Abstract
The insulin receptor substrate proteins IRS1 and IRS2 are key targets of the insulin receptor tyrosine kinase and are required for hormonal control of metabolism. Tissues from insulin-resistant and diabetic humans exhibit defects in IRS-dependent signalling, implicating their dysregulation in the initiation and progression of metabolic disease. However, IRS1 and IRS2 are regulated through a complex mechanism involving phosphorylation of >50 serine/threonine residues (S/T) within their long, unstructured tail regions. In cultured cells, insulin-stimulated kinases (including atypical PKC, AKT, SIK2, mTOR, S6K1, ERK1/2 and ROCK1) mediate feedback (autologous) S/T phosphorylation of IRS, with both positive and negative effects on insulin sensitivity. Additionally, insulin-independent (heterologous) kinases can phosphorylate IRS1/2 under basal conditions (AMPK, GSK3) or in response to sympathetic activation and lipid/inflammatory mediators, which are present at elevated levels in metabolic disease (GRK2, novel and conventional PKCs, JNK, IKKβ, mPLK). An emerging view is that the positive/negative regulation of IRS by autologous pathways is subverted/co-opted in disease by increased basal and other temporally inappropriate S/T phosphorylation. Compensatory hyperinsulinaemia may contribute strongly to this dysregulation. Here, we examine the links between altered patterns of IRS S/T phosphorylation and the emergence of insulin resistance and diabetes.
Keywords: Degradation, Dyslipidaemia, Hyperinsulinaemia, Insulin receptor substrate, Insulin resistance, Metabolic syndrome, Mammalian target of rapamycin complex 1, Review, Serine phosphorylation, Sympathetic activity
Introduction
Insulin resistance, defined as reduced responsiveness of tissues to normal insulin concentrations, is a principal feature of type 2 diabetes, which leads to compensatory hyperinsulinaemia [1]. It also underlies risk factors—including hyperglycaemia, dyslipidaemia and hypertension—for the clustering of type 2 diabetes with cardiovascular disease, non-alcoholic fatty liver disease and related maladies (metabolic syndrome) [2]. Although numerous genetic and physiological factors interact to produce and aggravate insulin resistance, human studies implicate dysregulated signalling by the insulin receptor substrate proteins IRS1 and IRS2 (hereafter referred to as ‘IRS’) as a common underlying mechanism [3, 4]. Cell-based studies demonstrate the impairment of insulin signalling by phosphor-ylation of IRS on serine and threonine residues (S/T), which might contribute to insulin resistance in metabolic disease. Here, we review the links between IRS S/T phosphorylation and the emergence of insulin resistance, as well as its exacerbation by dyslipidaemia and inflammation in diabetes/obesity. In contrast to prior reviews [5, 6], we emphasise the role of insulin-regulated IRS S/T phosphorylation. We also consider newer studies on transgenic and knock-in mice engineered to have altered IRS1 S/T phosphorylation.
Overview of IRS-dependent signalling pathways
The binding of insulin to the insulin receptor (IR), and in muscle tissues to hybrid insulin/IGF1 receptors (IR/IGF1R) [7], promotes the autophosphorylation of a trio of regulatory loop tyrosine residues, disinhibiting IR tyrosine kinase activity toward IRS [8]. Although IR phosphorylates numerous other proteins [9], work with knockout mice has revealed that many insulin responses, including the regulation of carbohydrate and lipid metabolism, require IRS1 and IRS2 [10]. Co-disruption of the mouse Irs1 and Irs2 genes largely phenocopies the deletions of Insr (which encodes IR) or Insr plus Igf1r genes in liver or muscle, respectively [11–15]. The co-deletion of Irs1 and Irs2 from adipose tissue has not been reported, but mice lacking Insr expression in adipose tissue, or Irs1 and Irs2 expression in all tissues, exhibit abnormal or severely compromised adipocyte differentiation [16, 17]. Thus, the contribution of IRS-independent pathways to insulin control of metabolism is minimal in comparison with signalling mediated by IRS.
Tyrosine phosphorylation of IRS by IR generates binding sites for Src homology 2 (SH2) domain proteins, including the regulatory subunits of class 1A phosphatidylinositol 3-kinase (PI3K), the RAS guanine nucleotide exchange factor complex known as growth factor receptor-bound protein 2/son of sevenless (GRB2/SOS), and SH2 domain-containing protein tyrosine phosphatase-2 (SHP2) (Fig. 1a) [18]. The binding of other SH2 proteins to IRS has been reported but is less well investigated. Recruitment of dimeric PI3K (p85•p110) to IRS produces membrane phosphatidylinositol 3,4,5-trisphosphate (PIP3), which recruits the S/T kinase AKT [19]. In turn, 3-phosphoinositide-dependent kinase (PDK1) activates AKT and related kinases via the phosphorylation of activation loop residues, including T308 of AKT and analogous sites within the calcium- and diacylglycerol-independent atypical protein kinase C isoforms (aPKCs) λ/ι and ζ [20].
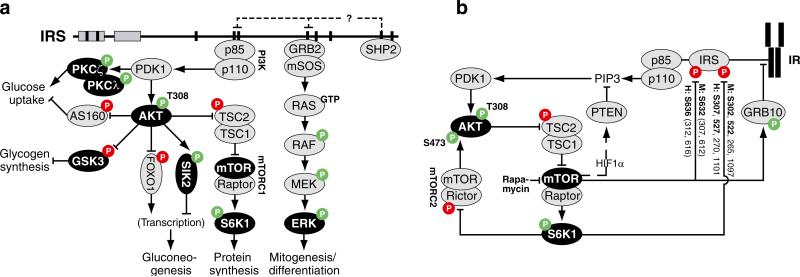
Fig. 1.
Insulin signalling and feedback pathways initiated by IRS (a) Tyrosine phosphorylation of IRS by IR kinase enables binding of SH2 domain proteins p85, GRB2, SHP2 and others (not shown). Metabolic signalling is accomplished largely by the recruitment of dimeric (p85•p110) PI3K to IRS, which stimulates (via PDK1) the activation of aPKCs (λ/ι, ζ) and AKT/PKB. In the absence of inhibitory phosphorylation by AKT, key regulatory proteins: (1) limit GLUT4-dependent glucose uptake (Akt substrate of 160 kDa; AS160); (2) inhibit the storage of glucose as glycogen (GSK3); (3) promote hepatic gluconeogenic gene transcription (forkhead box O1; FOXO1); and (4) block the stimulation of protein synthesis via mTORC1→S6K1 signalling (TSC2) [173]. IRS-mediated activation of the RAS→ERK kinase cascade is less important for metabolic control. Tyrosine phosphatase SHP2 negatively regulates insulin sensitivity, potentially in part by direct action on IRS phosphotyrosines. Multiple insulin-regulated S/T kinases (black ovals) can directly phosphorylate IRS, mediating positive and/or negative feedback regulation of insulin signalling (for more details, see Fig. 3). Arrows indicate stimulation/ activation, blocked lines indicate inhibition; green ‘P’, activating S/T phosphorylation; red ‘P’, inhibitory S/T phosphorylation. (b) Positive and negative regulation of AKT by tyrosine and feedback S/T phosphorylation of IRS. AKT is activated via PI3K/PDK1-dependent phosphorylation on T308 (lost in tissues lacking IRS), primed by phosphorylation on S473 by mTORC2 [21]. Excessive activation of mTORC1→S6K1 signalling by deletion of TSC1/2—or overexpression of their target, RHEB (not shown)—downregulates AKT activation, in part via mTOR- and S6K1-mediated S/T phosphorylation of IRS. Equivalent S/Ts on mouse (M:) and human (H:) IRS1 that are directly phosphorylated by mTOR and S6K1 in vitro are in bold type; those in parentheses are likely targets of mTOR. Related pathways that contribute to the regulation of AKT include: (1) mTORC1 phosphor-ylation/ stabilisation of GRB10 [174], which inhibits productive interaction of IRS with a key phosphotyrosine in IR [175]; (2) inhibition of mTORC2 by S6K1-mediated phosphorylation of rictor [176]; and (3) transcriptional upregulation, via hypoxia inducible factor 1α (HIF1α), of the phosphatidylinositol phosphatase known as phosphatase and tensin homologue (PTEN) [177]. The mTORC1, but not mTORC2, kinase complex is acutely sensitive to the inhibitor rapamycin
AKT T308 phosphorylation is undetectable in mouse tissues lacking IRS [11, 14]. In contrast, ‘priming’ phosphorylation of AKT at S473—by mammalian target of rapamycin (mTOR) complex 2 (mTORC2) [21] (Fig. 1b)—is retained, making this phosphorylation a poor indicator of IRS→PI3K signalling. AKT orchestrates the transition to the fed state in multiple tissues via inhibitory phosphorylation of key regulatory proteins (Fig. 1a) [8]; Akt2, but not Akt1, gene deletion in mice causes a diabetes-like phenotype [22]. Though AKT signalling is pleiotropic, combined defects in AKT- and aPKC-promoted muscle glucose uptake might be key in the initiation of metabolic disease [23]. Indeed, the loss of even one copy of the gene encoding PKCλ/ι in mouse muscle gives rise to a complete metabolic syndrome-like phenotype, including insulin resistance, hyperinsulinaemia, hepatosteatosis and dyslipidaemia [24].
Compared with PI3K, the effects of GRB2/SOS or SHP2 binding to IRS are less well understood. Insulin stimulation of the RAS→mitogen-activated protein kinase (MAPK) cascade depends partly on other substrates of the IR, such as SHC, yet activation of the MAPKs extracellular signal-regulated kinase-1 and -2 (ERK1/2) is impaired in IRS-deficient mouse liver [11]. Direct interaction of the tyrosine phosphatase SHP2 with IRS is difficult to observe in tissues, but liver-specific deletion of the mouse SHP2-encoding gene (Ptpn11) gives rise to increased IRS tyrosine phosphorylation, PI3K binding, and improved sensitivity to injected insulin [25]. However, Ptpn11 knockout liver also shows dramatically reduced hepatic ERK1/2 activation by insulin. Collectively, these data provide evidence that (1) IRS-dependent activation of PI3K is critical for insulin regulation of metabolism; (2) this may be negatively regulated by SHP2 in some tissues; and (3) IRS-dependent MAPK activation is less critical for metabolic control.
Structure/function of IRS: relationship to S/T phosphorylation
In contrast to tyrosine phosphorylation, the multi-site S/T phosphorylation of IRS both positively and negatively regulates insulin signalling. A number of different mechanisms appear to be involved, affecting tyrosine dephosphorylation of IRS, their dissociation from IR, intracellular localisation and eventual degradation. Though complicated by a large number of phosphorylated S/T, these are increasingly understandable in terms of structural/regional features within the IRS proteins. In the discussion below, we use the amino acid numbering of the mouse IRS proteins, except when discussing primary human data, in which case the corresponding mouse S/T (mS/T) follows in parentheses. In some instances, both the mouse and human S/T (hS/T) are provided for clarity. Figure 3 shows the cognate mouse and human S/T for most sites discussed.
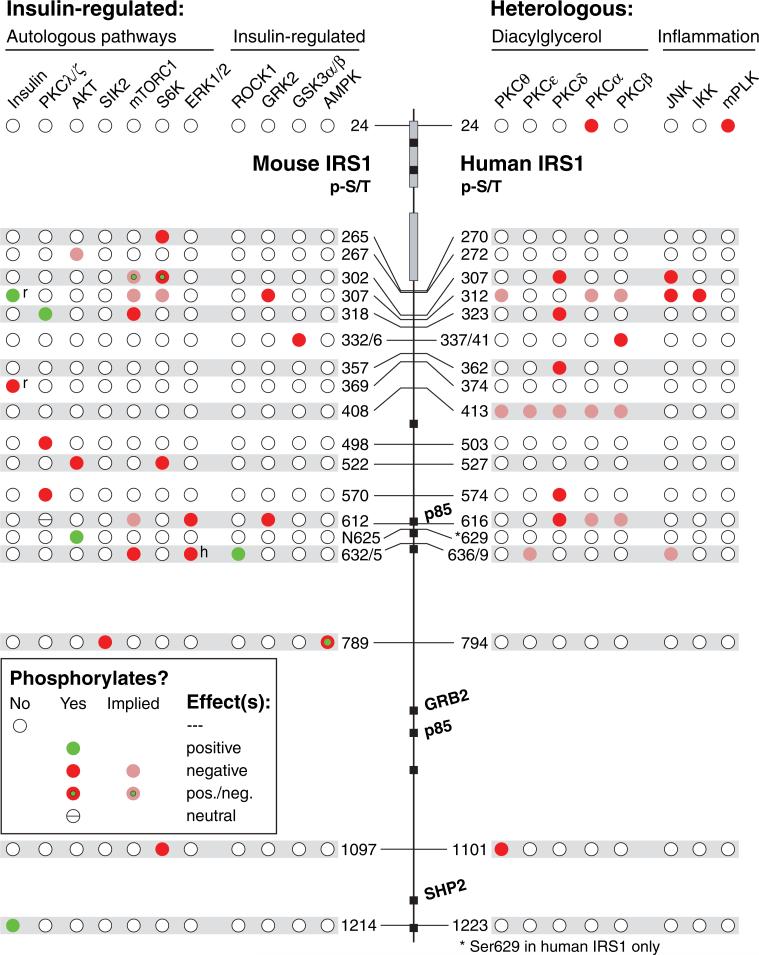
Fig. 3.
Functional effects of IRS1 S/T phosphorylation by insulin-regulated and heterologous kinase pathways. Shown are S/T sites and their known/implicated kinase(s) uniquely investigated by mutation in cells or mice, in vitro kinase assay, or discriminatory kinase-activating agents. Positive effects on insulin signalling (green-filled circles)— including temporally separable positive/negative effects (green centre)—are unique to S/T phosphorylation via insulin-regulated kinases.
In contrast, only negative effects on insulin signalling (red-filled circles) are observed by phosphorylation of IRS1 by heterologous (non-insulin) signalling pathways. In some studies, negative effects of multiple S/T kinases are implied or cannot be ruled out (light red-filled circles): The letters next to a circle indicate that the function is inferred from a rodent (r) or human (h) study. S332/6 and S632/5 phosphorylations are assayed by commercial antibodies to paired phosphorylation sites
IRS1 and IRS2 are large proteins (>1,200 amino acid residues [a.a.]) that contain highly similar amino-terminal pleckstrin homology (PH) and phosphotyrosine-binding (PTB) domains (~100 a.a. each), followed by long, unstructured carboxyl-terminal tail regions (Fig. 2a). The PH domain is the principal module that links IRS1 with the activated IR [26], whereas the PTB domain enhances this interaction via binding to the phospho-NPEY motif within the IR juxtamembrane region [27]. IRS2 alone contains the kinase regulatory loop binding (KRLB) domain, which interacts directly with the catalytic site of IR, but not IGF1R [28]. Unlike their amino termini, the tail regions of IRS1 and IRS2 are poorly conserved, except for the tyrosine residues that bind SH2 proteins (Fig. 2a). These ~1,000 a.a. tails are enriched in S/T residues, including many within canonical kinase phosphorylation motifs (~70 of 230 S/Ts within the IRS1 tail). The tails also include most of the phospho-S/T described to date; however, the IRS1 PH domain can be phosphorylated on S24, altering its membrane-binding properties in cultured cells [29] (Fig. 2b). Phosphorylation of S24 might be mediated in diabetes by the S/T kinase mouse Pelle-like kinase/interleukin-1 receptor-associated kinase (mPLK/IRAK) [30], or by canonical-type PKCα [29].
