Abstract
Objective: To characterize Ayurvedic perspectives on the etiopathogenesis and supportive treatments for a biomedical diagnosis of cancer.
Methods: Hour-long, digitally recorded interviews were conducted with 10 experienced Ayurvedic clinicians, transcribed verbatim, and analyzed using techniques of qualitative thematic analysis.
Results: Four major themes were identified. The Ayurvedic description of the pathophysiology of cancer uses traditional concepts translated into a modern context. Although the biomedical treatment of cancer is considered valuable, from an Ayurvedic perspective it results in degeneration and depletion. In cases where biomedical treatment of cancer is not feasible, an Ayurvedic approach focusing on strengthening digestion, eliminating toxins, reducing tumor growth, and improving tissue metabolism is useful. An Ayurvedic approach to cancer supportive care focuses on restoring equilibrium, building strength, and rejuvenation.
Conclusion: Ayurvedic medicine offers a unique perspective on the biomedical diagnosis of cancer that emphasizes restoring wholeness, uses natural remedies, includes a focus on emotional health, and emphasizes prevention strategies.
Introduction
Whole medical systems are usually based on canonical texts and are complete systems of theory and practice that have evolved parallel to biomedicine.1 They have their own systems of diagnosis and treatment independent of biomedicine. Many whole medical systems, such as Ayurveda and Traditional Chinese Medicine, use holistic treatment approaches individualized to both the patient and the disease.2,3
Ayurveda, a Sanskrit term that means “science of the preservation of life,” has a several-thousand-year history originating in the Indian subcontinent. It has evolved over time and remains an acknowledged system of medicine in India, where there are over 400,000 Ayurvedic physicians in practice.4,5 Ayurveda is a comprehensive system of medicine that emphasizes the interconnectedness of the body and mind and maintaining the innate harmony of the individual.
According to Ayurvedic theory, each individual has a unique combination of bioenergetic principles called doshas. There are three doshas (i.e., tridosha) and each represents distinct physiologic processes: vata (principle of movement), pitta (principle of transformation), and kapha (principle of structure). All three doshas are always present, albeit in varying proportions according to the individual. Each individual's health is influenced by the innate proportion of the three doshas, known as prakruti or nature, and by the state of disequilibrium of these doshas, known as vikruti (i.e., the current state of imbalance of the doshas). (For definitions of key Ayurvedic terms, see the Appendix.)
A clinical history and assessment of physical and psychological characteristics are used to determine an Ayurvedic diagnosis. Each patient receives prakruti and vikruti diagnoses based on which treatment decisions are made. Ayurvedic therapeutics include nutrition, lifestyle, exercise (i.e., yoga exercises), mind-body practices (i.e., yoga breathing practices), and botanicals. Typically a multimodality approach based on the Ayurvedic diagnoses is used.
The features of whole medical systems, such as Ayurveda, pose several important challenges for clinical research. Appropriate research methods that account for the unique features of whole systems are required. A primary concern is to balance the ecological validity of the system of study with research concerns, such as reproducibility, internal/external validity, and interpretable data. To perform research examining Ayurveda's utility for cancer supportive care, researchers need to characterize an Ayurvedic perspective on cancer and supportive care. Ayurvedic physicians and their patients inhabit a pluralistic medical system and are acutely aware of the biomedical diagnosis of cancer. Knowledge of the Ayurvedic perspective is critical for an accurate evaluation of the role that Ayurveda can play in cancer care.
The ultimate goal of the research reported here was to develop a manualized protocol6 that would be used in a clinical trial to improve symptoms and quality of life among cancer survivors. The aim of this study was to characterize an Ayurvedic perspective on the pathophysiology, causes, and supportive treatments for a biomedical diagnosis of cancer.
Methods
Hour-long individual interviews were conducted with 10 experienced Ayurvedic clinicians (Vaidyas). The study was approved by the University of California San Francisco institutional review board. Written informed consent was obtained from all participants.
Eligibility criteria
Vaidyas with at least 5 years of clinical experience, as well as experience treating at least 50 cancer survivors in their career, were eligible. The Vaidyas were required to have a high level of training in Ayurveda based on current standards in India and the United States: Vaidyas trained in India were required to have at least a Bachelor of Ayurvedic Medicine and Surgery (BAMS); United States–trained practitioners were required to have 1500 hours of training in Ayurveda or at least 10 years of full-time clinical experience.
