Abstract
Objective: Remote monitoring technology (RMT) may enhance healthcare quality and reduce costs. RMT adoption depends on perceptions of the end-user (e.g., patients, caregivers, healthcare providers). We conducted a systematic review exploring the acceptability and feasibility of RMT use in routine adult patient care, from the perspectives of primary care clinicians, administrators, and clinic staff. Materials and Methods: We searched the databases of Medline, IEEE Xplore, and Compendex for original articles published from January 1996 through February 2013. We manually screened bibliographies of pertinent studies and consulted experts to identify English-language studies meeting our inclusion criteria. Results: Of 939 citations identified, 15 studies reported in 16 publications met inclusion criteria. Studies were heterogeneous by country, type of RMT used, patient and provider characteristics, and method of implementation and evaluation. Clinicians, staff, and administrators generally held positive views about RMTs. Concerns emerged regarding clinical relevance of RMT data, changing clinical roles and patterns of care (e.g., reduced quality of care from fewer patient visits, overtreatment), insufficient staffing or time to monitor and discuss RMT data, data incompatibility with a clinic's electronic health record (EHR), and unclear legal liability regarding response protocols. Conclusions: This small body of heterogeneous literature suggests that for RMTs to be adopted in primary care, researchers and developers must ensure clinical relevance, support adequate infrastructure, streamline data transmission into EHR systems, attend to changing care patterns and professional roles, and clarify response protocols. There is a critical need to engage end-users in the development and implementation of RMT.
Key words: : home health monitoring, e-health, telehealth
Introduction
Remote health monitoring technology (RMT), defined as any technology that enables the monitoring of an individual's health status through a remote interface and then transmits the information to a healthcare provider,1 holds promise as a vehicle to improve health and wellness and help manage disease. RMT data may enable clinicians to more effectively detect early onset of disease or disease progression and monitor changes over time.2 In the context of global aging, RMT may help to address shortages in the healthcare workforce while mitigating costs.1,3
Although media sites tout the potential benefits of RMT4–7 and private sector investment nearly doubled in the first half of 2012,8 user-based research in the field is in its infancy. Patients, caregivers, and medical professionals are potential users of RMT, and each brings a unique perspective on the need for and utility of these technologies.2,3 Despite the critical role primary care professionals may play in responding to RMTs, few studies explore their views.9–11
For RMT to improve clinical practice, primary care clinicians must be involved in product development and testing.12 To our knowledge, the factors associated with the adoption of RMT in ambulatory care have not been rigorously explored. Therefore, we conducted a systematic review to better understand the perspectives of primary care clinicians, administrators, and clinic staff regarding the acceptability and feasibility of using RMT in routine adult patient care.
Materials and Methods
Key Questions
We conducted a systematic search for studies that provided data to address the following key questions:
- • Key Question 1. How do primary care clinicians view the use of RMT in routine patient care?
- 1a. What are the major barriers and facilitators to incorporating RMT into routine patient care as perceived by primary care clinicians?
- 1b. How do these barriers and facilitators affect the acceptability of RMT and the feasibility of its adoption?
- • Key Question 2. How do primary care administrators and clinic staff view the use of RMT in routine patient care?
- 2a. What are the major barriers and facilitators to incorporating RMT into routine patient care as perceived by primary care administrators and clinic staff?
- 2b. How do these barriers and facilitators affect the acceptability of RMT and the feasibility of adoption?
Search Strategy
We searched multiple databases (Ovid Medline, IEEE Xplore, and Compendex) for original articles published in English from January 1996 through February 2013. Our search strategy included terms for primary care, RMTs, and possible targets for monitoring (e.g., physiologic parameters, function, cognition). Although we intended to focus the review on care for older adults (i.e., over 65 years of age), we expanded our definition to explore care for patients over 18 years of age (i.e., adults) given the paucity of research. We obtained additional articles by manually screening the bibliographies of pertinent studies and by consulting experts. The search strategy and the initial yields from each database are given in the first section of Supplementary Data (Supplementary Data are available online at www.liebertonline.com/tmj).
Study Selection
We screened the titles and abstracts for inclusion according to prespecified criteria (see the second section of Supplementary Data). Articles selected at the abstract stage underwent full-text review by two investigators (M.M.D. and M.F.). If there was a discrepancy between the two reviewers, a third reviewer determined eligibility and inclusion (D.I.B.).
We included studies of any design on the use of RMT in primary care settings by adult patients with chronic illness. We defined RMT as any technology that enables the monitoring of an individual's health status (e.g., vital signs, heart rate, blood glucose levels, medication management, mental health, physical and cognitive fitness) through a remote interface and then transmits the information to a healthcare provider for review, care management, and/or patient education.1 The information must be transferred electronically to the health professional via download from a device, telephonically, via the Web, or on a smartphone, rather than brought as a written output to a visit at the primary care practice. We included studies where RMT was used in permanent or transitional residential settings, including home, assisted living, adult foster care, nursing home, “independent living,” and rehabilitation centers. Inpatient settings and skilled nursing facilities were excluded.