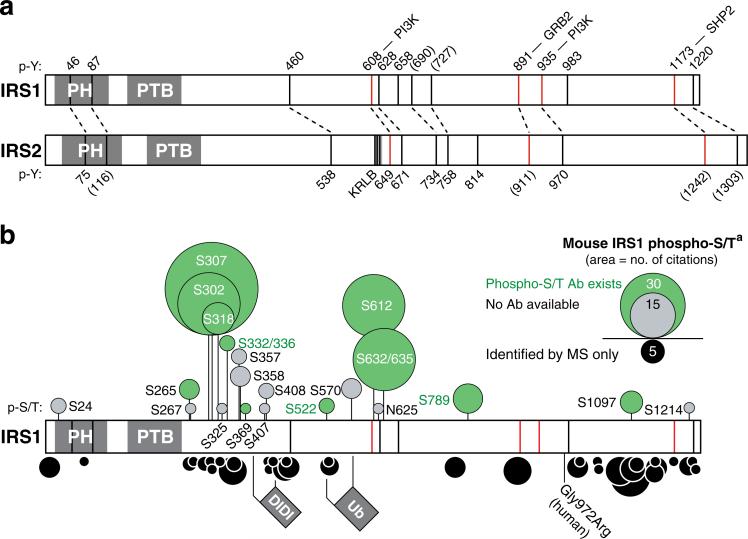
Fig. 2.
Structure/function of IRS and relationship to S/T phosphorylation. (a) The IRS1 and IRS2 proteins consist of similar amino-terminal PH and PTB domains (~100 amino acids each), followed by long C-terminal tail regions that are apparently unstructured. Shown are phosphorylated tyrosines (p-Y) within IRS1 and IRS2 (conserved tyrosines lacking evidence of phosphorylation are in parentheses). The tyrosines on IRS1 demonstrated by mutation or MS to recruit dimeric PI3K, GRB2 or SHP2 signalling proteins are indicated by the red bars [18, 178]. IRS2 uniquely contains the kinase regulatory loop binding (KRLB) ‘domain’, which modulates interaction IR [28]. (b) S/T phosphorylation of IRS1. Shown above the sequence are 20 phospho-S/T residues (p-S/T) for which the function has been investigated using site-specific methods; these include S→A (alanine) or S→E (glutamic acid) mutation to ablate or mimic phosphorylation, as well as descriptive investigation with phospho-specific antibodies (commercially available antibodies in green). Shown below the sequence are 34 additional conserved phospho-S/T sites identified only by MS of mouse/rat IRS1; different/additional phospho-S/T are known in human IRS1 (hS629 and not shown). The size of the circles is proportional to the number of PubMed references and/or MS datasets per site at the time of writing within the curated database at www.phosphosite.org (accessed 31 December 2011). Four phospho-S/T were added from [58]. The mouse amino acid numbering is used here except as noted. aFor the corresponding human phospho-S/T, please see Fig. 3
As the IRS tails are not structured within functional domains, several mechanisms have been proposed by which their S/T phosphorylation regulates IRS function. Almost all of the available data concern IRS1. Recently, specific phospho-S/T residues on IRS1—discovered via protein MS—have been shown to mitigate its tyrosine dephosphorylation or inhibitory phosphorylation at other S/T residues [31, 32] (see below). Initially, however, potential inhibitory S/Ts on IRS1 were investigated via a candidate approach, with a bias towards those near tyrosines in PI3K-binding (YXXM) motifs, or proximal to the IRS1 PTB domain. For example, the simultaneous mutation to alanine of four S/Ts near IRS1 YXXMs (mS612/632/662/731A; hS616/636/ 666/736A) was shown to increase basal and insulin-stimulated IRS1 tyrosine phosphorylation and associated PI3K activity [33]. In another early study, TNFα—an inflammatory cytokine that can cause insulin resistance in healthy human muscle [34, 35]—was shown to stimulate multi-site S/T phosphorylation of IRS1 and IRS2, blocking their interaction with an IR juxtamembrane domain peptide [36]. One result of this pattern of investigation is that— because of the availability of phospho-specific antibodies generated in early studies—the phosphorylation of a few IRS1 S/Ts has been interrogated in many different contexts, while the function of many others (particularly on IRS2) has never been addressed (Fig. 2b).
Role of IRS1 S307 (hS312) and other PTB-proximal S/T residues
The investigation of insulin desensitisation by TNFα bolstered the case for a special role of the PTB-proximal region. TNFα activates pathways involving the S/T kinases inhibitor of nuclear factor kB kinase β (IKKβ) and c-Jun N-terminal kinase (JNK) [37]. Treatment of CHO cells with the low-specificity JNK agonist anisomycin was used to identify S307 (hS312) near the IRS1 PTB domain as a major site of phosphorylation [38]. Anisomycin downregulates IRS1 tyrosine phosphorylation in cells, dependent on the presence of both S307 and the IRS1 PTB domain. Although other kinases are activated by anisomycin, JNK1 in CHO cells binds directly to IRS1 via a JNK-binding domain within a.a. 555–898 [38]. Other agents—including insulin in rodent and human tissues—can stimulate phosphorylation of S307 via JNK-independent pathways [39]. In cultured cells that produce very little IRS2, insulin stimulates S307 phosphorylation via a PI3K pathway requiring the IRS1 YXXM motifs [39, 40]. mTOR complex 1 (mTORC1) can mediate insulin- or anisomycin-stimulated S307 phosphor-ylation [41], casting some doubt on the significance of insulin-stimulated JNK phosphorylation of S307 observed in cultured cells [42]. Regardless, in a ‘three-hybrid system’ consisting of IR, IRS1 and activated JNK in yeast cells, S307 phosphorylation is specifically required for the disruption by JNK of the IR–IRS1 interaction [40], although other phospho-S/Ts might contribute [43].
Whether or not the conditions in yeast faithfully represent IR–IRS interaction in mammalian cells, phosphorylation of S307 (hS312) provides the best available ‘structure’-based mechanism for understanding the desensitisation of insulin signalling. Indeed, altered S307 phosphorylation is frequently used as evidence of insulin resistance (or its resolution) in mice, despite the influence of insulin on S307 phosphorylation and the probable contribution of other phospho-S/Ts [44]. As the exact spatial determinants affected by S307 phosphorylation remain unknown, it is unclear whether phosphorylation of other PTB-proximal S/Ts engages a similar mechanism; of those investigated to date, most are farther from the PTB domain than S307 (Fig. 2b), and were not required for anisomycin desensitisation of insulin signalling by IRS1 [38]. Additionally, a number of PTB-proximal S/Ts (including S307 in mice) have a partially permissive or positive role in IRS1 signalling (see below). Other phospho-S/T having inhibitory effects have also been described that lie some distance from either the IRS1 PTB domain or PI3K-binding YXXM motifs (Figs 2b and 3). Potentially then, the disruptive effect of S307 phosphorylation might be an assay- or condition-dependent aspect of a more generalised S/T phosphorylation-based mechanism governing IRS signalling [5, 45, 46].
Degradation of IRS by prolonged insulin/mTORC1 signalling
Importantly, multi-site S/T phosphorylation of IRS in cultured cells correlates with their subcellular re-localisation and/or proteasome-mediated degradation. This can be stimulated by prolonged exposure of cells to insulin, or specific activation of the mTORC1→ribosomal S6 protein kinase (S6K1) branch of the insulin signalling cascade [47–51]. For example, in 3T3L1 adipocytes, prolonged insulin stimulation causes transit of hyper-S/T-phosphorylated IRS1 from low-density membrane (LDM/high speed pellet) to the cytosol, and this can be inhibited by the mTORC1 inhibitor rapamycin [47, 48]. Prior treatment with proteasome inhibitors can block the insulin-induced degradation of IRS1, but not its intracellular transit or the desensitisation of downstream signalling and glucose uptake [48]. Thus, S/T phosphorylation at many sites together converts IRS proteins to an inactive state, separable from their inactivation by degradation; it was further suggested that this ‘array phosphorylation’ of IRS (particularly within the PTB-proximal regions) is necessary for the desensitisation of insulin signalling by diverse signals [5, 45]. Counter to this idea, the mutation of mS307 to alanine in cultured cells has a rapamycin-like effect, in that it blocks IRS1 disappearance during prolonged insulin stimulation [51, 52]; however, it is not shown that S307A mutation alone alters IRS1 localisation and/or PI3K signalling in these studies.
It can now be appreciated that feedback S/T phosphorylation of IRS by mTORC1 and/or S6K1 underlies their disappearance during persistent insulin stimulation [49, 50]. Among the IRS1 S/T phosphorylated directly by these kinases in vitro are S302 and S522 (hS307 and hS527) by S6K1 [51], and S632 (hS636) by mTORC1 [53, 54]. Additional S/T are phosphorylated in vivo by S6K1 (S265 and S1097; hS270, hS1101) [55, 56] or by mTORC1/other kinases (S307 and S612; hS312, hS616) [51] when mTORC1→S6K1 signalling is strongly activated (Fig. 1b). In cells that lack the tuberous sclerosis complex (TSC) proteins or overexpress their target, Ras homologue enriched in brain (RHEB), phosphorylation of these sites is associated with substantial diminution of the ‘active’ (LDM) fraction of IRS1 [51] and AKT activity (Fig. 1b and below); however, in some RHEB-overexpressing cells, IRS1 is degraded without prior trafficking to the cytosol [51]. Presumably, the active IRS1 fraction corresponds to the rare, non-cytoplasmic sites of PI3K localisation in insulin-treated cells [57]; however, it remains unclear to what degree the active fraction is S/T phosphorylated.
Phospho-S/T patterns governing normal insulin signalling
To expand the repertoire of IRS S/T sites available for study, we and others have employed MS of insulin- or serum-stimulated cells or human muscle tissue collected after hyperinsulinaemic–euglycaemic clamp [31, 58–60]. Though coverage by MS is usually incomplete and variable, the sum of these and other efforts may be approaching saturation, such that the validation of hot/cold-spots of IRS S/T-phosphorylation is now conceivable [5] (Fig. 2b). For example, little S/T phosphorylation occurs within the PH/ PTB region, or around the PI3K-binding tyrosine residues of IRS1 (mY608, mY628; hY612, hY632)—though this could be an artefact of sequence composition or coverage. Similarly, there may be relatively little S/T phosphorylation about the GRB2- and PI3K-binding tyrosines (mY891, mY935; hY896, hY941). Interestingly, this region of IRS1 contains the human Gly972Arg polymorphism that in some studies is associated with type 2 diabetes risk [61] and might reduce Y941 or Y989 phosphorylation by disrupting an (unknown) IRS1 secondary structure [62]. MS further reveals post-translational modification of IRS1 by lysine acetylation and serine-linked N-acetylglucosamine (O-GlcNAc) (www.phosphosite.org). The O-GlcNAc modification of serines near the mY935-XXM motif (a.a. 910–1037) or elsewhere can also impair IRS1–PI3K interaction [63, 64].
Using quantitative MS, Yi et al compared 15 IRS1 phospho-S/Ts in hyperinsulinaemic–euglycaemic clamped human muscle [59]. Phosphorylation of six S/T scattered across the IRS1 tail region—hS312, hS616, hS636, hS891, hS1101 and hS1223 (mS307, mS612, mS632, mS887, mS891, mS1097 and mS1214)—was elevated to between 125% and 300% of unclamped value. Of these, phospho-S312, -S616, -S636 and -S1101 are associated with desensitisation of insulin signalling (above and [56, 65]), whereas phospho-S1223 has a sensitising effect [31]. In the same samples, four other mostly clustered phospho-S/T—hS348, hT446, hT495 and hS1005 (mS343, mT441, mI490, mS999)—were decreased by 60–90%. This regionally decreased S/T phosphorylation might represent turnover (or dephosphorylation) of some phospho-species during prolonged stimulation. Interestingly, deletion of a.a. 386–430 of (rodent) IRS1 (termed ‘DIDI’) can block the degradation, but not ubiquitination, of IRS1 in insulin-stimulated cells via a nuclear proteasomal pathway [46]. Potentially, prohibiting ‘array’ phosphorylation of this S/T-rich region might block IRS1 degradation; mutation of S408 (hS413) alone does not [46]. In contrast with DIDI, a.a. 522–574 of (mouse) IRS1 are required for its ubiquitination and degradation via the cullin 7 E3 ligase [66]. Compatible with regulated ubiquitin/proteasomal processing of IRS1, exposure of HEK293 cells to very high insulin showed that about 50% of total IRS1 could be degraded within 10 min via internal cleavage around hS475 or hS641; however, the necessary factors were not investigated [67]. Together, these disparate observations are suggestive of the paths by which insulin-stimulated S/T phosphorylation governs normal signalling and turnover of IRS1. (IRS1 degradation by non-insulin stimuli, via lysosomal and caspase pathways, is briefly reviewed elsewhere [46].) IRS2 (but not IRS1) protein concentration in mouse liver is decreased during refeeding via a PI3K-dependent mechanism [68]. Reasonably, this could involve mTORC1→S6K1 activity; however, unique mechanisms might terminate IRS2 signalling, as it lacks the DIDI region (or an obvious counterpart to mS307/hS312 of IRS1), and exhibits different cell partitioning than IRS1 in cultured cells [69].
Making sense of ‘positive’ ‘negative’ S/T sites
Importantly, studies in cultured cells demonstrate a positive effect of some IRS1 phospho-S/T on insulin signalling (Fig. 3, green circles). For example, insulin-stimulated phosphorylation of hS1223 (mS1214) reduces IRS1–SHP2 interaction, sustaining IRS1 tyrosine phosphorylation and PI3K association [31]. Similarly, phosphorylation of hS629 reduces IRS1 phosphorylation at S636 [32]. Thus, feedback S/T phosphorylation of IRS by insulin-stimulated (autologous) pathways can strengthen the output insulin signal by reducing tyrosine dephosphorylation and inhibitory S/T phosphorylation at other sites. Another positively acting mechanism is the still poorly understood priming of insulin signalling by basal or rapid insulin-stimulated S/T phosphorylation. Early phosphorylation of IRS1 at S302 and S318 (hS307, hS323) after insulin treatment enhances insulin signalling and potentiates its later downregulation [70]. There may also be a priming effect of S632 (hS636) phosphorylation by rho-associated coiled-coil containing protein kinase 1 (ROCK1) in mice [71, 72]. These data demonstrate that the temporal pattern of insulin-stimulated S/T phosphorylation can determine whether some S/Ts are ‘positive’ or ‘negative’. Compatible with this, we have shown that, in CHO and 32D cells, glucose- or amino acid-stimulated phosphorylation of mS302 (hS307) in the basal state potentiates the insulin-stimulated tyrosine phosphorylation of IRS1 and downstream signalling [73]. Yet S302 phosphorylation is implicated in the degradation of IRS1 caused by excessive mTORC1→S6K1 activation [51]. Increased basal, or other temporally inappropriate phosphor-ylation of such ‘positive’ S/T during hyperinsulinaemia or by cross-talking pathways may underlie their pathogenic conversion to ‘negative’ sites [6]. Additionally, some S/T (e.g. S24) might be phosphorylated via inflammatory/stress pathways activated specifically in type 2 diabetes (Fig. 3).
