Abstract
Introduction: Cognitive behavioral therapy (CBT) for child anxiety, although efficacious, typically requires 16–20 weekly sessions with a therapist. Brief CBT (BCBT; eight sessions) for child anxiety is promising but may have less favorable outcomes owing to reduced session time. Mobile health (m-health) has the potential to improve BCBT efficacy by delivering ecological momentary intervention to engage youth in learning and practicing CBT skills in their everyday lives (in vivo). Materials and Methods: We developed an m-health platform entitled SmartCAT (Smartphone-enhanced Child Anxiety Treatment). SmartCAT consists of (1) a smartphone application (app) that cues youth to use the CBT skills taught in sessions, (2) an online portal that allows therapists to monitor skill use, to send cues and treatment-related materials, to engage youth in real-time via secure messages, and to manage rewards, and (3) a communication protocol that allows real-time bidirectional exchange between the app and the portal. A pilot study with nine youth (9–14 years old) examined the platform's feasibility as an adjunct to BCBT. Results: SmartCAT was found to be capable of supporting BCBT for child anxiety and received positive feedback from both therapists and youth patients. Patients rated the app as highly usable (mean=1.7 on a 1–7 scale, with 1=“easy”). Patients completed 5.36 skills coach entries per session (standard deviation=1.95) and took an average of 3.14 min (standard deviation=0.98 min) to complete the entries. Conclusions: A smartphone app is feasible within CBT for child anxiety. Users found SmartCAT both acceptable and easy to use. Integrating an m-health platform within BCBT for anxious children may facilitate involvement in treatment and dissemination of effective procedures.
Key words: : e-health, telehealth, telepsychiatry
Introduction
Anxiety disorders are among the most common child mental health problems, affecting 10–20% of school-aged children.1–3 Three of these anxiety disorders—generalized anxiety disorder (GAD), social phobia (SP), and separation anxiety disorder (SAD)—are highly comorbid and prevalent in children.4 Untreated anxiety in youth can be chronic and impairing,5,6 contributing to social and academic problems and the development of depression and substance abuse.7–9
Cognitive behavioral therapy (CBT) has been recognized by the American Psychological Association Taskforce as an efficacious treatment for childhood anxiety,10 based on the results of multiple independent randomized clinical trials.11–17 CBT is considered the first-line choice by most children and families,18 but it requires 16–20 weekly sessions with a CBT therapist.19 Families may be unable to commit to a 4–5-month treatment because of schedule and transportation difficulties.20 Many community practitioners also consider the number of sessions to be impractical for managed care settings.21,22
Mobile health (m-health) technologies can deliver CBT interventions to patients during their everyday lives and in natural settings through ecological momentary interventions (EMIs).23 Smartphone-based EMIs can provide in vivo skills coaching to patients when it is most needed, not only during discrete times (e.g., office visits).23 Smartphones are small and convenient to carry, have become widely available,24 have widespread network coverage, and have extensive computing abilities that allow them to run m-health applications (apps). Because children need practitioners to help them understand complex concepts in CBT such as cognitive restructuring,25 providing standalone m-health apps without weekly sessions with a therapist can be less effective.
A briefer treatment program would likely be more feasible and affordable and would enable in-demand CBT therapists to make treatment more accessible. Recently, Kendall and Hedtke26,27 developed and evaluated a brief CBT (BCBT) (eight sessions) for anxiety disorders adapted from the 16-session “Coping Cat” program. When applied with 26 youth (6–13 years old) diagnosed with GAD, SAD, and/or SP, the results indicated that BCBT was feasible, acceptable, and beneficial to anxious youth.28 Although favorable (42% response rate), BCBT was less favorable than the 60% responses rate typically seen in seen in full-length CBT trials for child anxiety.17,28,29
Lower rates of BCBT response may be related to reduced CBT skill acquisition and utilization. Because patients have less time to learn and practice new skills in BCBT, they may not learn the skills as well or use them out of session as often. When parents of the youth in the evaluation of BCBT were asked to rate impediments to improvement, 60% endorsed “difficulty practicing what s/he learned in therapy” as a major impediment.28
A smartphone-based EMI offers several advantages for improving CBT treatment of child anxiety, such as (1) providing opportunities for repetition (i.e., reviewing CBT skills on a daily basis) to improve learning, (2) facilitating skills practice by reminding patients to complete home-based exposures and to apply CBT skills during real-world emotional situations, and (3) providing increased communication opportunities between therapists and patients.
The purpose of the present project was to design and develop an m-health platform and to evaluate its feasibility and utility with youth receiving CBT for their anxiety disorder.
