Abstract
Obesity is one of the top health priorities in the United States. Primary care physicians are the designated “gatekeepers” for obesity prevention, detection, and treatment. However, they and the current U.S. health care structure and reimbursement systems are often ill-equipped to implement evidence-based obesity care. The Group Lifestyle Balance™ (GLB) program is a group-delivery adaptation of the predominantly one-on-one lifestyle intervention proven efficacious in the Diabetes Prevention Program (DPP) trial. Participant intervention goals are 7% weight loss and sustained moderate physical activity of 150 minutes or more each week. Sequential instruction and coaching encompasses nutrition, behavior modification, and physical activity principles. The E-LITE (Evaluation of Lifestyle Interventions to Treat Elevated Cardiometabolic Risk in Primary Care) trial evaluates the feasibility and potential effectiveness of delivering the GLB program, supplemented with food tasting and supervised physical activity during each of 12 group sessions, and electronic communication for long-term follow up, in a primary care setting. Benefits and potential areas for improvement in three areas of implementation emerged during the 15-month E-LITE trial: (1) delivery of an established lifestyle intervention program by specialized professionals, (2) integration of a lifestyle intervention program into a primary care clinic, and (3) information technology use in a primary care-based lifestyle intervention program. Our experience shows the feasibility of implementing an evidence-based lifestyle intervention program combining group-delivered nutrition and behavioral counseling, physical activity training, and technology-mediated follow-up in a primary care clinic setting, but challenges remain, and we offer possible solutions to overcome them.
Introduction
Approximately 68% of U.S. adults are overweight or obese (1), and the prevalence of obesity-related risk factors for diabetes and cardiovascular disease (CVD) continues to increase (2). Owing to its tremendous personal, societal, and economic burdens (3–6), obesity is one of the nation’s top health priorities.
Modest, sustained weight loss of 5–10% has been shown to delay or possibly prevent diabetes (7,8), and improve CVD risk factors such as abnormal blood pressure and lipids (9–12). Concerted, sustainable efforts are needed to prevent and treat obesity, not just its complications. The US Preventive Services Task Force recommends intensive lifestyle interventions to promote sustained weight loss for obese adults (13). Central to these recommendations are intensive lifestyle interventions that encompass counseling for a balanced-nutrient, energy-deficit diet, increased physical activity, and behavior modification (14–16).
Primary Care Providers (PCPs) are the designated “gatekeepers” for obesity prevention, detection, and treatment (16). However, PCPs often lack the training, skills, confidence, and time required to implement effective lifestyle interventions (17), and primary care delivery models often lack the required structure and organization for obesity prevention and treatment (18). Furthermore, the current U.S. health care system’s acute care orientation, structure of physician visits and reimbursement, and reluctance to reimburse for non-physician services contributes to the neglect of chronic and preventive care (19–21). As a result, obesity is undertreated, if not mistreated, in clinical practice, despite the existence of efficacious treatments and evidence-based guidelines (22–27).
Changes in federal health policy in the form of the Affordable Care Act (ACA) (28) require that Medicare and new private health plans provide evidence-based preventive services, including weight management for the obese, without cost-sharing (i.e. deductibles, coinsurance, or copayments). While physician counseling can facilitate weight loss attempts among obese patients (29), PCPs can rarely provide weight management interventions of sufficient intensity (30). Instead, the US Preventive Services Task Force suggests they refer patients for such care (13). The most common referral for weight management is to registered dietitians. Although the Affordable Care Act will increase access to this service, current evidence fails to support the efficacy of intermittent, low- to moderate-intensity counseling by dietitians (13,16,30).
The Diabetes Prevention Program (DPP) trial demonstrated that an intensive lifestyle intervention - focusing on 7% weight loss, and sustained moderate intensity physical activity of 150 minutes or more a week - reduced the risk for developing type 2 diabetes by 58%, and metabolic syndrome by 41% (7,31,32). Materials that focus on diet, physical activity, and behavior change were developed at the University of Pittsburgh by the DPP Lifestyle Resource Core, and used in 16 Lifestyle Coach-led one-on-one “core curriculum” sessions and a number of subsequent individual and group maintenance sessions (33).