Included studies reported on the perspectives of primary care clinicians, staff, or administrators regarding the use of RMT for routine patient care, as either primary or secondary outcomes. We also included studies that provided perspectives from a range of healthcare settings that included but were not limited to primary care. We defined primary care clinicians as licensed physicians (MD or DO), nurse practitioners, or physician assistants practicing family medicine, general internal medicine, or pediatrics. Primary care staff included other healthcare providers such as RNs, social workers, occupational therapists, and care coordinators, as well as office staff and administrators.
Data Abstraction and Synthesis
We abstracted data on the study objectives and design, the target patient population, RMT type, mode of data transmission, and processes used to access, review, and respond to the data. We also identified the training of the medical professionals and personnel providing feedback on the technologies and their perspectives as related to our key questions.
We conducted a qualitative synthesis of the studies to describe how patient data were remotely gathered and monitored. We highlight user perceptions about the use, acceptability, and feasibility of implementing the RMT in the primary care setting. Because the included studies used qualitative approaches with heterogeneous study designs, we were unable to apply systematic methods for rating study quality for risk of bias.
Although the objective of this review was to examine the perspectives of primary clinicians separately from the perspectives of staff and administrators, several studies gathered perspectives from multiple informants, including primary care clinicians or staff, non–primary care health professionals, and patients. We could not tease out the views of only primary care participants, so we report on these general perspectives as findings are related to RMT use in primary care.
Results
Study Characteristics
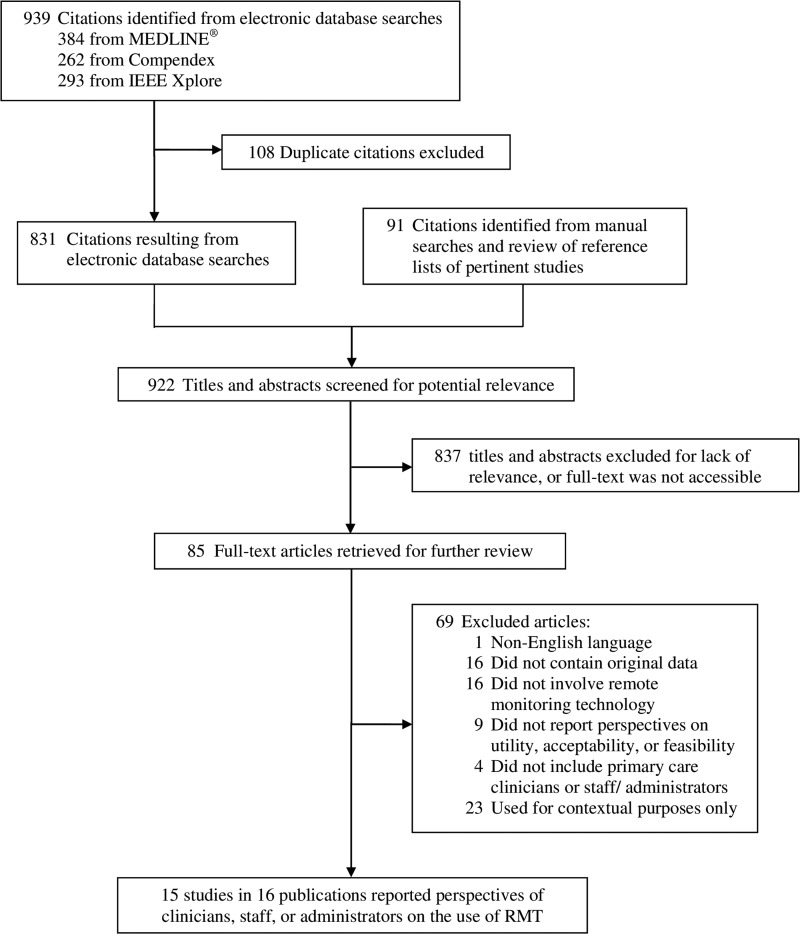
Of 939 abstracts and titles of potentially relevant studies, 15 studies reported in 16 publications met our inclusion criteria (Fig. 1).11,13–27 Six studies provided perspectives from primary care clinicians.16,19–23 Four studies published in five reports provided perspectives from clinical specialties including but not limited to primary care.11,17,25–27 Seven studies reported perspectives from primary care staff, administrators, or unspecified healthcare professionals.13–15,18,20,23,24
Fig. 1.
Literature search and selection. RMT, remote monitoring technology.
Table 1 summarizes key details of the included studies, describing the target patients, RMT used, mode of data transfer and processing, informant characteristics, and methods used to gather perspectives. Table 2 highlights the themes, identified across the studies, associated with the acceptability and feasibility of using RMT in primary care. Abstracted data on study characteristics are detailed in Supplementary Table S1. Supplementary Table S2 summarizes the views expressed by primary care clinicians, staff, and administrators regarding the barriers and facilitators of incorporating RMT in routine adult patient care by individual study.
Table 1.
