Abstract
Background: Prior research suggests that women do not accurately estimate their risk for breast cancer. Estimating and informing women of their risk is essential for tailoring appropriate screening and risk reduction strategies.
Methods: Data were collected for BreastCARE, a randomized controlled trial designed to evaluate a PC-tablet based intervention providing multiethnic women and their primary care physicians with tailored information about breast cancer risk. We included women ages 40–74 visiting general internal medicine primary care clinics at one academic practice and one safety net practice who spoke English, Spanish, or Cantonese, and had no personal history of breast cancer. We collected baseline information regarding risk perception and concern. Women were categorized as high risk (vs. average risk) if their family history met criteria for referral to genetic counseling or if they were in the top 5% of risk for their age based on the Gail or Breast Cancer Surveillance Consortium Model (BCSC) breast cancer risk model.
Results: Of 1,261 participants, 25% (N=314) were classified as high risk. More average risk than high risk women had correct risk perception (72% vs. 18%); 25% of both average and high risk women reported being very concerned about breast cancer. Average risk women with correct risk perception were less likely to be concerned about breast cancer (odds ratio [OR]=0.3; 95% confidence interval [CI]=0.2–0.4) while high risk women with correct risk perception were more likely to be concerned about breast cancer (OR=5.1; 95%CI=2.7–9.6).
Conclusions: Many women did not accurately perceive their risk for breast cancer. Women with accurate risk perception had an appropriate level of concern about breast cancer. Improved methods of assessing and informing women of their breast cancer risk could motivate high risk women to apply appropriate prevention strategies and allay unnecessary concern among average risk women.
Introduction
Many physicians do not discuss breast cancer risk with their patients, despite the availability of risk assessment tools that are easily available for administration in the clinic setting. The Gail model, for example, uses clinical variables including family history of breast cancer to generate a 5-year estimate of individual risk.1 More recently developed models include mammographic breast density, which is independently associated with breast cancer risk.2,3 Family history-based assessments, including BRCAPRO are available to determine breast cancer genetic susceptibility, although BRCAPRO has proven difficult to implement in the primary care setting.4 In response, shorter assessments including the breast/ovarian cancer genetics referral screening tool (RST) have been successfully validated and somewhat incorporated into clinical practice.5
Estimating and informing women of their breast cancer risk is an essential first step when tailoring appropriate screening and risk reduction strategies. Risk perception has been identified as a strong motivator for women to engage in preventive and screening behaviors,6,7 yet prior research suggests that many women misperceive their breast cancer risk.8–14 If average risk women perceive their risk to be higher than it actually is, they may experience unnecessarily high levels of concern or anxiety, leading to overuse of breast cancer screening and risk reduction options.8,15 In contrast, an optimistic perception of risk among those at high risk may lead to inappropriate screening and missed opportunities to utilize risk reduction options such as genetic counseling and chemoprevention.16–18
Although for many women, improving risk perception among those at high risk is crucial for promoting screening and use of risk reduction strategies, a potential unintended consequence of informing these women about their breast cancer risk is to increase worry or concern. Increased risk perception may be associated with increased breast cancer concern; however, this relationship has not been firmly established in a diverse study population.11
Results from the literature are mixed regarding the impact of risk perception and cancer concern on screening behaviors.19,20 While higher perceived risk and worry have been found to predict greater odds of mammography use among whites and African American women, the same may not be true for Latina women which strengthens the need for further investigation in multiethnic samples.20
To address some of the gaps in the literature, our study had two objectives. First, we aimed to assess the personal factors associated with correct perception of risk and breast cancer concern among a sample of multiethnic women at high and average breast cancer risk. Second, we aimed to determine the relationship between correct perception of risk and breast cancer concern. We hypothesized that correct risk perception among those at average risk would not be associated with concern, while correct perception among those at high risk would be associated with concern.
Materials and Methods
Sample
Potential participants for this study were identified through the BreastCARE Study, a randomized controlled trial designed to evaluate a tablet-based intervention providing multiethnic women and their primary care physicians with tailored information about each woman's breast cancer risk. Participants were recruited from two General Internal Medicine clinics in urban San Francisco (one academic practice, and one academic safety-net hospital practice) between June 2011 and August 2012. Women were eligible to participate in the study if they had an appointment at one of the participating clinic sites during the study period, had a working telephone number, were able to complete a telephone survey, were between the ages of 40 and 74, spoke English, Spanish, or Cantonese, and had no personal history of breast cancer or ductal carcinoma in situ.
As part of the BreastCARE study, women with upcoming primary care doctor's appointments were mailed a recruitment letter and an opt-out postcard. One week later, a BreastCARE recruiter called these women. Those women who were reached prior to their doctor's appointment and agreed to participate in the study completed a baseline telephone interview. During this phone call they were randomized into either the intervention or the comparison group. The comparison group completed a breast cancer risk assessment over the telephone, while the intervention group completed a tablet-based version of the assessment at the clinic immediately preceding their primary care appointment. All participants provided written informed consent when they presented for their clinic appointment. The research protocol was reviewed and approved by the institutional review boards of the participating institutions.