Interview approach
The interview guide focused on five domains, as described in Table 1.
Table 1.
Interview Approach with Sample Questions
| Category | Example questions |
|---|---|
| Practitioner qualifications | Please describe your training in Ayurveda. |
| Framework | What Ayurvedic principles would you use to evaluate and treat a cancer survivor? |
| Please describe the pathogenesis of cancer from an Ayurvedic perspective. | |
| Are there any predominant Ayurvedic diagnoses among cancer survivors? | |
| Treatment strategy | What are the goals of your Ayurvedic treatment? |
| Please describe the Ayurvedic treatment modalities that you would find most useful in the treatment of cancer survivors. | |
| Clinical outcomes | In what areas would you expect to find improvement? |
| In what areas would you expect to see no change? | |
| Were there any adverse effects of Ayurvedic treatment on these patients? | |
| Additional comments and recommendations | Please add any additional comments about the Ayurvedic treatment of cancer-related symptoms. |
Methods for analysis of qualitative data
The interviews were audio recorded digitally and then transcribed verbatim by a trained transcriber. Two investigators individually read the transcripts, created an initial coding scheme, and then met to resolve minor differences and develop a codebook, which was subsequently used to code all transcripts. A third study investigator reviewed the analyses in light of the codebook to check for accuracy and completeness. Coded data were then further analyzed for thematic interrelationships by using ATLAS.ti software (ATLAS.ti Scientific Software Development GmbH, Berlin, Germany).
Results
Sample characteristics
Ten Vaidyas consented to be interviewed (100% response rate). Their average number of years of clinical experience was 23 (range, 9–45 years). Six of the Vaidyas had a BAMS degree (a 6-year degree in Ayurveda), 4 had an MD in Ayurveda, and 3 had a PhD in Ayurveda. The MD in Ayurveda is an advanced degree that requires an additional 3 years of training beyond the BAMS and development of an area of specialization. Both BAMS and MD degrees are granted by universities in India. Four of the Vaidyas had clinical practices in India, 4 had practices in the United States, and 2 had practices in both the United States and India.
Themes
The qualitative analyses revealed 4 major themes relating to the Ayurvedic interpretation of biomedical oncology concepts spanning cancer development, progression, treatment, prevention, and supportive care.
Ayurvedic description of the pathophysiology of cancer
The Ayurvedic description of the pathophysiology of cancer uses traditional concepts translated into a modern context. This first theme addresses the exchanges between systems. Although the Vaidyas differed in some of the details, all framed the pathophysiology of cancer using traditional concepts, such as the tridosha theory, the sapta dhatu (7 body tissues), and agni (metabolic strength). In the Ayurvedic theoretical framework, identifying the nidana (causative factors) is a critical step in the evaluation and treatment of a patient:
In terms of cancer, first and most important are the causative factors. Half of the treatment is done when you alleviate the causative factors.
The Vaidyas identified nidana that can be reversed, such as diet and lifestyle factors. They also discussed inherited factors.
Many of the Vaidyas spoke about a weakening of the dhatu agni (weakened metabolic strength of the tissue in which the cancer originates) as important in the development of cancer:
The samprapti (pathogenesis) occurs due to various causes, such as repeated exposure to environmental toxins, which are pitta provoking factors at the deeper cellular level. The increased pitta at the cellular level can cause micro inflammatory changes, which disturb the cellular components of agni called pilu agni and pithar agni. Due to slow pilu agni, pithar agni produces poorly formed tissue. In Ayurvedic pathogenesis, vata is the active dosha and is involved in the process of metastasis. Kapha being heavy and gross is responsible for the abnormal growth of the cells creating the malignant tumor, and the tejas component of pitta enhances the metabolic activity of the cancerous cells. The malignant tissue has strong agni. According to Ayurveda, cancer is a tridoshic disorder which has the capacity to spread due to the interplay of abnormal vata, pitta, and kapha.
Some of the Vaidyas spoke about 2 diagnoses found in traditional textual sources, granthi and arbudha, that may correlate with the modern concept of cancer:
[Traditional concepts of] granthi and arbudha can be understood as similar to a cancer condition. Although it is a kapha predominant disease there is always an association of vata, because the multiplication of cells cannot go in excess without the imbalance of vata in it. And the dhatu agni (metabolic rate of the tissues) is diminished.