Materials and Methods
Requirement Analysis
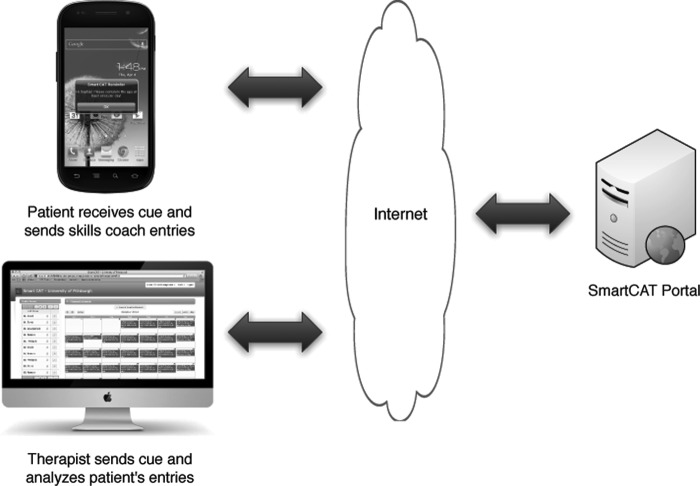
The objective was to develop an m-health platform called SmartCAT (Smartphone-enhanced Child Anxiety Treatment) to support clinician-directed CBT treatment by improving CBT skill acquisition and utilization, promoting in vivo skills coaching, and monitoring patients' skill utilization. As illustrated in Figure 1, the app cues patients to use skills learned in a CBT session during their daily activities. Instead of an isolated local app, the app can receive treatment cues from a Web-based portal and send monitoring data to the portal. Using the portal, therapists can monitor patients' adherence to treatment regimens and also view a graphical summary about patients' condition and app usage. The data are then available to be discussed in the weekly CBT session. Therapists can use the portal to manage reward points and/or to send audiovisual materials to patients. The platform allows patient and therapist to exchange messages securely without using text messaging (which poses potential threats to the security and confidentiality of sensitive health data). This seamless interaction represents advancement over existing health portals, which cannot push data in real-time to the app. The app was also designed to work with intermittent data connectivity typically found in mobile networks by switching between store-and-forward and real-time mode of connectivity to ensure data delivery.
Fig. 1.
Functional diagram of the SmartCAT (Smartphone-enhanced Child Anxiety Treatment) platform. LDAP, Lightweight Directory Access Protocol.
Platform Architecture
As illustrated in Figure 2, the architecture of SmartCAT consists of a smartphone app (SmartCAT App), a therapist portal (SmartCAT Portal), and a two-way communication connecting them. The app consists of a user interface that interacts with the patient and a background service that maintains real-time data connection with the portal when the smartphone is off. This architecture allows the smartphone to alert patients as new data were pushed from the portal (e.g., secure message sent by a therapist). The portal consists of a presentation layer, an app logic layer, and a persistence layer. The presentation layer provides a user interface that helps therapists completing tasks such as sending treatment regimens, monitoring treatment responses and rewards, and sending or replying to messages. The application logic layer provides services for data access and data synchronization connecting both the portal's presentation layer and the app's background service with the persistence layer. The persistence layer consists of relational database software that stores clinical data and Lightweight Directory Access Protocol software, which stores unique identifiers of the app and therapists' account information. The portal's security works closely with the directory service to provide a unified authentication mechanism for all users.
Fig. 2.
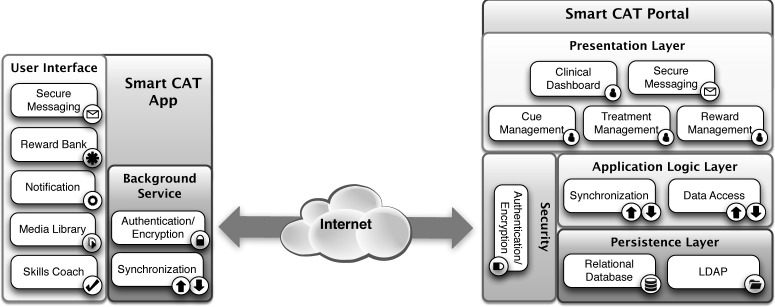
SmartCAT (Smartphone-enhanced Child Anxiety Treatment) architecture.
The most common m-health issue is privacy and data security.30 To address this, the platform incorporated the following integrated features:
• Seamless authentication and encryption. The app uses a unique identifier, a combination of cellphone and IMEI numbers to authenticate and establish a secure connection to the portal. Upon successful authentication, the data transmission is encrypted using the RSA algorithm with a 192-bit key. The key size is configurable up to 256 bits.
• Personal identification number feature on the app
• Password-protected online portal over secure socket layer. Therapists must provide login information before accessing the portal. The connection between the Web browser and the portal is also encrypted using RSA with a 192-bit key.