Aetiological framework for consideration of IRS S/T phosphorylation
Prospective studies first identify insulin resistance in human skeletal muscle, which is thought to contribute, via a dys-metabolic process, to the emergence of phenotypic disease [3, 74]. Key to this theory are studies of the non-diabetic offspring of type 2 diabetes patients. Screening of this group for impaired glucose tolerance (IGT) identifies ‘pre-diabetic’ individuals with variably increased fasting plasma insulin and triacylglycerol (TAG) concentrations, but nearly normal fasting glycaemia. Frequent sampling of postprandial blood in these individuals—in combination with more sophisticated tracer/ imaging techniques to monitor metabolism—reveals the redirection of dietary carbohydrate away from glycogen synthesis in muscle and toward the insulin-driven synthesis of TAG in the liver [75, 76]. Related studies show that decreased muscle glucose transport via the GLUT4 path underlies this alteration [74, 77]. Importantly, in early disease, compensatory insulin hypersecretion controls glycaemia, whilst further promoting hepatic TAG synthesis and dyslipidaemia [78]. In the longer term, increased delivery of NEFA/TAG to non-adipose tissues contributes to the activation of lipid-dependent and inflammatory signals that further aggravate insulin resistance [74, 79]. Thus, early muscle insulin resistance provides a unifying basis for emergent features of the metabolic syndrome.
Direct observations of human muscle do not support diminished IRS protein concentration as a primary cause of insulin resistance, though most studies have not examined IRS2 ([80, 81], and reviewed in [4]). Biopsies of muscle from non-diabetic relatives of type 2 diabetic patients taken during or after hyperinsulinaemic clamp show normal IR autophosphorylation but diminished total (or fold vs unclamped) IRS1 phosphotyrosine and associated PI3K activity [80, 81]. In contrast, insulin-stimulated AKT phosphorylation (S473) in these and other studies is not significantly reduced. However, few studies of human muscle have specifically examined the activity of AKT2 [82]. Additionally, AKT S473 phosphorylation may not fully reflect upstream IRS→PI3K signalling, as non-diabetic but glucose-intolerant individuals can show significantly impaired muscle aPKC activation [83]. aPKC signalling (and/or other steps in the muscle GLUT4 path) might be more sensitive to dysregulation than AKT, as one study found no difference vs control individuals in phosphorylation of AKT (S473) or AKTsubstrate of 160 kDa (AS160), despite the presence of impaired glucose disposal [84]. Regardless, defective muscle IRS1→PI3K→AKT signalling in lean normoglycaemic offspring of type 2 diabetics has been correlated with increased basal S/T phosphorylation of IRS1—including at mTORC1 sites S312 and S636 (mS307, mS632), and S616 (mS612) [85]. Thus, dysregulated S/T phosphorylation of IRS might contribute to impaired aPCK/AKT activation and glucose disposal in the pre-diabetic period.
Skeletal muscle samples/cultures from type 2 diabetic individuals exhibit defects in IRS/PI3K→aPKC signalling similar to those seen in ‘pre-diabetes’, but with more obvious diminishment of AKT phosphorylation [86, 87] (reviewed in [82]). In contrast with AKT, basal or insulin-stimulated ERK1/2 activation in diabetic muscle is unchanged or increased in several studies, compatible with its partial independence from IR/IRS [82, 86]. The activation/levels of two other IRS kinases, ROCK1 and G protein-coupled receptor kinase 2 (GRK2), is mechanistically independent of IRS [20] but is clearly influenced by insulin and altered in type 2 diabetes [88–90]. Increased basal phosphorylation of a few IRS S/T—S312 [87], S323 [60], and S636 [91] (mS307, mS318, mS632)—has been described in muscle of type 2 diabetic individuals, whereas basal and stimulated phosphorylation of S330 (mS325) is specifically decreased in muscle of obese insulin-resistant individuals [60]. Insulin additionally fails to normally stimulate the increase, in diabetic muscle, of phospho-S531 and phospho-S1142 (or decrease in phospho-S1100) (mS526, mS1136, mS994) seen in lean control muscle [60]. Further quantitative studies are necessary; however, the available data from human muscle are compatible with a model of temporally perturbed IRS S/T phosphorylation in metabolic disease.
(Dys-)regulation of IRS by insulin-regulated S/T kinases
Given their co-incidence and propensity to aggravate one another, it cannot be stated whether hyperinsulinaemia or dyslipidaemia (or still other factors) underlie increased IRS S/T phosphorylation in the pre-diabetic period [85]. However, as insulin is clearly a relevant stimulus for IRS S/T phosphorylation in healthy muscle (e.g. [59]), we emphasise that this regulatory function might be subverted/co-opted by diabetogenic factors—not excluding hyperinsulinaemia itself. For example, increased basal (or disordered) S/T phosphorylation owing to hyperinsulinaemia might be enough to temporally advance a step-wise signalling process. Alternatively, escape from feedback inhibition by partially insulin-independent pathways/kinases (mTORC1→S6K1 or ERK1/2) might contribute to nutrient and/or hyperinsulinaemia-driven signal termination. Below, we review the effects of specific insulin-regulated S/T kinases on IRS function. The affected S/T residues within IRS1 are outlined in Fig. 3. As far less is currently known about IRS2 S/T phosphorylation, we refer the reader to other, limited sources [5, 92].
Atypical PKCλ/ι, (PKCζ
In mice, the major aPKC isoform in skeletal muscle is PKCλ, whereas in cultured cells and rat muscle PKCζ may predominate; however, the two are highly similar and thought to have interchangeable activity [23]. (In human muscle, the PKCι orthologue of PKCλ appears to predominate [93].) Activation of aPKCs by ceramide can contribute to insulin resistance in mice, though this appears to be due mostly to effects on AKT (reviewed in [94]). In contrast, in Fao or NIH3T3 cells stably expressing IR, overexpression of PKCζ enhances the dissociation from IR and decrease in IRS1 tyrosine phosphorylation caused by prolonged insulin stimulation [95, 96]. An in vitro kinase assay identifies S318 (hS323) on IRS1 as a major site of PKCζ phosphorylation, and negative effects of PKCζ during prolonged insulin stimulation are abrogated by mutation of S318 to alanine (S318A) [97]. However, PKCζ can phosphorylate IRS1 in vitro on S498, S570 and S612 (hS503, hS574, hS616), with phospho-S570 having an adverse effect on PI3K binding [98]. In C2C12 myotubes or mouse skeletal muscle, S318 (hS323) can additionally be phosphorylated upon treatment with IL6 or leptin by the novel PKC (nPKC) isoform PKCδ [99, 100]. These results highlight the tendency for insulin-dependent and heterologous kinase pathways to promote phosphorylation of IRS on many of the same regulatory S/T.
Phosphorylation of mS318/hS323 provides a temporal model for understanding pathway cross-talk. Though S318A mutation aids retention of IRS1 tyrosine phosphor-ylation during prolonged stimulation, it impairs acute AKT S473 phosphorylation in skeletal muscle cells [101]. Conversely, phosphomimetic mutation of S318 to glutamate (S318E) enhances early signalling [70]. Treatment of C2C12 cells with inhibitors implicates JNK and mTORC1 as additional insulin-stimulated S318 kinases [102], demonstrating that multiple pathways may converge on unique S/T to programme the output signal. However, time-resolved studies show that the positive (acute) function of S318 results from its phosphorylation by PKCζ—dependent, to some degree, on S302 (hS307) phosphorylation—whereas its later, negative function results from phosphorylation by mTORC1 [70]. Thus, phosphorylation of S318 is not itself inhibitory, but is necessary to potentiate longer term down-regulation of signalling. PKCδ phosphorylation of S318/ hS323 and other residues may co-opt this chronic function to desensitise insulin signalling [99, 100, 103]. Given the impairment of aPKC activity in diabetes [82, 83], the recent observation of increased basal hS323 phosphorylation in muscle of type 2 diabetic individuals [60] could represent cross-talk by nPKCs or other kinase(s).
AKT
In contrast to PKCλ, overexpression of membrane-localised AKT (in CHO-T cells) promotes retention of IRS1 tyrosine phosphorylation during prolonged insulin stimulation (after 1 h), with no effect on its acute phosphor-ylation (after 2 min) [104]. Collective mutation of four serine residues accounting for much of the in vitro phosphorylation of IRS1 by AKT (mS265/S302/S325/S358A; hS270/S307/S330/S363A) eliminates this positive effect. AKT may also phosphorylate S267 (hS272) in TNFα-treated cells [105]. As revealed by mutation, AKT-dependent phosphorylation of S629 in human IRS1 aids IRS1 tyrosine phosphorylation and p85 binding [32]; however, S629 is an asparagine residue in rodent IRS1 (mN625). The positive effect of phospho-hS629 is associated with decreased phosphorylation of S636 (mS632), a site on IRS1 thought to mediate negative feedback by mTORC1 and ERK1/2 kinases [53, 54, 91]. Quantitative MS on muscle from lean, obese and type 2 diabetic humans does not identify differences in S629 phosphorylation [60]. In contrast to hS629, phosphorylation of mS522/hS527 by AKT is inhibitory. We have shown that insulin-stimulated S522 phosphorylation—which is inhibited by small interfering RNA against AKT—impairs IRS1 tyrosine phosphorylation and PI3K binding in HEK293 cells [58]. Compatible with phosphorylation of hS527 by AKT, phospho-S527 is significantly stimulated during hyperinsulinaemic clamp in muscle of healthy humans [60]. Any regulatory effects of AKT-mediated IRS phosphorylation are obscured in knockout mice by the necessity of AKT2 for downstream signalling [22]; however, less complete impairment of AKT activity, such as that observed in diabetic muscle, might have a partial homeostatic effect, by reducing inhibitory feedback via downstream mTORC1→S6K1 signalling.
mTORC1 and S6K1
The mTORC1 and S6K1 kinases directly phosphorylate unique sites on IRS1 and other proteins (Fig. 1b); S6K2 can also phosphorylate IRS1 in vitro, but does not compensate for loss of S6K1 in knockout mice [51, 106]. Mice lacking mTOR or raptor in muscle, or S6K1 in all tissues, highlight the role of mTORC1→S6K signalling in the growth and maintenance of skeletal muscle (reviewed in [107]). IRS-deficient muscles also undergo atrophy, with impaired phosphorylation of S6K and its substrate, ribosomal S6 protein [14]. Nonetheless, mTORC1/S6K can be stimulated by nutrients independently of IRS [107]—most clearly by branched-chain amino acids (BCAA) such as leucine [108]. Thus, though AKT signalling to mTORC1 is diminished in diabetes, the over-supply of nutrients in obesity is hypothesised to promote mTORC1/S6K phosphorylation of IRS and other targets, aggravating insulin resistance (reviewed in [109, 110]). Increased plasma BCAA levels in obese, insulin-resistant persons have long been regarded as part of an insulin-resistant metabolic ‘signature’ [110, 111], but supplementation of rodent diets with mixed BCAA or leucine has not clarified that this is diabetogenic [111, 112]. In contrast, infusion of complex amino acid mixtures (AA) into humans with clamped hyperinsulinaemia (to repress gluconeogenesis from amino acid precursors) decreases the rate of glucose disposal by about a third, with post-clamp muscle biopsies showing decreased IRS1 tyrosine phosphorylation and increased phosphorylation on S312 and S636 (mS307, mS632) [113]. Similar human studies demonstrate the involvement of mTORC1 in these effects [114], as well as the stimulation by AA of IRS1 S1101 (mS1097) phosphorylation in muscle, likely by S6K1 [56].
Rodents fed a high-fat diet to cause obesity and insulin resistance show increased basal mTORC1→S6K activation in metabolic tissues, with pronounced phosphorylation of IRS1 at S632 and/or S302 (hS636, hS307) [106, 115]. Adipose tissues of genetically obese (ob/ob) mice exhibit increased phosphorylation of S265 (hS270), S302 (hS307), S307 (hS312), S632 (hS636), and S1097 (hS1101) on IRS1— which (except for mS307/hS312) can be phosphorylated by S6K1 in vitro [51, 55]. Deletion of the gene encoding S6K1 protects mice against high-fat-diet-induced insulin resistance, while reducing phosphorylation of IRS1 S302 and S632 in adipose (and S1097 [hS1101] in liver) to levels seen in chowfed mice [56, 106]. However, mS302 (hS307) phosphorylation in cultured cells potentiates, rather than inhibits, downstream insulin signalling by IRS1 [73]. mTORC1 binds within a.a. 250–584 of rodent IRS1 in a nutrient-stimulated and AKT-independent fashion to phosphorylate S632 (hS636), but neither S302 nor S307 (hS307, hS312) phosphorylation are required for this to occur [54]. Thus, mTORC1 and S6K appear to independently target IRS1, despite the decreased S632 (h636) phosphorylation seen in mice lacking S6K1.
Interestingly, insulin-stimulated phosphorylation of S307 (mS302) in human primary adipocytes correlates with donor insulin sensitivity [116] and is decreased in adipocytes of humans with type 2 diabetes [117]. Though this could be due to lower AKT activity (i.e. upstream insulin resistance), the implication is that mTORC1 activity is reduced in insulin-resistant human adipocytes in vivo [116]. Whether nutrients per se drive mTORC1/S6K-mediated phosphorylation of IRS1 in obesity is also somewhat unclear. Hyper-insulinaemia might contribute, as phosphorylation of S636 (mS632) is elevated in muscle of lean insulin-resistant humans [85]. Additionally, mTORC1→S6K signalling can be activated by TNFα (levels of which are increased in obesity) via IKKβ-dependent phosphorylation of TSC1 [118]. Notably, in mouse embryonic fibroblasts, IKKβ is required for TNFα-stimulated phosphorylation of IRS1 S265; mutation of this residue in HEK293 cells (hS270) reduces TNFα stimulation of IRS1–S6K interaction and other IRS1 phospho-S/T elevated in adipose tissue from ob/ob mice [55].
ERK1/2
The partial IRS-independence of insulin-stimulated ERK1/2 activation makes these kinases candidates to mediate chronic IRS S/T phosphorylation in metabolic disease. For example, insulin-stimulated activation of ERK1/2 is normal in obese and type 2 diabetic individuals, whereas PI3K activation is impaired or almost absent [86]. ERK1/2 activation is also sensitised to insulin in adipocytes from humans fed a high-energy diet, potentially contributing to the adaptive expansion of adipose tissue [119]. Compatible with this, mice lacking ERK1 exhibit decreased white adipose mass [86], and greater sensitivity to insulin than control mice during high-fat feeding. Potentially contributing to the latter finding, ERK1/2 can promote lipolysis and NEFA-mediated insulin resistance, both by downregulating adipocyte perilipin [120] and activating hormone-sensitive lipase [121].
