Abstract
Background:
A region-specific (urban and rural parts of north, east, west, and south India) systematic review and meta-analysis of the prevalence, awareness, and control of hypertension among Indian patients have not been done before.
Methods:
Medline, Web of Science, and Scopus databases from 1950 to 30 April 2013 were searched for ‘prevalence, burden, awareness, and control of blood pressure (BP) or hypertension (≥140 SBP and or ≥90 DBP) among Indian adults’ (≥18 years). Of the total 3047 articles, 142 were included.
Results:
Overall prevalence for hypertension in India was 29.8% (95% confidence interval: 26.7–33.0). Significant differences in hypertension prevalence were noted between rural and urban parts [27.6% (23.2–32.0) and 33.8% (29.7–37.8); P = 0.05]. Regional estimates for the prevalence of hypertension were as follows: 14.5% (13.3–15.7), 31.7% (30.2–33.3), 18.1% (16.9–19.2), and 21.1% (20.1–22.0) for rural north, east, west, and south India; and 28.8% (26.9–30.8), 34.5% (32.6–36.5), 35.8% (35.2–36.5), and 31.8% (30.4–33.1) for urban north, east, west, and south India, respectively. Overall estimates for the prevalence of awareness, treatment, and control of BP were 25.3% (21.4–29.3), 25.1% (17.0–33.1), and 10.7% (6.5–15.0) for rural Indians; and 42.0% (35.2–48.9), 37.6% (24.0–51.2), and 20.2% (11.6–28.7) for urban Indians.
Conclusion:
About 33% urban and 25% rural Indians are hypertensive. Of these, 25% rural and 42% urban Indians are aware of their hypertensive status. Only 25% rural and 38% of urban Indians are being treated for hypertension. One-tenth of rural and one-fifth of urban Indian hypertensive population have their BP under control.
Keywords: awareness, control, hypertension, India, meta-analysis, prevalence, systematic review
INTRODUCTION
High blood pressure (BP) is ranked as the third most important risk factor for attributable burden of disease in south Asia (2010) [1]. Hypertension (HTN) exerts a substantial public health burden on cardiovascular health status and healthcare systems in India [2,3]. HTN is directly responsible for 57% of all stroke deaths and 24% of all coronary heart disease (CHD) deaths in India [4]. The WHO rates HTN as one of the most important causes of premature death worldwide [5]. The Global and Regional Burden of Disease and Risk Factors study (2001), in a systematic analysis of population health data for attributable deaths and attributable disease burden, has ranked HTN in south Asia as second only to child underweight for age [6].
In an analysis of worldwide data for the global burden of HTN, 20.6% of Indian men and 20.9% of Indian women were suffering from HTN in 2005 [7]. The rates for HTN in percentage are projected to go up to 22.9 and 23.6 for Indian men and women, respectively by 2025 [7]. Recent studies from India have shown the prevalence of HTN to be 25% in urban and 10% in rural people in India [4,8–10]. According to the WHO 2008 estimates, the prevalence of raised BP in Indians was 32.5% (33.2% in men and 31.7% in women) [11]. However, only about 25.6% of treated patients had their BP under control, in a multicenter study from India on awareness, treatment, and adequacy of control of HTN [12].
An alarming rise in HTN projected by Global Burden of Hypertension 2005 study, [7] the GBD 2010 study [1] and WHO 2011 NCD India specific data [11] portray a grim picture for the 17.8% of the world's population who reside in India. Previously, a systematic review on the prevalence of HTN in India, for studies published between 1969 and July 2011, reported a range between 13.9 to 46.3% and 4.5 to 58.8% in urban and rural areas of India, respectively [13]. The regional variations (between urban and rural) reported in prevalence of HTN are also seen in cardiovascular diseases. Published literature reports regional variations in mortality and prevalence of CHD and stroke in India (south India has higher CHD mortality and eastern India has higher stroke rates [14]). Similar variations are also seen among urban and rural areas with CHD prevalence being higher in urban parts of India [14]. Hence, we aimed to perform a systematic review and meta-analysis to arrive at pooled estimates for region-wise prevalence of HTN among rural and urban parts of India; and awareness, treatment, and control of BP among Indian patients suffering from HTN.