The university’s Diabetes Prevention Support Center (DPSC) adapted the 16-individual session core curriculum to a 12-session weekly group delivery format called the Group Lifestyle Balance™ (GLB) program for broader dissemination (34), and also developed a DVD version of the program for at-home use. Since the development and implementation of the E-LITE (Evaluation of Lifestyle Interventions to Treat Elevated Cardiometabolic Risk in Primary Care) protocol, the DPSC added 10 more sessions to extend the GLB program to 12 months. The GLB promotes the same goals for weight loss and physical activity as the DPP intervention. To achieve the recommended weight loss of 1–2 pounds/week, moderate calorie and fat intake reductions through healthy substitutions and portion control, rather than omission or elimination of specific foods, are advocated. Sustained physical activity is encouraged to assist with weight loss, and more importantly, for long-term weight maintenance. The DPSC has established a comprehensive infrastructure for Lifestyle Coach training, program material dissemination, and support for the GLB program.
Several nonrandomized prospective intervention studies have reported on the feasibility and potential effectiveness of the GLB program in primary care settings (34,37–39). The E-LITE (Evaluation of Lifestyle Interventions to Treat Elevated Cardiometabolic Risk in Primary Care) study is the first randomized controlled trial to evaluate the feasibility and potential effectiveness in reducing BMI of an adaptation of the GLB program in a primary care setting (35,36). This paper reports the lessons learned from the perspective of the study dietitian, study physician, and investigators. Our objective is to inform dissemination of effective weight management programs likely to be reimbursed under the Affordable Care Act, based on our experience implementing the class-based intervention.
The E-LITE Modifications to the Group Lifestyle Balance Program
The E-LITE trial was designed to compare a GLB in-person group intervention and a GLB DVD self-directed intervention with usual care. The Palo Alto Medical Foundation (PAMF) IRB approved the study protocol. In this report we discuss our experience with integrating the in-person class into primary care. At baseline, the mean age of participants (n = 241) was 52.9 (SD10.9) years, with 47% female, 78% Non Hispanic White, 17% Asian/Pacific Islander, and 4% Hispanic. The mean BMI was 32.0 kg/m2 (SD 5.4). Approximately 54% of participants had impaired fasting glucose, 87% metabolic syndrome, and 41% both conditions. The main objective of the trial is to evaluate the GLB program, with modifications, in a primary care setting, rather than a research clinic. As such, the program was implemented in a 29-physician primary care clinic of the PAMF, where participants receive their general medical care. PAMF is a large, community-based, multispecialty group practice that is a certified Patient Centered Medical Home. It provides integration of health care services and patient information through a fully-functional electronic health record (EHR). The EHR facilitates coordination of care, patient referrals, and communication among health care providers, as well as between providers and their patients through secure messaging.
The adaptation implemented in this trial retained all the key attributes of the core 12-session GLB program. E-LITE classes were delivered by a Lifestyle Coach, who is a registered dietitian and received the DPSC’s GLB training certification. Classes were sequential, provided information and support, and followed the DPP content. This content includes basic nutrition concepts encompassing eating a balanced, lower calorie, lower fat diet to enable weight loss, spontaneous and planned physical activity, and behavior modification problem solving and relapse prevention skills (Table 1). Participants were provided with weekly handouts, a commercially available calorie- and fat gram-counting book, and self-monitoring booklets for logging food intake, calorie and fat grams, steps, and minutes of planned physical activity. To facilitate self-monitoring, each participant was also given a pedometer and bathroom and food scales. Weekly feedback and encouragement was provided by the Lifestyle Coach, based on participant logged information. DVDs containing professional actors enacting the classes were available for viewing by participants who missed a class.
Table 1.
