Abstract
Background
Proposing a strategy for sellar reconstruction in endoscopic transsphenoidal transsellar approachfor pituitary adenoma.
Methods
240 patients with pituitary adenoma underwent pure endoscopic endonasal transsphenoidal surgery.Intra-operative CSF leaks were classified as grade 0, no observable leak; grade 1, CSF dripping through anarachnoid membrane defect of less than 1 mm; and grade 2, CSF flowing through an arachnoid defect of morethan 1 mm. Sellar reconstruction was performed according to our staging system; in stage I, the defect was coveredwith oxidized cellulose and sphenoid sinus filled up with Gelfoam. In stage II, a layer of fat was appliedon the defect and fascia lata placed epidurally. In stage III, one or two layers of fascia were used with addingsurgical glue and/or lumbar drainage. Mucosa of sphenoid sinuses was kept intact as much as possible and approximatedat the end of procedure.
Result
intra-operative CSF leaks grade 0, 1 and 2 resulted in 133(55.4%), 78 (32.5%) and 29(12.1%) patients,respectively. Stage I of reconstruction was used in 126 patients (52.5%) with no intra-operative CSF leak orsever prolapse of arachnoid membrane. Stage II was performed in 80 patients (33.3%) with either leak grade 1(73 patients) or grade 0 with severe prolapse of the suprasellar components induced in the sella (2 cases) or inwhom extra-pseudocapsular dissection performed (5 cases). Stage III was performed in 34 cases (14.2%) witheither CSF leak grade 2 (29 patients) or grade 1 with simultaneous severe destruction or removal of sellar floorlaterally, superiorly or inferiorly (5 patients) which made it impossible to place the fascia underlay to the bone.A minimum of 18 months follow-up showed development of 2 CSF leaks (0.8%), one pneumocephalus (0.4%)and 2 meningitis (0.8%) cases.
Conclusion
Given the low postoperative CSF leak rate, we demonstrated that our adopted sellar reconstructionstrategy focusing mostly on the adopted intra-operative CSF leak grading system is safe and useful forovercoming devastating complications like postoperative CSF leaks.
Keywords: Endoscopic transsphenoidal surgery, reconstruction, cerebrospinal fluid leak
Introduction
Postoperative cerebrospinal fluid (CSF) leak is still the most serious complication of the transsphenoidal approaches to pitui tary adenoma with the rate of 0 to 27% (1). The CSF Leak predisposes the patients to life-threatening bacterial contamination that can lead to serious infections, especially meningitis (2-6). For many years, sellar reconstruction has been postulated as a crucial step in this approach to overcome such complications. However, there is still a lot of controversy regarding reconstruction techniques, graft materials and the necessity of reconstruction in every case (2-5,7). As an intra-operative CSF leak is an imperative predictive factor for developing a postoperative leak, and several authors now suggest that this should be considered as a factor to determine whether sellar reconstruction is needed (2,7-11). So far several intra-operative CSF leak grading systems have been suggested according to the size of arachnoid defect or CSF flow (7,10,11). In this study, we explain the intra-operative CSF leak grading system used in the research and the staging devised for sellar reconstruction following endoscopic transsphenoidal transsellar approach for pituitary adenoma along with the results of this strategy.
Methods
Study population: Between April 2006 and April 2011, 240 patients with pituitary adenoma with endoscopic transsphenoidal transsellar procedure were enrolled in the study. Patients who underwent extended approaches were excluded from the study; however the cases in which tuberculum sellar bone was removed (without the planum sphenoidale removal) were included in the analysis. The ethics committee of ENTHead and Neck research center approved the study, and written informed consent was preoperatively obtained from the patients. The same neurosurgeon and otolaryngologist performed the procedures. We perioperatively administered prophylactic antibiotic regimens for the patients. All patients were followed up for at least 18 months.
Surgical technique: After the infiltration of xylocaine (1%) with Epinephrine (1/100,000), the adenomas were removed through a purely endoscopic endonasal transsphenoidal transsellar approach, using a rigid endoscope, pituitary ring curettes and suctions.