In mouse liver, knockout of Gab1 or Ptpn11 (encoding an IRS-like adaptor protein or SHP2, respectively) dramatically reduces insulin-stimulated ERK1/2 activity, while increasing IRS1 tyrosine phosphorylation and systemic insulin sensitivity [25, 122]. However, the effects of Ptpn11 deletion might be due to improved tyrosine phosphorylation of IRS, rather than diminished ERK1/2 activity. Interestingly, in Ptpn11 knockout liver, insulin-stimulated IRS1 phospho-S307 (hS312) increases, contrary to the inhibitory function of S307 phosphorylation in cultured cells [25]. In Gab1 knockout liver, insulin-stimulated IRS1 phospho-S612 (hS616) is clearly decreased [122]. Impaired feedback phosphorylation of S612 (presumably by ERK1/2) is also seen in muscle of Grb2+/- heterozygous mice, in conjunction with increased AKT activation [123]. Conversely, increased ERK1/2 phosphorylation of mS612/hS616 is associated with angiotensin II-mediated impairment of endothelial nitric oxide synthase activation (by AKT) in vascular endothelial cells [124]. Knockdown of Grb2 expression in C2C12 muscle cells decreases both S612 (hS616) and S632 (hS636) phosphorylation [123]. Consistent with a pathological effect of ERK-dependent IRS1 phosphor-ylation, hS636 phosphorylation is elevated in muscle cells from type 2 diabetic individuals, and this is reduced by chemical inhibition of ERK1/2 activity [91].
ROCK1
Activity of the ROCK1 S/T kinase correlates positively with insulin sensitivity in cells and animals. Inhibition of ROCK1 in cell and muscle cultures reduces insulin-stimulated IRS1 tyrosine phosphorylation, PI3K activity and glucose uptake, and similar effects are achieved by ROCK1 inhibition in mice [71]. ROCK1 can phosphorylate IRS1 in vitro on the S632/635 pair (hS636/639), as well as mS932 and mS968. Insulin-stimulated phosphorylation of S632/635 (assayed by a single antibody) is decreased by ROCK1 inhibition or knockdown, or by expression of dominant-negative ROCK1 [71]. Surprisingly—given the apparent involvement of phospho-S632 (hS636) in desensitisation of insulin signalling [53, 91]—double mutation of S632/ 635 to alanine in CHO cells reduces IRS1 tyrosine phosphor-ylation and PI3K binding [71]. Some data suggest that ROCK1 inhibits, rather than promotes, IRS signalling [125], and it has not been demonstrated whether phosphomimetic mutation of mS632 and mS635 can overcome the negative effects of ROCK1 inhibition/knockdown. Regardless, Rock1 knockout mice exhibit insulin resistance with impaired muscle insulin signalling, including decreased insulin-stimulated S632/5 phosphorylation [72]. Insulin-stimulated ROCK1 activity is also decreased in muscle of obese diabetic humans, in conjunction with upregulation of its kinase inhibitor RhoE [88]. Thus, RhoE or other negative regulators of ROCK1 might be suitable targets for the treatment of insulin resistance in diabetes.
GRK2
Also known as β-adrenergic receptor kinase-1 or βARK1, GRK2 provides a link between altered vascular/ tissue physiology in insulin resistance and impaired IRS signalling. GRK2 is a ubiquitously expressed kinase involved in termination of G protein-coupled receptor (GPCR) signalling, including that mediated by endothelin-1 (ET-1) and β-adrenergic receptors [89, 126]. Phosphorylation of activated GPCRs by GRK family kinases desensitises their signalling by recruiting arrestins that uncouple G protein effectors and promote GPCR internalisation. GRK2 can additionally interfere directly with Gαq/11-mediated signalling via its RGS (regulator of G protein signalling) domain/GAP activity [127]. Increased plasma concentration of the vasoconstrictive ET-1 polypeptide is associated with insulin resistance and/or hypertension [128, 129], which is, in turn, promoted by direct and indirect (sympathoadrenal and angiotensin II-dependent) effects of compensatory hyperinsulinaemia to cause sodium retention (reviewed in [130]). The correlation between excessive β-adrenergic activity and insulin resistance has long been noted [131]. While tissue GRK2 levels have been correlated with plasma norepinephrine/epinephrine levels [132], GRK2 can be upregulated in cultured cells by chronic insulin [89, 90], potentially as a result of PI3K-dependent stabilisation of GRK2 [133]. Thus, both local/circulating GPCR ligands associated with insulin resistance/ hyperinsulinaemia, and insulin itself, contribute to the high GRK2 levels observed in insulin-resistant rodent/human tissues [90]. In this light, it is notable that increased expression of type 1 angiotensin II receptors, promoted by experimental hyperinsulinaemia, correlates with increased IRS1 phosphor-ylation on mS369 [134].
In 3TL1 adipocytes, the IR phosphorylates Gαq/11 to promote CDC42-mediated activation of PI3K- and GLUT4-dependent glucose uptake [135]. ET-1 treatment of these cells reduces GLUT4 translocation, both by GRK2 kinase-independent effects on Gαq/11 (or IR), and by decreasing the level and tyrosine phosphorylation of IRS1 [126]. ET-1 also stimulates phosphorylation of mS612/hS616 on IRS1, and both this phosphorylation and the impairment of GLUT4 translocation by ET-1 are blocked by overexpression of kinase-dead GRK2 [126]. Similarly, insulin-stimulated glucose uptake in HEK293 cells is impaired by overexpression of the β2-adrenergic receptor, which, like insulin, drives increased production of GRK2 [89]. Insulin stimulation rapidly disrupts basal GRK2–IRS1 interaction [90], but excess GRK2 produced during prolonged insulin stimulation becomes progressively bound to IRS1 [89]. In FL83B mouse liver cells, glycogen synthesis is upregulated by GRK2 knockdown, and this is associated with decreased basal and insulin-stimulated IRS1 S307 (hS312) phosphorylation [136]. However, S307 is apparently not directly phosphorylated by GRK2 in ET-1-treated 3T3 cells [126]. Heterozygous mice lacking one copy of the gene encoding GRK2 show enhanced insulin sensitivity and do not develop insulin resistance from TNFα, ageing or high-fat diet challenge [90]. Importantly, and consistent with these data, GRK2-interfering peptides improve insulin sensitivity in diabetic animal models [137]; thus, GRK2 is a potential target for the treatment of insulin resistance.
GSK3
In either its α or β isoform, GSK3 is not an insulin-dependent kinase, but an insulin-regulated one. Its inhibition by AKT means that GSK3 regulation of IRS is important in the basal, rather than insulin-stimulated, state (Fig. 1a). Basal IRS1 phosphorylation by GSK3—investigated via dephosphorylation and re-phosphorylation with purified GSK3β—can inhibit IRS1 tyrosine phosphorylation in vitro by IR [138]. (However, dephosphorylation of basally present phospho-S/Ts is itself inhibitory vs no dephosphorylation [138].) Serine residues phosphorylated by GSK3 are typically primed by phosphorylation at a nearby site (SXXXS motif), and mutation of both S332 and S336 of IRS1 (hS337, hS341) to alanine enhances both basal and insulin-stimulated tyrosine phosphorylation of IRS1, as well as insulin-stimulated AKT activation in cultured cells [139]. Comparison of knock-in mice with constitutively active GSK3 isoforms (α, β, or α and β) demonstrates the predominance of GSK3β in muscle, yet none of these mice show impaired AKT activation or become diabetic [140]. Hence, it seems unlikely that increased GSK3 protein/activity has the potential to significantly dysregulate IRS in diabetes.
AMP-activated protein kinase and salt-inducible kinase 2
AMP-activated protein kinase (AMPK) activity is stimulated by cellular energy deprivation, and so is inversely correlated with AKT activation and ATP production by glycolysis. Placement of serum-starved HEK293 cells into serum/glucose-free medium rapidly activates AMPK phosphorylation of IRS1 on mS789/hS794, and mutation of this residue blocks the impairment of insulin-stimulated AKT activation caused by glucose deprivation [141]. However, the elevated S789 phosphorylation seen in the liver of obese rats is apparently not due to AMPK [142]. The SNF1/ AMPK family kinase known as salt-inducible kinase 2 (SIK2) is upregulated in adipose tissue of obese db/db mice, and can also phosphorylate S789 of IRS1 when co-expressed in cells [143]. However, SIK2 kinase activity is positively regulated by insulin via phosphorylation by AKT2 [144], suggesting an autologous feedback role in the regulation of IRS. Interestingly, treatment of C2C12 muscle cells with the AMPK agonist 5-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside (AICAR) has an additive effect, with insulin, to promote IRS1-associated PI3K activity [145]. However, because this could be due to causes other than S789 phosphorylation, the true effect of phospho-S789 on IRS1 in vivo remains somewhat unclear.
Dysregulation of IRS by heterologous S/T kinase pathways in type 2 diabetes
Despite the existence of numerous insulin-regulated control loops, IRS signalling in metabolic disease is not homeostatic. This is likely due to the continued input of hyperinsulinaemia and partially insulin-independent feedback pathways. As a further complication, lipid and inflammatory signals—which are, at base, potentiated by insulin—can ‘hijack’ the normal insulin regulation of IRS via S/T phosphorylation of the same and additional sites [6] (Fig. 3).
Novel PKCs (PKCθ, ε and δ)
Insulin-driven TAG synthesis, together with impaired prandial repression of adipocyte lipolysis, causes significant dyslipidaemic effects in type 2 diabetes. These include the increased delivery of fatty acids to, and TAG deposition within, non-adipose tissues (e.g. intramyocellular TAG , hepatosteatosis) (reviewed in [74]). Rodent and human studies validate the contribution of dyslipidaemia to skeletal muscle and liver insulin resistance via diacylglycerol-mediated activation of nPKCs, including PKCθ [65, 146, 147], PKCδ [148] and PKCε [149, 150] (reviewed in [74, 94]). Diabetic skeletal muscle and liver tissues are characterised by increased PKCθ and PKCε levels, respectively [151, 152].
Intramyocellular diacylglycerol can be generated in humans and rodents by normal phospholipid metabolism or, experimentally, by the infusion of TAG emulsions plus heparin to activate tissue lipase [153]. In rats, the induction of high plasma NEFA concentrations (~3 mmol/l) by this method impairs clamp-stimulated muscle IRS1 tyrosine phosphorylation and PI3K activity, glucose transport/oxidation, and glycogen synthesis, while increasing membrane PKCθ activity [153]. Lipid infusion in humans can also activate muscle PKCδ and (canonical) PKCβ2 [154]. Diverse mechanisms may underlie insulin resistance in different lipid infusion protocols, depending on the concentration of NEFA achieved. Regardless, moderate lipid infusion in mice (~1.5 mmol/l NEFA) impairs muscle IRS1 tyrosine phosphorylation, PI3K activity and glucose disposal, and these effects are lost in Prkcq (PKCθ) knockout mice [147]. Infusion-mediated induction of somewhat higher NEFA levels causes insulin resistance in rats, accompanied by elevated muscle IRS1 S307 (hS312) phosphorylation [146]. Nevertheless, PKCθ is not a proline-directed kinase, and phospho-S307 is not diminished in muscle of lipid-infused Prkcq knockout mice. In contrast, PKCθ directly phosphorylates IRS1 on hS1101/mS1097, and mutation of this residue protects against PKCθ-mediated desensitisation of insulin resistance in CHO cells [65].
Kahn and colleagues [148] analysed levels of the various PKCs in liver from non-obese and obese mice, identifying upregulation of PKCδ in insulin-resistant C57BL6 mice. Liver-specific or global knockout of Prkcd (which encodes PKCδ) enhances liver insulin sensitivity and signalling, improves glucose tolerance, and reduces age-dependent hepatosteatosis [148]. Prkcd knockout liver shows decreased IRS1 S307 (hS312) phosphorylation; however, it is unclear (see above) whether aPKCs directly phosphory-late S307 in vivo. In contrast, decreased S612 (hS616) phosphorylation in Prkcd knockout liver likely reflects its targeting by PKCδ [148]. Mutation of S612 is sufficient to protect HEK293 cells against the desensitisation of insulin signalling by phorbol 12-myristate 13-acetate (PMA)-activated novel and conventional PKC (cPKC) isoforms [155]. PKCδ can phosphorylate IRS1 in vitro on at least 18 S/T, reducing its tyrosine phosphorylation by IR [156]. However, S302, S318 and S570 (hS307, hS323, hS574) are the major sites, and mutation of these residues alleviates inhibition of IRS1 tyrosine phosphorylation by IR in vitro [156]. Similarly, mutation of S408 or S357 (hS413, hS362) at least partially blocks the desensitisation of insulin signalling by PKC pathways in PMA-treated cells [157, 158].
Conventional PKCs (PKCα, PKCβ)
In mouse muscle and adipose tissues, knockout of Prkca (encoding PKCα) enhances IRS1/PIK3→AKT and aPKC signalling, as well as glucose transport [159]. The IRS1 PH domain can bind to and be phosphorylated by PKCα on S24; however, phospho-S24 is not observed during chronic insulin stimulation [29]. PKCα in rodent muscle associates basally with IRS1; insulin transiently disrupts this interaction while increasing PKCα association with AKT [160]. In contrast, prolonged insulin stimulation in cultured cells can increase PKCα binding to IRS1 in complex with 14-3-3ε [161]. PKCβ2 can phosphorylate IRS1 on mS336/hS341 in vitro, suggesting it is a priming kinase for GSK3 phosphorylation of IRS1 [162]. Either PKCα or PKCβ can, further, promote IRS1 S307 and S612 (hS312, S616) phosphorylation in PMA-treated cells [29]. Knockout of the gene encoding PKCβ protects mice against high-fat diet induced obesity, insulin resistance, and hepatosteatosis, but might do so independently of effects on IRS [163].
IKKβ and JNK
Impaired glucose uptake and/or insulin resistance within adipose tissue can contribute to the development of type 2 diabetes [164], likely by altering its secretion of adipokines, such as adiponectin or retinol-binding protein 4 (reviewed in [165]). Additionally, the expanded adipose compartment in diabetes/obesity produces pro-inflammatory cytokines such as TNFα and IL1β that can contribute to insulin resistance systemically (reviewed in [79]). These and other stress factors associated with insulin-resistant obesity—including AGEs, vascular glucotoxicity, and liver and adipose tissue endoplasmic reticulum stress—can each contribute to activation of IKKβ and/or JNK (reviewed in [37]). Thus, insulin resistance caused by IKKβ and JNK depends on their cumulative influence on diverse cellular and non-cell-autonomous processes (including immune activation), a fact made clear by analyses of knockout mice lacking JNK1 and/or JNK2 in different tissues (reviewed in [166]).