Weekly group session topics for GLB core program and E-LITE weekly physical activity sessions.
| Session | GLB Core Program | E-LITE Physical Activity |
|---|---|---|
| 1 | Welcome Getting Started Losing Weight | Introduction to Physical Activity Basic Stretches |
| 2 | Be a Fat and Calorie Detective | Establishing a Baseline: Timed Walk |
| 3 | Healthy Eating | Different Ways to Move |
| 4 | Move Those Muscles | Monitoring Your Intensity |
| 5 | Tip the Calorie Balance | Flexibility |
| 6 | Take Charge of What’s Around You | Checking Your Progress: Timed Walk |
| 7 | Problem Solving | Functional Fitness |
| 8 | Four Keys to Healthy Eating Out | Core and Balance Training |
| 9 | The Slippery Slope of Lifestyle Change | Strength Training |
| 10 | Jump Start Your Activity Plan | No Excuses |
| 11 | Make Social cues Work for You | Design Your Own Circuit |
| 12 | Ways to Stay Motivated | Celebration: Timed Walk |
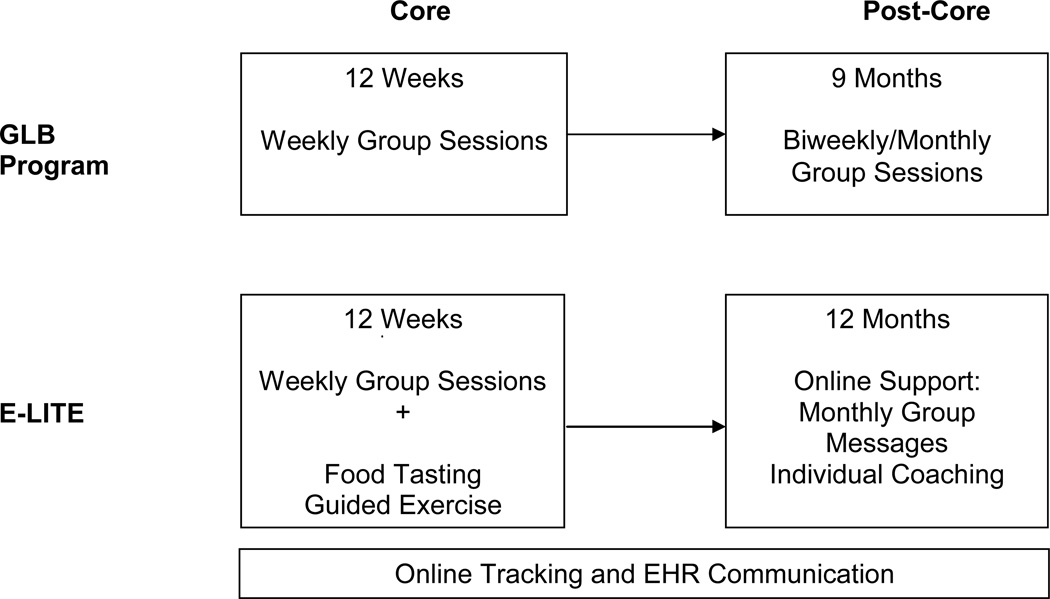
With approval of the DPSC, we supplemented the GLB program with (1) weekly food tasting and supervised physical activity for class participants, and (2) utilization of an electronic health record (EHR) for patient-provider communication, and online logging of physical activity and weight (Figure 1).
Figure 1.
Comparison of GLB program to a modified GLB program, as delivered in the E-LITE trial.
To expose individuals to healthy food options, in each of the first 6 sessions, the Lifestyle Coach offered samples of bought moderate calorie/moderate fat foods, such as low calorie beverages, lower calorie/lower fat salad dressings, dairy, and snack foods, and a variety of fruits and vegetables. Participants shared their own new discoveries or favorite healthy foods during the last 6 sessions.