However, others felt that granthi and arbudha did not exactly correlate with cancer.
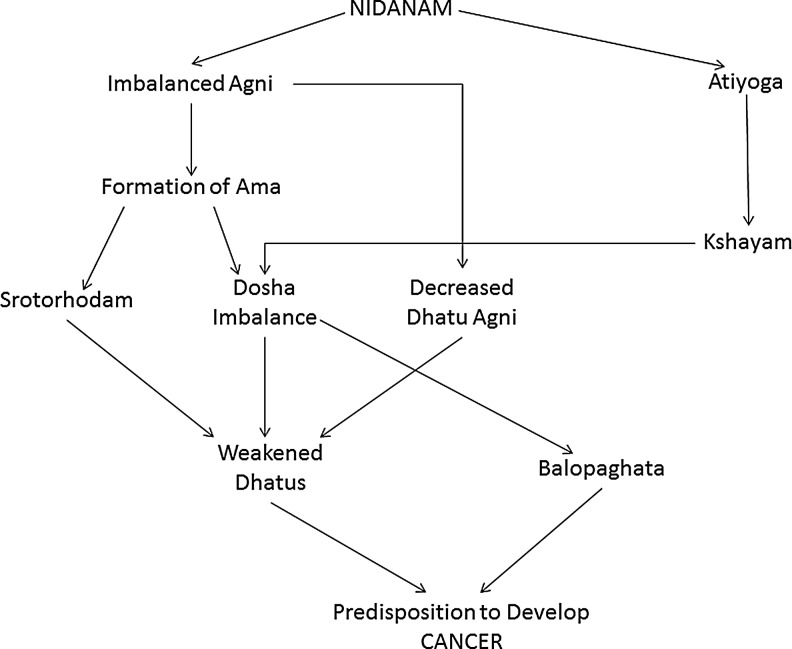
Figure 1 summarizes the Ayurvedic conceptual model for the development of cancer. The participants discussed that the multistep process of the development of cancer occurs over the course of many years, and the particular manifestations of the disease depend on the individual person and their constitution.
FIG. 1.
The Ayurvedic description of the pathophysiology of cancer. Definitions of Ayurvedic terms: Nidanam are causes of a disease and include inherited, dietary, and lifestyle-related causes. Agni represents the digestive strength and metabolic rate of the body tissues. Atiyoga means chronic physical and psychological strain. Ama represents impurities and toxins in the body. Kshayam means degeneration and depletion of the body tissues. Srotorhodam means blockage(s) of body channels, both physical and energetic. Dosha imbalance means an imbalance of vata, pitta, and/or kapha. Dhatu agni is the metabolic rate of the dhatus. Dhatus are the body tissues. Balopaghata means altered immunity or impaired resistance to disease.
Biomedical treatment of cancer results in degeneration and depletion
Although the biomedical treatment of cancer is considered valuable, from an Ayurvedic perspective it results in degeneration and depletion. The Vaidyas spoke about the importance of ojas (vital essence or immunity) and that ojas is depleted due to cancer treatment:
Their ojas is depleted because the ojas is the essence of all the dhatus. They are very depleted in ojas and even all the dhatus, what we call in Ayurveda dhatukshaya (depleted body tissues).
The Vaidyas used traditional Ayurvedic concepts to describe the adverse effects of the biomedical treatment of cancer (i.e., surgery, radiation therapy, and chemotherapy). They discussed the concepts of degeneration and depletion as defining characteristics of the adverse effects of these treatments:
One of the aftermaths is that the whole body is going to feel absolutely devitalized, exhausted, and unable to cope with day-to-day maintenance, with its vital functioning. Nutrition is going to be affected, because the cellular fires will almost be flickering. You have to eat food that is intelligent food, which is filled with prana (vitality). The tissues and the cells, whether you look at chemotherapy, whether you look at radiation, it's going to be left with heat and dryness. There will be a chronic state of low-grade inflammation in the system.
They also commented on the interconnectedness of the body systems and that damage in one system adversely affects other systems:
[Biomedical treatment of cancer] is definitely life-saving, or it's an emergency management. In many cases, it is necessary. You may kill the cancer cell, but the outcome is damage of systems. When the damage happens your efficiency goes and degeneration occurs. When one system is weak it will contribute to weakness in other systems, since all the systems are interconnected.