Study Characteristics, Mode of Data Collection, and Stakeholder Perspectives
| REFERENCE (YEAR) | STUDY NAME OR SETTING | PATIENT CHARACTERISTICS, MORBIDITY, AND SAMPLE SIZE | RMT USED AND PHYSIOLOGIC DATA GATHERED | MODE OF DATA COLLECTION, TRANSMISSION, AND REVIEW | INFORMANT CHARACTERISTICS AND METHODS USED TO GATHER PERSPECTIVES | WAS THE TECHNOLOGY FAVORABLY RECEIVED BY CLINICIANS? | WAS THE TECHNOLOGY FAVORABLY RECEIVED BY STAFF AND/OR ADMINISTRATORS? |
|---|---|---|---|---|---|---|---|
| Abraham and Rosenthal13 (2008) | VHA Office of Care Coordination Care and Coordination Home Telehealth Program | Veteran patients with CHF, COPD, DM, HTN, or wound care; high utilization and hospitalization; multiple medications; and home environment conducive to remote monitoring; number of patients not specified | The Health Buddy devices and the Viterion 100 collected BP, blood oxygen, blood glucose, weight, temperature, heart rate, oxygen intake, and peak bodily fluids flow. | Patient-entered data were transmitted via telephone lines to a central monitoring service. | Semistructured interviews with five VA personnel: the physician program director, the nurse lead care coordinator, the program support assistant, the prosthetics staff manager, and the data technician | — | Yes, but staff ratio should be re-evaluated. |
| Fursse et al.14 (2008) | A medium-sized primary care practice northwest of London, United Kingdom | 51 patients with DM, CHF, or HTN | The RMT unit included a touchscreen device to allow manual entry of certain data (glucose) and attached peripheral devices as appropriate to the medical condition: CHF patients received weight scales, SpO2, and BP attachments; diabetes patients received a glucometer; and HTN patients received a BP unit. | Patients entered daily physiological measurements into the unit. Data were sent via the participant's telephone line to the primary care practice. | Unclear: reports user satisfaction of the primary healthcare team, but methods used for gathering perspectives are not reported | — | Yes |
| Gagnon et al.15 (2006) | Project 1 Quebec City, Canada Project 3: Lorraine region, France | Project 1: 26 patients with COPD and cardiac insufficiency Project 3: 30 patients with chronic kidney insufficiency |
Project 1: The patient's home was equipped with an RMT device that transmitted patient data to a central monitor located in the community health organization. Project 3: Experimental patients received “Diatelic” equipment, a remote surveillance system for patients with chronic kidney insufficiency who are on continuous ambulatory peritoneal dialysis that collects data on weight, BP, and temperature. |
Project 1: Data (NOS) were transmitted to the central monitor located in the community health organization. Project 3: Patients transmitted self-entered health data daily to the central monitoring service via a secure Internet connection. |
Unclear: the methods used for gathering informants' perspectives are not described. The primary sources are conference proceedings that we were not able to access; two were non-English publications. | — | Project 1: Yes Project 3: NR |
| Goodrich et al.16 (2011) | Stepping up to Health (SUH) Internet-mediated walking program in two family practice clinics in a large U.S. healthcare system | 37 adults with CAD, DM, or BMI >25 kg/m2; mean age, 45.2 years | Patients were asked to wear a pedometer to gather step count for 6 weeks. | Patients uploaded step-count data to a server via the Internet. Data were available to their clinicians through an online interface. | Semistructured interviews with six primary care physicians and seven medical assistants | Yes, but usage was low. | — |
| Hardisty et al.17 (2011) Peirce et al.27 (2011) |
Interviews with various clinical professionals, medical and informatics academics, and others with policy-level roles for healthcare IT or chronic disease, United Kingdom | COPD, CHF, DM; number of patients not specified | Physiological variables included pulse rate and SpO2. | Patients measured their physiological variables and answered questions about symptoms. Patient-entered data were transmitted to a central database. Review of the data not described | Mixed methods, including a literature review and focus groups with a mix of informants (n=26) from academic, clinical (specialist, generalist, consultant, and nursing), policy-making, telehealth, and medical technology development backgrounds | Mixed | Mixed |
| Hicks et al.18 (2009) | Home health agency in rural Midwest, United States | 47 monitored patients and 47 controls with CVD, lung disease, cancer, DM, infections, or surgical aftercare | An FDA Class II medical device that collects key vital signs (BP, heart rate, SpO2, and temperature) and information on a series of questions on a patient's perceived health status | User information was automatically sent securely via a standard telephone line means to the central monitoring service center. | Interviews and Likert scale questions gathered perspectives of six home health agency staff: LPN, social worker, physical therapist, PT aide, speech therapist, and RN. | — | Yes |
| Kim et al.25 (2011) | Qualitative study of user experience with ubiquitous healthcare in Korea | NR | NR | NR | In-depth interviews with six MDs and five nurses about ubiquitous healthcare on subjective user experience, expectation, business prospects, and prerequisites for the success of the ubiquitous healthcare market | Yes | Yes |
