral instruction how to complete the questionnaires.
Statistical analysis
Questionnaires with four or more questions missing were excluded from statistical analysis (n = 1). When three or less questions were missing those missing scores were replaced by the mean score for that particular question (n = 3). Chi-square tests were used to test if the MABC scores in the three groups (ADHD children, siblings without ADHD and normal control children) differed from the expected distribution in the reference population in the manual. Because of non-normality of the MABC data and the CBSK data we applied a square root transformation, which reduced skewness and kurtosis.
Group differences were examined by a Linear Mixed Model, with diagnosis (3 levels: ADHD, siblings and controls) as between subjects variable, age as covariate, and the MABC Total Impairment Scores, subscale scores, total self perceived motor competence scores and domain interest scores as dependent measures. Linear Mixed Model was chosen to check for within-family correlation. The correlations between the MABC scores, the self-perceived motor competence scores and the interest in the motor domain score were calculated using Spearman correlation coefficients. We also explored whether these correlations were dependent on the MABC results. To this end, we used the three categories according to the MABC Total Impairment Scores as described above: 1. Total Impairment Score >15th percentile: normal; 2. Total Impairment Score between 5 and 15th percentile: borderline; and 3. Total Impairment Score <5th percentile: motor problems conform DCD.
The statistical significance level was set at p < .05, and SPSS 14.0 was used for all statistical analyses.
Results
The 25 participating ADHD families had 33 children with ADHD as well as 19 unaffected siblings (see Table 1). In addition, 51 control children from 51 families participated.
Table 1.
Demographics and Mean total scores and Standard Deviation (SD) on the Movement Assessment Battery for Children (MABC), the self-perception questionnaire and the different sub-domains of the domain interest questionnaire in children with ADHD, siblings without ADHD and control children
| children with ADHD n = 32 | unaffected siblings n = 18 | controls n = 50 | |
|---|---|---|---|
| mean (SD) | mean (SD) | mean (SD) | |
| Age (years) | 11.0 (2.4) | 10.2 (2.3) | 9.1 (0.3) |
| Gender | |||
| boys | 27 | 8 | 29 |
| girls | 5 | 10 | 21 |
| MABC Total Score | 11.8 (7.2)* | 8.2 (5.2)* | 5.6 (3.0)* |
| subscale manual dexterity | 5.3 (4.0)* | 3.7 (2.9)* | 3.1 (2.3)* |
| subscale ball skills | 2.2 (2.3)* | 1.4 (2.2)° | 0.6 (0.9)* |
| subscale balance | 4.4 (3.3)* | 3.1 (2.8)° | 1.9 (1.5)* |
| Motor self-perception | 36.7 (6.3)° | 35.9 (4.8)° | 35.4 (4.2)° |
| Interest motor domain | 6.1 (1.7)° | 6.0 (1.6)° | 5.7 (1.5)° |
| Interest cognitive domain | 6.7 (1.4)° | 7.2 (0.9)° | 7.3 (0.8)° |
| Interest ‘physical appearance’ | 5.3 (1.7)° | 5.7 (0.9)° | 5.8 (1.2)° |
| Interest social domain | 5.2 (1.6)* | 6.0 (1.0)° | 6.2 (1.5)° |
| Interest ‘generally behavior’ | 6.3 (1.2)° | 6.5 (1.0)° | 6.6 (1.1)° |
no significant differences between probands and siblings and/or controls
significant differences between probands and siblings and/or controls
Actual Motor Performance
One child from each of the three groups did not complete the MABC test, so 32 ADHD-affected children (27 boys and 5 girls),18 unaffected siblings (8 boys and 10 girls) and 50 control children (29 boys and 21 girls) were included in the analyses.