• Increased security by physically separating Web application and database via a three-tier architecture
The data synchronization process between the app and the portal is conducted through the Internet. The platform's synchronization module is responsible for managing bidirectional data exchange between the app and the portal in real-time. Because network connectivity is not guaranteed to be constantly available as patients move from one location to another, the app and the portal detect each other's connection information before exchanging data. In the case that the receiving end lacks an Internet connection, the sender will store data indefinitely and send them whenever the receiving end acquires a connection. This mechanism ensures successful data delivery even when the connection is not reliable.
Smartphone App
The smartphone app was designed to ensure patients' sufficient CBT skills practice outside the clinic by reminding them to practice, to motivate patients through rewards, to enable patients to receive personalized education materials from therapists, and to provide seamless patient–therapist interaction. The app has five main components: (1) notification, (2) skills coach, (3) reward bank, (4) media library, and (5) secure messaging.
Notification
Notification is the app's central component and offers two functions: (1) to prompt patients when certain tasks need to be done (e.g., completing skills coach entries) and (2) to provide livability features (e.g., the ability to suspend prompting for a short time when responding would be inconvenient).
Skills coach (EMI)
The heart of the app is the “skills coach,” which cues patients to complete a series of questions about recent emotional events and to use skills learned in therapy. The skills coach is scheduled by the therapist to launch automatically once per day (either at a fixed or random time) and can be completed more frequently if desired by the patient for “bonus points.” The skills coach can also be activated when patients experience acute anxiety. These are EMI features that promote the use of skills coach at “opportune” moments. The skills coach component walks the patient through a series of steps, summarized in Table 1. Patients are also asked whether or not a parent assisted in completing the entry and to describe the current social context (activity, companions, and location). To reduce patient burden, checklists are provided that include common responses to items (i.e., typical activities, locations, negative scenarios, automatic thoughts, coping thoughts). Each skills coach entry ends with a customized motivational message from the therapist (entered weekly via the portal) that includes encouragement as well as a reminder to complete any assigned home-based exposure or skills practice (i.e., “Great job, John! Remember to invite a friend to sleep over this week.”).
Table 1.
Skills Coach Steps
| SKILL | PATIENT IS ASKED TO |
|---|---|
| Emotion identification | 1. Label and rate current emotions |
| 2. Identify a recent scenario (since last entry) in which the patient felt “scared, worried, nervous, or upset” | |
| 3. Identify somatic symptoms and emotions experienced during the scenario | |
| Automatic thoughts | 4. Identify negative automatic thoughts associated with the chosen scenario |
| Coping thoughts | 5. List coping thoughts used during the scenario |
| 6. List coping thoughts not used during the scenario that might be helpful in the future | |
| Problem-solving | 7. List any problem-solving steps used during the scenario |
| Overcoming avoidance | 8. Indicate whether or not a feared situation was avoided |
| Self-assessment and reward | 9. Indicate any rewards earned |
| 10. Rate self-efficacy at coping with the scenario |
Reward bank
Patients earn prizes for completing skills coach entries. They select from a collection of prizes of different values, such as small toys or games, accessories, or stickers, each of which can be earned with a specific number of points. Each time a patient completes an entry, the reward bank opens to show how many points he or she has earned and how many more are needed to obtain the selected reward. The reward bank is reset each time points are “cashed in” for a prize.
Media library
The media library includes documents, photographs, video, and audio files provided by the therapist to help the patient remember and practice skills learned in treatment or supplemental skills (i.e., “coping cards” completed during the session, video messages from the therapist, relaxation audio scripts).
Secure messaging
A secure messaging system is used to support therapist–patient interaction. The patient composes a message on the phone that is sent to the portal rather than the therapist's private phone. This protects the therapist's personal space and also allows communication between therapists and patients to be recorded. When the portal receives a message, the therapist will be notified via e-mail. The therapist may view these messages and/or send the patient a message at any time using the portal.
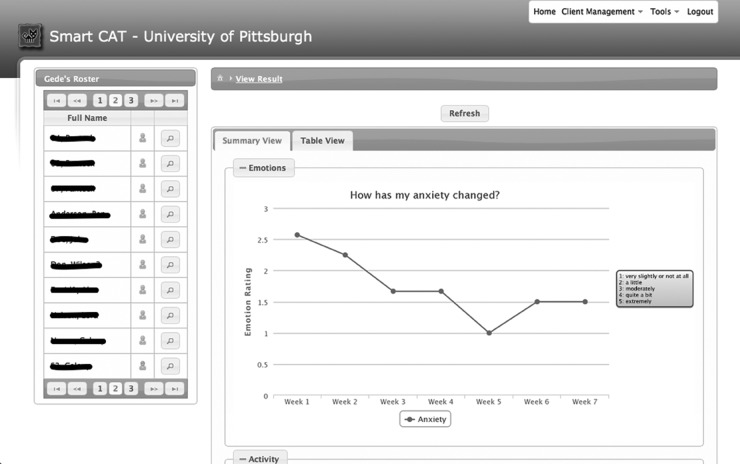
Therapist Portal
The therapist portal is a secure Web site that can be accessed from a computer, tablet, or smartphone. Therapists can use the portal to receive or send messages, documents, and audio/video files, to manage skills coach cues, to manage rewards, and to view data from skills coach entries. The therapist may view each entry in a table format or may view summary graphs that visualize information obtained from patients' entries. Graphs of summary information (average ratings for anxiety and self-efficacy, rates of use of specific coping thoughts, anxiety in different social contexts) are grouped by session. Graphs are also available showing session-by-session change in these variables. The therapist selects graphs and/or entries to review with the patient at the beginning of each session.