To reach the sphenoid sinus, we used a monostril or binostril transseptal approach via a septal mucosal incision 2 mm anterior to the rostrum and up to 5 mm posterior septectomy, respectively. After partial removal of the anterior face of the sphenoid sinus, the sphenoid mucosa was incised to reach the sinus. Removal of sphenoid rostrum added more space posteriorly thus alleviate the need for larger posterior septectomy. After removing the inter-sinus septum and the localization of the sella, the mucosa of the posterior wall of the sinus covering the sella was pushed laterally to expose the sellar floor bone. The mucosal layer was thereby kept untouched as much as possible in the other parts of the sinus. Wherever possible, extra pseudo-capsular dissection was performed via a bimanual microsurgical technique and using the binostril approach. Angled endoscopes (mostly 30 degrees) were used to remove any suprasellar, lateral or inferior extension of the tumor. At the end of the procedure, reconstruction of the sella was performed according to degree of CSF leak and our devised staging system.
a-Intra-operative CSF leakage grading system: The adopted grading system of intraoperative CSF leak was somehow similar to Kelly’s classification (7). In this grading system, cases with no observable leak were considered as grade 0; if CSF was obviously dripping or there was an arachnoid membrane defect of less than 1 mm; as grade 1and if there was a stream of CSF through an arachnoid defect of more than 1 mm; grade 2 (Table.1).
Table 1. Intra-operative CSF leak grading system in cranial base surgery .
| Grade of CSF leak | Description |
| Grade 0 | No observable CSF leak |
| Grade I | Obvious CSF dripping trough an arachnoid membrane defect of less than 1 mm |
| Grade II | Obvious CSF flow through an arachnoid defect of more than 1 mm |
Cerebrospinal fluid, CSF
b- Sellar reconstruction staging system: The proposed staging system for sellar reconstruction based on factors such as intraoperative CSF leak, floppiness of arachnoid membrane, the tumor removal technique, and characteristics of the bony defect which predictably contribute to postoperative complications (Algorhythm 1 and Table. 2).
Algorhythm 1 .
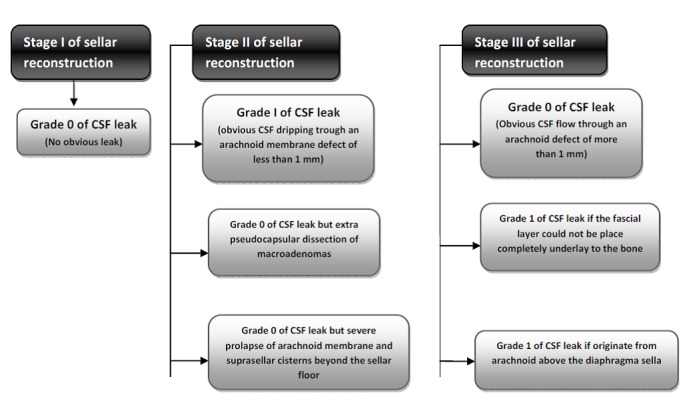
Staging of sellar reconstruction in cranial base surgery
Table 2. Sellar reconstruction staging in endoscopic transnasal approach .
| Staging | Reconstruction |
| Stage I |
1) Covering the defect with a layer of Surgicel +2) Filling sphenoid sinus with Gelfoam |
| Stage II |
1) A thin layer of fat on surgicel applying on arachnoid membrane defect +2) a layer of fascia underlay/to bone +3, 4) The same as stage I |
|
Stage III |
1) A thin layer of fat on surgicel applying on arachnoid membrane defect +2) One or two layer of fascia underlay/onlay to dura +3,4) The same as stage I +5) covering the surgicel layer with surgical glue +/- lumbar drain |
Stage I: In the absence of an intraoperative CSF leak (grade 0), the sellar floor was repaired using oxidized cellulose (Surgicel from Ethicon Inc, Somerville, NJ, USA), and the sphenoid sinus subsequently filled with Gelfoam (Fig.1).The exceptions were cases in whom extra pseudocapsular dissection performed or had severe prolapse of the arachnoid membrane and suprasellar cisterns out of sellar floor, which reconstructed according to stage II.
Stage II: this stage of reconstruction was mainly used in cases with grade 1 CSF leaks. In this stage, the arachnoid membrane was faced with a thin layer of fat applied to a small piece of Surgicel (the fat touching the arachnoid membrane). Then, a layer of fascia lata was placed as an underlay to the bone in the epidural space. Subsequently the graft was covered by Surgicel and the sphenoid sinus filled with Gelfoam (Fig.2). But there were two exceptions that when it encountered, patients with grade 1 CSF leak were reconstructed according to stage III. First, if the fascial layer could not be place underlay to the bone in situations like severe sellar bone destruction (ghost sella or sphenoid sinus invasion) or bone removal far laterally. Second, if leak happened due to the violation of the arachnoid above the diaphragm under the tuberculum sella which were mostly occur when bone removal extended to include tuberculum sella.