Measures
Baseline demographic information collected included age at survey (40–50 years, 51–65 years, 66–74 years), self-reported race/ethnicity (non-Latina white, Latina, black or African American, Asian Pacific Islander), marital status (married or living with a partner versus other), years of schooling (high school diploma or less, some college, college or greater), medical insurance coverage (private, public, no insurance), employment status (working full- or part-time versus other), and clinic site (site 1 or site 2).
Health information collected at baseline included self-reported general health (excellent/very good versus good/fair/poor), self-reported number of primary care visits in the past year (0–1, 2–3, 4+), and self-reported number of comorbidities (0–1, 2–3, 4+) using a validated survey instrument.21
Breast cancer risk assessment indicators
We collected data on the following breast cancer risk factors: age at menarche, age at first birth, age at menopause, breast biopsy history, tamoxifen or raloxifene use, Ashkenazi Jewish ancestry, history of ovarian cancer, and number of relatives who have been diagnosed with breast and/or ovarian cancer.
Objective assessment of risk
To estimate objective risk for breast cancer, we used three measures: the RST,5 the Gail Model,1 and the Breast Cancer Surveillance Consortium Model (BCSC).2 These measures and risk-level thresholds were chosen by a consensus panel of experts convened for the BreastCARE study. The rationale for all thresholds was to choose clinically actionable cut-points; in other words, thresholds above which a woman would be referred for genetic counseling or high risk evaluation for chemoprevention. Women were considered to be high risk if they met at least one of two criteria: (1) positive family history based on the RST (≥2 risk categories checked), (2) Gail score in the top 5% estimated 5-year risk for their age group,1 or BCSC score in top 5% of estimated 5-year risk for their age group when mammographic breast density data was available (age groups included 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, and 70–74 years).2 In addition, women between the ages of 40 and 50 years were considered to be high risk if their Gail or BCSC score was ≥1.67.16 Some women were high risk according to RST score but not according to Gail/BCSC score while others were high risk according to Gail/BCSC score but not according to RST score. For the BreastCARE intervention, recommendations for women were tailored to their specific high risk type. Women who were high risk according to both indicators received screening/prevention recommendations based on RST score. All other women were classified as average risk.
Outcomes
We examined two outcome variables. The first outcome, correct perception of risk, was defined as a match between objective and perceived risk of developing breast cancer, relative to other women of the same age. We considered high risk women who reported that their chance of getting breast cancer was “higher than other women of the same age” to have correct risk perception. Similarly, we considered average and risk women who responded that their chance of getting breast cancer was “the same or lower than other women of the same age” to have correct risk perception. The second outcome variable was breast cancer concern (survey question: “How concerned are you about getting breast cancer?”). This variable was dichotomized as “very concerned” versus “somewhat,” “a little,” or “not at all” concerned, in bivariate and multivariate analyses.
Analysis
Chi-square tests were used to determine bivariate associations between covariates and measures of correct risk perception and breast cancer concern. Separate multivariable logistic regression models were constructed to examine factors associated with (a) correct perception of breast cancer risk relative to other women of the same age, and (b) breast cancer concern. These models were stratified by objective breast cancer risk (dichotomized as average versus high risk). Variables were selected for inclusion in the multivariate models based on bivariate associations (p<0.2) or a priori hypotheses. Models of correct perception of risk controlled for race/ethnicity, age, marital status, education, language of interview, insurance status, study site, number of comorbid conditions, and any blood relatives with breast cancer (among average risk women). Models of breast cancer worry controlled for race/ethnicity, age, marital status, education, language of interview, insurance status, study site, number of comorbid conditions, correct perception of risk and any blood relative with breast cancer (among average risk women). Analyses were performed in STATA 11.2 (Stata Corp LP).
Results
Description of sample
Among 4,029 women who were reached during the study recruitment period, a total of 556 (14%) were ineligible to participate. Of the 3,473 eligible women, 1,635 (47%) agreed to participate, completed baseline surveys, and were randomized to one of the two study arms, while 1,838 (53%) declined to participate. Among 1,635 women who completed the baseline survey, 1,278 (78%) signed a study consent form at the clinic site. Of this total, 1,261 women were included in our analysis, based on race/ethnicity (17 women who described themselves as Native American or Other were excluded due to low numbers).
Baseline demographic and health characteristics for all participants are shown in Table 1. Over a third of the participants (35%) were non-Latina white, 24% were Latina, 22% were black or African American, and 19% were Asian Pacific Islanders (API). Twenty-five percent of the women were classified as high risk; of these women, 16% were classified as high risk based on the Gail or BCSC models, and 9% were high risk based on the RST. Of 947 average risk women, 179 (14%) reported having at least one relative with breast cancer.
Table 1.