Initial Evaluation
We conducted a two-phase evaluation. The first phase was platform testing and evaluation, which was performed for 1 month in a lab environment involving CBT therapists and a software engineer. In this phase, therapists tested the platform and offered feedback to improve usability. After this feedback was implemented, the second phase incorporated SmartCAT into CBT with anxious youth. Informed consent was obtained, and youth were given a smartphone with an unlimited data plan throughout the study. A protocol for feasibility study was reviewed and approved by the Institutional Review Board of the University of Pittsburgh, Pittsburgh, PA.
In the second phase, a feasibility study with nine anxious youth (9–14 years old; mean=11.33) with a Diagnostic and Statistical Manual of Mental Disorders-IV31 diagnosis of GAD, SP, specific phobia, attention deficit hyperactivity disorder, oppositional defiant disorder, and/or SAD was conducted. Three patients were given 16-session CBT; the other 6 patients were given eight-session BCBT. Patients were assessed by a trained independent evaluator using the Schedule for Affective Disorders and Schizophrenia for School-Aged Children—Present and Lifetime Version32 to establish diagnoses. Sixteen-session treatment was delivered using the “Coping Cat” therapist manual and workbook.26,27 Eight-session BCBT was delivered using a new “Brief Coping Cat” manual and workbook.33,34 Both programs, like other CBT interventions for anxious youth, include two key components: (1) skills training, including emotion identification and labeling, cognitive reframing, and problem-solving skills, and (2) graded exposure to feared stimuli. Therapists meet with parents for two 1-h sessions in the 16-session treatment and two 30-min sessions in the eight-session treatment. Treatment was delivered by Masters-level therapists trained in CBT for child anxiety.
Each patient received the smartphone after completing the first session. As is typical in CBT, all participated in a weekly face-to-face session with a therapist. Between sessions, the therapist used the portal to create daily skills coach reminders for each patient. When reminded by the app, patients responded by completing the skills coach entries. Participants could also complete the entries at other times when they were feeling anxious. The time that patients took to complete the entries was recorded by the app and then sent to the portal. The therapist would discuss the data with the patients during the weekly sessions.
Feasibility was evaluated based on (1) compliance with the skills coach cues and (2) overall satisfaction with the treatment. Compliance was measured by analyzing the number of skills coach entries that was sent to the portal (five or more entries per session).
At the end of the treatment, patients' and parents' comments were collected using a Summary Therapist Feedback Form to assess overall satisfaction with the treatment. Other measures, such as the Therapeutic Alliance Scales for Children—Revised,35 the Client Evaluation of Services Questionnaire, and the Computer System Usability Questionnaire, were used to assess app and portal usability. The average time that patients took to complete skills coach entries was also calculated.
Results
SmartCAT App
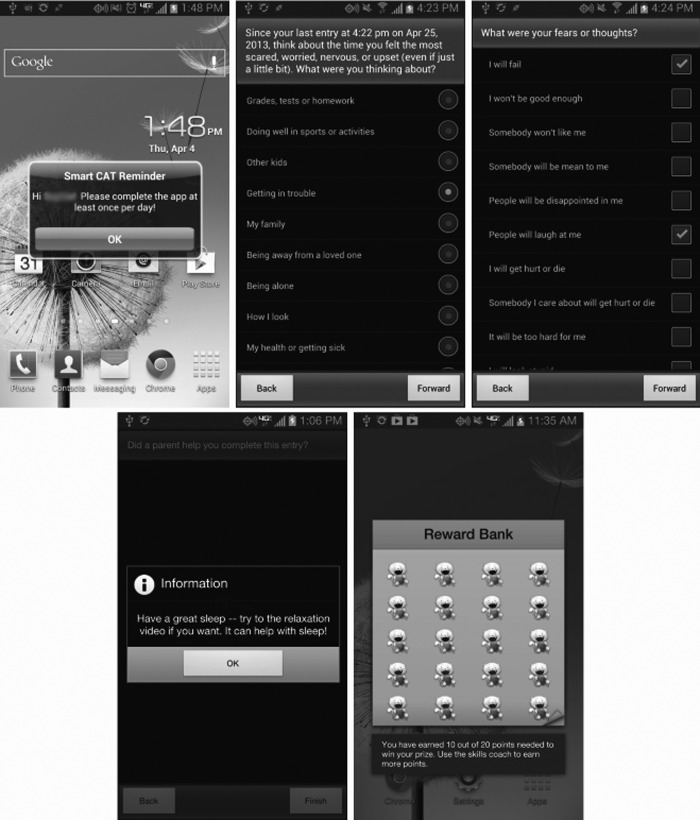
The app was developed using Android® (Google, Mountainview, CA) Software Development Kit (SDK). To accommodate the wide range of Android devices available, the app was built using SDK version 2.3, which is available on less expensive Android devices and can run on later versions of Android. The app is illustrated in Figure 3.