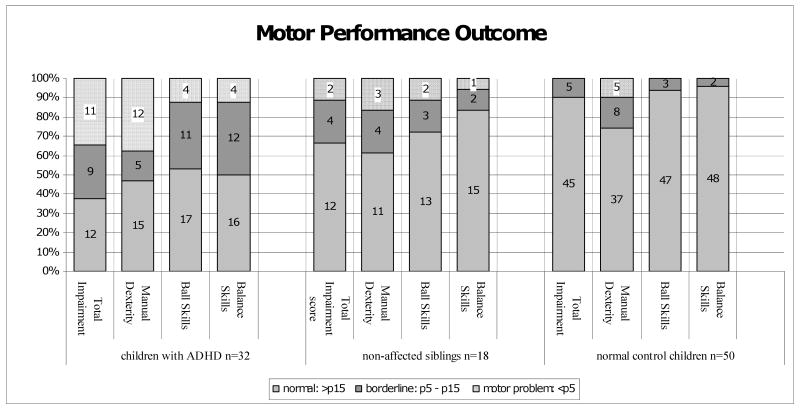
In the ADHD group, the mean Total Impairment scores differed significantly from the expected distribution of scores in the reference population (X2 = 74.23; p < .001; see Table 1). Twenty-one out of 32 (63%) of children with ADHD scored below the 15th percentile of the MABC. Of these 21, 11 (34%) scored below the 5th percentile (Figure 1). The mean Total Impairment Scores in the unaffected sibling group and in the control group did not differ significantly from the normal distribution (siblings X2 = 4.74; p > .05; controls X2 = 2.67; p > .05; Table 1). In the Linear Mixed Model a significant effect of diagnosis on the Total Impairment Score of the MABC was observed (F(2, 87.6)=7.85, p=0.001). Post hoc testing showed that children with ADHD differed significantly from their unaffected siblings and controls (p= 0.038 and p<.001, respectively). Unaffected siblings did not differ significantly from controls (p = 0.12).
Figure 1.
Motor performance in ADHD, siblings and control children according to the Movement Assessment Battery for Children (MABC). Numbers in bars are numbers of children.
Percentile ranges: 0-5 = motor problem; 5-15= borderline; >15 = normal
Diagnosis had a significant effect on all three subscales of the MABC: manual dexterity (F(2, 85.0)=4.14, p= 0.019), ball skills (F(2, 86.8)=7.18, p=0.001), and balance (F(2, 100)=3.98, p=0.022). For manual dexterity, probands performed worse than both siblings (p=0.019) and controls (p=0.018). Siblings did not differ from controls (p=0.83). However, for the other two subscales, non-affected siblings formed an intermediate group, not differing significantly from probands (ball skills: p=0.07; balance: p=0.21) or controls (ball skills: p=0.11; balance: p=0.22). As expected, probands did differ from controls on both scales (ball skills: p<0.001; balance: p=0.006).
Perceived motor competence
There was no significant effect of diagnosis on the self-perceived motor competence (F(2,88.0)=.02, p=0.98). Moreover, there was no significant effect of diagnosis on the domain interest scales, except for the social domain (F(2,79.1)=3.47, p=0.036), where children with ADHD scored lower than siblings and controls. This means that the children with ADHD consider the social domain less important than their siblings and control children.
MABC scores were not significantly correlated with the scores on the motor self-perception questionnaire in the total group (r=0.169; p=0.115). For the most motor-impaired children (Total Impairment Score ≥ 13.5, corresponding to < 5th percentile on the MABC; n=13), the scores on the MABC were significantly correlated with self-perceived motor competence (r= -0.586; p=0.035). In the other groups the correlation between self-perception of motor performance and actual motor performance was negative.
The correlation between scores on the interest in the motor domain and the self-perceived motor competence was significant (r=0.445; p=0.001). The interest in the motor domain was not related to the actual motor performance level (p=0.871).