In contrast with genetic loss of IKKβ or JNK, the treatment of cells/animals with TNFα offers a straightforward model for understanding the connection between adipose inflammation and impaired insulin sensitivity. Type 2 diabetic individuals exhibit increased circulating, adipose and skeletal muscle TNFα concentrations [34], and infusion or treatment with TNFα causes insulin resistance in healthy humans or their cultured muscle cells [34, 35]. TNFα activates multiple kinases in muscle, including S6K, ERK1/2, IKKβ and the IRS1 mS307/hS312 kinase JNK1; however, muscle hS312 phosphorylation is not significantly elevated by TNFα infusion prior to the period in which TNFα causes reduced IRS1 tyrosine phosphorylation and insulin resistance [34]. In contrast, S636/9 (mS632/5) phosphorylation is significantly increased in TNFα-infused humans [34]. In addition, it should be noted that anti-sense knockdown of IKKβ expression in cultured human myotubes does not prevent TNFα-stimulated phosphorylation of IRS1 S312, although it does prevent insulin resistance [35].
IKKβ and JNK are among the few non-AGC family kinases implicated in the dysregulation of IRS, and little direct evidence exists that they phosphorylate IRS, other than at IRS1 S307 (hS312) [39] and S302 (hS307) [43] in cultured cells. JNK, but not IKKβ, can directly phosphory-late S302 and S307 of rodent IRS1 in yeast cells [43]. In contrast, in mammalian cells, IKKβ physically associates with IRS1, and its TNFα-stimulated activity correlates with phosphorylation of mS307/hS312—consistent with IKKβ phosphorylation of this residue in vitro [167]. Nevertheless, the expression of a mutant IRS1 protein (mS265/302/325/ 336/358/407/408A) that retains the possibility of phosphor-ylation at mS307 can block desensitisation of insulin signalling by activated IKKβ in Fao cells [45]. In 3T3L1 cells, TNFα-stimulated phosphorylation of mS307 is dependent upon the interaction of IRS1 with the NEMO/IKKγ subunit of the IĸB kinase complex, promoted by the actin-directed motor protein MYO1C [168]. Phosphorylation of mS307 by insulin and TNFα is additive in these cells, indicating a possible role of IKKβ and/or JNK in feedback phosphorylation of IRS and desensitisation of insulin signalling. Although mechanisms have been described by which insulin might activate JNK, it is not clear to what degree these are operant in healthy tissue [37]. Moreover, although IKKβ can be activated by insulin (via a PI3K-dependent path), neither IKKβ inhibition nor genetic loss of IKKβ potentiates insulin signalling [169]. Furthermore, overexpression of IKKβ in 3T3L1 adipocytes does not impair IRS1 tyrosine phosphorylation/PI3K activity or glucose uptake [169].
Manipulation of IRS S/T phosphorylation in mice
To our knowledge, two studies have directly investigated the function of IRS1 S/T phosphorylation in mice using trans-genesis or genetic knock-in to augment or replace endogenous (wild-type) IRS1 with a mutant version. Shulman and colleagues created transgenic mice with moderate overexpression in skeletal muscle (~twofold vs littermates) of non-mutant IRS1, or mutant IRS1 with alanine substitution of three serine residues—S302/307/612A (hS307/312/ 616A)—to block phosphorylation [170]. Thus, in the triple-mutant transgenic mice, possibly half the total IRS1 protein was endogenous in origin. Matching of IRS1 protein levels is a potentially important consideration given the role of autologous feedback in cultured cells; nonetheless, the mutant transgenic mice showed better glucose tolerance than non-mutant transgenic mice when both were fed a high-fat diet. Compared on a high-fat diet with true wild-type littermates, the mutant transgenic mice showed increased total and muscle glucose disposal during a hyperinsulinemic–euglycemic clamp, and enhanced muscle IRS1 tyrosine phosphorylation and p85 binding in response to insulin. Though somewhat complicated in design, this experiment is consistent with the notion that S/T phosphor-ylation of IRS in skeletal muscle contributes to the development of insulin resistance in animals/humans.
In contrast, we used genetic knock-in to replace wild-type IRS1 in mice with a mutant form (S307A, ‘A’) lacking the ability to be phosphorylated at S307 (hS312) [171]. To control for potential ancillary effects of the knock-in process on IRS1 production/function [172], non-mutant control knock-in mice were also generated (S307S, ‘S’). Surprisingly, given the sensitising effect of the S307A mutation in cell-based assays, homozygous A/A mice show increased fasting insulin vs S/S controls, as well as mild glucose intolerance. Furthermore, high-fat-fed A/A mice exhibit higher fasting insulin and more severe glucose intolerance than wild-type mice, and the A307 IRS1 protein exhibits decreased PI3K binding in insulin-stimulated primary hepatocytes. Thus, S307 phosphorylation appears permissive, rather than inhibitory, for insulin signalling in mice. But why is this? Possibly, a serine is structurally required at position 307 of the IRS1 protein for its normal function. Alternatively, S307 phosphorylation could have a partial positive effect on insulin signal transduction that is more important in tissues/primary cells than its desensitising function in continuous cell lines. By analogy with JNK1 activity, IRS1 S307 phosphorylation could also have mixed, tissue-specific effects that are obscured by the standard knock-in approach [166]. In any case, the phenotype of S307A mice confirms that (non)-phosphorylation of unique S/T sites on IRS1 can affect whole-body insulin sensitivity.
Perspective
The investigation of IRS1 phospho-S/T provides evidence of a highly regulated signalling process. While additional mechanisms clearly contribute, current data suggest that the desensitisation of proximal insulin signalling by IRS S/T phosphorylation plays a significant role in the pathogenesis of human insulin resistance. Nonetheless, a complete understanding of the links between S/T phosphorylation and insulin resistance remains challenging. The large number of known and potential phospho-S/T on IRS makes it difficult to determine their overall patterns in human/animal tissues. Although MS analysis has remedied this situation somewhat, an expanded collection of phospho-specific antibodies might prove advantageous for discerning the co-phosphorylation of disparate S/T. There is also very little knowledge of the structure of the IRS proteins outside their amino termini. This apparent lack of structure is compatible with a mass action effect of S/T phosphorylation in the regulation of IRS. However, as reviewed herein and elsewhere [5, 6], unique phospho-S/T on IRS1 can have negative (or positive) effects on insulin signalling that are currently unexplainable in either structural terms or by a requirement for multiple phosphorylation. We suggest that, collectively, these problems call for the simultaneous quantitative assay of IRS phosphorylation at many S/T in healthy and diseased tissues, coupled with a continued reductive approach to address IRS S/T function in mutant cells, tissues or mice. Regardless of whether IRS constitute drugable targets for the treatment of insulin resistance, a more complete understanding of the S/T phosphorylation patterns that govern their signalling will continue to help delineate the pathophysiological processes that contribute to insulin resistance and diabetes.
Abbreviations
- a.a.
Amino acid residue
- AA
Complex amino acid mixtures
- AMPK
AMP-activated protein kinase
- aPKC
Atypical protein kinase C
- cPKC
Conventional protein kinase C
- ERK
Extracellular signal-regulated kinase
- ET-1
Endothelin 1
- GPCR
G-protein coupled receptor
- GRB2
Growth factor receptor-bound protein 2
- GRK2
G protein-coupled receptor kinase 2
- GSK3
Glycogen synthase kinase
- IGF1R
IGF1 receptor
- IKKβ
Inhibitor of nuclear factor KB kinase β
- IR
Insulin receptor
- IRS
IRS1,2
- JNK
c-Jun N-terminal protein kinase
- MAPK
Mitogen-activated protein kinase
- mTOR
Mammalian target of rapamycin
- mTORC
mTOR complex
- nPKC
Novel protein kinase C
- PDK1
3-Phosphoinositide-dependent kinase
- PH
Pleckstrin homology
- PI3K
Phosphatidylinositol 3-kinase
- PMA
Phorbol 12-myristate 13-acetate
- PTB
Phosphotyrosine-binding
- RHEB
Ras homologue enriched in brain
- ROCK1
Rho-associated coiled-coil containing protein kinase 1
- S6K
Ribosomal S6 protein kinase
- SH2
Src homology 2
- SHP2
SH2 domain-containing protein tyrosine phosphatase-2
- SIK2
Salt-inducible kinase 2
- S/T
Serine/threonine residue(s)
- TAG
Triacylglycerol
- TSC
Tuberous sclerosis complex
Footnotes
Duality of interest The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement The article was conceived, edited and approved for publication in its final form by KDC and MFW.
References
- 1.Reaven G. The metabolic syndrome or the insulin resistance syndrome? Different names, different concepts, and different goals. Endocrinol Metab Clin North Am. 2004;33:283–303. doi: 10.1016/j.ecl.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 2.Biddinger SB, Kahn CR. From mice to men: insights into the insulin resistance syndromes. Annu Rev Physiol. 2006;68:123–158. doi: 10.1146/annurev.physiol.68.040104.124723. [DOI] [PubMed] [Google Scholar]
- 3.DeFronzo RA, Tripathy D. Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care. 2009;32(Suppl 2):S157–S163. doi: 10.2337/dc09-S302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karlsson HK, Zierath JR. Insulin signaling and glucose transport in insulin resistant human skeletal muscle. Cell Biochem Biophys. 2007;48:103–113. doi: 10.1007/s12013-007-0030-9. [DOI] [PubMed] [Google Scholar]
- 5.Boura-Halfon S, Zick Y. Phosphorylation of IRS proteins, insulin action, and insulin resistance. Am J Physiol Endocrinol Metab. 2009;296:E581–E591. doi: 10.1152/ajpendo.90437.2008. [DOI] [PubMed] [Google Scholar]
- 6.Tanti JF, Jager J. Cellular mechanisms of insulin resistance: role of stress-regulated serine kinases and insulin receptor substrates (IRS) serine phosphorylation. Curr Opin Pharmacol. 2009;9:753–762. doi: 10.1016/j.coph.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 7.Fernandez AM, Kim JK, Yakar S, et al. Functional inactivation of the IGF-I and insulin receptors in skeletal muscle causes type 2 diabetes. Genes Dev. 2001;15:1926–1934. doi: 10.1101/gad.908001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng Z, Tseng Y, White MF. Insulin signaling meets mitochondria in metabolism. Trends Endocrinol Metab. 2010;21:589–598. doi: 10.1016/j.tem.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmelzle K, Kane S, Gridley S, Lienhard GE, White FM. Temporal dynamics of tyrosine phosphorylation in insulin signaling. Diabetes. 2006;55:2171–2179. doi: 10.2337/db06-0148. [DOI] [PubMed] [Google Scholar]
- 10.White MF. Insulin signaling in health and disease. Science. 2003;302:1710–1711. doi: 10.1126/science.1092952. [DOI] [PubMed] [Google Scholar]
- 11.Dong XC, Copps KD, Guo S, et al. Inactivation of hepatic Foxo1 by insulin signaling is required for adaptive nutrient homeostasis and endocrine growth regulation. Cell Metab. 2008;8:65–76. doi: 10.1016/j.cmet.2008.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Michael MD, Kulkarni RN, Postic C, et al. Loss of insulin signaling in hepatocytes leads to severe insulin resistance and progressive hepatic dysfunction. Mol Cell. 2000;6:87–97. [PubMed] [Google Scholar]
- 13.Biddinger SB, Hernandez-Ono A, Rask-Madsen C, et al. Hepatic insulin resistance is sufficient to produce dyslipidemia and susceptibility to atherosclerosis. Cell Metab. 2008;7:125–134. doi: 10.1016/j.cmet.2007.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Long YC, Cheng Z, Copps KD, White MF. Insulin receptor substrates Irs1 and Irs2 coordinate skeletal muscle growth and metabolism via Akt and AMPK pathways. Mol Cell Biol. 2011;31:430–441. doi: 10.1128/MCB.00983-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Laustsen PG, Russell SJ, Cui L, et al. Essential role of insulin and insulin-like growth factor 1 receptor signaling in cardiac development and function. Mol Cell Biol. 2007;27:1649–1664. doi: 10.1128/MCB.01110-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bluher M, Michael MD, Peroni OD, et al. Adipose tissue selective insulin receptor knockout protects against obesity and obesity-related glucose intolerance. Dev Cell. 2002;3:25–38. doi: 10.1016/s1534-5807(02)00199-5. [DOI] [PubMed] [Google Scholar]
- 17.Miki H, Yamauchi T, Suzuki R, et al. Essential role of insulin receptor substrate 1 (IRS-1) and IRS-2 in adipocyte differentiation. Mol Cell Biol. 2001;21:2521–2532. doi: 10.1128/MCB.21.7.2521-2532.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hanke S, Mann M. The phosphotyrosine interactome of the insulin receptor family and its substrates IRS-1 and IRS-2. Mol Cell Proteomics. 2009;8:519–534. doi: 10.1074/mcp.M800407-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Franke TF, Kaplan DR, Cantley LC, Toker A. Direct regulation of the Akt proto-oncogene product by phosphatidylinositol-3,4-bisphosphate [see comments] Science. 1997;275:665–668. doi: 10.1126/science.275.5300.665. [DOI] [PubMed] [Google Scholar]
- 20.Pearce LR, Komander D, Alessi DR. The nuts and bolts of AGC protein kinases. Nat Rev Mol Cell Biol. 2010;11:9–22. doi: 10.1038/nrm2822. [DOI] [PubMed] [Google Scholar]
- 21.Sarbassov DD, Guertin DA, Ali SM, Sabatini DM. Phosphor-ylation and regulation of Akt/PKB by the rictor-mTOR complex. Science. 2005;307:1098–1101. doi: 10.1126/science.1106148. [DOI] [PubMed] [Google Scholar]
- 22.Cho H, Mu J, Kim JK, et al. Insulin resistance and a diabetes mellitus-like syndrome in mice lacking the protein kinase Akt2 (PKBβ). Science. 2001;292:1728–1731. doi: 10.1126/science.292.5522.1728. [DOI] [PubMed] [Google Scholar]