Baseline Demographic and Health Characteristics Among 1,261 Participants
| Total n (%)* | |
|---|---|
| Race/ethnicity | |
| Non-Latina white | 441 (35.0%) |
| Latina | 301 (23.9%) |
| Black or African American | 281 (22.2%) |
| Asian/Pacific Islander | 238 (18.9%) |
| Age at survey | |
| 40–50 | 379 (30.0%) |
| 51–65 | 668 (53.0%) |
| 65–74 | 214 (17.0%) |
| Marital status | |
| Married/living with partner | 565 (45.1%) |
| Other | 688 (54.9%) |
| Education | |
| High school diploma or less | 405 (32.4%) |
| Some college | 322 (25.8%) |
| College graduate or more | 522 (41.8%) |
| Employment status | |
| Full time | 340 (27.0%) |
| Part time | 244 (19.4%) |
| Retired | 219 (17.4%) |
| Not working | 455 (36.2%) |
| Insurance | |
| Private insurance | 603 (47.8%) |
| Public insurance | 625 (49.6%) |
| No insurance | 33 (2.6%) |
| Language of interview | |
| English | 1,098 (87.1%) |
| Spanish or Cantonese | 163 (12.9%) |
| Clinic site | |
| Site 1 (academic) | 865 (68.6%) |
| Site 2 (safety net) | 396 (31.4%) |
| Randomization group | |
| Intervention | 596 (47.2%) |
| Comparison | 665 (52.8%) |
| Number of comorbid conditions | |
| 0 | 86 (6.8%) |
| 1–2 | 504 (40.0%) |
| 3 or more | 671 (53.2%) |
| Number of primary care visits in last year | |
| 0–1 | 357 (28.7%) |
| 2–3 | 429 (34.4%) |
| 4+ | 460 (36.9%) |
| Self-perceived general health | |
| Excellent/very good | 426 (34.0%) |
| Good/fair/poor | 828 (66.0%) |
| Breast cancer risk | |
| High risk – Gail/BCSC | 202 (16.0%) |
| High risk – RST | 112 (8.9%) |
| Average risk – relatives with BC | 179 (14.2%) |
| Average risk – no relatives with BC | 768 (60.9%) |
Percentages based on non-missing values.
BC, breast cancer; BCSC, Breast Cancer Surveillance Consortium Model; RST, referral screening tool.
Correct risk perception
Among average risk women, the majority (72%) correctly perceived themselves to be at average or less than average risk for breast cancer compared to other women their age. In contrast, only 18% of high risk women correctly perceived themselves to be at increased risk.
The proportions of women with correct risk perception, according to demographic and health characteristics, are shown in Table 2. Among average risk women, older age, and no blood relatives with breast cancer were significantly associated with correct risk perception in bivariate analyses. Among high risk women, younger age was associated with correct risk perception.
Table 2.
Predictors of Correct Perception of Breast Cancer Risk, Stratified by Objective Breast Cancer Risk*
| Average risk women | High risk women | |||||||
|---|---|---|---|---|---|---|---|---|
| Correct perception of risk, n (%) | p | aOR (95% CI)† | p | Correct perception of risk, n (%) | p | aOR (95% CI)† | p | |
| Race/Ethnicity | 0.08 | 0.41 | ||||||
| Non-Latina white | 233 (85.4%) | Reference | — | 42 (25.3%) | Reference | — | ||
| Latina white | 212 (82.8%) | 0.89 (0.47–1.7) | 0.71 | 10 (22.7%) | 0.65 (0.21–2.1) | 0.47 | ||
| Black/African American | 177 (76.6%) | 0.75 (0.44–1.3) | 0.30 | 18 (36.0%) | 1.5 (0.68–3.3) | 0.31 | ||
| Asian Pacific Islander | 153 (83.2%) | 0.73 (0.42–1.3) | 0.26 | 16 (30.2%) | 1.3 (0.62–2.7) | 0.48 | ||
| Age (years) | 0.008 | 0.003 | ||||||
| ≤50 | 247 (78.4%) | 0.32 (0.17–0.62) | 0.001 | 26 (40.6%) | 4.3 (1.7–10.9) | 0.002 | ||
| 51–65 | 390 (81.9%) | 0.47 (0.25–0.88) | 0.02 | 52 (27.5%) | 2.4 (1.0–5.5) | 0.04 | ||
| Over 65 | 138 (90.2%) | Reference | — | 8 (13.3%) | Reference | — | ||
| Marital status | 0.22 | 0.46 | ||||||
| Married/living with a partner | 340 (84.0%) | Reference | — | 40 (25.5%) | Reference | — | ||
| Other | 431 (80.9%) | 1.2 (0.79–1.7) | 0.47 | 45 (29.2%) | 0.78 (0.42–1.4) | 0.42 | ||
| Education | 0.29 | 0.99 | ||||||
| High school graduate or less | 272 (80.5%) | Reference | — | 18 (26.9%) | Reference | — | ||
| Some college | 192 (80.7%) | 1.2 (0.76–1.9) | 0.42 | 23 (27.7%) | 1.2 (0.54–2.7) | 0.65 | ||
| College graduate or more | 303 (84.6%) | 1.4 (0.87–2.4) | 0.15 | 45 (28.0%) | 1.3 (0.59–2.9) | 0.51 | ||
| Number of comorbid conditions | 0.10 | 0.23 | ||||||
| 0 | 63 (90.0%) | Reference | — | 6 (40.0%) | Reference | — | ||
| 1–2 | 304 (83.3%) | 0.48 (0.20–1.1) | 0.09 | 32 (23.2%) | 0.51 (0.16–1.6) | 0.26 | ||
| 3 or more | 408 (80.2%) | 0.40 (0.17–0.95) | 0.04 | 48 (30.0%) | 0.67 (0.21–2.2) | 0.51 | ||
| Any blood relative with breast cancer‡ | <0.001 | <0.001 | — | — | ||||
| No | 653 (85.3%) | Reference | N/A | N/A | ||||
| Yes | 122 (68.5%) | 0.36 (0.24–0.53) | N/A | N/A | ||||
Bold numerals denote statistically significant values with p<0.05.