Fig. 3.
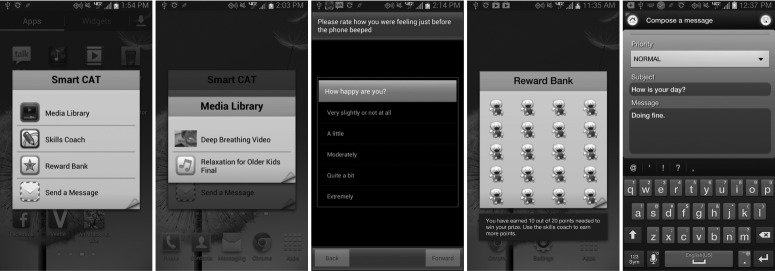
SmartCAT (Smartphone-enhanced Child Anxiety Treatment) application.
To notify patients to use skills while engaging in daily activities, the SmartCAT app automatically wakes the device, shows a notification dialog, and then plays a distinct sound to get the patient's attention. The patient has the option to suspend the notification for 15 min by pressing the device's power button if the time is inconvenient. As shown in Figure 4, the notification is implemented as a small dialog with a title, message, and action button. The therapist can customize the message for each patient. When the action button is pressed, the app asks the patient to complete the entries. At the end, a customized motivational message and the reward bank are displayed consecutively to motivate the patient. Similar notifications with different message content are also displayed when education materials or secure messages are pushed from the portal.
Fig. 4.
SmartCAT (Smartphone-enhanced Child Anxiety Treatment) notification to complete the skills coach entries.
SmartCAT Portal
The SmartCAT portal allows therapists to access patients' data and to send information to patients' apps, including personalized skills coach plans, education materials, and secure messages. The portal is illustrated in Figure 5. After successful login, therapists can see a list of their patients. The list provides information about each patient's smartphone connectivity, with a green mark indicating that a patient's phone is currently connected and a gray mark indicating no connection. An action button, next to the connectivity status, is used to initiate patient-related actions such as viewing skills coach entries, sending audio/video materials, managing skills coach plans, and managing reward points. The utility bar is used for administrative tasks, such as smartphone registration, uploading audio/video files, and authentication management.
Fig. 5.
The SmartCAT (Smartphone-enhanced Child Anxiety Treatment) portal displaying the patient's emotions.
To ensure that patients use CBT skills in real-world experiences, the therapist develops a skills coach plan for each patient that is pushed to the patient's app. As shown in Figure 6, a skill coach plan represents a calendar consisting of a series of daily skills coach events. The event has four parts: (1) opening notes—an instructional message that will be shown on the message part of the app's notification dialog; (2) time—the specific time of the day that a notification should pop up; (3) protocol—each protocol is associated with a different set of skills coach entries; and (4) closing notes—a customized motivational message that will be shown upon skills coach entry completion. After successful transmission, the app automatically schedules reminders according to the plan to notify the patient to complete the skill coach entries.
Fig. 6.
The SmartCAT (Smartphone-enhanced Child Anxiety Treatment) portal's features: Skills coach plan.
SmartCAT Communication Protocol
The SmartCAT communication protocol was built on top of the Extensible Messaging and Presence Protocol (XMPP) standard. The protocol allows two or more network entities connected through the Internet to exchange data bidirectionally and asynchronously in near real-time.36 The XMPP protocol was originally designed to work reliably on a wired communication link. On wireless, where the network connectivity is not reliable, a mechanism needs to be implemented on the app's background service to proactively acquire network quality information such as signal strength. When signal strength is considered poor but still usable, the app will notify the portal to close the connection, allowing both entities to temporarily suspend network operations. During this state, activities involving network connectivity will be queued locally by the participating entities. When signal strength improves, the app resumes the connection, and all pending activities in the queue will be executed. This extension can potentially increase data transmission reliability on unreliable wireless networks.
Initial Development Study and Initial Feasibility and Acceptability Study
The initial development study identified a few usability issues related to the app and the portal. For the app, one issue was the need for an option to suspend the notification for a specific amount of time when the time to complete skills coach entries was not appropriate. Another issue was the need to include two additional questions in the skills coach entries. For the portal, the only issue was the need for an activity logger that records certain app activities such as when the app's notification dialog appears, how often the notification is suspended, and the smartphone's status (e.g., powered on/off, battery level). These issues were addressed before the initial feasibility and acceptability study was initiated.