After the nutrition/behavior change core content in each class, an exercise specialist provided demonstration and guided practice of exercises using a circuit design, with information sharing and participant discussion before, during, and after the circuit training. Each module lasted 30–45 minutes and focused on one or more of the components of a balanced physical fitness program, including aerobic, strength, and flexibility training (Table 1).
Following completion of the 12-week core program, individual communication continued for 12 months through EHR-integrated secure messaging between the Lifestyle Coach and participants to support long-term behavior change. Participants received monthly group messages that reviewed and expanded on topics from the core GLB curriculum. In addition, the Lifestyle Coach contacted participants individually to check on progress and offer assistance with lifestyle changes. When necessary, the exercise specialist was also available for consultations through the EHR.
Participants were advised to log their daily planned physical activity, steps, and weight on the American Heart Association’s Heart360™, an online heart health resource and self-monitoring website (www.hearthub.org). Although they also logged this information in paper tracking booklets, online availability allowed the Lifestyle Coach, with participant permission, to monitor individual progress through shared access.
Lessons Learned
Below, we discuss the benefits and potential areas for improvement in three areas of implementation in primary care of the GLB program with supplementation as described above (Table 2).
Table 2.
Lessons learned from the implementation of a modified GLB program, as delivered in the E-LITE trial, including observed benefits and potential areas of improvement
| Lessons Learned | Observed Benefits | Potential Areas for Improvement |
|---|---|---|
| Delivery of an evidence-based lifestyle intervention program by specialized professionals |
|
|
| Integration of an evidence-based lifestyle intervention program into primary care |
|
|
| Information technology in an evidence-based lifestyle intervention program |
|
|
Delivery of an Evidence-based Lifestyle Intervention Program by Specialized Professionals
The GLB program is an evidence-based structured lifestyle intervention program that is nationally available, and supported by the DPSC. Lifestyle Coach training for program delivery is provided by the DPSC or DPSC certified local Master Trainers. Professionals from a variety of health care disciplines are trained as Lifestyle Coaches, but the majority are dietitians and nurses. The curriculum, including Lifestyle Coach scripts, participant handouts (written in English at a 5th grade reading level), and DVDs is available from the DPSC, therefore eliminating the need for in-house course development and training. The standardized training and program materials help ensure consistent implementation across a variety of settings.
Although the GLB program is structured for use with individuals of various educational backgrounds, E-LITE participants were almost universally college-educated, with 97% of the individuals having attained education at the college level or above. The Lifestyle Coach was a registered dietitian, with more than 10 years of weight management counseling experience, who was trained at the DPSC’s 2-day GLB training session, and later certified as a Master Trainer. The exercise specialist worked as a personal trainer, and had considerable experience with overweight/obese individuals. Having professionals with experience well beyond the minimum required was beneficial for this patient population, as they were able to answer participant questions that might not have been anticipated in less educated populations (e.g., questions regarding dietary fat quality, diet myths, media coverage of nutrition topics, and exercise modifications for physical limitations). Working together, the Lifestyle Coach and exercise specialist embedded the supplemented components (food tasting, physical activity instruction and practice, and computer technology tools for online logging and secure messaging) within the GLB class structure, and delivered it as an integrated program.
Barriers encountered during program delivery were primarily related to participant adherence, including class attendance, logging of food intake, weight, and physical activity, completion of home assignments, and engaging in regular planned physical activity. Although 86% of participants attended or made up at least 10 class sessions, and 96% at least 6 sessions, compliance with logging was modest. Forty-nine percent of participants completed food records for at least 10 weeks, but 10% completed none. Twenty-nine percent of participants completed weight records and 38% kept physical activity records for at least 10 weeks, but 6% did not complete any. Participants identified time constraints as the primary challenge to meeting program requirements and goals. Participant adherence is a known problem in behavioral intervention programs, and an active area of research.