Discussion
In this study comparing actual and perceived motor performance in children with ADHD, their unaffected siblings and control children, actual motor performance was significantly poorer in children with ADHD compared to their siblings and healthy control children. A high percentage (63%) of the children with ADHD displayed motor difficulties. 34% of the ADHD-children performed in the clinical DCD-range (Figure 1). Especially manual dexterity, which comprises fine motor abilities was affected. This is in line with previous reports (1;4;25). However, self-perceived motor performance did not differ between groups, moreover, self-perceived competence and actual performance showed a negative correlation. This indicates an inflated self-perception in the children with ADHD. This is congruent with a growing body of evidence that children with ADHD overestimate their own competence, a phenomenon known as Positive Illusory Bias (16;17;29). The causes and function of this phenomenon are unclear. Cognitive immaturity, neuropsychological deficits, ignorance and self-protection have been suggested as possible explanations (4). All of these suggestions make sense. Inflated self-perceptions may be seen as self-protection, which helps children to cope with failure experiences. Evidence for this comes from a study in which ADHD-affected boys tended to overestimate their performance most in domains in which they were most impaired (4;16). In the current study this was not the case: the most motor-impaired group of children (MABC scores < 5th percentile) was the only group in which the perceived competence and the actual performance were significantly related. A possible explanation for this is that these children performed so poorly, that it could not be denied.
In fact, many children with ADHD have comorbid DCD. In previous studies, this comorbidity was not always taken into account. In the current study, the most motor-impaired children may be considered as suffering from both ADHD and DCD. Apparently in this group of children with serious motor performance problems, perceived motor competence is indeed reduced. This is in line with previous reports about DCD and self-perceived competence (4,11,12).
As expected, the interest of children in motor activities was related to their self-perceived motor competence level. However, the level of interest was not related to their actual motor performance level. So, we did not find support for the hypothesis that more interest is related to an increase in skill level e.g. as result of a higher participation.
Remarkably this study also found lower motor performance concerning ball skills and balance in the siblings without ADHD. These siblings formed an intermediate group between ADHD probands and healthy control children. This is a further indication for a shared underpinning of decreased motor performance and ADHD, which could be of genetic or shared familial origin (5,6).
Our study should be viewed in the context of some strengths and limitations. A strong feature in this study is the fact that all children, both ADHD and non-ADHD-affected, were tested by the same trained tester (MdH), which avoided bias as result of inter-individual tester differences. Moreover, there was an accurate diagnosis of ADHD with detailed and standardized procedures. A potential limitation comes from the fact we investigated relatively small samples of children. Also, in the clinical group we had more boys, owing to the fact that ADHD in clinical samples shows an overrepresentation of boys. It has been proposed that the MABC may penalize children with attention problems with the consequence of false positive scores. We tried to overcome this problem by providing the child with clear and short instructions in a structured quiet environment. Moreover, the tester started the test only if she was sure that the child really focused on the task.
More in-depth studies are necessary to determine which personal child characteristics and factors in the physical and social environment are related to actual motor performance and perceived motor competence in a child.
Based on the findings in this study we conclude that children with ADHD perform poorer on the MABC. Especially manual dexterity is affected. However, there is no relationship between actual and self-perceived motor competence, except for children with ADHD and severe motor problems. Generally, children with ADHD overestimate their motor performance.
For clinicians our study implies that motor performance needs more attention in children with ADHD, as motor problems occur in about half of them. Motor coordination problems (DCD) may have negative consequences in social, educational and prognostic respect.
Even if children with ADHD do not perceive themselves as being clumsy, professionals should pay attention to this important comorbidity.
Acknowledgments
The authors thank all the participating parents and children for their enthusiastic cooperation. We greatly acknowledge the management and the teachers of the schools in Drenthe.
This study was partly funded by NIH Grant R01MH62873 to SV Faraone.
Support: partly funded by NIH Grant R01MH62873 to Steve Faraone.