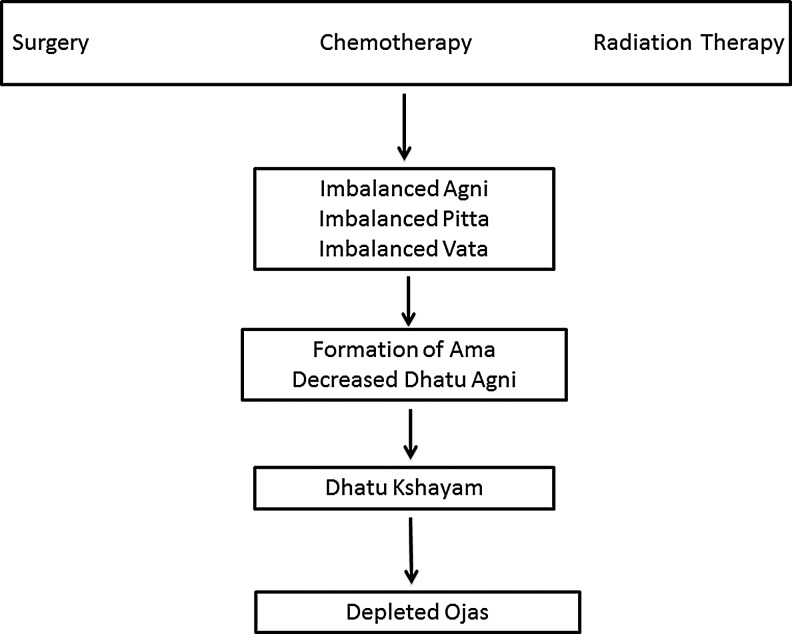
Figure 2 summarizes the effects of biomedical treatment of cancer from an Ayurvedic perspective. These treatments affect agni, vata, and pitta, leading to poor tissue metabolism and impaired ojas.
FIG. 2.
The Ayurvedic description of the effects of cancer treatment. Definitions of Ayurvedic terms: Agni represents the digestive strength and metabolic rate of the body tissues. Ama represents impurities and toxins in the body. Kshayam means degeneration and depletion of the body tissues. Dosha imbalance means an imbalance of vata, pitta, and/or kapha. Dhatu agni is the metabolic rate of the dhatus. Dhatus are the body tissues.
Ayurvedic approach for the treatment of cancer
In cases where the biomedical treatment has stopped working or is not available, an Ayurvedic approach focusing on strengthening digestion, eliminating toxins, reducing tumor growth, and improving tissue metabolism is viewed as useful. Although the Vaidyas agreed that they would not normally use Ayurveda as the primary treatment of cancer, in cases where biomedicine is not possible they would take a specific Ayurvedic approach to treat cancer. This approach exemplifies Ayurvedic interpretations of the nature of cancer that parallel biomedical oncology concepts of the cytoreduction of a tumor:
The general approach to this treatment protocol will be the kindling of dhatu agni, pachana (eliminating toxins), and lekahana (reducing the size of the tumor).
Ayurvedic approach for supportive care
An Ayurvedic approach to cancer supportive care focuses on restoring equilibrium, building mental and physical strength, and rejuvenation. Given the Ayurvedic conceptualization of the adverse effects of the biomedical treatment for cancer, traditional approaches to reintroduce balance in the system were proposed:
It's the role of a Vaidya to create proper equilibrium within the body, because imbalance in the body has the potential to create metastasis.
The holistic view of the body is matched by this holistic approach to treatment:
Post-chemo, post-radiation, sharira balam (physical strength) and satva balam (mental strength) are low. When they are low, recovery is not easy. According to Ayurveda, food and lifestyle are the two controllable reasons for health problems as well as health creation. When you follow an appropriate diet and routine, you are enhancing your health. There are many items available for every patient in their own kitchen. We educate them on that, and then pranayama, yoga, meditation. Then we go ahead with specific herbs and customized formulations. A way to approach herbs and formulations in Ayurveda is to strengthen the physical system, mental system, and immune system. We provide those formulations according to the type of cancer and system or dhatu that is affected.