Average risk women who responded that their lifetime risk was the same or lower than other women of the same age were considered to have correct perception of their breast cancer risk, as were high risk women who responded that their lifetime risk was higher than other women of the same age.
All multivariate models controlled for race/ethnicity, age, marital status, education, language of interview, insurance status, study site, and number of comorbidities. Multivariate models only controlled for any blood relative with breast cancer for average-risk women, as the Gail, BCSC, and RST models all incorporate family history of breast cancer.
This variable was only examined in average risk women as the Gail, BCSC, and RST models all incorporate family history of breast cancer.
aOR, adjusted odds ratio; 95% CI, 95% confidence interval.
In multivariate analyses, age remained a statistically significant predictor of correct risk perception among average and high risk women (Table 2). Compared with women over age 65, average risk women under age 65 had significantly lower odds of correctly perceiving their breast cancer risk. In contrast, high risk women under age 65 were significantly more likely to correctly perceive their breast cancer risk when compared with women over age 65. Among average risk women, those with four or more comorbidities and a family history of breast cancer also had lower odds of correctly perceiving their breast cancer risk compared with those with 0–1 comorbidities and no family breast cancer history, respectively.
Breast cancer concern
Twenty-four percent of average risk women and 26% of high risk women reported being very concerned about breast cancer.
Table 3 shows the proportions of women who indicated they were very concerned about developing breast cancer according to demographic and health characteristics. In bivariate analyses, both average and high risk participants who were African American and ≤50 years old were more likely to report increased concern than their counterparts. Among average risk women, those with some college education, at least one relative with breast cancer and incorrect perception of risk were more likely to report concern than their counterparts.
Table 3.
Predictors of Concern About Developing Breast Cancer, Stratified by Objective Breast Cancer Risk*
| Average risk women | High risk women | |||||||
|---|---|---|---|---|---|---|---|---|
| Very concerned about breast cancer, n (%) | p | aOR (95% CI)† | p | Very concerned about breast cancer, n (%) | p | aOR (95% CI)† | p | |
| Race/ethnicity | <0.001 | 0.41 | ||||||
| Non-Latina white | 32 (11.7%) | Reference | — | 22 (13.2%) | Reference | — | ||
| Latina white | 59 (23.0%) | 2.1 (1.1–4.0) | 0.02 | 15 (34.1%) | 2.5 (0.79–8.0) | 0.12 | ||
| Black/African American | 97 (42.2%) | 4.6 (2.7–7.8) | <0.001 | 28 (56.0%) | 7.2 (3.0–17.1) | <0.001 | ||
| Asian Pacific Islander | 39 (21.3%) | 2.3 (1.3–4.0) | 0.004 | 18 (34.0%) | 3.7 (1.6–8.5) | 0.002 | ||
| Age | <0.001 | 0.003 | ||||||
| ≤50 | 94 (29.8%) | 2.4 (1.3–4.5) | 0.005 | 25 (39.1%) | 2.3 (0.84–6.2) | 0.11 | ||
| 51–65 | 115 (24.2%) | 1.7 (0.94–3.1) | 0.08 | 48 (25.3%) | 1.3 (0.54–3.0) | 0.57 | ||
| Over 65 | 18 (11.8%) | Reference | — | 10 (16.7%) | Reference | — | ||
| Marital status | 0.02 | 0.46 | ||||||
| Married/living with a partner | 82 (20.3%) | Reference | — | 29 (18.4%) | Reference | — | ||
| Other | 144 (27.1%) | 0.90 (0.62–1.3) | 0.58 | 54 (35.1%) | 0.47 (0.24–0.93) | 0.03 | ||
| Education | <0.001 | 0.99 | ||||||
| High school graduate or less | 93 (17.8%) | Reference | — | 28 (41.8%) | Reference | — | ||
| Some college | 75 (31.4%) | 1.0 (0.67–1.6) | 0.89 | 24 (28.9%) | 0.63 (0.26–1.5) | 0.30 | ||