- 23.Farese RV, Sajan MP, Standaert ML. Insulin-sensitive protein kinases (atypical protein kinase C and protein kinase B/Akt): actions and defects in obesity and type II diabetes. Exp Biol Med (Maywood) 2005;230:593–605. doi: 10.1177/153537020523000901. [DOI] [PubMed] [Google Scholar]
- 24.Farese RV, Sajan MP, Yang H, et al. Muscle-specific knockout of PKC-λ impairs glucose transport and induces metabolic and diabetic syndromes. J Clin Invest. 2007;117:2289–2301. doi: 10.1172/JCI31408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matsuo K, Delibegovic M, Matsuo I, et al. Altered glucose homeostasis in mice with liver-specific deletion of Src homology phosphatase 2. J Biol Chem. 2010;285:39750–39758. doi: 10.1074/jbc.M110.153734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yenush L, Makati KJ, Smith-Hall J, Ishibashi O, Myers MG, Jr, White MF. The pleckstrin homology domain is the principal link between the insulin receptor and IRS-1. J Biol Chem. 1996;271:24300–24306. doi: 10.1074/jbc.271.39.24300. [DOI] [PubMed] [Google Scholar]
- 27.Eck MJ, Dhe-Paganon S, Trub T, Nolte RT, Shoelson SE. Structure of the IRS-1 PTB domain bound to the juxtamembrane region of the insulin receptor. Cell. 1996;85:695–705. doi: 10.1016/s0092-8674(00)81236-2. [DOI] [PubMed] [Google Scholar]
- 28.Wu J, Tseng YD, Xu CF, Neubert TA, White MF, Hubbard SR. Structural and biochemical characterization of the KRLB region in insulin receptor substrate-2. Nat Struct Mol Biol. 2008;15:251–258. doi: 10.1038/nsmb.1388. [DOI] [PubMed] [Google Scholar]
- 29.Nawaratne R, Gray A, Jorgensen CH, Downes CP, Siddle K, Sethi JK. Regulation of insulin receptor substrate 1 pleckstrin homology domain by protein kinase C: role of serine 24 phosphorylation. Mol Endocrinol. 2006;20:1838–1852. doi: 10.1210/me.2005-0536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim JA, Yeh DC, Ver M, et al. Phosphorylation of Ser24 in the pleckstrin homology domain of insulin receptor substrate-1 by Mouse Pelle-like kinase/interleukin-1 receptor-associated kinase: cross-talk between inflammatory signaling and insulin signaling that may contribute to insulin resistance. J Biol Chem. 2005;280:23173–23183. doi: 10.1074/jbc.M501439200. [DOI] [PubMed] [Google Scholar]
- 31.Luo M, Reyna S, Wang L, et al. Identification of insulin receptor substrate 1 serine/threonine phosphorylation sites using mass spectrometry analysis: regulatory role of serine 1223. Endocrinology. 2005;146:4410–4416. doi: 10.1210/en.2005-0260. [DOI] [PubMed] [Google Scholar]
- 32.Luo M, Langlais P, Yi Z, et al. Phosphorylation of human insulin receptor substrate-1 at Serine 629 plays a positive role in insulin signaling. Endocrinology. 2007;148:4895–4905. doi: 10.1210/en.2007-0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mothe I, Van Obberghen E. Phosphorylation of insulin receptor substrate-1 on multiple serine residues, 612, 632, 662, and 731, modulates insulin action. J Biol Chem. 1996;271:11222–11227. doi: 10.1074/jbc.271.19.11222. [DOI] [PubMed] [Google Scholar]
- 34.Plomgaard P, Bouzakri K, Krogh-Madsen R, Mittendorfer B, Zierath JR, Pedersen BK. Tumor necrosis factor-α induces skeletal muscle insulin resistance in healthy human subjects via inhibition of Akt substrate 160 phosphorylation. Diabetes. 2005;54:2939–2945. doi: 10.2337/diabetes.54.10.2939. [DOI] [PubMed] [Google Scholar]
- 35.Austin RL, Rune A, Bouzakri K, Zierath JR, Krook A. siRNA-mediated reduction of inhibitor of nuclear factor-κB kinase prevents tumor necrosis factor-α-induced insulin resistance in human skeletal muscle. Diabetes. 2008;57:2066–2073. doi: 10.2337/db07-0763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Paz K, Hemi R, LeRoith D, et al. A molecular basis for insulin resistance. Elevated serine/threonine phosphorylation of IRS-1 and IRS-2 inhibits their binding to the juxtamembrane region of the insulin receptor and impairs their ability to undergo insulin-induced tyrosine phosphorylation. J Biol Chem. 1997;272:29911–29918. doi: 10.1074/jbc.272.47.29911. [DOI] [PubMed] [Google Scholar]
- 37.Solinas G, Karin M. JNK1 and IKKβ: molecular links between obesity and metabolic dysfunction. FASEB J. 2010;24:2596–2611. doi: 10.1096/fj.09-151340. [DOI] [PubMed] [Google Scholar]
- 38.Aguirre V, Uchida T, Yenush L, Davis R, White MF. The c-Jun NH2-terminal kinase promotes insulin resistance during association with insulin receptor substrate-1 and phosphorylation of Ser307. J Biol Chem. 2000;275:9047–9054. doi: 10.1074/jbc.275.12.9047. [DOI] [PubMed] [Google Scholar]
- 39.Rui L, Aguirre V, Kim JK, et al. Insulin/IGF-1 and TNF-αstimulate phosphorylation of IRS-1 at inhibitory Ser307 via distinct pathways. J Clin Invest. 2001;107:181–189. doi: 10.1172/JCI10934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aguirre V, Werner ED, Giraud J, Lee YH, Shoelson SE, White MF. Phosphorylation of Ser307 in insulin receptor substrate-1 blocks interactions with the insulin receptor and inhibits insulin action. J Biol Chem. 2002;277:1531–1537. doi: 10.1074/jbc.M101521200. [DOI] [PubMed] [Google Scholar]
- 41.Carlson CJ, White MF, Rondinone CM. Mammalian target of rapamycin regulates IRS-1 serine 307 phosphorylation. Biochem Biophys Res Commun. 2004;316:533–539. doi: 10.1016/j.bbrc.2004.02.082. [DOI] [PubMed] [Google Scholar]
- 42.Lee YH, Giraud J, Davis RJ, White MF. c-Jun N-terminal kinase (JNK) mediates feedback inhibition of the insulin signaling cascade. J Biol Chem. 2003;278:2896–2902. doi: 10.1074/jbc.M208359200. [DOI] [PubMed] [Google Scholar]
- 43.Werner ED, Lee J, Hansen L, Yuan M, Shoelson SE. Insulin resistance due to phosphorylation of IRS-1 at serine 302. J Biol Chem. 2004;279:35298–352305. doi: 10.1074/jbc.M405203200. [DOI] [PubMed] [Google Scholar]
- 44.Ozcan U, Cao Q, Yilmaz E, et al. Endoplasmic reticulum stress links obesity, insulin action, and type 2 diabetes. Science. 2004;306:457–461. doi: 10.1126/science.1103160. [DOI] [PubMed] [Google Scholar]
- 45.Herschkovitz A, Liu YF, Ilan E, Ronen D, Boura-Halfon S, Zick Y. Common inhibitory serine sites phosphorylated by IRS-1 kinases, triggered by insulin and inducers of insulin resistance. J Biol Chem. 2007;282:18018–18027. doi: 10.1074/jbc.M610949200. [DOI] [PubMed] [Google Scholar]
- 46.Boura-Halfon S, Shuster-Meiseles T, Beck A, et al. A novel domain mediates insulin-induced proteasomal degradation of insulin receptor substrate 1 (IRS-1). Mol Endocrinol. 2010;24:2179–2192. doi: 10.1210/me.2010-0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Clark SF, Molero JC, James DE. release of insulin receptor substrate proteins from an intracellular complex coincides with the development of insulin resistance. J Biol Chem. 2000;275:3819–3826. doi: 10.1074/jbc.275.6.3819. [DOI] [PubMed] [Google Scholar]
- 48.Takano A, Usui I, Haruta T, et al. Mammalian target of rapamycin pathway regulates insulin signaling via subcellular redistribution of insulin receptor substrate 1 and integrates nutritional signals and metabolic signals of insulin. Mol Cell Biol. 2001;21:5050–5062. doi: 10.1128/MCB.21.15.5050-5062.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Harrington LS, Findlay GM, Gray A, et al. The TSC1-2 tumor suppressor controls insulin-PI3K signaling via regulation of IRS proteins. J Cell Biol. 2004;166:213–223. doi: 10.1083/jcb.200403069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shah OJ, Wang Z, Hunter T. Inappropriate activation of the TSC/Rheb/mTOR/S6K cassette induces IRS1/2 depletion, insulin resistance, and cell survival deficiencies. Curr Biol. 2004;14:1650–1656. doi: 10.1016/j.cub.2004.08.026. [DOI] [PubMed] [Google Scholar]
- 51.Shah OJ, Hunter T. Turnover of the active fraction of IRS1 involves raptor-mTOR- and S6K1-dependent serine phosphorylation in cell culture models of tuberous sclerosis. Mol Cell Biol. 2006;26:6425–6434. doi: 10.1128/MCB.01254-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Greene MW, Sakaue H, Wang L, Alessi DR, Roth RA. Modulation of insulin-stimulated degradation of human insulin receptor substrate-1 by serine 312 phosphorylation. J Biol Chem. 2003;278:8199–8211. doi: 10.1074/jbc.M209153200. [DOI] [PubMed] [Google Scholar]
- 53.Tzatsos A, Kandror KV. Nutrients suppress phosphatidylinositol 3-kinase/Akt signaling via raptor-dependent mTOR-mediated insulin receptor substrate 1 phosphorylation. Mol Cell Biol. 2006;26:63–76. doi: 10.1128/MCB.26.1.63-76.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tzatsos A. Raptor binds the SAIN (Shc and IRS-1 NPXY binding) domain of insulin receptor substrate-1 (IRS-1) and regulates the phosphorylation of IRS-1 at Ser-636/639 by mTOR. J Biol Chem. 2009;284:22525–22534. doi: 10.1074/jbc.M109.027748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhang J, Gao Z, Yin J, Quon MJ, Ye J. S6K directly phosphorylates IRS-1 on Ser-270 to promote insulin resistance in response to TNF-α signaling through IKK2. J Biol Chem. 2008;283:35375–35382. doi: 10.1074/jbc.M806480200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tremblay F, Brule S, Hee US, et al. Identification of IRS-1 Ser-1101 as a target of S6K1 in nutrient- and obesity-induced insulin resistance. Proc Natl Acad Sci U S A. 2007;104:14056–14061. doi: 10.1073/pnas.0706517104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Luo J, Field SJ, Lee JY, Engelman JA, Cantley LC. The p85 regulatory subunit of phosphoinositide 3-kinase down-regulates IRS-1 signaling via the formation of a sequestration complex. J Cell Biol. 2005;170:455–464. doi: 10.1083/jcb.200503088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Giraud J, Haas M, Feener EP, et al. Phosphorylation of Irs1 at SER-522 inhibits insulin signaling. Mol Endocrinol. 2007;21:2294–2302. doi: 10.1210/me.2007-0159. [DOI] [PubMed] [Google Scholar]
- 59.Yi Z, Langlais P, De Filippis EA, et al. Global assessment of regulation of phosphorylation of insulin receptor substrate-1 by insulin in vivo in human muscle. Diabetes. 2007;56:1508–1516. doi: 10.2337/db06-1355. [DOI] [PubMed] [Google Scholar]
- 60.Langlais P, Yi Z, Finlayson J, et al. Global IRS-1 phosphor-ylation analysis in insulin resistance. Diabetologia. 2011;54:2878–2889. doi: 10.1007/s00125-011-2271-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Prudente S, Morini E, Trischitta V. Insulin signaling regulating genes: effect on T2DM and cardiovascular risk. Nat Rev Endocrinol. 2009;5:682–693. doi: 10.1038/nrendo.2009.215. [DOI] [PubMed] [Google Scholar]
- 62.McGettrick AJ, Feener EP, Kahn CR. Human insulin receptor substrate-1 (IRS-1) polymorphism G972R causes IRS-1 to associate with the insulin receptor and inhibit receptor autophosphorylation. J Biol Chem. 2005;280:6441–6446. doi: 10.1074/jbc.M412300200. [DOI] [PubMed] [Google Scholar]
- 63.Klein AL, Berkaw MN, Buse MG, Ball LE. O-linked N-acetylglucosamine modification of insulin receptor substrate-1 occurs in close proximity to multiple SH2 domain binding motifs. Mol Cell Proteomics. 2009;8:2733–2745. doi: 10.1074/mcp.M900207-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Whelan SA, Dias WB, Thiruneelakantapillai L, Lane MD, Hart GW. Regulation of insulin receptor substrate 1 (IRS-1)/AKT kinase-mediated insulin signaling by O-linked β-N-acetylglucosamine in 3 T3-L1 adipocytes. J Biol Chem. 2010;285:5204–5211. doi: 10.1074/jbc.M109.077818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Li Y, Soos TJ, Li X, et al. Protein kinase C θ inhibits insulin signaling by phosphorylating IRS1 at Ser1101. J Biol Chem. 2004;279:45304–45307. doi: 10.1074/jbc.C400186200. [DOI] [PubMed] [Google Scholar]
- 66.Xu X, Sarikas A, as-Santagata DC, et al. The CUL7 E3 ubiquitin ligase targets insulin receptor substrate 1 for ubiquitin-dependent degradation. Mol Cell. 2008;30:403–414. doi: 10.1016/j.molcel.2008.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lu XM, Hamrahi VF, Tompkins RG, Fischman AJ. Effect of insulin levels on the phosphorylation of specific amino acid residues in IRS-1: implications for burn-induced insulin resistance. Int J Mol Med. 2009;24:531–538. doi: 10.3892/ijmm_00000262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kubota N, Tobe K, Terauchi Y, et al. Disruption of insulin receptor substrate 2 causes type 2 diabetes because of liver insulin resistance and lack of compensatory beta-cell hyperplasia. Diabetes. 2000;49:1880–1889. doi: 10.2337/diabetes.49.11.1880. [DOI] [PubMed] [Google Scholar]
- 69.Inoue G, Cheatham B, Emkey R, Kahn CR. Dynamics of insulin signaling in 3 T3-L1 adipocytes: Differential compartmentalization and trafficking of insulin receptor substrate (IRS)-1 and IRS-2. J Biol Chem. 1998;273:11548–11555. doi: 10.1074/jbc.273.19.11548. [DOI] [PubMed] [Google Scholar]
- 70.Weigert C, Kron M, Kalbacher H, et al. Interplay and effects of temporal changes in the phosphorylation state of serine-302, -307, and -318 of insulin receptor substrate-1 on insulin action in skeletal muscle cells. Mol Endocrinol. 2008;22:2729–2740. doi: 10.1210/me.2008-0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Furukawa N, Ongusaha P, Jahng WJ, et al. Role of Rho-kinase in regulation of insulin action and glucose homeostasis. Cell Metab. 2005;2:119–129. doi: 10.1016/j.cmet.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 72.Lee DH, Shi J, Jeoung NH, et al. Targeted disruption of ROCK1 causes insulin resistance in vivo. J Biol Chem. 2009;284:11776–11780. doi: 10.1074/jbc.C900014200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Giraud J, Leshan R, Lee YH, White MF. Nutrient-dependent and insulin-stimulated phosphorylation of insulin receptor substrate-1 on serine 302 correlates with increased insulin signaling. J Biol Chem. 2004;279:3447–3454. doi: 10.1074/jbc.M308631200. [DOI] [PubMed] [Google Scholar]