Stage III: Reconstruction in this stage was the same as stage II, except for the use of synthetic glue as a buttress over the grafts and/or the use of a lumbar drain for CSF diversion. If the arachnoid defect was more than 5 mm, an intradural layer of fascia was also applied. This stage of reconstruction was considered mainly for cases with a grade 2 CSF leak. Synthetic glue, N-butyl- 2-cyanoacrylate (Glubran 2, Viareggio, Italy), was applied as the final layer extracranially on the Surgicel layer and the sphenoid sinus filled with Gelfoam (Fig.3). Lumbar drainage adopted as an adjuvant therapy for very high output leaks since these leaks were considered to be more susceptible to continue postoperatively.
Fig.1 .
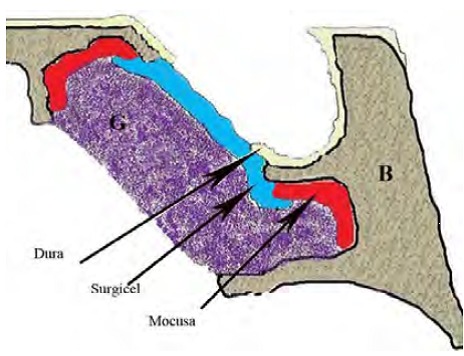
stage I of sellar floor reconstruction using surgicel; field is supported with Gelfoam; (B) bone, (G) Glubran
Fig.2 .
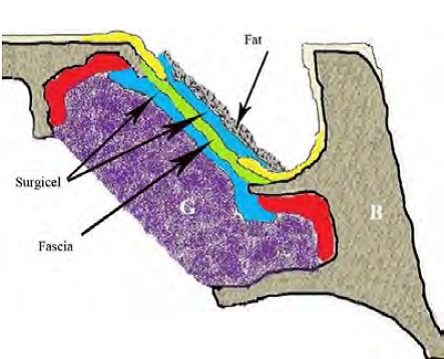
stage II of sellar floor reconstruction using layers of fat, surgicel, fascia and second layer of surgicel, respectively; field is also supported with Gelfoam; (B) bone, (G) Gelfoam
Fig.3 .
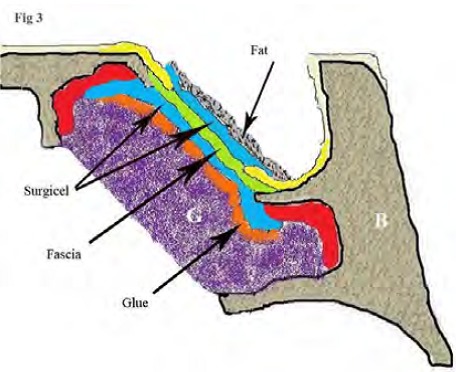
stage III of sellar floor reconstruction using layers of fat, surgicel, fascia, second layer of surgicel and finally a layer of glue; field is also supported with Glubran; (B) bone, (G) Gelfoam
In all cases, in order to decrease the dead space, Valsalva maneuver was performed at the end of tumor removal. To insure watertight closure, the field was checked with endoscope before applying the surgicel layer and no Valsalva maneuver was applied after the reconstruction. Sphenoid sinus mucosa was approximated as much as possible on the arachnoid layer or graft material (under the surgicel layer).We routinely used a light nasal packing for patients to prevent nasal blowing. Restriction of straining in all kinds (nasal blowing, weight lifting, bending, getting Mecca position, etc.) was completely discussed with the patient preoperatively and during first postoperative visit for nasal toileting one week postoperatively. Nasal packing was removed around day 3 postoperative and patients were discharged if remained uneventful within 24 hours thereafter. The patients were checked for nasal symptoms on week 2 and 4 and month 2 and 3 post-operatively and according to routine neurosurgical follow up visits thereafter.
Postoperative complications related to the adopted reconstruction strategies (including CSF leaks and meningitis) were evaluated in all patients.
Statistical analysis: Data are presented as number (frequency percentage, %) and means ± standard deviation. A p-value of less than .05 was considered significant. Statistical analyses were performed using SPSS 17 for Windows (SPSS Inc., Chicago, Illinois).