Based on our experience, additional motivational strategies to increase adherence may improve participants’ experience and motivation, and promote long-term success. One strategy that was not part of the E-LITE implementation given the research design, but would be realistic in clinical practice, is to involve support from program participants’ PCPs at and between routine office visits to provide encouragement and reinforce sustained adherence (further discussed below) (Table 2).
Integration of an Evidence-based Lifestyle Intervention Program into Primary Care
In contrast to most weight management interventions, which occur in commercial settings or registered dietitian offices, the E-LITE classes were held in a primary care clinic. In addition to being a convenient location for participants to access (since it was the site at which they received their primary care), offering these classes in a medical facility conveyed to participants that the health care system endorsed the benefits of lifestyle changes. Although not a concern in the E-LITE trial, the safety of the clinic location (especially at night), might need to be taken into consideration.
Class sessions were conducted in the evening, after normal clinic hours. The core nutrition/behavior change portion of the class was held in a conference room, whereas the exercise circuit was performed in a waiting area. Limitations of this locale were a conference room of insufficient size to comfortably accommodate larger classes (class size ranged from 7–16 participants), and the need to perform the exercise circuits in a waiting area. The configuration and small size of the waiting room, as well as restricted storage facilities for exercise equipment, limited the exercise modules, and evening clinical staff sometimes came through this area during class. Space is likely limited in most busy primary care clinics, which needs to be taken into account when planning class capacity and schedule.
Since PAMF, including its primary care departments, utilizes a state-of-the-art EHR system (Epic, Madison, WI), this was used to identify a pool of potentially appropriate patients. PCPs received a list of their own patients from this pool, and served as the gatekeeper for referral to the E-LITE study. Housing this program in a primary care clinic allowed PCPs to easily refer patients for participation, and communicate with the Lifestyle Coach and exercise specialist. As needed, the Lifestyle Coach communicated patient health concerns to the PCPs through the EHR. Messages exchanged between the patient and Lifestyle Coach became part of the permanent EHR, and could be viewed by other health care providers on the patient’s care team. While the E-LITE trial had the luxury of using an EHR, other modes of communication between care providers are available (e.g., in person, telephone).
PCPs can support and encourage patients as they attempt lifestyle changes. However, as physicians were blinded in this study, they were not provided the tools to do this. In a real life situation, participant class attendance and progress, as well as program information and content, could be made available to physicians. This would allow them to support and reinforce the goals of the program, and endorse the benefit of regular class attendance, during any patient appointment.
Based on our experience, potential areas of improvement include active physician support of patient participation in a lifestyle education program, as well as adequate facilities for class discussions and exercise circuits (Table 2).
Information Technology in an Evidence-based Lifestyle Intervention Program
Recent advances in information technology allowed for a GLB program with supplemental online communication and participant logging. The Lifestyle Coach and exercise specialist had access to participant online logs of planned physical activity, pedometer-logged steps, and weight throughout the 15-month extended program. All food records, however, were kept manually, and were only available during the 12-week class.
The EHR used at PAMF supports sending messages to a group of patients simultaneously, which allowed for easy dissemination of information in the form of group messages once a month for one year after completion of the core class. The messages provided review and expansion of topics covered in the core curriculum, and asked participants to reply to the Lifestyle Coach with updates on progress, barriers, and current lifestyle goals. However, the average reply rate was only 1.5 replies per participant over the 12 month follow-up period. In addition to the group messages, the Lifestyle Coach sent an average of four messages per participant asking for progress updates, but received an average of only 1.8 replies. Participants themselves only initiated an average of 0.5 messages over one year. These rates of participation in online communication were lower than anticipated, and the time commitment for the Lifestyle Coach and exercise specialist less than expected. Some participants indicated that they preferred the in-person group support, rather than online messaging, to maintain motivation for ongoing weight management.