| Kobb et al.19 (2003) | VHA Rural Home Care Project, southern Georgia and north Florida, United States | 281 Veterans with high utilization, most commonly for HTN, CHF, COPD, DM, or cardiac arrhythmias | Equipment was selected according to patient needs and included an in-home messaging device, the Health Buddy from Health Hero Network, American Telecare's audiovideo units, the Aviva 1010SLX with peripheral vital sign monitoring, Wind Currents TeleVyou 500 videophone, and the telephone. | Patients transmitted data from monitoring equipment via regular analog telephone service. Data were reviewed by project care coordinators. | Interviews and satisfaction surveys among 57 VA primary care providers | Yes | — |
| Lamothe et al.24 (2006) | Remote monitoring pilot project in urban and rural Manitoba and Quebec, Canada | 82 patients with high utilization for COPD, cardiac insufficiency, HTN, or DM | Patients were equipped with a local monitor (HomMed Sentry; Honeywell) to which peripheral devices were connected. Weight, temperature, BP, SpO2, pulse, blood glucose, lung function, ECG, and blood clotting measures could be recorded as needed. | Patients transmitted their data daily to a central monitoring service via wireless connection or telephone line. | 82 individual interviews and 5 group interviews with managers, partners, healthcare professionals NOS, and patients | — | Yes |
| Langstrup20 (2008) | Online asthma monitoring in eight primary care practices in Denmark | Patients with asthma; number not specified | LinkMedica, a Danish online asthma and allergy portal developed by AstraZeneca, to record and transmit peak flow readings | Patients entered peak flow readings in an online diary and were advised to log-on from home each day; clinicians could review patient data online and opt to use a decision support tool. | Ethnographic case study including semistructured interviews with eight clinicians and one nurse | No | Mixed |
| Liddy et al.21 (2008) | A family health network in semirural eastern Ontario, Canada (this study was nested in a larger trial called the Anticipatory and Preventive Team Care [APTCare] project.) | 22 patients who were frail, age 50+ years, with life expectancy >6 months, excluding severe cognitive impairment or language barrier | Monitoring technologies included a BP monitor, wired or wireless weight scale, wireless glucometer, wireless pulse oximeter, peak flow meter, and stethoscope chest piece. | Patient-entered data were transferred via telephone lines to a secure server at the manufacturer's data center. Data were uploaded to a secure Web-based application that allowed care providers to review it from any location with Internet access. | In-depth interviews with eight physicians, 3 nurse practitioners, and one pharmacist | Yes | — |
| Terschuren et al.22 (2007) | A primary care practice in rural Germany (a larger study of the same intervention is reported by van den Berg et al.23) | 8 patients with CHF, DM, or at risk of developing glaucoma | Devices included a 1-lead ECG meter, electric scale, sphygmomanometer, teletonometer, and blood glucose meter. | All data were transmitted to a central monitoring service center, which then transferred the data into the patient's digital file at the primary care clinic. | Unclear; reports clinician perspectives, methods not described | Yes | — |
| Thompson and Thielke11 (2009) | University of Washington, Seattle | Older adults, NOS; number of patients NR | NR | NR | Focus groups with an unspecified number personnel from nursing, medicine, PT, psychiatry, psychology, and massage therapy | Mixed | Mixed |
| Ure et al.26 (2012) | Four practices in lower-income areas of Lothian, Scotland, United Kingdom | 27 patients with moderate/severe COPD | TELESCOT COPD telemonitoring service: patients used a touchscreen computer to record a validated daily symptom score, including FEV1 taken with Bluetooth-linked monitoring devices. | Data were transmitted via a dedicated broadband link to the central monitoring service. | Semistructured interviews with a mix of 18 providers (GPs, practice nurses, hospital-based respiratory nurses, nurse managers, physiotherapy managers, physiotherapists) and 2 nonclinical managers; focus groups with 6 community nurse managers | Mixed | — |
| Van den Berg et al.23 (2009) | AGnES-practice concept in rural Germany | 48 patients with chronic illness and limited mobility | Patients were trained to use the following devices: (1) system digital scale/sphygmomanometer (34 patients); (2) 1-lead ECG (8 patients); (3) system intraocular pressure/sphygmomanometer/blood glucose meter (4 patients); (4) 12-lead ECG (2 patients). | Patients or their caregivers took daily measurements and transferred data via a secure Internet connection to the data service center. | A questionnaire elicited the perceptions of two clinicians and three RNs. | Yes | Yes |
AGnES, German abbreviation for general practitioner (GP)-supporting, community-based, e-health-assisted, systematic intervention; BMI, body mass index; BP, blood pressure; CAD, coronary artery disease; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; CVD, cardiovascular disease; DM, diabetes mellitus; ECG, electrocardiograph; FDA, Food and Drug Administration; FEV1, forced expiratory volume in the first second; HTN, hypertension; IT, information technology; NOS, not otherwise specified; NR, not reported; PT, physical therapy; RMT, remote monitoring technology; SpO2, oxygen saturation; VA, Veterans Administration; VHA, Veterans Health Administration.
Table 2.