Results
We analyzed data from 112(46.7 %) male and 128 (53.3%) female patients, with a mean age of 39.4± 9.7 years (ranging from 16 to 73), who underwent pure endoscopic endonasal transsphenoidal surgery for pituitary adenomas. Nineteen (7.9 %) patients had a history of at least one previous conventional transsphenoidal surgery, and 11 (4.5 %) had at least one previous craniotomy. Among the 240 adenomas, 34 (14.1 %) were microadenoma and 206 (85.8 %) macroadenoma. The tumors included 117 (48.8 %) non-functional adenomas, and 123 (51.2%) functional ones.
Intra-operative CSF leak: One hundred and thirty three patients (55.4%) had CSF leaks of grade 0, 78 patients (32.5%) grade 1, and 29 patients (12%) grade 2. Stage I of reconstruction was used in 126 patients (52.5%) who had neither intra-operative CSF leak nor sever prolapse of arachnoid membrane. Stage II reconstruction was performed in 80 patients (33.3%) with either CSF leak grade 1 (73 patients) or grade 0 with a severe prolapse of the suprasellar components coming out of the sella (2 cases) or in whom extra-pseudocapsular dissection performed (5 cases). Stage III reconstruction was performed in 34 cases (14.2%) with CSF leak grade 2 (29 patients) or in cases with grade 1 CSF leak having severe destruction (ghost sella) or removal of sellar floor laterally or having leak originating from arachnoid above the diaphragm under the tuberculum sella (5 patients).
Outcomes: Postoperative CSF leaks developed in 2 cases (0.8%), both of them with grade 1 of intra-operative leak (reconstructed according to stage II) which was treated by lumbar drainage in one and revision endoscopic repair in the other. The latter case had a much vascularized tumor that made the neurosurgeon uncertain about the pathology. Therefore only biopsies were made and because of CSF leak grade 1, the sella was reconstructed according to stage 2. But the patient experienced vision deterioration due to intra lesional hemorrhage at the same night which led to trans-cranial resection of the tumor. The patient’s course of recovery went normal until he encounter with CSF rhinorrhea on day 8 post operatively and after sever nasal blowing since he missed the routine post-operative visit of otolaryngologist for nasal clearing.
There were 2 cases of post-operative meningitis (0.8%), one with grade 1 of intraoperative leak and the other one with grade 2. They had no obvious post-operative CSF leak in examination. Outbreak of Acinetobacter in ICU which led to one patient death but the other one successfully managed medically. Post-operative CSF leak or meningitis did not occurred again in the latter case in at least 2 years of follow up. We had no case of vision deterioration due to empty sella syndrome after the surgery.
Discussion
As the pituitary adenomas originate under the sellar diaphragm and out of the arachnoid membrane and subarachnoid space, transsphenoidal approach could be applied to resect these tumors usually without disrupting the arachnoid membrane and subsequent CSF leak (12).
The use of an endoscope makes a transsphenoidal approach much easier in large tumors with vast extensions. However, as with conventional transsphenoidal approach, devastating postoperative complications can occur, such as CSF leaks that predispose the patients to life-threatening infections including meningitis, encephalitis and pituitary abscesses (4,10,13,14).
Therefore, several strategies using different autologus or synthetic materials, techniques and instruments with different success rates have been suggested for repairing or reconstructing defects of the sellar floor to prevent postoperative CSF leak (1-4,7,11,10,15,16).
Fig. 4 .
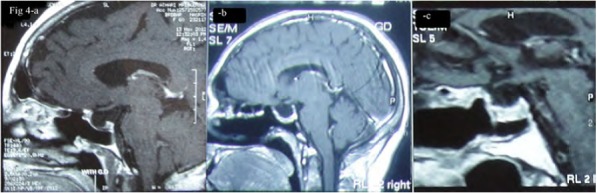
Postoperative MRI: sagittal views of postoperative sellar reconstruction: a) Stage I, b) Stage II and c) Stage III of sellar reconstruction
The postoperative CSF leak following microscopic or endoscopic transsphenoidal pituitary surgeries is described to be encountered in 0 to as high as 27% of procedures, with generally less than 5% (1,9,17,10). Various factors have been postulated to affect the likelihood of post-operative CSF leak including GH-secreting adenoma, old age, previous transsphenoidal surgery or radiotherapy and surgical experience, but arachnoid membrane violations and intraoperative CSF leak has been found to be the most important prognostic factors affecting the risk of postoperative CSF leaks that could increase the likelihood by 6 times (8-11,18).