METHODS
Search strategy
Between January 2013 and 30 May 2013 (last date searched), we comprehensively searched Medline (1950 to present), Embase (1950 to present), Scopus (1996 to present), and Web of knowledge (1950 to present). We used combinations of medical subject headings (MESH) and free text words that included search terms related to the exposure (e.g., BP, SBP, DBP, HTN, raised BP, and high BP), which were combined with search terms related to the outcomes (e.g., prevalence, disease burden, estimate, awareness, control). We identified articles eligible for further review by performing an initial screen of identified titles or abstracts, followed by a full-text review. Complete details on the search terms used in Medline have been included (see section A, Supplemental Digital Content).
Selection criteria and data extraction
Articles were considered for inclusion if the study was cross-sectional, case–control, or cohort; studies conducted among adult populations (≥18 years old); studies were on prevalence, burden, risk factors, awareness, and control of BP or HTN; HTN was defined as SBP more than or equal to 140 and or DBP more than or equal to 90 mmHg. Articles were excluded if they were letters, abstracts, conference proceedings, reviews, and meta-analysis; not conducted on humans; and not community-based studies.
Study selection
Two independent reviewers (RA and HP) screened the titles and abstracts of the initially identified studies to determine whether they would satisfy the selection criteria. Any disagreements about selection were resolved through consensus or consultation with a third author (NKK). Full-text articles were retrieved for the selected titles. Reference lists of the retrieved articles were searched for additional publications. We also contacted the authors of the retrieved articles directly for any additional and unpublished studies. The retrieved studies were assessed again by two independent authors (R.A. and N.K.K.) to ensure that they satisfied the inclusion criteria.
Data extraction
A data collection form was designed prior to the implementation of the search strategy. This form was used by two independent reviewers to extract the relevant information from the selected studies (R.A. and H.P.). The data collection form included questions on year of publication, design, geographic origin and setting, selection criteria, patient samplings and location of research group, participant characteristics (e.g. number of population included in the analysis, age range, mean age, sex, sample size, residential region, comorbidities, and associated risk factors), and information on the reported outcomes (e.g. measure of disease frequency, number of patients aware of being a hypertensive, percentage on hypertensive treatment, percentage of hypertensive patients having BP under control on drug treatment, type of statistical analysis, and adjustment variables).
Statistical analysis
The standard error (SE) of prevalence was calculated from the reported percentage prevalence and sample size for each of the studies. SE was calculated as √ [p × (1−p)/n], where p is the proportion of prevalence and n is the reported sample size. We assessed heterogeneity by reporting the I2 (% residual variation due to heterogeneity) and τ2 (method of moments estimate of between-study variance) for each of the pooled estimates. As the differences between trials were very large (95–99% inconsistency), a random effects model was used to pool the prevalence of HTN. Region-wise pooled estimates weighted by population size in each study place within a given region (NEWS) for prevalence of HTN were also calculated. The pooled estimate for overall prevalence of HTN in India was calculated using regional population size weights. Metareg, which performs random-effects meta-regression using aggregate-level data, was also done to assess the heterogeneity and combinability. The values of I2 and τ2 for both urban and rural areas have been mentioned in the text and shown in the supplemental digital content file. The mean percentage (%) prevalence and the 95% confidence intervals (CIs) have been reported in the pooled analysis. Freeman-Tukey transformations (variant of the arcsine square root transformed proportion) were done to stabilize the regional variances to arrive at overall prevalence of HTN in India. All analyses were done using STATA version 11.2 (StataCorp., College Station, Texas, USA). The methods used for Freeman-Tukey transformation have been described in section B of the supplemental digital content file.
RESULTS
Study selection
Overall 8647 references were initially identified in our study: 8622 from electronic databases and 25 from bibliographies and experts (Fig. 1). After removing 5553 duplicates, a total of 3094 abstracts were screened by inclusion criteria, as described in Methods. Full-text assessment of the 242 potentially relevant articles resulted in 142 eligible studies (cross-sectional – 97; cohort – six; case–control – 12; and mixed methods – 27) that were included in our review.
FIGURE 1.