Thematic Factors Associated with Acceptability and Feasibility of Incorporating Remote Monitoring Technology into Routine Primary Care for Adult Patients
| THEME | DESCRIPTION | REFERENCE (YEAR) |
|---|---|---|
| Supports early intervention and follow-up (facilitated by alert system) | Implementation of RMT perceived as useful for eligible patients by improving monitoring, follow-up, and diagnosis. RMT can help identify emerging health issues, aid in detection of other health issues, and prompt clinical interventions. However, a few expressed concerns regarding overtreatment from increased recognition of exacerbations. Alerts (via e-mail, fax, EHR notifications) help clinicians/staff assess when outreach is needed. RMT use may be facilitated if (a) alerts are tailored to specific users (e.g., family versus clinicians) or (b) electronic alerting systems are developed (most alerts triggered following nurse inspection). |
Fursse et al.14 (2008) Gagnon et al.15 (2006) Goodrich et al.16 (2011) Hardisty et al.17 (2011); Peirce et al.27 (2011) Kim et al.25 (2011) Kobb et al.19 (2003) Lamothe et al.24 (2006) Liddy et al.21 (2008) Thompson and Thielke11 (2009) Ure et al.26 (2012) Van den Berg et al.23 (2009) |
| Uncertain medicolegal liability | Informants expressed concern regarding the medicolegal liability associated with receiving RMT data. In particular, there was uncertainty regarding who was supposed to respond to critical values and how quickly. | Gagnon et al.15 (2006) Hardisty et al.17 (2011); Peirce et al.27 (2011) Kim et al.25 (2011) Liddy et al.21 (2008) Van den Berg et al.23 (2009) |
| Fosters direct patient education | RMT served as a direct patient education tool (even without involvement of medical clinicians and staff ). Providing RMT data directly to the patient can lead to improvements in healthcare. | Abraham and Rosenthal13 (2008) Langstrup20 (2008) Liddy et al.21 (2008) |
| Data actionable and of clinical relevance | RMT data must be of clinical importance, from a trusted source, and relevant to the goals of the medical providers. It is helpful if the data are tailored to individuals (e.g., uses their personal baseline). RMT data should be actionable (e.g., you can make a change based on data that have the potential to improve health). | Hardisty et al.17 (2011); Peirce et al.27 (2011) Kim et al.25 (2011) Langstrup20 (2008) Liddy et al.21 (2008) Thompson and Thielke11 (2009) Ure et al.26 (2012) Van den Berg et al.23 (2009) |
| Ease of access and functional interface facilitates use | RMT should be easy to use and convenient to access across multiple settings. Ideally, the RMT interfaces directly with existing clinic systems (e.g., EHR) and doesn't require logging-in to a separate system. The RMT interface should be informative. Data presented in summaries or graphs are helpful. | Abraham and Rosenthal13 (2008) Gagnon et al.15 (2006) Goodrich et al.16 (2011) Hicks et al.18 (2009) Kim et al.25 (2011) Lamothe et al.24 (2006) Ure et al.24 (2012) |
| Changing clinical roles and patterns of clinical care | Use of RMT contributed to changes in clinician and staff roles, as well as in patient relationships. Although clinicians wanted to review RMT data during patient visits, there was not always adequate time. Frequently, the RMT allowed clinicians to delegate tasks to ancillary staff, contributing to increased autonomy for nursing staff. Use of RMT may reduce the need for face-to-face visits; some expressed concern this could lead to increased social isolation for patients and decreased quality of care. Communication between all involved stakeholders is critical. | Gagnon et al.15 (2006) Goodrich et al.16 (2011) Hicks et al.18 (2009) Kim et al.25 (2011) Lamothe et al.24 (2006) Liddy et al.21 (2008) Terschuren et al.22 (2007) Thompson and Thielke11 (2009) Van den Berg et al.23 (2009) |
| Support by and training for ancillary staff | Ancillary staff played critical roles in processing and reviewing RMT data so as not to overburden or overwhelm clinicians. However, the time required for staff to process RMT data was often underestimated as staff must respond ad hoc to patient needs in addition to delivering pre-established interventions. Additional staff training may also be needed. | Abraham and Rosenthal13 (2008) Gagnon et al.15 (2006) Kim et al.25 (2011) Lamothe et al.24 (2006) Langstrup20 (2008) Van den Berg et al.23 (2009) |
| Engaging end-users critical to adoption | Clinicians and staff had variable adoption of RMT. Not all clinicians used the system—and of those who do, not all use it in the same ways. Target users need to be involved in product development and implementation. | Goodrich et al.16 (2011) Hicks et al.18 (2009) Kim et al.25 (2011) Langstrup20 (2008) |
EHR, electronic health record; RMT, remote monitoring technology.
Key Question 1. Views of Primary Care Clinicians on Incorporating RMT
Eleven publications provided data about clinicians' perspectives (Table 1).11,16,17,19–23,25–27 Three studies were conducted in the United States,11,16,19 one in Canada,21 one in Denmark,20 two in Germany,22,23 and one in Korea,25 and two studies in the United Kingdom were published in three reports.17,26,27 Clinicians in several studies conveyed positive views about RMT, and some reported RMT resulted in a decrease in workload due to delegation of activities to ancillary staff. Emerging themes included concerns about the potential for lower quality of care due to fewer face-to-face patient visits, increased provider burden and insufficient staffing for monitoring and responding to data, inconvenience resulting from poor integration between RMT and the clinic's electronic health record (EHR), and uncertain medicolegal liability (see Table 2).