The Vaidyas agreed that Ayurvedic cleansing therapies (panchakarma) were, in most cases, not advisable immediately after the completion of the biomedical treatment for cancer. They felt that patients must first regain their strength before undertaking panchakarma:
Ayurveda says that there are proper indications for shodana (e.g., panchakarma) and if the patient has recently completed chemotherapy, the body is still toxic. If we do shodana, we are actually pushing the toxins into the deeper tissues. The first thing we have to do is shamana, palliative measures. There will be ama in the body due to chemotherapy and radiation therapy. That ama will be neutralized by the shamana protocol and then we will come to the main line of treatment – shodhana – possibly after six months or three months, depending on prakruiti. Kapha prakruiti people usually detox quickly, pitta takes time, and vata takes still more time.
Discussion
In the exploration of the integration of Eastern and Western medical systems into holistic therapeutic programs, a bridging dialogue has been called for. In this study, the qualitative analysis revealed 4 themes that relate to the correlation of biomedical concepts in oncology with those of Ayurvedic medicine. Although several authors have described cancer from an Ayurvedic perspective using traditional textual sources,7–11 this study appears to be the first to evaluate correlations between Ayurvedic and biomedical oncology concepts using rigorous research methods in addition to traditional textual sources. It is believed that this study provides the first evidenced based description of cancer from an Ayurvedic perspective to date.
Using the traditional approach of samprapti, the participants provided an Ayurvedic view of the pathophysiology of cancer that translated and correlated modern and traditional concepts. Therefore, the samprapti of cancer described in this study represents the optimal Ayurvedic description of cancer that combines traditional and modern biomedical frameworks and integrates textual sources with what is in use today by Vaidyas. The model from this study (Fig. 1) is similar to that proposed by other authors.8,9 Ayurvedic treatment depends on an accurate description of the samprapti. Therefore, these results are relevant to both clinical work and future research efforts in the supportive care and treatment of cancer using Ayurvedic approaches. The Ayurvedic perspectives on cancer that were described in this study were used to develop a manualized protocol for cancer supportive care that is currently being tested in a prospective clinical study.
In the Ayurvedic description of the pathophysiology of cancer, the role of causative factors was highlighted. The Vaidyas discussed classic Ayurvedic perspectives on causes of cancer, which included inherited, dietary, and lifestyle causes, that parallel biomedical causes of cancer. Inherited causes are an important consideration in biomedicine. In addition, parallels exist in biomedicine in terms of dietary causes of cancer. For example, low-fat diets may reduce breast cancer recurrence, and obesity has been linked to endometrial cancer.12 Similar ideas were expressed by the Vaidyas in that kapha-increasing (high-fat) diets could result in an increased risk of cancer. Lifestyle-related causes of cancer are identified by both biomedicine and Ayurveda. For example, research has linked night shift work with cancer incidence.13,14 Ayurveda also refers to the importance of natural biorhythms in maintaining health.
On the basis of the current data, a summary of the tridosha perspective on cancer includes the involvement of kapha to induce growth of tissue, the role of pitta in transforming the tissue from normal to malignant, and the role of vata in the spread of cancer outside of the organ of origin (i.e., metastasis).
Traditional diagnoses (i.e., granthi and arbudha) that are found in classic Ayurvedic texts were suggested to loosely correlate with the biomedical concept of cancer. However, these correlations are imperfect, as was demonstrated in the current data. Some Vaidyas noted that granthi and arbuda were similar to cancer, but others disagreed.
Weakened dhatus and dhatu agnis were highlighted as important Ayurvedic concepts in the pathophysiology of cancer. The Vaidyas suggested that when the dhatus are weakened, that patients are vulnerable to disease and that in particular a weakened dhatu agni predisposes them to cancer in that dhatu. This concept is unique to Ayurveda. However, a parallel exist in biomedicine in the idea of field cancerization, in which particular tissues (e.g., sites in the aerodigestive tract after tobacco exposure) are vulnerable to cancer.15
Agreement was found among the Vaidyas that the biomedical treatment of cancer was valuable. They advocated for integration of Ayurveda rather than limiting Ayurveda to an alternative form of medicine. This sentiment echoes findings from a study of patients who expressed that an integrative approach is preferred to one that excludes one system in favor of another.16 The Vaidyas suggested that the after-effects of biomedical treatment cause degeneration, depletion, and inflammation (Fig. 2). They also discussed the inter-connectedness of body systems. This holistic view of the body is distinctive and contrasts somewhat with the biomedical focus on individual organ systems.