Reference List
- 1.Fliers E, Rommelse N, Vermeulen SH, et al. Motor coordination problems in children and adolescents with ADHD rated by parents and teachers: effects of age and gender. J Neural Transm. 2008;115(2):211–20. doi: 10.1007/s00702-007-0827-0. [DOI] [PubMed] [Google Scholar]
- 2.Gillberg C. Deficits in attention, motor control, and perception: a brief review. Arch Dis Child. 2003 Oct;88(10):904–10. doi: 10.1136/adc.88.10.904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sergeant JA, Piek JP, Oosterlaan J. ADHD and DCD: a relationship in need of research. Hum Mov Sci. 2006 Feb;25(1):76–89. doi: 10.1016/j.humov.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Harvey WJ, Reid G, Grizenko N, et al. Fundamental Movement Skills and Children with Attention-Deficit Hyperactivity Disorder: Peer Comparisons and Stimulant Effects. J Abnorm Child Psychol. 2007 May 15; doi: 10.1007/s10802-007-9140-5. [DOI] [PubMed] [Google Scholar]
- 5.Martin NC, Piek JP, Hay D. DCD and ADHD: a genetic study of their shared aetiology. Hum Mov Sci. 2006 Feb;25(1):110–24. doi: 10.1016/j.humov.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 6.Fliers E, Vermeulen S, Rijsdijk F, et al. ADHD and poor motor performance from a family genetic perspective. J Am Acad Child Adolesc Psychiatry. 2009 Jan;48(1):25–34. doi: 10.1097/CHI.0b013e31818b1ca2. [DOI] [PubMed] [Google Scholar]
- 7.Fisher A, Reilly JJ, Kelly LA, et al. Fundamental movement skills and habitual physical activity in young children. Med Sci Sports Exercise. 2005;37:684–88. doi: 10.1249/01.mss.0000159138.48107.7d. [DOI] [PubMed] [Google Scholar]
- 8.Raudsepp L, Liblik R. Relationship of perceived and actual motor competence in children. Percept Mot Skills. 2002 Jun;94(3 Pt 2):1059–70. doi: 10.2466/pms.2002.94.3c.1059. [DOI] [PubMed] [Google Scholar]
- 9.Raustorp A, Stahle A, Gudasic H, et al. Physical activity and self-perception in school children assessed with the Children and Youth--Physical Self-Perception Profile. Scand J Med Sci Sports. 2005 Apr;15(2):126–34. doi: 10.1111/j.1600-0838.2004.406.x. [DOI] [PubMed] [Google Scholar]
- 10.Harter S. Manual for the self-perception profile for children. Denver: University of Denver Department of Developmental Psychology; 1985. [Google Scholar]
- 11.Losse A, Henderson SE, Elliman D, et al. Clumsiness in children--do they grow out of it? A 10-year follow-up study. Dev Med Child Neurol. 1991 Jan;33(1):55–68. doi: 10.1111/j.1469-8749.1991.tb14785.x. [DOI] [PubMed] [Google Scholar]
- 12.Skinner RA, Piek JP. Psychosocial implications of poor motor coordination in children and adolescents. Hum Mov Sci. 2001 Mar;20(1-2):73–94. doi: 10.1016/s0167-9457(01)00029-x. [DOI] [PubMed] [Google Scholar]
- 13.Kadesjo B, Gillberg C. The comorbidity of ADHD in the general population of Swedish school-age children. J Child Psychol Psychiatry. 2001 May;42(4):487–92. [PubMed] [Google Scholar]
- 14.Piek JP, Dyck MJ, Nieman A, et al. The relationship between motor coordination, executive functioning and attention in school aged children. Arch Clin Neuropsychol. 2004 Dec;19(8):1063–76. doi: 10.1016/j.acn.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 15.Barber S, Grubbs L, Cottrell B. Self-perception in children with attention deficit/hyperactivity disorder. J Pediatr Nurs. 2005 Aug;20(4):235–45. doi: 10.1016/j.pedn.2005.02.012. [DOI] [PubMed] [Google Scholar]