Clinicians expressed unfavorable views of RMT use in two studies.16,20 Goodrich et al.16 studied an intervention in which sedentary adult patients wore a pedometer for 6 weeks and uploaded data to a Web-based system accessible by patients and clinicians. Although clinicians noted that the graphical display of patients' walking progress was informative, they found it inconvenient that data were not integrated into their EHR.16 The extra time required to locate the Web site, remember passwords, and log-in as well as lack of time for physical activity discussions during patient visits presented barriers to using the interface. Langstrup20 had patients with asthma record daily peak flow readings in an online diary that could be accessed by healthcare personnel. Clinicians expressed low interest in examining patients' peak flow data, questioned their role in encouraging patients to use the online system, or disagreed with the decision support functions. These clinicians indicated that RMT implementation was limited because patients did not use the system, rather than being due to clinician-related factors.20
Two related studies in rural Germany reported that clinicians had positive views about the RMT.22,23 In these studies, patients with heart failure, diabetes, or risk of developing glaucoma were equipped with and trained to use electrocardiogram meters, scales, sphygmomanometer, teletonometer, and blood glucose monitors. Patients transferred physiologic data via the public telephone network to the data service center, which then transmitted data by secure Internet connection directly into a digital patient file at the primary care clinic. Data were transferred daily, weekly, or when patients had symptoms, depending on clinician guidance and the type of data collected. The data service center alerted clinicians by fax when monitoring values exceeded preset thresholds. During the study clinicians delegated an increasing number of monitoring and intervention tasks to qualified RNs, which reduced clinician workload and saved time from traveling.22,23
Four studies in five publications reported multiple perspectives that included, but were not limited to, representatives from primary care. Participants included individuals from a range of healthcare services (e.g., nursing, medicine, mental health), academic (e.g., medicine, informatics) and nonacademic settings (e.g., policy-making, medical technology development).11,17,25–27 These informants conveyed concerns about collecting excessive data without clinical relevance and that monitoring for ongoing care (e.g., an alert to caregivers or family members for a one-time missed dose of medication) should be differentiated from monitoring for clinical practice (e.g., an alert for a pattern of multiple missed doses of medications).11,17,27 Some informants expressed concern that RMTs could lead to fewer patients visit and reduce quality of care25 or worsen the isolation, loneliness, and morale of elderly patients.11 Uncertainty regarding liability for maintaining the accuracy of the system and making the correct clinical response(s) was also identified.17,25,27 Informants suggested protocols with response hierarchies related to RMT alert severity should be developed.17,27 In one study, however, the interpretation of a threshold trigger varied with the context of the individual patient, and clinicians raised concerns about the risks of overtreatment and adverse effects from increased prescribing.26 Challenges associated with implementing RMTs that are not integrated with EHR systems, as well as insufficient resources for clinicians or staff to monitor data, also emerged.25 Kim et al.25 proposed several essential elements for the successful expansion of RMT, including cooperation among interested groups, active participation of medical staff who will be using equipment in the design, and a business model that addresses customers' needs.
Key question 2. Views of Primary Care Administrator and Staff on Incorporating RMT
Seven publications reported on perspectives of clinic staff or administrators (Table 1). Two studies were conducted in the United States,13,18 one in Canada,24 one in the United Kingdom,14 one in Germany,23 and one in Denmark.20 One publication reported findings from two studies conducted in Canada and France.15 In general, staff held positive views about using RMT but expressed concerns about workload and staffing.13,15,24 In some studies, nurses reported greater professional autonomy with RMT use.15,20,23,24 The need for better integration between RMT data and the patients' EHRs was also noted.15
In a study of a multisite RMT program in Canada, interviews were conducted with 82 informants, including managers, patients, and healthcare professionals (training unspecified).24 The program equipped chronically ill patients with devices, as indicated for disease status, which transmitted data on weight, temperature, and other factors to the regional primary care organization where a nurse responded to alerts by phone or with home visits. Healthcare providers indicated that the RMT resulted in higher quality of services, helped avoid potential visits to the emergency room through more rapid treatment adjustment, and enabled identification of new clinical problems. Introduction of the RMT program stimulated more efficient communication networks among patients, nurses, and doctors in the hospital and homecare setting. However, several factors were challenging for managers and providers, including responding ad hoc to patients' alerts, developing clinical competencies for expanded services, and scheduling and training demands.24
Nursing staff played critical roles managing and responding to RMT data. Greater autonomy among nurses, from the delegation of medical decision making and other tasks usually restricted to clinicians, was noted in several studies.15,20,23,24 One study reported “groundbreaking” shifts in responsibilities from clinician to nursing staff as study nurses trained the patients, installed the devices, and controlled data.23 In another study of online asthma monitoring, RMT data helped establish connections between the nurse and the patient and allowed the nurse to override inaccurate system alerts.20
Two studies highlight the need for additional staff time to review and respond to RMT data. One study estimated the time required for a lead nurse care coordinator to enroll patients, review daily RMT data, and complete all additional medical and administrative requirements was 62.88 h/week if the program's maximum nurse/patient ratio of 1:125 was reached; thus study staffing was inadequate.13 In another study, in which one nurse centrally monitored 26 patients with chronic obstructive pulmonary disease and cardiac insufficiency while a second nurse responded to alerts and conducted home visits, project managers often underestimated the time required to implement the program.15 Additionally, RMT activities were often conducted in isolation, raising the need for better integration with regular homecare nursing services and other healthcare personnel.15
Discussion
There is a paucity of published research exploring primary care clinician, administrator, and staff perspectives on the acceptability and feasibility of incorporating RMT in routine patient care. Only 15 studies met our inclusion criteria for this review. These studies are heterogeneous by country, type of RMT used, patient and provider characteristics, and method of implementation and evaluation—all of which preclude definitive conclusions about the perceived benefits and feasibility of implementing RMTs in routine primary care.