| College graduate or more | 57 (15.9%) | 0.57 (0.35–0.93) | 0.03 | 31 (19.1%) | 0.57 (0.24–1.3) | 0.19 | ||
| Number of comorbid conditions | 0.32 | 0.23 | ||||||
| 0 | 12 (16.9%) | Reference | — | 4 (26.7%) | Reference | — | ||
| 1–2 | 92 (25.3%) | 1.7 (0.82–3.6) | 0.15 | 28 (20.3%) | 0.98 (0.22–4.3) | 0.97 | ||
| 3 or more | 123 (24.2%) | 1.3 (0.64–2.9) | 0.43 | 51 (31.7%) | 1.2 (0.29–5.4) | 0.77 | ||
| Any blood relative with breast cancer‡ | <0.001 | — | ||||||
| No | 163 (21.3%) | Reference | — | N/A | N/A | — | ||
| Yes | 64 (36.0%) | 2.0 (1.3–2.9) | 0.001 | N/A | N/A | — | ||
| Correct perception of risk** | <0.001 | <0.001 | ||||||
| No | 85 (50.3%) | Reference | — | 40 (17.6%) | Reference | — | ||
| Yes | 142 (18.4%) | 0.26 (0.18–0.39) | <0.001 | 43 (50.0%) | 5.1 (2.7–9.6) | <0.001 | ||
Bold numerals denote statistically significant values with p<0.05.
Concern about breast cancer was dichotomized into “very concerned” about getting breast cancer vs. “somewhat/a little/not at all” concerned.
All models controlled for race/ethnicity, age, marital status, level of education, language of interview, insurance status, study site, number of comorbid conditions, and correct perception of risk. Multivariate models only controlled for any blood relative with breast cancer for average risk women, as the Gail, BCSC, and RST models all incorporate family history of breast cancer.
This variable was only examined in average risk women as the Gail, BCSC, and RST models all incorporate family history of breast cancer.
Average risk women who responded that their lifetime risk was the same or lower than other women of the same age were considered to have correct perception of their breast cancer risk, as were high risk women who responded that their lifetime risk was higher than other women of the same age.
In multivariate analyses, non-white race/ethnicity and younger age were associated with increased breast cancer concern for both average and high risk participants (Table 3). Average risk women with at least a college degree had greater odds of breast cancer concern than those with less than a college degree, while those with ≥1 blood relative with breast cancer had greater odds of breast cancer concern than women with no family history of breast cancer. Average risk women with correct perception of breast cancer risk had lower odds of concern about breast cancer than those with an incorrect perception of risk. In contrast, the odds of breast cancer concern were five times higher among high risk women who correctly perceived their breast cancer risk compared with those who incorrectly perceived their risk.
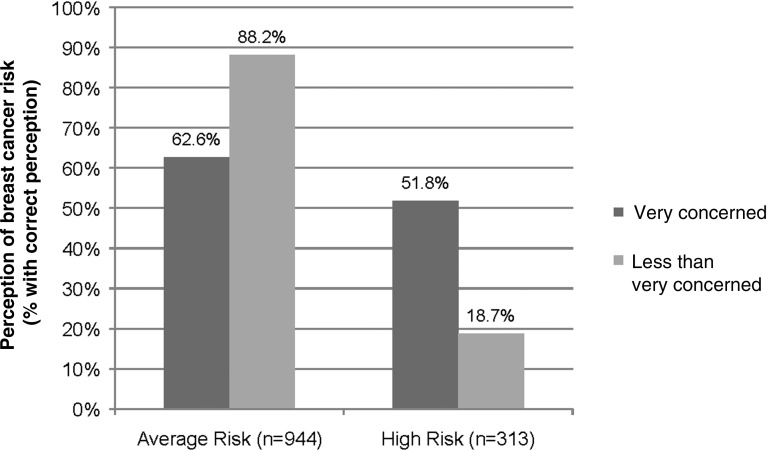
Correct perception of risk and concern about breast cancer
Average risk women who were very concerned about breast cancer were less likely to correctly perceive their breast cancer risk than average risk women who were not very concerned about breast cancer (Fig. 1, 62.6% vs. 88.2%; p<0.001). High risk women who were very concerned about breast cancer were more likely to correctly perceive their breast cancer risk than those who were not very concerned about breast cancer (51.8% vs. 18.7%; p<0.001).
Fig. 1.
Relationship between correct breast cancer risk perception and breast cancer concern.
Discussion
We aimed to assess the relationship between correct perception of risk and concern about breast cancer. While prior research has explored factors associated with breast cancer risk perception and concern, these topics have not been well explored in multiethnic populations, or in populations of women with varying levels of risk. To address some of the gaps in the literature, our study examined factors associated with each of these measures in a multiethnic sample.