The therapeutic framework for Ayurvedic supportive care after cancer treatment that focuses on restoring equilibrium, building mental and physical strength, and rejuvenation is well matched to the problems patients with cancer face. These patients frequently face physical and psychological symptoms in addition to impaired quality of life after treatment.17 Research on Ayurvedic longevity preparations, called rasayanas, suggest that in addition to reducing the toxicity of chemotherapy, they may have an immune modulating role that may constitute a novel dimension to cancer treatment akin to new directions in cancer immunotherapy.18
The current study has some limitations and several strengths. The study sample was moderately small and as such may not fully represent modern Ayurveda. However, it included very experienced Vaidyas with rigorous university-level training in Ayurveda. Additionally, many of the Vaidyas had advanced degrees in Ayurveda (i.e., MD and PhD) obtained in India, which currently provides the most comprehensive training in Ayurveda available in the world. Although they were all trained in India, 60% practice Ayurveda in the United States.
In conclusion, the correlations between Ayurvedic and biomedical concepts in oncology provide an example of ways in which exchange between traditional and modern systems may enrich perspectives on cancer and supportive care. The exact cause of cancer is not known in most cases. The Ayurvedic perspectives on the development, treatment, after effects of treatment, and supportive care for cancer demonstrate that understanding different perspectives in complex diseases, such as cancer, provides valuable insights. The correlations found in these data between Ayurvedic and biomedical concepts in oncology provide an example of ways in which dialogue can occur between traditional and modern medicine. This dialogue is particularly important in this era of global and integrative medicine.
Appendix 1: Glossary of Key Ayurvedic Terms
Agni: Represents the digestive strength and metabolic rate of the body tissues.
Ama: Impurities and toxins in the body.
Arbudha: A term found in classic Ayurvedic texts, meaning a tumor or growth.
Balam: Literally means strength. Can be specifically sharirabalam (physical strength) or satvabalam (mental strength).
Chikitsa: Ayurvedic therapeutics.
Dhatu: One of the body tissues. Ayurveda describes 7 dhatus (i.e., saptadhatu).
Dhatu agni: The metabolic rate of the body tissues.
Dhatu kshaya: Depleted and weakened dhatus (body tissues).
Dosha: Bioenergetic principle governing human physiology and pathophysiology. There are 3 doshas: vata, pitta, and kapha. The three doshas are often called tridoshas.
Granthi: A term found in classic Ayurvedic texts, meaning a tumor or growth.
Kapha: The dosha representing structure.
Langhan: Treatments that are reducing and cleansing, such as reducing the growth of a tumor.
Nidana: The causes of a disease.
Ojas: The vital essence of the body, often likened to immunity. It is the subtle structural energy behind kapha.
Pachana: Eliminating impurities and toxins. Also called amapachana.
Panchakarma: Ayurvedic therapeutic approach to cleanse the body of abnormal doshas. It involves 5 treatments. Panchakarma is a kind of shodhana.
Pitta: The dosha representing transformation.
Prakruti: The natural state of the doshas that is determined at birth and is unchanging throughout life. It is synonymous with a person's nature or constitution.
Prana: The life energy and the subtle energy behind vata.
Samprapti: Ayurvedic description of the pathophysiology of a disease.
Shamana: An approach to treatment that can include diet, lifestyle, herbs, and mind-body therapies. It is often translated as palliative therapy and is in contrast to shodhana.
Shodhana: The Ayurvedic therapeutic approach to cleanse the body and remove abnormal doshas. Panchakarma is a kind of shodhana.
Tejas: Cellular intelligence and the subtle transformative energy behind pitta.
Tridoshas: Refers to the 3 doshas: vata, pitta, and kapha.
Vikruti: Refers to an imbalanced state of the doshas and may be synonymous with a disease state.
Vaidya: An Ayurvedic physician. Literally “one who knows.”
Vata: The dosha representing kinetics or movement.