- 16.Hoza B, Pelham WE, Jr, Dobbs J, et al. Do boys with attention-deficit/hyperactivity disorder have positive illusory self-concepts? J Abnorm Psychol. 2002 May;111(2):268–78. doi: 10.1037//0021-843x.111.2.268. [DOI] [PubMed] [Google Scholar]
- 17.Hoza B, Gerdes AC, Hinshaw SP, et al. Self-perceptions of competence in children with ADHD and comparison children. J Consult Clin Psychol. 2004 Jun;72(3):382–91. doi: 10.1037/0022-006X.72.3.382. [DOI] [PubMed] [Google Scholar]
- 18.Brookes K, Xu X, Chen W, et al. The analysis of 51 genes in DSM-IV combined type attention deficit hyperactivity disorder: association signals in DRD4, DAT1 and 16 other genes. Mol Psychiatry. 2006 Oct;11(10):934–53. doi: 10.1038/sj.mp.4001869. [DOI] [PubMed] [Google Scholar]
- 19.Kuntsi J, Neale BM, Chen W, et al. The IMAGE project: methodological issues for the molecular genetic analysis of ADHD. Behav Brain Funct. 2006;2:27. doi: 10.1186/1744-9081-2-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Conners CK. Conners' Rating Scales-Revised: Technical Manual. MHS; 2003. Sixth Printing. [Google Scholar]
- 21.Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry. 1997 Jul;38(5):581–6. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- 22.Taylor E, Schachar R, Thorley G, et al. Conduct disorder and hyperactivity: I. Separation of hyperactivity and antisocial conduct in British child psychiatric patients. Br J Psychiatry. 1986 Dec;149:760–7. doi: 10.1192/bjp.149.6.760. [DOI] [PubMed] [Google Scholar]
- 23.Berument SK, Rutter M, Lord C, et al. Autism screening questionnaire: diagnostic validity. Br J Psychiatry. 1999 Nov;175:444–51. doi: 10.1192/bjp.175.5.444. [DOI] [PubMed] [Google Scholar]
- 24.Henderson SE, Sugden DA. Manual Movement Assessment Battery for Children. The Psychological Corporation; 1992. [Google Scholar]
- 25.Pitcher TM, Piek JP, Hay DA. Fine and gross motor ability in males with ADHD. Dev Med Child Neurol. 2003 Aug;45(8):525–35. doi: 10.1017/s0012162203000975. [DOI] [PubMed] [Google Scholar]
- 26.Nijhuis-van der Sanden RW, Smits-Engelsman BC, Eling PA. Motor performance in girls with Turner syndrome. Dev Med Child Neurol. 2000 Oct;42(10):685–90. doi: 10.1017/s0012162200001262. [DOI] [PubMed] [Google Scholar]
- 27.Schoemaker MM, Smits-Engelsman BC, Jongmans MJ. Psychometric properties of the movement assessment battery for children-checklist as a screening instrument for children with a developmental co-ordination disorder. Br J Educ Psychol. 2003 Sep;73(Pt 3):425–41. doi: 10.1348/000709903322275911. [DOI] [PubMed] [Google Scholar]
- 28.Rossum JHA, Vermeer A. Manual supplelment competentie belevingsschaal kinderen (CBSK) Motorische Competentie-Zelfbeoordeling; 2000. [Google Scholar]
- 29.Pitcher TM, Piek JP, Hay DA. Fine and gross motor ability in males with ADHD. Dev Med Child Neurol. 2003 Aug;45(8):525–35. doi: 10.1017/s0012162203000975. [DOI] [PubMed] [Google Scholar]
- 30.Hoza B, Pelham WE, Milich R, et al. The self-perceptions and attributions of attention deficit hyperactivity disordered and nonreferred boys. J Abnorm Child Psychol. 1993 Jun;21(3):271–86. doi: 10.1007/BF00917535. [DOI] [PubMed] [Google Scholar]