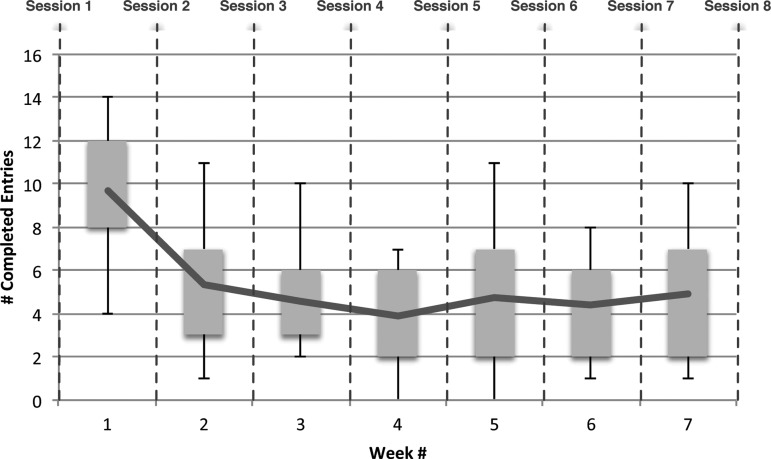
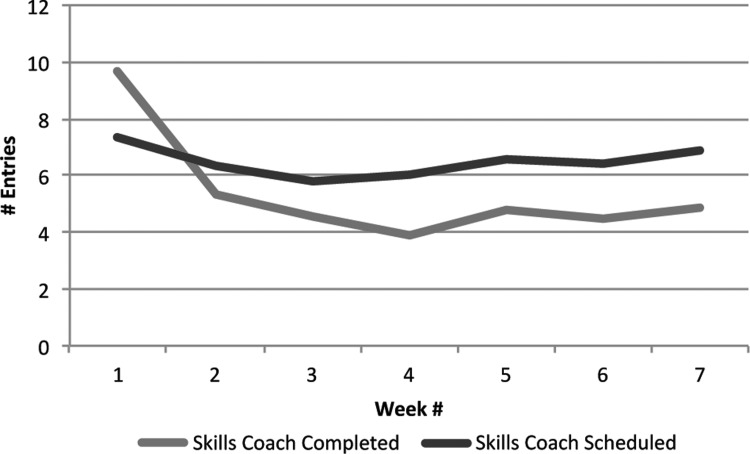
The data from patient use revealed that the app was used frequently during treatment. As illustrated in Figure 7, the app was used more frequently during the first week, and usage leveled off toward the end. The high usage frequency during the first week might reflect the fact that patients were becoming familiar with the app by self-initiating the skills coach entries several times.
Fig. 7.
Smartphone-enhanced Child Anxiety Treatment application usage frequency. Usage data were collected after Session 1 and calculated at the end of Session 8.
Compliance with treatment protocol was measured by the number of skills coach entries completed throughout the treatment. Figure 8 suggests that patients were compliant with the protocol, completing an average of 5.36 entries out of 6.48 requests (82.8% completion rate) between each session (standard deviation=1.95).
Fig. 8.
Treatment compliance.
On a 1–7 scale, with 1 indicating “easy” to use, patients rated the app as highly usable (mean=1.7). They took an average of 3.44 min (standard deviation=0.98 min) to complete the skills coach entries. All parents indicated that they were satisfied with the treatment and would recommend the program to others.
Discussion
The results suggest that a SmartCAT app can be successfully integrated into CBT for children with anxiety disorders. Patients were actively using the app, averaging 5.36 entries per session, and were in compliance with treatment protocol. The inclusion of goal setting through rewards can potentially increase patients' participation in treatment through skill coaching practice. The therapists could also monitor and assess patients' skills coaching practice through an advanced health portal.
Although most EMI interventions have focused on physical health behaviors (e.g., smoking, weight management, and diabetes), EMIs have also been used in a few CBT studies.37–39 In these studies, palmtop computers were used to supplement BCBT interventions by prompting participants to practice CBT skills. The results indicated similar reductions in anxiety symptoms for BCBT+EMI compared with standard CBT after treatment.37–39
The pilot study results show positive feedback from patients and therapists about the feasibility and effectiveness of m-health using an advanced communication protocol for supporting in vivo skills coaching and treatment monitoring of children with anxiety. The integration of m-health with CBT appears to be a promising avenue to provide effective treatments in a shorter period of time, potentially improving dissemination, faster amelioration of symptoms, and healthcare affordability.
Limitations
The pilot study was an initial development study with a small sample to assess the feasibility, utility, and acceptability of the SmartCAT platform. Although we observed positive results from patients and therapists, the conclusion is preliminary.