We found correct risk perception varied by actual cancer risk. The vast majority of women at high risk underestimated their risk, whereas the majority of average risk women were informed that their risk was not higher than other women their age. This contrasts with literature that suggests women tend to overestimate their breast cancer risk,7 although some women may exhibit an optimistic bias toward their personal risk.22 While many women at high risk had strong family histories of breast cancer, family history alone is not sufficient to increase breast cancer risk perception: in one study, women perceived themselves to be at lower risk if they were not emotionally close to family members with breast cancer.22 In addition, our survey measures asked participants to report their comparative, rather than absolute, breast cancer risk. Several studies have shown this decreases the likelihood of risk overestimation compared with asking participants for a specific numeric estimate.14,23
The relationship between age and correct risk perception in our population varied by actual risk. High risk women of younger age tended to correctly perceive themselves to be at high risk compared to high risk older women, while older average risk women were more likely to correctly estimate their risk. This may be explained by a tendency to overestimate the likelihood of developing breast cancer at younger ages compared to older ages, although older women may not understand how their risk of breast cancer changes as they age.24–26 Lower levels of breast cancer knowledge have been identified in older women in other studies;25,26 this may explain our findings, but we were unable to explore this relationship, as our baseline questionnaire did not assess breast cancer knowledge.
African American and API women in our population were more likely to be concerned about breast cancer than non-Latina white or Latina women, regardless of objective breast cancer risk. Previously published studies with African American, Latina, and non-Latina white women have yielded mixed results on the influence of race/ethnicity on breast cancer concern, leading some authors to attribute observed differences to income and education rather than race/ethnicity.20,27,28 In addition, the few published studies of women with API ancestry have focused on specific populations rather than a diverse sample of Asian American women.29–32 Our analyses controlled for household income and years of education, but unmeasured differences in breast cancer knowledge may account for increased concern among African American and API participants relative to Latinas and non-Latina whites.
We found the relationship between correct perception of risk and concern about breast cancer differed between average and high risk women in our study. Among average risk women, correct perception of risk was associated with decreased concern, while high risk women with correct risk perception reported increased concern. Breast cancer concern has been associated with willingness to initiate breast cancer risk reduction and preventive strategies in certain populations.33
Accurate risk perception is crucial for women at all levels of breast cancer risk, as average risk women who incorrectly perceive themselves to be at high risk tend to be very concerned when they need not be, while high risk women who incorrectly perceive themselves to be at average risk tend not to be concerned about getting breast cancer, when perhaps they should be. To the extent that correct perception of risk among high risk women leads to increased concern and subsequent initiation of preventive action, our findings suggest that high risk women benefit from efforts to educate them about their objective risk of breast cancer. Average risk women who incorrectly perceive their risk to be high and are very concerned about breast cancer as a result, also benefit from efforts to educate them about their objective breast cancer risk, which may reduce unnecessary anxiety. However, it is important to note that the literature has mixed findings regarding the impact of risk perception and cancer concern on screening practices.20 Higher perceived risk and cancer worry have been found to predict greater odds of mammography use among non-Latina white and African American women but not among Latina women.
Strengths of this study include our large, racially and ethnically diverse study population, broad study inclusion criteria, and comprehensive survey measurements. Sixty-five percent of our survey population was non-white, and the distribution of racial and ethnic groups in this study reflects the patient population at the two participating clinic sites. In addition, our population was selected from primary care clinics, allowing for the inclusion of women from diverse backgrounds representing diverse levels of risk.
Our study has several limitations. We considered risk to be a binary, rather than continuous, variable, which may have decreased our power to detect differences between demographic and clinical variables included in our survey. This binary risk construct did not differentiate between average and low risk women, however, which may have led us to overestimate correct risk perception among average risk women who perceived themselves to be at lower than average risk. Women who did not speak English, Spanish, or Cantonese were excluded, although these three languages represent the vast majority of patients seen in the participating clinics (only 47 screened women were considered ineligible due to language).
Our study had a response rate of 47%, which may impact the generalizability of the results. In addition, subjects participating in a randomized clinical trial may not constitute a representative sample of the female population. Women who chose to participate in our study were relatively well educated; while our study population was racially and ethnically diverse, our findings may not be generalizable to women with lower levels of education or those seen in other clinical settings. Some racial/ethnic groups may also be less likely to recall or openly discuss breast cancer family history and therefore more likely to underestimate their risk.