Despite the benefits realized with the information technology available at the time of the study, there were technical limitations. With the available EHR it was not possible to send materials beyond typed messages. Patient handouts require prior organizational review and approval, and the use of web links and interactive activities is not supported. As a result, we had to choose a separate stand-alone application for participant self-monitoring and sharing of data with the Lifestyle Coach, which could have been a barrier to adherence. Heart360 is a freely available patient-self-management website maintained by the American Heart Association, and has won numerous technology innovation awards. However, it does not support tracking of dietary intake, which precluded the Lifestyle Coach having access to diet records after the 12-week class had ended.
Based on our experience, several areas of improvement were identified. Building screening parameters to identify potentially appropriate candidates for the program into the EHR would provide PCPs with a tool to assist with patient referrals. Documenting class attendance and measured weight in the EHR would allow PCPs to monitor patient progress, and is possible with the EHR used, but was not done in our study. Furthermore, to expand the ability of clinicians to provide ongoing management for obesity, it could be useful for GLB data (e.g., body weight measurements taken on a home scale, or step measurements from a pedometer) to be directly uploaded to the EHR. Having participants log not only physical activity and weight, but also dietary intake, on an electronic device, where information is readily shared with a Lifestyle Coach via the internet, could allow for feedback and guidance beyond the 12-week class. Expanding EHR secure messaging capabilities for sending materials beyond simple messages could enhance patient learning and engagement in lifestyle change. Online support groups might also enhance the experience and potency of the intervention (40) (Table 2).
Conclusions
Obesity is a chronic disease that requires concerted, sustained, evidence-based interventions for treatment. Although PCPs have a central role in diagnosing and overseeing obesity management, they cannot be expected to provide long-term, high intensity, effective therapy. An established weight management program based on integrating nutrition, physical activity, and behavior modification therapy, and delivered by allied health professionals, can provide this treatment. Furthermore, a mature EHR system can help identify eligible patients, support and enhance patient success through secure online messaging, and provide an efficient means of communication among health care providers.
The GLB program is based on interventions proven to be efficacious in the multicenter randomized controlled DPP trial. The modified GLB offered in the E-LITE trial provides lessons regarding the potential feasibility and effectiveness of delivering a nutrition and physical activity lifestyle intervention program in a primary care clinic setting.
Our experience shows that an established weight control program supplemented with food tasting and physical activity opportunities as well as online communication tools can be offered in a primary care clinic setting. We have identified strategies that may be crucial to overcoming the identified challenges encompassing active physician support of participant adherence, appropriate space for group sessions, and optimum use of available information technology.
Acknowledgments
We are indebted to the following individuals who made substantial contributions to the E-LITE study: Amy L. Muzaffar, MD (study physician); Lan Xiao, PhD (biostatistician); Rachel Press, BA (exercise specialist); Veronica Luna, BS (project coordinator); and Alicia Geurts, BS, Elizabeth Jameiro, MD, and Debbie Miller, BS (research assistants). Special thanks go to the E-LITE Data and Safety Monitoring Board and study participants and their families who made this study possible. We also would like to acknowledge the Diabetes Prevention Support Center of the University of Pittsburgh for training and support in the Group Lifestyle Balance™ program; the current program is a derivative of this material. Dr. Stafford reports that he has provided consulting services to Mylan Pharmaceuticals in the past. The remaining authors declare that they have no competing interests. The