In 2001 Kelly and colleagues (7) presented their experience regarding repair and reconstruction of the sellar floor according to the severity of the intra-operative CSF leak in microscopic endonasal transsphenoidal pituitary procedures. To reconstruct the sellar floor, they applied only collagen sponge in case of small “weeping” CSF leak and abdominal fat for relatively large arachnoid defects. In both level, they reinforced the sellar floor using titanium mesh afterward. Using this strategy they reported an overall postoperative CSF leaks of 3.2%.
he grading system was then modified to consider the size of arachnoid defects in addition to the severity of the leak flow and then they used as a base for different reconstruction strategies (10,11). Esposito and colleagues (10) classified intra-operative CSF leak in microscopic endonasal transsphenoidal pituitary approach according to the size of the defect and severity of leak as grade 0, if no leak observed; grade 1, if there was small leak without obvious diaphragmatic defect; grade 2, if moderate leak observed and grade 3, if there was a large diaphragmatic or dural defect. They repaired cranial base on the bases of using collagen sponge in grade 0, two layer of collagen sponge with intrasellar titanium mesh buttress in grade 1, intrasellar and sphenoid sinus fat grafts with collagen sponge overlay and titanium buttress in grade 2 and grade 3 and CSF diversion in most cases of grade 3. By applying this strategy they achieved 2.5% postoperative CSF leak.
The previous mentioned methods was modified by Kong et al (10) who took into consideration the size of opening in the arachnoid membrane (<5 or ≥5 mm) (7,10). They used simple closure without tissue grafting in grade 0 (without intraoperative CSF leak) and reconstructed the sellar floor (non-randomly)in other grades using free-tissue grafting such as fat and mucosal grafting or gasket-seal method and entail postoperative CSF leaks of 10%.
Beside intra-operative CSF leak, other situations have also been considered as indications for reconstruction by others. Cappabianca et al (2) adopted a policy to reconstruct the sella in endoscopic transsphenoidal pituitary approach according to the presence of prolapse of the suprasellar cistern toward the sellar floor, bleeding from the medial wall of the cavernous sinus, injury of the carotid artery, paninvasive macroadenoma, and intra-operative CSF leaks regardless of the severity of the stream and with rate of postoperative CSF leaks of only 2.3 % (2).
In this study we graded the intra-operative CSF leak according to both the severity of the stream and the size of arachnoid defect. We thought the strength of the leak flow is an important factor that must be considered in the reconstruction since it can displace the graft materials. The size of the arachnoid defect also should be included as a relatively large defect that could show up with low output flow due to low ICP. The cutoff point for the size of arachnoid defect that we chose in the grading system was 1 mm because we believed that larger defects required stronger repair.
According to the strategy adopted for reconstruction, the main factor to categorize the cases was the aforementioned CSF leak grading system. The exceptions of each stage are factors that could have influenced success of the repair. For example at the time we started the extra pseudocapsular dissection method, it was previously suggested by Laws that this method may increases the likelihood of post-operative CSF leak (19). In order to take the advantage of this marvelous technique in total removal of the pituitary adenomas while overcoming the complication, we used at least stage II of reconstruction technique even though no CSF leak was encountered (of course in most of these cases we encountered grade 1 of CSF leak). In 2 cases we encountered severe prolapsed of arachnoid membrane coming out of sella with no intra operative CSF leak but reconstructed them according to the upper stage. Leaks originating from arachnoid membrane above the diaphragm sella were mostly high flow streams falling into the stage III category. In two of these cases that there were only drippings of CSF, since it was difficult to put the fat graft on the site of arachnoid membrane violation, the repair was supported by glue as stage III.
Apart from the CSF leak grading system and reconstruction strategy, the favorable outcome of postoperative leak of about 0.8% is likely to be the result of some additional adopted strategies. For instance the otolaryngologist was observing the entire field through the surgery as we believe meticulous homeostasis and continuous observation of the field especially arachnoid membrane for intra-operative leak is important to accurately classify the degree of leak, as small arachnoid violation or leaks that may remain undetectable at the end of procedure especially in tumors with suprasellar extension (because of folding of the loose diaphragma sella). Even application of Valsalva maneuver could have been increased the bleeding obscuring the lowoutput leakages.