In addition, the study population was unintentionally enriched with high risk women. Although our designated thresholds for high risk women were designed to only include the top 5% in each 5-year age group, 16% of our population qualified as high risk based on the Gail or BCSC models, and an additional 9% of participants qualified based on the RST. Finally, the objective risk models we applied to a diverse sample of women may provide better estimates of breast cancer risk for certain racial/ethnic groups (e.g., non-Latina whites) than for others, although the Gail model has been validated in diverse populations.34–37
Conclusions
In our study population, the majority of women at high risk of developing breast cancer incorrectly perceived their risk, while a significant minority of average risk women perceived themselves to be at higher risk than other women their age. Breast cancer concern is prevalent among both high and average risk women, and most common among non-white women and those who perceive themselves to be at high risk of developing breast cancer. Accurate perception of breast cancer risk among average risk and high risk women was directly related to appropriate concern about breast cancer, suggesting improved methods of assessing and informing women of their breast cancer risk could motivate women to apply appropriate prevention strategies. Our findings point to the need for interventions designed to improve correct perception of risk across a range of absolute risk to facilitate meaningful discussions between providers and patients regarding breast cancer screening and prevention practices.
Acknowledgments
This research was supported by grants from the Susan G. Komen for the Cure Foundation (KG090504) and the California Breast Cancer Research Program (150B-0158).
Disclosure Statement
No competing financial interests exist.
References
- 1.Gail MH, Brinton LA, Byar DP, et al. . Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst 1989;81:1879–1886 [DOI] [PubMed] [Google Scholar]
- 2.Tice JA, Cummings SR, Smith-Bindman R, Ichikawa L, Barlow WE, Kerlikowske K. Using clinical factors and mammographic breast density to estimate breast cancer risk: Development and validation of a new predictive model. Ann Intern Med 2008;148:337–347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tice JA, Cummings SR, Ziv E, Kerlikowske K. Mammographic breast density and the Gail model for breast cancer risk prediction in a screening population. Breast Cancer Res Treat 2005;4:115–122 [DOI] [PubMed] [Google Scholar]
- 4.Riley BD, Culver JO, Skrzynia C, et al. . Essential elements of genetic cancer risk assessment, counseling, and testing: updated recommendations of the National Society of Genetic Counselors. J Genet Couns 2012;21:151–161 [DOI] [PubMed] [Google Scholar]
- 5.Bellcross CA, Lemke AA, Pape LS, Tess AL, Meisner LT. Evaluation of a breast/ovarian cancer genetics referral screening tool in a mammography population. Genet Med 2009;11:783–789 [DOI] [PubMed] [Google Scholar]
- 6.Haber G, Ahmed NU, Pekovic V. Family history of cancer and its association with breast cancer risk perception and repeat mammography. Am J Public Health 2012;102:2322–2329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sivell S, Elwyn G, Gaff CL, et al. . How risk is perceived, constructed and interpreted by clients in clinical genetics, and the effects on decision making: systematic review. J Genet Couns 2008;17:30–63 [DOI] [PubMed] [Google Scholar]
- 8.Andersen MR, Smith R, Meischke H, Bowen D, Urban N. Breast cancer worry and mammography use by women with and without a family history in a population-based sample. Cancer Epidemiol Biomarkers Prev 2003;12:314–320 [PubMed] [Google Scholar]
- 9.Black WC, Nease RF, Jr., Tosteson AN. Perceptions of breast cancer risk and screening effectiveness in women younger than 50 years of age. J Natl Cancer Inst 1995;87:720–731 [DOI] [PubMed] [Google Scholar]
- 10.Davis S, Stewart S, Bloom J. Increasing the accuracy of perceived breast cancer risk: results from a randomized trial with Cancer Information Service callers. Prev Med 2004;39:64–73 [DOI] [PubMed] [Google Scholar]
- 11.Graves KD, Huerta E, Cullen J, et al. . Perceived risk of breast cancer among Latinas attending community clinics: risk comprehension and relationship with mammography adherence. Cancer Causes Control 2008;19:1373–1382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gross CP, Filardo G, Singh HS, Freedman AN, Farrell MH. The relation between projected breast cancer risk, perceived cancer risk, and mammography use. Results from the National Health Interview Survey. J Gen Intern Med 2006;21:158–164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haas JS, Kaplan CP, Des Jarlais G, Gildengoin V, Perez-Stable E, Kerlikowske K. Perceived risk of breast cancer among women at average and increased risk. J Womens Health 2005;14:845–851 [DOI] [PubMed] [Google Scholar]