- 74.Samuel VT, Petersen KF, Shulman GI. Lipid-induced insulin resistance: unravelling the mechanism. Lancet. 2010;375:2267–2277. doi: 10.1016/S0140-6736(10)60408-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Petersen KF, Dufour S, Savage DB, et al. The role of skeletal muscle insulin resistance in the pathogenesis of the metabolic syndrome. Proc Natl Acad Sci U S A. 2007;104:12587–12594. doi: 10.1073/pnas.0705408104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rabol R, Petersen KF, Dufour S, Flannery C, Shulman GI. Reversal of muscle insulin resistance with exercise reduces postprandial hepatic de novo lipogenesis in insulin resistant individuals. Proc Natl Acad Sci U S A. 2011;108:13705–13709. doi: 10.1073/pnas.1110105108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rothman DL, Magnusson I, Cline G, et al. Decreased muscle glucose transport/phosphorylation is an early defect in the pathogenesis of non-insulin-dependent diabetes mellitus. Proc Natl Acad Sci U S A. 1995;92:983–987. doi: 10.1073/pnas.92.4.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Brown MS, Goldstein JL. Selective versus total insulin resistance: a pathogenic paradox. Cell Metab. 2008;7:95–96. doi: 10.1016/j.cmet.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 79.Schenk S, Saberi M, Olefsky JM. Insulin sensitivity: modulation by nutrients and inflammation. J Clin Invest. 2008;118:2992–3002. doi: 10.1172/JCI34260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pratipanawatr W, Pratipanawatr T, Cusi K, et al. Skeletal muscle insulin resistance in normoglycemic subjects with a strong family history of type 2 diabetes is associated with decreased insulin-stimulated insulin receptor substrate-1 tyrosine phosphorylation. Diabetes. 2001;50:2572–2578. doi: 10.2337/diabetes.50.11.2572. [DOI] [PubMed] [Google Scholar]
- 81.Storgaard H, Song XM, Jensen CB, et al. Insulin signal transduction in skeletal muscle from glucose-intolerant relatives of type 2 diabetic patients [corrected]. Diabetes. 2001;50:2770–2778. doi: 10.2337/diabetes.50.12.2770. [DOI] [PubMed] [Google Scholar]
- 82.Frojdo S, Vidal H, Pirola L. Alterations of insulin signaling in type 2 diabetes: a review of the current evidence from humans. Biochim Biophys Acta. 2009;1792:83–92. doi: 10.1016/j.bbadis.2008.10.019. [DOI] [PubMed] [Google Scholar]
- 83.Beeson M, Sajan MP, Dizon M, et al. Activation of protein kinase C-zeta by insulin and phosphatidylinositol-3,4,5-(PO4)3 is defective in muscle in type 2 diabetes and impaired glucose tolerance: amelioration by rosiglitazone and exercise. Diabetes. 2003;52:1926–1934. doi: 10.2337/diabetes.52.8.1926. [DOI] [PubMed] [Google Scholar]
- 84.Karlsson HK, Ahlsen M, Zierath JR, Wallberg-Henriksson H, Koistinen HA. Insulin signaling and glucose transport in skeletal muscle from first-degree relatives of type 2 diabetic patients. Diabetes. 2006;55:1283–1288. doi: 10.2337/db05-0853. [DOI] [PubMed] [Google Scholar]
- 85.Morino K, Petersen KF, Dufour S, et al. Reduced mitochondrial density and increased IRS-1 serine phosphorylation in muscle of insulin-resistant offspring of type 2 diabetic parents. J Clin Invest. 2005;115:3587–3593. doi: 10.1172/JCI25151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cusi K, Maezono K, Osman A, et al. Insulin resistance differentially affects the PI 3-kinase- and MAP kinase-mediated signaling in human muscle. J Clin Invest. 2000;105:311–320. doi: 10.1172/JCI7535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bandyopadhyay GK, Yu JG, Ofrecio J, Olefsky JM. Increased p85/55/50 expression and decreased phosphotidylinositol 3-kinase activity in insulin-resistant human skeletal muscle. Diabetes. 2005;54:2351–2359. doi: 10.2337/diabetes.54.8.2351. [DOI] [PubMed] [Google Scholar]
- 88.Chun KH, Choi KD, Lee DH, et al. In vivo activation of ROCK1 by insulin is impaired in skeletal muscle of humans with type 2 diabetes. Am J Physiol Endocrinol Metab. 2011;300:E536–E542. doi: 10.1152/ajpendo.00538.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Cipolletta E, Campanile A, Santulli G, et al. The G protein coupled receptor kinase 2 plays an essential role in beta-adrenergic receptor-induced insulin resistance. Cardiovasc Res. 2009;84:407–415. doi: 10.1093/cvr/cvp252. [DOI] [PubMed] [Google Scholar]
- 90.Garcia-Guerra L, Nieto-Vazquez I, Vila-Bedmar R, et al. G protein-coupled receptor kinase 2 plays a relevant role in insulin resistance and obesity. Diabetes. 2010;59:2407–2417. doi: 10.2337/db10-0771. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 91.Bouzakri K, Roques M, Gual P, et al. Reduced activation of phosphatidylinositol-3 kinase and increased serine 636 phosphor-ylation of insulin receptor substrate-1 in primary culture of skeletal muscle cells from patients with type 2 diabetes. Diabetes. 2003;52:1319–1325. doi: 10.2337/diabetes.52.6.1319. [DOI] [PubMed] [Google Scholar]
- 92.Fritsche L, Neukamm SS, Lehmann R, et al. Insulin-induced serine phosphorylation of IRS-2 via ERK1/2 and mTOR: studies on the function of Ser675 and Ser907. Am J Physiol Endocrinol Metab. 2011;300:E824–E836. doi: 10.1152/ajpendo.00409.2010. [DOI] [PubMed] [Google Scholar]
- 93.Farese RV, Sajan MP. Metabolic functions of atypical protein kinase C: “good” and “bad” as defined by nutritional status. Am J Physiol Endocrinol Metab. 2010;298:E385–E394. doi: 10.1152/ajpendo.00608.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Turban S, Hajduch E. Protein kinase C isoforms: mediators of reactive lipid metabolites in the development of insulin resistance. Growth Regul. 2011;585:269–274. doi: 10.1016/j.febslet.2010.12.022. [DOI] [PubMed] [Google Scholar]
- 95.Liu YF, Paz K, Herschkovitz A, et al. Insulin stimulates PKCzeta -mediated phosphorylation of insulin receptor substrate-1 (IRS-1). A self-attenuated mechanism to negatively regulate the function of IRS proteins. J Biol Chem. 2001;276:14459–14465. doi: 10.1074/jbc.M007281200. [DOI] [PubMed] [Google Scholar]
- 96.Ravichandran LV, Esposito DL, Chen J, Quon MJ. Protein kinase C-ζ phosphorylates insulin receptor substrate-1 and impairs its ability to activate phosphatidylinositol 3-kinase in response to insulin. J Biol Chem. 2001;276:3543–3549. doi: 10.1074/jbc.M007231200. [DOI] [PubMed] [Google Scholar]
- 97.Moeschel K, Beck A, Weigert C, et al. Protein kinase C-ζ-induced phosphorylation of Ser318 in insulin receptor substrate-1 (IRS-1) attenuates the interaction with the insulin receptor and the tyrosine phosphorylation of IRS-1. J Biol Chem. 2004;279:25157–25163. doi: 10.1074/jbc.M402477200. [DOI] [PubMed] [Google Scholar]
- 98.Sommerfeld MR, Metzger S, Stosik M, Tennagels N, Eckel J. In vitro phosphorylation of insulin receptor substrate 1 by protein kinase C-zeta: functional analysis and identification of novel phosphorylation sites. Biochemistry. 2004;43:5888–5901. doi: 10.1021/bi049640v. [DOI] [PubMed] [Google Scholar]
- 99.Weigert C, Hennige AM, Lehmann R, et al. Direct cross-talk of interleukin-6 and insulin signal transduction via insulin receptor substrate-1 in skeletal muscle cells. J Biol Chem. 2006;281:7060–7067. doi: 10.1074/jbc.M509782200. [DOI] [PubMed] [Google Scholar]
- 100.Hennige AM, Stefan N, Kapp K, et al. Leptin down-regulates insulin action through phosphorylation of serine-318 in insulin receptor substrate 1. FASEB J. 2006;20:1206–1208. doi: 10.1096/fj.05-4635fje. [DOI] [PubMed] [Google Scholar]
- 101.Weigert C, Hennige AM, Brischmann T, et al. The phosphorylation of Ser318 of insulin receptor substrate 1 is not per se inhibitory in skeletal muscle cells but is necessary to trigger the attenuation of the insulin-stimulated signal. J Biol Chem. 2005;280:37393–37399. doi: 10.1074/jbc.M506134200. [DOI] [PubMed] [Google Scholar]
- 102.Mussig K, Fiedler H, Staiger H, et al. Insulin-induced stimulation of JNK and the PI 3-kinase/mTOR pathway leads to phosphorylation of serine 318 of IRS-1 in C2C12 myotubes. Biochem Biophys Res Commun. 2005;335:819–825. doi: 10.1016/j.bbrc.2005.07.154. [DOI] [PubMed] [Google Scholar]
- 103.del Rincon SV, Guo Q, Morelli C, Shiu HY, Surmacz E, Miller WH. Retinoic acid mediates degradation of IRS-1 by the ubiquitin-proteasome pathway, via a PKC-dependent mechanism. Oncogene. 2004;23:9269–9279. doi: 10.1038/sj.onc.1208104. [DOI] [PubMed] [Google Scholar]
- 104.Paz K, Liu YF, Shorer H, et al. Phosphorylation of insulin receptor substrate-1 (IRS-1) by protein kinase B positively regulates IRS-1 function. J Biol Chem. 1999;274:28816–28822. doi: 10.1074/jbc.274.40.28816. [DOI] [PubMed] [Google Scholar]
- 105.Gao Z, Zuberi A, Quon MJ, Dong Z, Ye J. Aspirin inhibits serine phosphorylation of insulin receptor substrate 1 in tumor necrosis factor-treated cells through targeting multiple serine kinases. J Biol Chem. 2003;278:24944–24950. doi: 10.1074/jbc.M300423200. [DOI] [PubMed] [Google Scholar]
- 106.Um SH, Frigerio F, Watanabe M, et al. Absence of S6K1 protects against age- and diet-induced obesity while enhancing insulin sensitivity. Nature. 2004;431:200–205. doi: 10.1038/nature02866. [DOI] [PubMed] [Google Scholar]
- 107.Howell JJ, Manning BD. mTOR couples cellular nutrient sensing to organismal metabolic homeostasis. Trends Endocrinol Metab. 2011;22:94–102. doi: 10.1016/j.tem.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Patti ME, Brambilla E, Luzi L, Landaker EJ, Kahn CR. Bidirectional modulation of insulin action by amino acids. J Clin Invest. 1998;101:1519–1529. doi: 10.1172/JCI1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Li S, Brown MS, Goldstein JL. Bifurcation of insulin signaling pathway in rat liver: mTORC1 required for stimulation of lipogenesis, but not inhibition of gluconeogenesis. Proc Natl Acad Sci U S A. 2010;107:3441–3446. doi: 10.1073/pnas.0914798107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Um SH, D'Alessio D, Thomas G. Nutrient overload, insulin resistance, and ribosomal protein S6 kinase 1, S6K1. Cell Metab. 2006;3:393–402. doi: 10.1016/j.cmet.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 111.Newgard CB, An J, Bain JR, et al. A branched-chain amino acid-related metabolic signature that differentiates obese and lean humans and contributes to insulin resistance. Cell Metab. 2009;9:311–326. doi: 10.1016/j.cmet.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Macotela Y, Emanuelli B, Bang AM, et al. Dietary leucine —an environmental modifier of insulin resistance acting on multiple levels of metabolism. PLoS One. 2011;6:e21187. doi: 10.1371/journal.pone.0021187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Tremblay F, Krebs M, Dombrowski L, et al. Overactivation of S6 kinase 1 as a cause of human insulin resistance during increased amino acid availability. Diabetes. 2005;54:2674–2684. doi: 10.2337/diabetes.54.9.2674. [DOI] [PubMed] [Google Scholar]
- 114.Krebs M, Brunmair B, Brehm A, et al. The mammalian target of rapamycin pathway regulates nutrient-sensitive glucose uptake in man. Diabetes. 2007;56:1600–1607. doi: 10.2337/db06-1016. [DOI] [PubMed] [Google Scholar]
- 115.Khamzina L, Veilleux A, Bergeron S, Marette A. Increased activation of the mammalian target of rapamycin pathway in liver and skeletal muscle of obese rats: possible involvement in obesity-linked insulin resistance. Endocrinology. 2005;146:1473–1481. doi: 10.1210/en.2004-0921. [DOI] [PubMed] [Google Scholar]
- 116.Ost A, Svensson K, Ruishalme I, et al. Attenuated mTOR signaling and enhanced autophagy in adipocytes from obese patients with type 2 diabetes. Mol Med. 2010;16:235–246. doi: 10.2119/molmed.2010.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Danielsson A, Ost A, Nystrom FH, Stralfors P. Attenuation of insulin-stimulated insulin receptor substrate-1 serine 307 phosphorylation in insulin resistance of type 2 diabetes. J Biol Chem. 2005;280:34389–34392. doi: 10.1074/jbc.C500230200. [DOI] [PubMed] [Google Scholar]
- 118.Lee DF, Kuo HP, Chen CT, et al. IKKβ suppression of TSC1 function links the mTOR pathway with insulin resistance. Int J Mol Med. 2008;22:633–638. doi: 10.3892/ijmm_00000065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Danielsson A, Fagerholm S, Ost A, et al. Short-term overeating induces insulin resistance in fat cells in lean human subjects. Mol Med. 2009;15:228–234. doi: 10.2119/molmed.2009.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ryden M, Arvidsson E, Blomqvist L, Perbeck L, Dicker A, Arner P. Targets for TNF-α-induced lipolysis in human adipocytes. Biochem Biophys Res Commun. 2004;318:168–175. doi: 10.1016/j.bbrc.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 121.Greenberg AS, Shen WJ, Muliro K, et al. Stimulation of lipolysis and hormone-sensitive lipase via the extracellular signal-regulated kinase pathway. J Biol Chem. 2001;276:45456–45461. doi: 10.1074/jbc.M104436200. [DOI] [PubMed] [Google Scholar]
- 122.Bard-Chapeau EA, Hevener AL, Long S, Zhang EE, Olefsky JM, Feng GS. Deletion of Gab1 in the liver leads to enhanced glucose tolerance and improved hepatic insulin action. Nat Med. 2005;11:567–571. doi: 10.1038/nm1227. [DOI] [PubMed] [Google Scholar]
- 123.Liu X, Liu M, Zhang J, et al. Downregulation of Grb2 contributes to the insulin-sensitizing effect of calorie restriction. Am J Physiol Endocrinol Metab. 2009;296:E1067–E1075. doi: 10.1152/ajpendo.90714.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Andreozzi F, Laratta E, Sciacqua A, Perticone F, Sesti G. Angiotensin II impairs the insulin signaling pathway promoting production of nitric oxide by inducing phosphorylation of insulin receptor substrate-1 on Ser312 and Ser616 in human umbilical vein endothelial cells. Circ Res. 2004;94:1211–1218. doi: 10.1161/01.RES.0000126501.34994.96. [DOI] [PubMed] [Google Scholar]