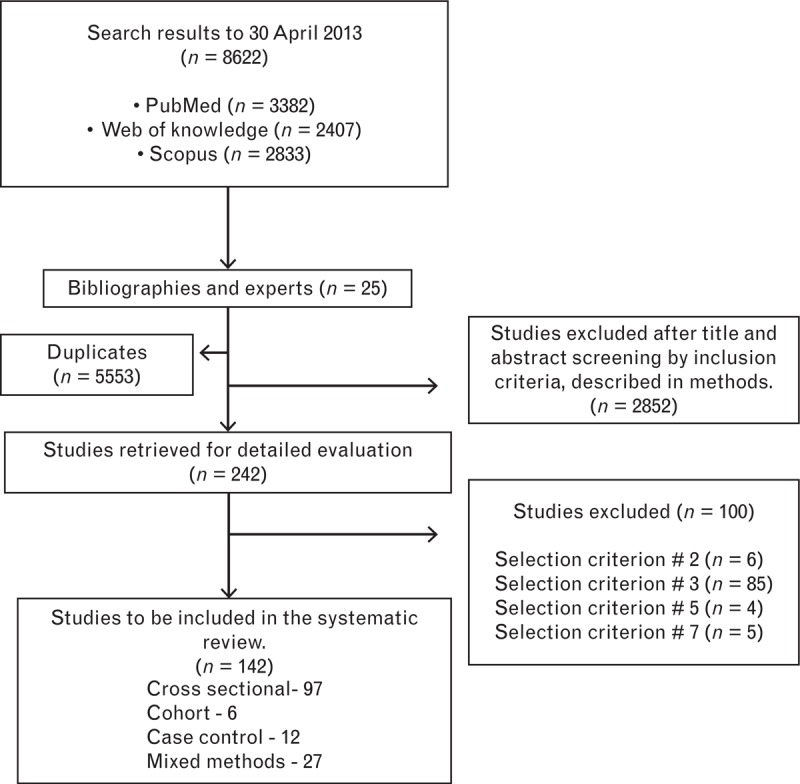
Flow diagram for selection of studies.
Characteristics of studies included
Six [15–20], eight [21–26], two [27,28], and nine [8,29–37] studies reported on the prevalence of HTN among adult Indians from rural parts of north India, east India, west India, and south India, respectively (see table S1, supplemental digital content). Four [38–41], four [10,21,39,42], 10 [27,39,43–50], and seven studies [35,39,51–56] reported on the prevalence of HTN among adult Indians from urban parts of north India, east India, west India, and south India, respectively. Data for the prevalence studies came from 7448, 18 724, 4832, and 21 964 participants from the rural parts of north, east, west, and south India, respectively, and 4415, 3199, 249 226, and 16 836 participants from the urban parts of north, east, west, and south India, respectively. Five studies were done in different regions of India, three were in urban parts [39,57,58] and two were done in both urban and rural areas of India [59,60] (see table S1, supplemental digital content). Awareness, treatment, and control of BP were reported in 14, 11, and 10 studies; and 19, 14, and 15 studies in rural and urban parts of India, respectively (see table S2, supplemental digital content).
Study quality
Strobe guidelines [61] were used to assess the quality of the selected articles. Quality scores were defined based on presence of eligibility criterion, sources and methods of selection of participants, reported numbers of outcome events or summary measures, and mentioned limitations of the study [62]. Three studies scored on all four measures, 43 studies obtained a score of 3, and 61 and 35 studies obtained scores of 2 and 1, respectively. Although quality was rated for each study, quality scores have not been incorporated in the meta-analysis weights.
Burden of hypertension in India
Overall prevalence of HTN in India, after weighting the regional population size, was 29.8% (95% CI: 26.7–33.0; I2 = 79.8%, P <0.001). After stabilizing the region-wise data using Freeman-Tukey transformations, the overall prevalence of HTN in India was 29.2% (95% CI: 25.7–35.6; I2 = 77.2%, P <0.001). Significant differences in HTN prevalence were noted between rural and urban parts of India [rural vs. urban: 27.6% (23.2–32.0; I2 = 84%, P <0.001) and 33.8% (29.7–37.8); I2 = 0%, P = 0.05]. The data on reported prevalence of HTN in India from published community-based studies, done between 2011 and 2013, have been summarized in table S1, supplemental digital content [13]. Figure 2 summarizes the rural and urban differences in HTN prevalence for each region. Figures S1–S4 in the supplemental digital content, depict the pooled prevalence of HTN, region-wise, using population size weights. Figures S5–S8 in the supplemental digital content, depict the pooled prevalence of HTN using random effects model, region-wise, without adjusting for population size. Region-specific pooled estimates (and 95% CIs) are described below.