E-LITE study was supported by Grant No. R34DK080878 from the National Institute of Diabetes and Digestive and Kidney Diseases, a Scientist Development Grant award (0830362N) from the American Heart Association, and internal funding from the Palo Alto Medical Foundation Research Institute (PAMFRI). Dr. Wilson was a coinvestigator on this study; all contributors except Dr. Rosas received support from this grant. Dr. Stafford was supported by Grant No. K24HL086703 from the National Institutes of Health, Lung and Blood Institute. PAMFRI was the employer and part of the health care delivery system in which the study was conducted. PAMFRI has no financial interest in the outcomes of the study. Contributors Blonstein, Yank, Wilson, and Ma received salary support from PAMFRI or (in the case of Yank) through a postdoctoral fellowship at Stanford University School of Medicine funded by PAMFRI. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the American Heart Association. No sponsor or funding source had a role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the article.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults 1999–2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Mozumdar A, Liguori G. Persistent increase of prevalence of metabolic syndrome among U.S. adults: NHANES III to NHANES 1999–2006. Diabetes Care. 2011;34(1):216–219. doi: 10.2337/dc10-0879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood) 2009;28(5):w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 4.Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 5.Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med. 2003;138(1):24–32. doi: 10.7326/0003-4819-138-1-200301070-00008. [DOI] [PubMed] [Google Scholar]
- 6.Thompson D, Edelsberg J, Colditz GA, Bird AP, Oster G. Lifetime health and economic consequences of obesity. Arch Intern Med. 1999;159(18):2177–2183. doi: 10.1001/archinte.159.18.2177. [DOI] [PubMed] [Google Scholar]
- 7.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344(18):1343–1350. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- 9.Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003;289(16):2083–2093. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]
- 10.Pi-Sunyer X, Blackburn G, Brancati FL, Bray GA, Bright R, Clark JM, et al. Reduction i n weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one- year results of the look AHEAD trial. Diabetes Care. 2007;30(6):1374–1383. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stevens VJ, Obarzanek E, Cook NR, Lee IM, Appel LJ, Smith West D, et al. Long-term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase II. Ann Intern Med. 2001;134(1):1–11. doi: 10.7326/0003-4819-134-1-200101020-00007. [DOI] [PubMed] [Google Scholar]
- 12.Wing RR. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med. 2010;170(17):1566–1575. doi: 10.1001/archinternmed.2010.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.US Preventive Services Task Force. Screening for obesity in adults: recommendations and rationale. Ann Intern Med. 2003;139(11):930–932. doi: 10.7326/0003-4819-139-11-200312020-00012. [DOI] [PubMed] [Google Scholar]
- 14.Bray GA, Wilson JF. In the clinic. Obesity. Ann Intern Med. 2008;149(7):ITC4-1– ITC4-15. doi: 10.7326/0003-4819-149-7-200810070-01004. quiz ITC4-6. [DOI] [PubMed] [Google Scholar]
- 15.Kushner RF. Roadmaps for clinical practice: case studies in disease prevention and health promotion -- assessment and management of adult obesity: a primer for physicians. Chicago, IL: American Medical Association; 2003. [Google Scholar]
- 16.NHLBI. Practical Guide to the Identification, Evaluation and Treatment of Overweight and Obesity in Adults. Bethesda, MD: Public Health Service, U.S. Department of Health and Human Services; 2000. Oct, Report No.: NIH Publication No. 00-4084. [Google Scholar]
- 17.Kushner RF. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prev Med. 1995;24(6):546–552. doi: 10.1006/pmed.1995.1087. Epub 1995/11/01. [DOI] [PubMed] [Google Scholar]
- 18.Ostbye T, Yarnall KS, Krause KM, Pollak KI, Gradison M, Michener JL. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3(3):209–214. doi: 10.1370/afm.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bergeson SC, Dean JD. A systems approach to patient-centered care. JAMA. 2006;296(23):2848–2851. doi: 10.1001/jama.296.23.2848. [DOI] [PubMed] [Google Scholar]