Acknowledgments
Dr. Dhruva is supported through National Institutes of Health (NIH)/National Center for Complementary and Alternative Medicine (NCCAM) Mentored Patient-Oriented Research Career Development Award (K23 AT005340). Dr. Hecht is supported by NCCAM-NIH grant # K24 AT007827. Dr. Miaskowski is funded by the American Cancer Society as a Clinical Research Professor. Dr. Kaptchuk is supported by NCCAM-NIH grant # K24 AT004095. We sincerely thank the participants for their valuable contribution to this work.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.National Center for Complementary and Alternative Medicine. What is complementary and alternative medicine? [Home page on Internet] 2008. Online document at: http://nccam.nih.gov/health/whatiscam Accessed September23, 2013
- 2.Ritenbaugh C, Verhoef M, Fleishman S, Boon H, Leis A. Whole systems research: a discipline for studying complementary and alternative medicine. Altern Ther Health Med 2003;9:32–36 [PubMed] [Google Scholar]
- 3.Bodeker G. Integrative oncology meets immunotherapy: new prospects for combination therapy grounded in Eastern medical knowledge. Chin J Integr Med 2012;18:652–662 [DOI] [PubMed] [Google Scholar]
- 4.Department of AYUSH, Government of India. Ayurveda. 2011 [homepage on Internet]. Online document at: http://indianmedicine.nic.in/index.asp?lang=1 Accessed September23, 2013
- 5.Bodeker G, Ong C-K, Burford G, Grundy C, Shein K, Eds. World Health Organization Global Atlas on Traditional & Complementary Medicine. Geneva, Switzerland: World Health Organization, 2005 [Google Scholar]
- 6.Schnyer RN, Allen JJ. Bridging the gap in complementary and alternative medicine research: manualization as a means of promoting standardization and flexibility of treatment in clinical trials of acupuncture. J Altern Complement Med 2002;8:623–634 [DOI] [PubMed] [Google Scholar]
- 7.Sumantran VN, Tillu G. Cancer, inflammation, and insights from ayurveda. Evid Based Complement Alternat Med 2012;2012:306346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh RH. An assessment of the ayurvedic concept of cancer and a new paradigm of anticancer treatment in Ayurveda. J Altern Complement Med 2002;8:609–614 [DOI] [PubMed] [Google Scholar]
- 9.Balachandran P, Govindarajan R. Cancer—an ayurvedic perspective. Pharmacol Res 2005;51:19–30 [DOI] [PubMed] [Google Scholar]
- 10.Garodia P, Ichikawa H, Malani N, Sethi G, Aggarwal BB. From ancient medicine to modern medicine: ayurvedic concepts of health and their role in inflammation and cancer. J Soc Integr Oncol 2007;5:25–37 [DOI] [PubMed] [Google Scholar]
- 11.Prasad GC, Sahu M, Deshpande PJ. Concept of cancer in ayurveda. Anc Sci Life 1982;1:172–176 [PMC free article] [PubMed] [Google Scholar]
- 12.McTiernan A, Irwin M, Vongruenigen V. Weight, physical activity, diet, and prognosis in breast and gynecologic cancers. J Clin Oncol 2010;28:4074–4080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bhatti P, Cushing-Haugen KL, Wicklund KG, Doherty JA, Rossing MA. Nightshift work and risk of ovarian cancer. Occup Environ Med 2013;70:231–237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kamdar BB, Tergas AI, Mateen FJ, Bhayani NH, Oh J. Night-shift work and risk of breast cancer: a systematic review and meta-analysis. Breast Cancer Res Treat 2013;138:291–301 [DOI] [PubMed] [Google Scholar]
- 15.Braakhuis BJ, Tabor MP, Kummer JA, Leemans CR, Brakenhoff RH. A genetic explanation of Slaughter's concept of field cancerization: evidence and clinical implications. Cancer Res 2003;63:1727–1730 [PubMed] [Google Scholar]
- 16.Astin JA. Why patients use alternative medicine: results of a national study. JAMA 1998;279:1548–1553 [DOI] [PubMed] [Google Scholar]
- 17.Bower JE. Behavioral symptoms in patients with breast cancer and survivors. J Clin Oncol 2008;26:768–777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saxena A, Srivastava A, Misra M, et al. An ayurvedic herbal compound to reduce toxicity to cancer chemotherapy: a randomized controlled trial. Ind J Med Paediatr Oncol 2008;29:11–18 [Google Scholar]