Nowadays, more studies are focused on using vascularized mucosal flaps like middle turbinate mucosa and vascularized pediculed septal flaps, e.g. Hadad's nasoseptal flap, in extended approaches to reduce the risk of postoperative CSF leaks (3,20-22). We have not use vascularized mucosal flap in a standard transsellar approach for pituitary adenoma but we tried to save sphenoid sinus mucosa as best as we could by using through-cutting instruments trying not to elevate it from the bone and only pushing it back from the sellar floor and bring the mucosal edges back over the defect as much as possible at the end of procedure before covering the defect with Surgicel. We believe this maneuver could accelerate mucosal repair, decreasing the likelihood of graft displacement and thereby reducing the likelihood of postoperative CSF leak.
This surgical strategy also had some disadvantages. An external skin incision is needed for graft harvesting, although it has the advantage of being autologous and inexpensive. The other issue was with the glue we used which needed to be cleaned out during postoperative visits. The use of absorbable glue may greatly alleviate this problem.
Conclusion
We believe that this reconstruction strategy according to the proposed CSF leak grading system with emphasize on a meticulous technique have minimized the postoperative leaks. The result support the strategy of not to reconstruct the sella as a routine step in the absence of CSF leaks. However, the use of pedicled flap for reconstruction of sellar defect needs to be evaluated in the future studies.
References
- 1.Tabaee A, Anand V.k, Barrón Y, Hiltzik DH, Brown SM, Kacker A, Mazumdar M, Schwartz TH. Endoscopic pituitary surgery: a systematic review and meta-analysisJ. Neurosurg. 2009;111:545–54. doi: 10.3171/2007.12.17635. [DOI] [PubMed] [Google Scholar]
- 2.Cappabianca P, Cavallo LM, Esposito F, Valente V, De Divitiis E, Cappabianca P. Sellar repair in endoscopic endonasal transsphenoidal surgery: results of 170 cases. Neurosurgery. 2002;51:1365–71. [PubMed] [Google Scholar]
- 3.Thakur B, Jesurasa A, Thakur B, Jesurasa AR, Ross R, Carroll TA, Mirza S, Sinha S. Transnasal trans-sphenoidal endoscopic repair of CSF leak secondary to invasive pituitary tumors using a nasoseptal flap. Pituitary. 2011;14:163–7. doi: 10.1007/s11102-010-0274-z. [DOI] [PubMed] [Google Scholar]
- 4.Gagliardi F, Boari N, Mortini P. Reconstruction techniques in skull base surgery. J Craniofac Surg. 2011;22:1015–20. doi: 10.1097/SCS.0b013e31821015b5. [DOI] [PubMed] [Google Scholar]
- 5.Jones N, Becker DG. Advances in the management of CSF leaks. BMJ. 2001;322:122–3. doi: 10.1136/bmj.322.7279.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El-Banhawy O.A, Halaka AN, Ayad H, El-Altuwaijri M, El-Sharnoby MM. Long-term endonasal endoscopic review of successful duraplasty after endonasal endoscopic skull base surgery. Am J Rhinol. 2008;22:175–81. doi: 10.2500/ajr.2008.22.3157. [DOI] [PubMed] [Google Scholar]
- 7.Kelly DF, Oskouian RJ, Fineman I. Collagen sponge repair of small cerebrospinal fluid leaks obviates tissue grafts and cerebrospinal fluid diversion after pituitary surgery. Neurosurgery. 2001;49:885–9. doi: 10.1097/00006123-200110000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Nishioka H, Haraoka J, Ikeda Y. Risk factors of cerebrospinal fluid rhinorrhea following transsphenoidal surgery. Acta Neurochir (Wien) 2005;147:1163–6. doi: 10.1007/s00701-005-0586-3. [DOI] [PubMed] [Google Scholar]