Strengths
The majority of existing EMIs have utilized stand-alone programs installed on palmtop computers or voice or text-messaging capabilities on mobile phones.23 The SmartCAT platform offers better integration, compelling user interface, and visualization of information collected in real-time, as well as secure two-way communication between the patient and therapist. To our knowledge, we are not aware of any m-health platforms for EMI to enhance treatment for anxious youth.
Despite the increasing adoption rates of mobile technology in children and adolescents,24 research on harnessing smartphone apps for delivering health interventions in this group is still lacking.40 The SmartCAT platform will be a significant contribution to current research literature on m-health for children and adolescents.
Acknowledgments
This project was funded in part by grant 1R21HD071810-01A1 from the National Institutes of Health and by the RERC on Telerehabilitation of the National Institute on Disability and Rehabilitation Research (projects H133E040012 and H133E980025). The authors thank Marcie L. Walker and Han-Tsung (Marcus) Min from the Western Psychiatric Institute and Clinic of the University of Pittsburgh Medical Center for their help with project and data management.
Disclosure Statement
No competing financial interests exist.
References
- 1.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry 2003;60:837–844 [DOI] [PubMed] [Google Scholar]
- 2.Gurley D, Cohen P, Pine DS, Brook J. Discriminating depression and anxiety in youth: A role for diagnostic criteria. J Affect Disord 1996;39:191–200 [DOI] [PubMed] [Google Scholar]
- 3.Shaffer D, Fisher P, Dulcan MK, et al. . The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): Description, acceptability, prevalence rates, and performance in the MECA Study. Methods for the Epidemiology of Child and Adolescent Mental Disorders Study. J Am Acad Child Adolesc Psychiatry 1996;35:865–877 [DOI] [PubMed] [Google Scholar]
- 4.Kendall PC, Compton SN, Walkup JT, et al. . Clinical characteristics of anxiety disordered youth. J Anxiety Disord 2010;24:360–365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Costello EJ, Angold A. Epidemiology. In: March JS, ed. Anxiety disorders in children and adolescents. New York: Guilford Press, 1995:109–124 [Google Scholar]
- 6.Ferdinand RF, Verhulst FC. Psychopathology from adolescence into young adulthood: An 8-year follow-up study. Am J Psychiatry 1995;152:1586–1594 [DOI] [PubMed] [Google Scholar]
- 7.Pine DS, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch Gen Psychiatry 1998;55:56–64 [DOI] [PubMed] [Google Scholar]
- 8.Strauss CC, Frame CL, Forehand R. Psychosocial impairment associated with anxiety in children. J Clin Child Psychol 1987;16:235–239 [Google Scholar]
- 9.Woodward LJ, Fergusson DM. Life course outcomes of young people with anxiety disorders in adolescence. J Am Acad Child Adolesc Psychiatry 2001;40:1086–1093 [DOI] [PubMed] [Google Scholar]
- 10.Hollon SD, Beck AT.Cognitive and cognitive behavior therapies. In: Lambert MJ, ed. Bergin & Garfield's handbook of psychotherapy and behavior change, 6th ed. New York: Wiley, 2013:393–442 [Google Scholar]
- 11.Barrett PM, Dadds MR, Rapee RM. Family treatment of childhood anxiety: A controlled trial. J Consult Clin Psychol 1996;64:333–342 [DOI] [PubMed] [Google Scholar]
- 12.Barrett PM. Evaluation of cognitive-behavioral group treatments for childhood anxiety disorders. J Clin Child Psychol 1998;27:459–468 [DOI] [PubMed] [Google Scholar]
- 13.Beidel DC, Turner SM, Morris TL. Behavioral treatment of childhood social phobia. J Consult Clin Psychol 2000;68:1072–1080 [PubMed] [Google Scholar]
- 14.Kendall PC, Flannery-Schroeder E, Panichelli-Mindel SM, Southam-Gerow M, Henin A, Warman M. Therapy for youths with anxiety disorders: A second randomized clinical trial. J Consult Clin Psychol 1997;65:366–380 [DOI] [PubMed] [Google Scholar]
- 15.Kendall PC, Hudson JL, Gosch E, Flannery-Schroeder E, Suveg C. Cognitive-behavioral therapy for anxiety disordered youth: A randomized clinical trial evaluating child and family modalities. J Consult Clin Psychol 2008;76:282–297 [DOI] [PubMed] [Google Scholar]
- 16.Silverman WK, Kurtines WM, Ginsburg GS, Weems CF, Lumpkin PW, Carmichael DH. Treating anxiety disorders in children with group cognitive-behaviorial therapy: A randomized clinical trial. J Consult Clin Psychol 1999;67:995–1003 [DOI] [PubMed] [Google Scholar]