- 14.Banegas MP, Puschel K, Martinez-Gutierrez J, Anderson JC, Thompson B. Perceived and objective breast cancer risk assessment in chilean women living in an underserved area. Cancer Epidemiol Biomarkers Prev 2012;21:1716–1721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trask PC, Paterson AG, Wang C, et al. . Cancer-specific worry interference in women attending a breast and ovarian cancer risk evaluation program: impact on emotional distress and health functioning. Psychooncology 2001;10:349–360 [DOI] [PubMed] [Google Scholar]
- 16.Vogel VG, Costantino JP, Wickerham DL, et al. . Effects of tamoxifen vs. raloxifene on the risk of developing invasive breast cancer and other disease outcomes: The NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA 2006;295:2727–2741 [DOI] [PubMed] [Google Scholar]
- 17.Saslow D, Boetes C, Burke W, et al. . American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin 2007;57:75–89 [DOI] [PubMed] [Google Scholar]
- 18.Cummings SR, Eckert S, Krueger KA, et al. . The effect of raloxifene on risk of breast cancer in postmenopausal women: results from the MORE randomized trial. Multiple outcomes of raloxifene evaluation. JAMA 1999;281:2189–2197 [DOI] [PubMed] [Google Scholar]
- 19.Edwards AG, Naik G, Ahmed H, et al. . Personalised risk communication for informed decision making about taking screening tests. Cochrane Database Syst Rev 2013;2:CD001865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Orom H, Kiviniemi MT, Shavers VL, Ross L, Underwood W. Perceived risk for breast cancer and its relationship to mammography in Blacks, Hispanics, and whites. J Behav Med 2013;36:466–476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: A new method to assess comorbidity for clinical and health services research. Arthritis Rheum 2003;49:156–163 [DOI] [PubMed] [Google Scholar]
- 22.Katapodi MC, Dodd MJ, Facione NC, Humphreys JC, Lee KA. Why some women have an optimistic or a pessimistic bias about their breast cancer risk: experiences, heuristics, and knowledge of risk factors. Cancer Nurs 2010;33:64–73 [DOI] [PubMed] [Google Scholar]
- 23.Woloshin S, Schwartz LM, Black WC, Welch HG. Women's perceptions of breast cancer risk: how you ask matters. Med Decis Making 1999;19:221–229 [DOI] [PubMed] [Google Scholar]
- 24.Dolan NC, Lee AM, McDermott MM. Age-related differences in breast carcinoma knowledge, beliefs, and perceived risk among women visiting an academic general medicine practice. Cancer 1997;80:413–420 [DOI] [PubMed] [Google Scholar]
- 25.Mah Z, Bryant H. Age as a factor in breast cancer knowledge, attitudes, and screening behaviour. CMAJ 1992;146:2167–2174 [PMC free article] [PubMed] [Google Scholar]
- 26.Grunfeld EA, Ramirez AJ, Hunter MS, Richards MA. Women's knowledge and beliefs regarding breast cancer. Br J Cancer 2002;86:1373–1378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lipkus IM, Iden D, Terrenoire J, Feaganes JR. Relationships among breast cancer concern, risk perceptions, and interest in genetic testing for breast cancer susceptibility among African-American women with and without a family history of breast cancer. Cancer Epidemiol Biomarkers Prev 1999;8:533–539 [PubMed] [Google Scholar]
- 28.Miller AM, Champion VL: Attitudes about breast cancer and mammography: racial, income, and educational differences. Women Health 1997;26:41–63 [DOI] [PubMed] [Google Scholar]
- 29.Maxwell AE, Bastani R, Warda US. Breast cancer screening and related attitudes among Filipino-American women. Cancer Epidemiol Biomarkers Prev 1997;6:719–726 [PubMed] [Google Scholar]
- 30.Phipps E, Cohen MH, Sorn R, Braitman LE. A pilot study of cancer knowledge and screening behaviors of Vietnamese and Cambodian women. Health Care Women Intl 1999;20:195–207 [DOI] [PubMed] [Google Scholar]
- 31.Mehrotra N, Gaur S, Petrova A. Health care practices of the foreign born Asian Indians in the United States. A community based survey. J Community Health 2012;37:328–334 [DOI] [PubMed] [Google Scholar]
- 32.Lee HY, Vang S. Barriers to cancer screening in Hmong Americans: the influence of health care accessibility, culture, and cancer literacy. J Community Health 2010;35:302–314 [DOI] [PubMed] [Google Scholar]
- 33.Bastian LA, Lipkus IM, Kuchibhatla MN, et al. . Women's interest in chemoprevention for breast cancer. Arch Intern Med 2001;161:1639–1644 [DOI] [PubMed] [Google Scholar]
- 34.Gail MH, Costantino JP, Pee D, et al. . Projecting individualized absolute invasive breast cancer risk in African American women. J Natl Cancer Inst 2007;99:1782–1792 [DOI] [PubMed] [Google Scholar]
- 35.Adams-Campbell LL, Makambi KH, Palmer JR, Rosenberg L. Diagnostic accuracy of the Gail model in the Black Women's Health Study. Breast J 2007;13:332–336 [DOI] [PubMed] [Google Scholar]
- 36.Banegas MP, Gail MH, LaCroix A, et al. . Evaluating breast cancer risk projections for Hispanic women. Breast Cancer Res Treat 2012;132:347–353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Matsuno RK, Costantino JP, Ziegler RG, et al. . Projecting individualized absolute invasive breast cancer risk in Asian and Pacific Islander American women. J Natl Cancer Inst 2011;103:951–961 [DOI] [PMC free article] [PubMed] [Google Scholar]