However, several findings may inform future development and implementation of RMT in primary care. First, aligning the method for data transmission with clinic workflow appears critical. Challenges to adoption emerged when technologies had to be accessed through a separate Web interface.16,20 Technologies that directly transferred to a clinic's EHR or that generated alerts when values exceed a preset threshold were more positively received.22,23 Second, concerns emerged regarding the burden clinicians and staff experienced in reviewing additional data from RMTs.11,17,25 Although the few studies using ancillary staff to help review the data tended to have positive assessments, authors frequently noted that actual time required to review and respond to the data exceeded allocated staff resources.13,15 Supporting appropriate infrastructure for data management as well as developing protocols that reduce the legal liability implications11,17,25 will be critical.
These studies also highlight how perceived clinical relevance, technology functionality, and context influence adoption. Gathering data that had clinical relevance was critical; some RMTs may be better suited more for use by patients or caregivers rather than by primary care professionals.11,20,28 Additionally, automatic alerts or clinical decision support tools in the RMTs that do not account for variations in a patient's health status (e.g., temporary colds and flu) may undermine system trust.20 As new RMTs are introduced, responsibilities may shift between clinicians and nursing staff. Therefore training, and attention to local contexts, will be important to consider during implementation.22–24 Finally, these studies span various countries and healthcare systems, and the pressures for RMT adoption may vary considerably based on existing payment structures and models of care provision. Based on the number of citations meeting our inclusion criteria, European interest in RMT in healthcare appears to be greater than that in the United States.
Some limitations in this review must be acknowledged. Although we comprehensively searched academic journals, as well as two engineering databases (IEEE Xplore and Compendex), using standard systematic review protocols, only a few articles met our inclusion criteria. Our review may not have captured relevant studies that were not indexed in the databases we searched. Additionally, many studies had small sample sizes, ranging from 122 to 57,13 with a median of 10 informants. Articles that focused on the effectiveness of interventions often did not report on perceived acceptability and feasibility in a systematic way, failing to clearly document method of participant selection, data collection, and/or analysis. In some cases, conclusions about perceptions may stem from the authors' views on the study, rather than on the experiences of frontline clinical informants. Finally, some studies focused on perceptions from general informants, including primary care as well as other health professionals, rather than participants from an actual intervention.11,17,25,27
Despite these limitations, our review informs this emerging field. Although authors emphasize the importance of engaging stakeholders in the development and implementation of RMT, our findings suggests that primary care clinicians, administrators, and staff may not routinely be involved. Future research should:
a. Determine what types of RMT primary care clinicians would be interested in using, with particular attention to how preferences vary according to particular disease conditions and their associated clinical management demands
b. Identify which types of RMT are best suited for use in primary care settings and which may be more appropriate for other users (e.g., patients, caregivers)
c. Explore staff requirements to adequately track and appropriately respond to RMT data. This may address important legal concerns, and findings may vary by country.
d. Improve RMT integration with EHRs and clarify processing procedures while evaluating the impact on technology adoption
e. Test models of implementation and dissemination of RMTs in primary care using rigorous research designs with adequately powered sample sizes
Conclusions
RMT systems are being actively developed as strategies to improve upon usual care while reducing rising healthcare costs. The studies included in this review highlight that for RMT to be adopted as part of routine primary care, researchers and developers must improve data transmission into clinic EHRs, support adequate infrastructure for data processing, ensure clinical relevance and “fit” of technologies within primary care workflow, maintain quality of clinical care, and respond to changes in patient care patterns and professional roles.
Supplementary Material
Acknowledgments
We thank Andrew Hamilton, Oregon Health & Science University (OHSU) senior reference and instruction librarian, for his assistance with the search strategy. Funding for this project is provided by the Oregon Roybal Center for Translational Research on Aging (grant P30AG024978) at OHSU, Portland, OR, and by a Clinical and Translational Science Award to OHSU (grant 1 UL1 RR024140 01 from the National Center for Research Resources, National Institutes of Health). J.K.'s time was supported by grants P30AG024978 and P30AG008017 from the National Institute on Aging, National Institutes of Health.
Disclosure Statement
N.V. is an employee of Intel Corporation. M.M.D., M.F., J.K., and D.I.B. declare no competing financial interests exist.