- 17.Walkup JT, Albano AM, Piacentini J, et al. . Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. N Engl J Med 2008;359:2753–2766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Asarnow JR, Jaycox LH, Duan N, et al. . Effectiveness of a quality improvement intervention for adolescent depression in primary care clinics: A randomized controlled trial. JAMA 2005;293:311–319 [DOI] [PubMed] [Google Scholar]
- 19.James A, Soler A, Weatherall R. Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database Syst Rev 2005;(4):CD004690. [DOI] [PubMed] [Google Scholar]
- 20.Collins KA, Westra HA, Dozois DJA, Burns DD. Gaps in accessing treatment for anxiety and depression: Challenges for the delivery of care. Clin Psychol Rev 2004;24:583–616 [DOI] [PubMed] [Google Scholar]
- 21.Nelson TD, Steele RG, Mize JA. Practitioner attitudes toward evidence-based practice: Themes and challenges. Adm Policy Ment Health 2006;33:398–409 [DOI] [PubMed] [Google Scholar]
- 22.Addis ME. Methods for disseminating research products and increasing evidence-based practice: Promises, obstacles, and future directions. Clin Psychol 2006;9:367–378 [Google Scholar]
- 23.Heron KE, Smyth JM. Ecological momentary interventions: Incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol 2010;15:1–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Madden M, Lenhart A, Duggan M, Cortesi S, Gasser U. Teens and technology 2013. 2013 [Google Scholar]
- 25.Khanna MS, Kendall PC. Exploring the role of parent training in the treatment of childhood anxiety. J Consult Clin Psychol 2009;77:981–986 [DOI] [PubMed] [Google Scholar]
- 26.Kendall PC, Hedtke KA. Cognitive-behavioral therapy for anxious children: Therapist manual, 3rd ed. Ardmore, PA: Workbook Publishing, 2006 [Google Scholar]
- 27.Kendall PC, Hedtke KA. Coping Cat workbook, 2nd ed. Ardmore, PA: Workbook Publishing, 2006 [Google Scholar]
- 28.Crawley SA, Kendall PC, Benjamin CL, et al. . Brief cognitive-behavioral therapy for anxious youth: Feasibility and initial outcomes. Cogn Behav Pract 2013;20:123–133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reynolds S, Wilson C, Austin J, Hooper L. Effects of psychotherapy for anxiety in children and adolescents: A meta-analytic review. Clin Psychol Rev 2012;32:251–262 [DOI] [PubMed] [Google Scholar]
- 30.Whittaker R. Issues in mhealth: Findings from key informant interviews. J Med Internet Res 2012;14:e129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.American Psychiatric Association Diagnostic and statistical manual of mental disorders: DSM-IV, 4th ed. Washington, DC: American Psychiatric Association, 1994 [Google Scholar]
- 32.Kaufman J, Birmaher B, Brent D, et al. . Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 1997;36:980–988 [DOI] [PubMed] [Google Scholar]
- 33.Kendall PC, Beidas RS, Mauro CF. Brief Coping Cat: The 8-session Coping Cat workbook. Ardmore, PA: Workbook Publishing, 2012 [Google Scholar]
- 34.Kendall PC, Crawley SA, Benjamin CL, Mauro CF. Brief Coping Cat: The 8-session therapist manual. Ardmore, PA: Workbook Publishing, 2012 [Google Scholar]
- 35.Shirk SR, Gudmundsen G, Kaplinski HC, McMakin DL. Alliance and outcome in cognitive-behavioral therapy for adolescent depression. J Clin Child Adolesc Psychol 2008;37:631–639 [DOI] [PubMed] [Google Scholar]
- 36.Saint-Andre P. XMPP: Lessons learned from ten years of XML messaging. IEEE Commun Mag 2009;47:92–96 [Google Scholar]
- 37.Gruber K, Moran PJ, Roth WT, Taylor CB. Computer-assisted cognitive behavioral group therapy for social phobia. Behav Ther 2001;32:155–165 [Google Scholar]
- 38.Newman MG, Kenardy J, Herman S, Taylor CB. Comparison of palmtop-computer-assisted brief cognitive-behavioral treatment to cognitive-behavioral treatment for panic disorder. J Consult Clin Psychol 1997;65:178–183 [DOI] [PubMed] [Google Scholar]
- 39.Kenardy JA, Dow MGT, Johnston DW, Newman MG, Thomson A, Taylor CB. A comparison of delivery methods of cognitive-behavioral therapy for panic disorder: An international multicenter trial. J Consulti Clin Psychol 2003;71:1068–1075 [DOI] [PubMed] [Google Scholar]
- 40.Dennison L, Morrison L, Conway G, Yardley L. Opportunities and challenges for smartphone applications in supporting health behavior change: Qualitative study. J Med Internet Res 2013;15:e86. [DOI] [PMC free article] [PubMed] [Google Scholar]