FIGURE 2.
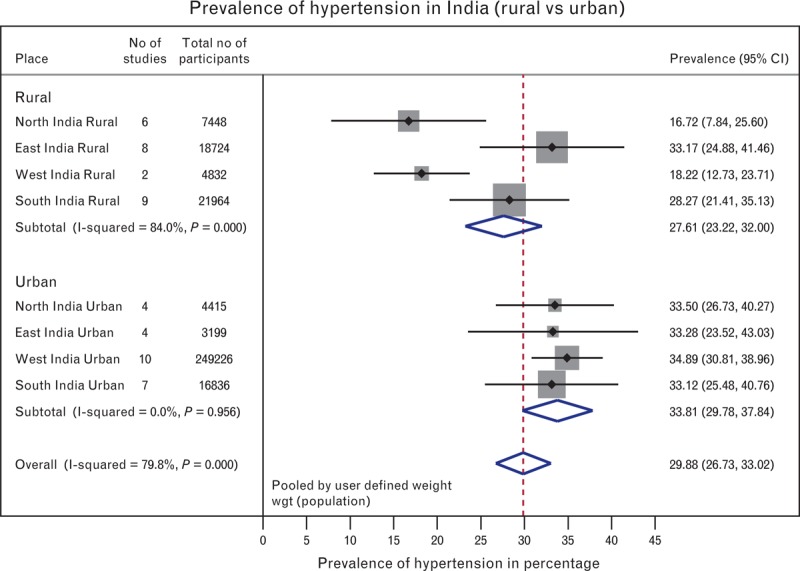
Overall pooled estimates: region-wise (north, east, west, and south) and place-wise (rural and urban). P value for overall rural and urban differences in hypertension (HTN) prevalence = 0.05∗; P value for rural and urban differences in HTN prevalence for east India = 0.98; P value for rural and urban differences in HTN prevalence for north India = 0.07; P value for rural and urban differences in HTN prevalence for south India = 0.62; P value for rural and urban differences in HTN prevalence for west India = 0.05∗. CI, confidence interval. ∗Statistically significant.
North India
The pooled prevalence of HTN for the rural and urban north Indian population was 14.5% (13.3–15.7) and 28.8% (26.9–30.8), respectively (see figure S1, supplemental digital content). Heterogeneity was significantly present in both rural and urban north India [I2 = 99.3% (95% CI: 95–100; P <0.001); I2 = 91.1% (97–99; P <0.001), respectively]. There was no significant difference between the rural and urban prevalence of HTN in north India (P value = 0.07).
East India
The pooled prevalence of HTN for the rural and urban east Indian population was 31.7% (30.2–33.3) and 34.5% (32.6–36.5), respectively (see figure S2, supplemental digital content). Heterogeneity was significantly present in both rural and urban east India [I2 = 99.3% (95% CI: 99–100; P <0.001); I2 = 97.1% (95–98; P <0.001), respectively]. There was no significant difference between the rural and urban prevalence of HTN in east India (P value = 0.98).
West India
The pooled prevalence of HTN for the rural and urban west Indian population was 18.1% (16.9–19.2) and 35.8% (35.2–36.5), respectively (see figure S3, supplemental digital content). Heterogeneity was significantly present in both rural and urban west India [I2 = 95.9% (95% CI: 70–98; P <0.001); I2 = 99.6% (97–100; P <0.001), respectively]. There was a significant difference between the rural and urban prevalence of HTN in east India (P value = 0.05).
South India
The pooled prevalence of HTN for the rural and urban south Indian population was 21.1% (20.1–22.0) and 31.8% (30.4–33.1), respectively (see figure S4, supplemental digital content). Heterogeneity was significantly present in both rural and urban south India [I2 = 99% (95% CI: 99–99; P <0.001); I2 = 99% (99–100; P <0.001), respectively]. There was no significant difference between the rural and urban prevalence of HTN in south India (P value = 0.62).