- 125.Begum N, Sandu OA, Ito M, Lohmann SM, Smolenski A. Active Rho kinase (ROK-α) associates with insulin receptor substrate-1 and inhibits insulin signaling in vascular smooth muscle cells. J Biol Chem. 2002;277:6214–6222. doi: 10.1074/jbc.M110508200. [DOI] [PubMed] [Google Scholar]
- 126.Usui I, Imamura T, Babendure JL, et al. G protein-coupled receptor kinase 2 mediates endothelin-1-induced insulin resistance via the inhibition of both Gαq/11 and insulin receptor substrate-1 pathways in 3 T3-L1 adipocytes. Mol Endocrinol. 2005;19:2760–2768. doi: 10.1210/me.2004-0429. [DOI] [PubMed] [Google Scholar]
- 127.Usui I, Imamura T, Satoh H, et al. GRK2 is an endogenous protein inhibitor of the insulin signaling pathway for glucose transport stimulation. EMBO J. 2004;23:2821–2829. doi: 10.1038/sj.emboj.7600297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Takahashi K, Ghatei MA, Lam HC, O'Halloran DJ, Bloom SR. Elevated plasma endothelin in patients with diabetes mellitus. Diabetologia. 1990;33:306–310. doi: 10.1007/BF00403325. [DOI] [PubMed] [Google Scholar]
- 129.Kohno M, Yasunari K, Murakawa K, et al. Plasma immunoreactive endothelin in essential hypertension. Am J Med. 1990;88:614–618. doi: 10.1016/0002-9343(90)90527-k. [DOI] [PubMed] [Google Scholar]
- 130.Yatabe MS, Yatabe J, Yoneda M, et al. Salt sensitivity is associated with insulin resistance, sympathetic overactivity, and decreased suppression of circulating renin activity in lean patients with essential hypertension. Am J Clin Nutr. 2010;92:77–82. doi: 10.3945/ajcn.2009.29028. [DOI] [PubMed] [Google Scholar]
- 131.Deibert DC, DeFronzo RA. Epinephrine-induced insulin resistance in man. J Clin Invest. 1980;65:717–721. doi: 10.1172/JCI109718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Cho MC, Rao M, Koch WJ, Thomas SA, Palmiter RD, Rockman HA. Enhanced contractility and decreased β-adrenergic receptor kinase-1 in mice lacking endogenous norepinephrine and epinephrine. Cirulation. 1999;99:2702–2707. doi: 10.1161/01.cir.99.20.2702. [DOI] [PubMed] [Google Scholar]
- 133.Salcedo A, Mayor F, Jr, Penela P. Mdm2 is involved in the ubiquitination and degradation of G-protein-coupled receptor kinase. 2. EMBO J. 2006;25:4752–4762. doi: 10.1038/sj.emboj.7601351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Samuelsson AM, Bollano E, Mobini R, et al. Hyperinsulinemia: effect on cardiac mass/function, angiotensin II receptor expression, and insulin signaling pathways. Am J Physiol Heart Circ Physiol. 2006;291:H787–H796. doi: 10.1152/ajpheart.00974.2005. [DOI] [PubMed] [Google Scholar]
- 135.Imamura T, Vollenweider P, Egawa K, et al. G alpha-q/11 protein plays a key role in insulin-induced glucose transport in 3 T3-L1 adipocytes. Mol Cell Biol. 1999;19:6765–6774. doi: 10.1128/mcb.19.10.6765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Shahid G, Hussain T. GRK2 negatively regulates glycogen synthesis in mouse liver FL83B cells. J Biol Chem. 2007;282:20612–20620. doi: 10.1074/jbc.M700744200. [DOI] [PubMed] [Google Scholar]
- 137.Anis Y, Leshem O, Reuveni H, et al. Antidiabetic effect of novel modulating peptides of G-protein-coupled kinase in experimental models of diabetes. Diabetologia. 2004;47:1232–1244. doi: 10.1007/s00125-004-1444-1. [DOI] [PubMed] [Google Scholar]
- 138.Greene MW, Garofalo RS. Positive and negative regulatory role of insulin receptor substrate 1 and 2 (IRS-1 and IRS-2) serine/ threonine phosphorylation. Biochemistry. 2002;41:7082–7091. doi: 10.1021/bi015992f. [DOI] [PubMed] [Google Scholar]
- 139.Liberman Z, Eldar-Finkelman H. Serine 332 phosphorylation of insulin receptor substrate-1 by glycogen synthase kinase-3 attenuates insulin signaling. J Biol Chem. 2005;280:4422–4428. doi: 10.1074/jbc.M410610200. [DOI] [PubMed] [Google Scholar]
- 140.McManus EJ, Sakamoto K, Armit LJ, et al. Role that phosphorylation of GSK3 plays in insulin and Wnt signalling defined by knockin analysis. EMBO J. 2005;24:1571–1583. doi: 10.1038/sj.emboj.7600633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Tzatsos A, Tsichlis PN. Energy depletion inhibits phosphatidylinositol 3-kinase/Akt signaling and induces apoptosis via AMP-activated protein kinase-dependent phosphorylation of IRS-1 at Ser-794. J Biol Chem. 2007;282:18069–18082. doi: 10.1074/jbc.M610101200. [DOI] [PubMed] [Google Scholar]
- 142.Qiao LY, Zhande R, Jetton TL, Zhou G, Sun XJ. In vivo phosphorylation of IRS-1 at Serine789 by a novel serine kinase in insulin resistant rodents. J Biol Chem. 2002;277:26530–26539. doi: 10.1074/jbc.M201494200. [DOI] [PubMed] [Google Scholar]
- 143.Horike N, Takemori H, Katoh Y, et al. Adipose-specific expression, phosphorylation of Ser794 in insulin receptor substrate-1, and activation in diabetic animals of salt-inducible kinase-2. J Biol Chem. 2003;278:18440–18447. doi: 10.1074/jbc.M211770200. [DOI] [PubMed] [Google Scholar]
- 144.Dentin R, Liu Y, Koo SH, et al. Insulin modulates gluconeogenesis by inhibition of the coactivator TORC2. Nature. 2007;449:366–369. doi: 10.1038/nature06128. [DOI] [PubMed] [Google Scholar]
- 145.Jakobsen SN, Hardie DG, Morrice N, Tornqvist HE. 5′-AMP-activated protein kinase phosphorylates IRS-1 on Ser-789 in mouse C2C12 myotubes in response to 5-aminoimidazole-4-carboxamide riboside. J Biol Chem. 2001;276:46912–46916. doi: 10.1074/jbc.C100483200. [DOI] [PubMed] [Google Scholar]
- 146.Yu C, Chen Y, Cline GW, et al. Mechanism by which fatty acids inhibit insulin activation of insulin receptor substrate-1 (IRS-1)-associated phosphatidylinositol 3-kinase activity in muscle. J Biol Chem. 2002;277:50230–50236. doi: 10.1074/jbc.M200958200. [DOI] [PubMed] [Google Scholar]
- 147.Kim JK, Fillmore JJ, Sunshine MJ, et al. PKC-θ knockout mice are protected from fat-induced insulin resistance. J Clin Invest. 2004;114:823–827. doi: 10.1172/JCI22230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Bezy O, Tran TT, Pihlajamaki J, et al. PKCδ regulates hepatic insulin sensitivity and hepatosteatosis in mice and humans. J Clin Invest. 2011;121:2504–2517. doi: 10.1172/JCI46045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Mack E, Ziv E, Reuveni H, et al. Prevention of insulin resistance and beta-cell loss by abrogating PKCε-induced serine phosphorylation of muscle IRS-1 in Psammomys obesus. Diabetes Metab Res Rev. 2008;24:577–584. doi: 10.1002/dmrr.881. [DOI] [PubMed] [Google Scholar]
- 150.Samuel VT, Liu ZX, Wang A, et al. Inhibition of protein kinase Cε prevents hepatic insulin resistance in nonalcoholic fatty liver disease. J Clin Invest. 2007;117:739–745. doi: 10.1172/JCI30400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Itani SI, Pories WJ, MacDonald KG, Dohm GL. Increased protein kinase C theta in skeletal muscle of diabetic patients. Metabolism. 2001;50:553–557. doi: 10.1053/meta.2001.22512. [DOI] [PubMed] [Google Scholar]
- 152.Considine RV, Nyce MR, Allen LE, et al. Protein kinase C is increased in the liver of humans and rats with non-insulin-dependent diabetes mellitus: an alteration not due to hyperglycemia. J Clin Invest. 1995;95:2938–2944. doi: 10.1172/JCI118001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Griffin ME, Marcucci MJ, Cline GW, et al. Free fatty acid-induced insulin resistance is associated with activation of protein kinase C theta and alterations in the insulin signaling cascade. Diabetes. 1999;48:1270–1274. doi: 10.2337/diabetes.48.6.1270. [DOI] [PubMed] [Google Scholar]
- 154.Itani SI, Ruderman NB, Schmieder F, Boden G. Lipid-induced insulin resistance in human muscle is associated with changes in diacylglycerol, protein kinase C, and IκB-α. Diabetes. 2002;51:2005–2011. doi: 10.2337/diabetes.51.7.2005. [DOI] [PubMed] [Google Scholar]
- 155.De Fea K, Roth RA. Protein kinase C modulation of insulin receptor substrate-1 tyrosine phosphorylation requires serine. 612. Biochemistry. 1997;36:12939–12947. doi: 10.1021/bi971157f. [DOI] [PubMed] [Google Scholar]
- 156.Greene MW, Morrice N, Garofalo RS, Roth RA. Modulation of human insulin receptor substrate-1 tyrosine phosphorylation by protein kinase Cdelta. Biochem J. 2004;378:105–116. doi: 10.1042/BJ20031493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Liu YF, Herschkovitz A, Boura-Halfon S, et al. Serine phosphorylation proximal to its phosphotyrosine binding domain inhibits insulin receptor substrate 1 function and promotes insulin resistance. Mol Cell Biol. 2004;24:9668–9681. doi: 10.1128/MCB.24.21.9668-9681.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Waraich RS, Weigert C, Kalbacher H, et al. Phosphorylation of Ser357 of rat insulin receptor substrate-1 mediates adverse effects of protein kinase C-delta on insulin action in skeletal muscle cells. J Biol Chem. 2008;283:11226–11233. doi: 10.1074/jbc.M708588200. [DOI] [PubMed] [Google Scholar]
- 159.Leitges M, Plomann M, Standaert ML, et al. Knockout of PKCα enhances insulin signaling through PI3K. Mol Endocrinol. 2002;16:847–858. doi: 10.1210/mend.16.4.0809. [DOI] [PubMed] [Google Scholar]
- 160.Cipok M, Aga-Mizrachi S, Bak A, et al. Protein kinase Cα regulates insulin receptor signaling in skeletal muscle. Biochem Biophys Res Commun. 2006;345:817–824. doi: 10.1016/j.bbrc.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 161.Oriente F, Andreozzi F, Romano C, et al. Protein kinase Cα regulates insulin action and degradation by interacting with insulin receptor substrate-1 and 14-3-3ε. J Biol Chem. 2005;280:40642–40649. doi: 10.1074/jbc.M508570200. [DOI] [PubMed] [Google Scholar]
- 162.Liberman Z, Plotkin B, Tennenbaum T, Eldar-Finkelman H. Coordinated phosphorylation of insulin receptor substrate-1 by glycogen synthase kinase-3 and protein kinase CβII in the diabetic fat tissue. Am J Physiol Endocrinol Metab. 2008;294:E1169–E1177. doi: 10.1152/ajpendo.00050.2008. [DOI] [PubMed] [Google Scholar]
- 163.Huang W, Bansode RR, Bal N, Mehta M, Mehta KD. Protein kinase Cβ deficiency attenuates obesity syndrome of ob/ob mice by promoting white adipose tissue remodeling. J Lipid Res. 2011;53:368–378. doi: 10.1194/jlr.M019687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Zisman A, Peroni OD, Abel ED, et al. Targeted disruption of the glucose transporter 4 selectively in muscle causes insulin resistance and glucose intolerance. Nat Med. 2000;6:924–928. doi: 10.1038/78693. [DOI] [PubMed] [Google Scholar]
- 165.Galic S, Oakhill JS, Steinberg GR. Adipose tissue as an endocrine organ. Mol Cell Endocrinol. 2010;316:129–139. doi: 10.1016/j.mce.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 166.Sabio G, Davis RJ. cJun NH2-terminal kinase 1 (JNK1): roles in metabolic regulation of insulin resistance. Trends Biochem Sci. 2010;35:490–496. doi: 10.1016/j.tibs.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Gao Z, Hwang D, Bataille F, et al. Serine phosphorylation of insulin receptor substrate 1 by inhibitor κB kinase complex. J Biol Chem. 2002;277:48115–48121. doi: 10.1074/jbc.M209459200. [DOI] [PubMed] [Google Scholar]
- 168.Nakamori Y, Emoto M, Fukuda N, et al. Myosin motor Myo1c and its receptor NEMO/IKK-γ promote TNF-α-induced serine307 phosphorylation of IRS-1. J Cell Biol. 2006;173:665–671. doi: 10.1083/jcb.200601065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Lancaster GI, Skiba B, Yang C, et al. IκB kinase β (IKKβ) does not mediate feedback inhibition of the insulin-signaling cascade. Biochem J. 2012;442:723–732. doi: 10.1042/BJ20112037. [DOI] [PubMed] [Google Scholar]
- 170.Morino K, Neschen S, Bilz S, et al. Muscle-specific IRS-1 Ser->Ala transgenic mice are protected from fat-induced insulin resistance in skeletal muscle. Diabetes. 2008;57:2644–2651. doi: 10.2337/db06-0454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Copps KD, Hancer NJ, Opare-Ado L, Qiu W, Walsh C, White MF. Irs1 serine 307 promotes insulin sensitivity in mice. Cell Metab. 2010;11:84–92. doi: 10.1016/j.cmet.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Katsnelson A. Breaking the silence. Nat Med. 2011;17:1536–1538. doi: 10.1038/nm1211-1536. [DOI] [PubMed] [Google Scholar]
- 173.White MF, Copps KD, Ozcan U, Tseng YD. The molecular basis of insulin action. In: Jameson JL, DeGroot LJ, editors. Endocrinology. 6th edn. Elsevier; Philadelphia: 2010. pp. 636–659. [Google Scholar]
- 174.Hsu PP, Kang SA, Rameseder J, et al. The mTOR-regulated phosphoproteome reveals a mechanism of mTORC1-mediated inhibition of growth factor signaling. Science. 2011;332:1317–1322. doi: 10.1126/science.1199498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Wick KR, Werner ED, Langlais P, et al. Grb10 inhibits insulin-stimulated insulin receptor substrate (IRS)-phosphatidylinositol 3-kinase/Akt signaling pathway by disrupting the association of IRS-1/IRS-2 with the insulin receptor. J Biol Chem. 2003;278:8460–8467. doi: 10.1074/jbc.M208518200. [DOI] [PubMed] [Google Scholar]
- 176.Dibble CC, Asara JM, Manning BD. Characterization of Rictor phosphorylation sites reveals direct regulation of mTOR complex 2 by S6K1. Mol Cell Biol. 2009;29:5657–5670. doi: 10.1128/MCB.00735-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Das F, Ghosh-Choudhury N, Dey N, et al. Unrestrained mammalian target of rapamycin complexes 1 and 2 increase expression of phosphatase and tensin homolog deleted on chromosome 10 to regulate phosphorylation of akt kinase. J Biol Chem. 2012;287:3808–3822. doi: 10.1074/jbc.M111.246397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Sun XJ, Crimmins DL, Myers MG, Jr, Miralpeix M, White MF. Pleiotropic insulin signals are engaged by multisite phosphorylation of IRS-1. Mol Cell Biol. 1993;13:7418–7428. doi: 10.1128/mcb.13.12.7418. [DOI] [PMC free article] [PubMed] [Google Scholar]