- 9.Shiley S, Limonadi F, Delashaw JB, Barnwell SL, Andersen PE, Hwang PH, Wax MK. Incidence, etiology, and management of cerebrospinal fluid leaks following trans-sphenoidal surgery. Laryngoscope. 2003;113:1283–88. doi: 10.1097/00005537-200308000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Esposito F, Dusick J.R, Fatemi N, Kelly DF. Graded repair of cranial base defects and cerebrospinal fluid leaks in transsphenoidal surgery. Neurosurgery. 2007;60(4 Suppl 2):295–303. doi: 10.1227/01.NEU.0000255354.64077.66. [DOI] [PubMed] [Google Scholar]
- 11.Kong D.S, Kim HY, Kim SH, Min JY, Nam DH, Park K, Dhong HJ, Kim JH. Challenging reconstructive techniques for skull base defect following endoscopic endonasal approachesActa. Neurochir (Wien) 2011;153:807–13. doi: 10.1007/s00701-011-0941-5. [DOI] [PubMed] [Google Scholar]
- 12.Romero Adel C, Nora J, Nora JE, Topczewski TE, Aguiar PH, Alobid I, Rodriguéz EF. Cerebrospinal fluid fistula after endoscopic transsphenoidal surgery: experience in a spanish centerArq. Neuropsiquiatr. 2010;68:414–7. doi: 10.1590/s0004-282x2010000300017. [DOI] [PubMed] [Google Scholar]
- 13.Snyderman C.H, Kassam AB, Carrau R, Mintz A. Endoscopic Reconstruction of Cranial Base Defects following Endonasal Skull Base SurgerySkull. Base. 2007;17:73–8. doi: 10.1055/s-2006-959337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carrau R.L, Snyderman CH, Kassam AB. The management of cerebrospinal fluid leaks in patients at risk for high-pressure hydrocephalus. Laryngoscope. 2005;115:205–12. doi: 10.1097/01.mlg.0000154719.62668.70. [DOI] [PubMed] [Google Scholar]
- 15.Farhadi M, Jalessi M, Sharifi G, Khamesi S, Bahrami E, Hammami M.R, Behzadi AH. Use of image guidance in endoscopic endonasal surgeries: a 5-year experience. B-ENT. 2011;7(4):277–82. [PubMed] [Google Scholar]
- 16.Wang Y.Y, Kearney T, Gnanalingham KK. Low-grade CSF leaks in endoscopic transsphenoidal pituitary surgery: efficacy of a simple and fully synthetic repair with a hydrogel sealant. Acta Neurochir (Wien) 2011;153:815–22. doi: 10.1007/s00701-010-0862-8. [DOI] [PubMed] [Google Scholar]
- 17.Casler J.D, Doolittle AM, Mair EA. Endoscopic surgery of the anterior skull base. Laryngoscope. 2005;115:16–24. doi: 10.1097/01.mlg.0000150681.68355.85. [DOI] [PubMed] [Google Scholar]
- 18.Tamasauskas A, Sinkunas K, Draf W, Deltuva V, Matukevicius A, Rastenyte D, Vaitkus S. Management of cerebrospinal fluid leak after surgical removal of pituitary adenomas. Medicina (Kaunas) 2008;44:302–7. [PubMed] [Google Scholar]
- 19.Kaptain G.J, Vincent DA, Sheehan JP, Laws ER Jr. Transsphenoidal approaches for the extracapsular resection of midline suprasellar and anterior cranial base lesions. Neurosurgery. 2008;62(6 Suppl 3):1264–71. doi: 10.1227/01.neu.0000333791.29091.83. [DOI] [PubMed] [Google Scholar]
- 20.Kassam A.B, Thomas A, Carrau RL, Snyderman CH, Vescan A, Prevedello D, Mintz A, Gardner P. Endoscopic reconstructionof the cranial base using a pediclednasoseptal flap. Neurosurgery. 2008;63:ONS44–ONS52. doi: 10.1227/01.neu.0000297074.13423.f5. [DOI] [PubMed] [Google Scholar]
- 21.El-Banhawy O.A, Halaka AN, El-Dien AE, Ayad H. Sellarfloor reconstruction with nasal turbinate tissue after endoscopicendonasal transsphenoidal surgery for pituitary adenomasMinimInvasive. Neurosurg. 2003;46:289–92. doi: 10.1055/s-2003-44453. [DOI] [PubMed] [Google Scholar]
- 22.Hadad G, Bassagasteguy L, Carrau R.L, Mataza J.C, Kassam A, Snyderman C.H, Mintz A. A novel reconstructive techniqueafter endoscopic expanded endonasal approaches: vascular pediclenasoseptal flap . Laryngoscope. 2006;116(10):1882–6. doi: 10.1097/01.mlg.0000234933.37779.e4. [DOI] [PubMed] [Google Scholar]