- 20.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 21.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 22.Ma J, Urizar GG, Jr, Alehegn T, Stafford RS. Diet and physical activity counseling during ambulatory care visits in the United States. Prev Med. 2004;39(4):815–822. doi: 10.1016/j.ypmed.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 23.Ma J, Xiao L. Assessment of body mass index and association with adolescent preventive care in U.S. outpatient settings. J Adolesc Health. 2009;44(5):502–504. doi: 10.1016/j.jadohealth.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 24.Ma J, Xiao L, Stafford RS. Underdiagnosis of obesity in adults in US outpatient settings. Arch Intern Med. 2009;169(3):313–414. doi: 10.1001/archinternmed.2008.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ma J, Xiao L, Stafford RS. Adult obesity and office-based quality of care in the United States. Obesity (Silver Spring) 2009;17(5):1077–1085. doi: 10.1038/oby.2008.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stafford RS, Farhat JH, Misra B, Schoenfeld DA. National patterns of physician activities related to obesity management. Arch Fam Med. 2000;9(7):631–638. doi: 10.1001/archfami.9.7.631. [DOI] [PubMed] [Google Scholar]
- 27.Stafford RS, Radley DC. National trends in antiobesity medication use. Arch Intern Med. 2003;163(9):1046–1050. doi: 10.1001/archinte.163.9.1046. [DOI] [PubMed] [Google Scholar]
- 28.Patient Protection and Affordable Care Act, Pub. L. No. 111-148 Stat. 124 STAT. 119. 2010. Mar 23, [Google Scholar]
- 29.Kreuter MW, Chheda SG, Bull FC. How does physician advice influence patient behavior? Evidence for a priming effect. Arch Fam Med. 2000;9(5):426–433. doi: 10.1001/archfami.9.5.426. [DOI] [PubMed] [Google Scholar]
- 30.Tsai AG, Wadden TA. Treatment of obesity in primary care practice in the United States: a systematic review. J Gen Intern Med. 2009;24(9):1073–1079. doi: 10.1007/s11606-009-1042-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Orchard TJ, Temprosa M, Goldberg R, Haffner S, Ratner R, Marcovina S, et al. The effect of metformin and intensive lifestyle intervention on the metabolic syndrome: the Diabetes Prevention Program randomized trial. Ann Intern Med. 2005;142(8):611–619. doi: 10.7326/0003-4819-142-8-200504190-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wing RR, Hamman RF, Bray GA, Delahanty L, Edelstein SL, Hill JO, et al. Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obes Res. 2004;12(9):1426–1434. doi: 10.1038/oby.2004.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Diabetes Prevention Program Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25(12):2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kramer MK, Kriska AM, Venditti EM, Miller RG, Brooks MM, Burke LE, et al. Translating the Diabetes Prevention Program: a comprehensive model for prevention training and program delivery. Am J Prev Med. 2009;37(6):505–511. doi: 10.1016/j.amepre.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 35.Ma J, King AC, Wilson SR, Xiao L, Stafford RS. Evaluation of lifestyle interventions to treat elevated cardiometabolic risk in primary care (E-LITE): a randomized controlled trial. BMC Fam Pract. 2009;10:71. doi: 10.1186/1471-2296-10-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yank V, Stafford RS, Wilson SR, Xiao L, Luna V, Ma J. Global Obesity Summit. Mississippi: Jackson; 2010. Nov 9–11, Baseline Data from an RCT of Obesity Management in Primary Care. [Google Scholar]
- 37.Kramer MK, Miller R, Venditti E, Orchard TO. Group lifestyle intervention for diabetes prevention in those with metabolic syndrome in primary care practice. Diabetes Care. 2006;55(suppl):A517. [Google Scholar]
- 38.McTigue KM, Conroy MB, Bigi L, Murphy C, McNeil M. Weight loss through living well: translating an effective lifestyle intervention into clinical practice. Diabetes Educ. 2009;35(2):199–204. 208. doi: 10.1177/0145721709332815. [DOI] [PubMed] [Google Scholar]
- 39.Seidel MC, Powell RO, Zgibor JC, Siminerio LM, Piatt GA. Translating the Diabetes Prevention Program into an urban medically underserved community: a nonrandomized prospective intervention study. Diabetes Care. 2008;31(4):684–689. doi: 10.2337/dc07-1869. [DOI] [PubMed] [Google Scholar]
- 40.Lorig KR, Ritter PL, Laurent DD, Plant K. Internet-based chronic disease self- management: a randomized trial. Med Care. 2006;44(11):964–971. doi: 10.1097/01.mlr.0000233678.80203.c1. [DOI] [PubMed] [Google Scholar]