References
- 1.Sarasohn-Kahn J. The connected patient—Charting the vital signs of remote health monitoring. California Health Foundation. 2011. Available at www.chcf.org/publications/2011/02/the-connected-patient (last accessed March25, 2014)
- 2.Alwan M, Nobel J. State of technology in aging services: Summary. Center for Aging Services Technologies. March2008. Available at www.leadingage.org/uploadedFiles/Content/About/CAST/Resources/state_technology_summary.pdf (last accessed August27, 2012)
- 3.Ahern DK, Kreslake JM, Phalen JM. What is eHealth (6): Perspectives on the evolution of eHealth research. J Med Internet Res 2006;8:e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hill C. Tech to track your aging parents. Smart Money. 2011. Available at www.smartmoney.com/personal-finance/elder-care/tech-to-track-your-aging-parents-1294880369537/ (last accessed January20, 2011) [Google Scholar]
- 5.Olson EG. The virtual doctor visit: New technology is helping elderly patients and those with chronic diseases monitor their condition from the comfort of home. The Washington Post November17, 2009. Available at http://www.washingtonpost.com/wp-dyn/content/article/2009/11/16/AR2009111602900.html?hpid=artslot (last accessed March25, 2014) [Google Scholar]
- 6.Singer N. In a graying population, business opportunity. The New York Times February5, 2011. Available at http://www.nytimes.com/2011/02/06/business/06aging.html?pagewanted=all&_r=0 (last accessed March25, 2014)
- 7.Terry K. Home monitoring devices: Why innovation doesn't pay in healthcare. The CBS Interactive Business Network (BNET). 2010. Available at www.bnet.com/blog/healthcare-business/home-monitoring-devices-why-innovation-doesn-8217t-pay-in-healthcare/1396 (last accessed February3, 2011)
- 8.Burrill & Company. Digital health takes hold with venture investors, says Burrill & Company: First half of 2012 sees private financings nearly double for the emerging sector. Available at www.burrillandco.com/content/news/PR-Month-End%20July%202012-v4.pdf (last accessed August27, 2012)
- 9.Kang HG, Mahoney DF, Hoenic H, et al. In situ monitoring of health in older adults: Technologies and issues. J Am Geriatr Soc 2010;58:1579–1586 [DOI] [PubMed] [Google Scholar]
- 10.Martin S, Kelly G, Kernohan WG, McCreight B, Nugent C. Smart home technologies for health and social care support. Cochrane Database Syst Rev 2008;(4):CD006412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thompson HJ, Thielke SM. How do healthcare providers perceive technologies for monitoring older adults? Conf Proc IEEE Eng Med Biol Soc 2009:4315–4318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bitterman N. Design of medical devices—A home perspective. Eur J Intern Med 2011;22:39–42 [DOI] [PubMed] [Google Scholar]
- 13.Abraham C, Rosenthal DA. Merging home and health via contemporary care delivery: Program management insights on a home telehealth project. Comput Inform Nurs 2008;26:273–281 [DOI] [PubMed] [Google Scholar]
- 14.Fursse J, Clarke M, Jones R, Khemka S, Findlay G. An automated personalised intervention algorithm for remote patient monitoring. Stud Health Technol Inform 2008;136:181–186 [PubMed] [Google Scholar]
- 15.Gagnon M-P, Lamothe L, Hebert M, Chanliau J, Fortin J-P. Telehomecare for vulnerable populations: The evaluation of new models of care. Telemed J E Health 2006;12:324–331 [DOI] [PubMed] [Google Scholar]
- 16.Goodrich DE, Buis LR, Janney AW, et al. Integrating an internet-mediated walking program into family medicine clinical practice: A pilot feasibility study. BMC Med Inform Decis Mak 2011;11:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hardisty AR, Peirce SC, Preece A, et al. Bridging two translation gaps: A new informatics research agenda for telemonitoring of chronic disease. Int J Med Inform 2011;80:734–744 [DOI] [PubMed] [Google Scholar]
- 18.Hicks LL, Fleming DA, Desaulnier A. The application of remote monitoring to improve health outcomes to a rural area. Telemed J E Health 2009;15:664–671 [DOI] [PubMed] [Google Scholar]
- 19.Kobb R, Hoffman N, Lodge R, Kline S. Enhancing elder chronic care through technology and care coordination: Report from a pilot. Telemed J E Health 2003;9:189–195 [DOI] [PubMed] [Google Scholar]
- 20.Langstrup H. Making connections through online asthma monitoring. Chronic Illn 2008;4:118–126 [DOI] [PubMed] [Google Scholar]
- 21.Liddy C, Dusseault JJ, Dahrouge S, Hogg W, Lemelin J, Humbert J. Telehomecare for patients with multiple chronic illnesses: Pilot study. Can Fam Physician 2008;54:58–65 [PMC free article] [PubMed] [Google Scholar]
- 22.Terschuren C, Fendrich K, van den Berg N, Hoffmann W. Implementing telemonitoring in the daily routine of a GP practice in a rural setting in northern Germany. J Telemed Telecare 2007;13:197–201 [DOI] [PubMed] [Google Scholar]
- 23.van den Berg N, Fiss T, Meinke C, Heymann R, Scriba S, Hoffmann W. GP-support by means of AGnES-practice assistants and the use of telecare devices in a sparsely populated region in Northern Germany—Proof of concept. BMC Fam Pract 2009;10:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lamothe L, Fortin J-P, Labbe F, Gagnon M-P, Messikh D. Impacts of telehomecare on patients, providers, and organizations. Telemed J E Health 2006;12:363–369 [DOI] [PubMed] [Google Scholar]
- 25.Kim J, Kim S, Kim H, Kim K, Yang S, Shin Y. Development of implementation strategies for u-health services based on the healthcare professionals' experiences. Telemed J E Health 2011;17:80–87 [DOI] [PubMed] [Google Scholar]
- 26.Ure J, Pinnock H, Hanley J, et al. Piloting tele-monitoring in COPD: A mixed methods exploration of issues in design and implementation. Prim Care Respir J 2012;21:57–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peirce SC, Hardisty AR, Preece AD, Elwyn G. Designing and implementing telemonitoring for early detection of deterioration in chronic disease: Defining the requirements. Health Inform J 2011;17:173–190 [DOI] [PubMed] [Google Scholar]
- 28.Davis MM, Currey JM, Howk S, et al. A qualitative study of rural primary care clinician views on remote monitoring technologies. J Rural Health 2014;30:69–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.