Awareness treatment and control of blood pressure
The pooled estimate for awareness of BP in rural and urban India was 25.1% (21.0–29.1) and 41.9% (35.1–48.9), respectively. The pooled estimate for the percentage of treated among those diagnosed with HTN in rural and urban areas was 24.9 (16.7–33.0) and 37.6 (23.9–51.2), respectively. The pooled estimate for percentage of hypertensive patients having their BP under control in rural and urban India was 10.7 (6.4–15.0) and 20.2 (11.6–28.8), respectively. Significant differences were noted in the rural and urban areas for awareness and control of HTN (P values of 0.002 and 0.03, respectively). No statistically significant difference was noted in the rural and urban areas for percentage treated among hypertensive patients (P = 0.112; Fig. 3). The figures S9–S11 in the supplemental digital content, portray the forest plots for percentage aware, treated, and having BP under control, respectively. Similar to HTN prevalence, significant heterogeneity was also seen in awareness, treatment, and control of BP [I2 = 99 (95% CI: 99–100; P <0.001)].
FIGURE 3.
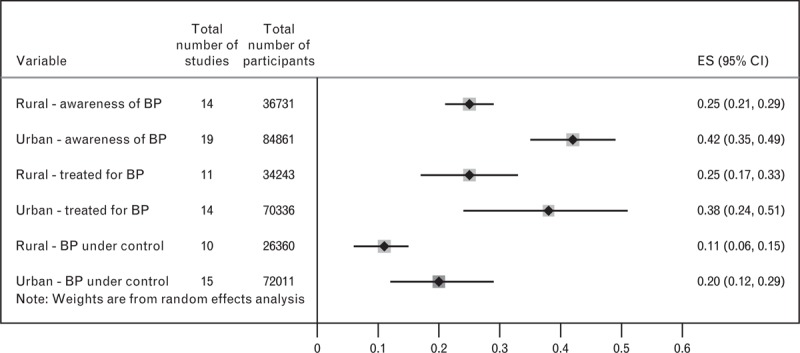
Percentage aware, treated, and under control for hypertension (HTN): urban and rural areas. P value for overall rural and urban differences in awareness of hypertension = 0.002∗; P value for rural and urban differences in HTN treatment = 0.112; P value for rural and urban differences in HTN control = 0.03∗. BP, blood pressure; CI, confidence interval; ES, pooled estimate; ∗Statistically significant.
Risk factors
Eleven studies [8,23,25,33,36,42,52,53,57,63,64] reported on the risk factors associated with HTN (see table S3, supplemental digital content). Age, alcohol, smoking and chewing tobacco, BMI, central obesity (defined as waist circumference >90 cm in men and >80 cm in women), consumption of low vegetables/fruits, high consumption of dietary fat and salt, and sedentary activity were the significant risk factors for HTN among Indian patients.
DISCUSSION
To the best of our knowledge, this is the most comprehensive systematic review on disease burden, awareness, treatment, and control of BP among rural and urban Indians done separately. Region-wise categorization into north, east, west, and south (NEWS) for both urban and rural parts of India allowed us to capture and present the significant differences among the four regions of India in this review and arrive at representative figures. Our systematic review differs in several ways from the previously published one [13] – first, it includes additional 25 studies (81 503 participants) on prevalence of HTN among adult Indians, published in the period between August 2011 to April 2013 [15,16,21–24,27,31–35,39,42,43,57–60,64–67]; and second, it provides region-specific estimates on the disease burden, awareness, treatment, and control of BP.
The majority of studies were cross-sectional (90%). Fifty percent of studies scored 3 and above (on a scale of 4) on assessing their quality based on Strobe's guidelines for observational studies. Twenty five community-based studies each from rural and urban parts of India (52 968 and 273 676 participants, respectively) reported on prevalence of HTN. Rural areas had lesser prevalence of HTN as compared with urban areas. Fewer studies and lesser sample size could be the reasons for a lower prevalence in rural northern and western parts of India. Very few studies reported age-adjusted rates for HTN among both rural and urban areas. All were community-based studies (no hospital-based studies were included). Among rural areas, eastern India had the highest prevalence equaling the prevalence seen in urban parts of India. The prevalence of HTN in urban parts of India was similar across all the four regions (NEWS). Considerable variation in prevalence of HTN (20–59%) was seen among the studies from rural east India with higher prevalence seen from Assam (owing to the indigenous prevalence of excess salt, alcohol, and Khaini consumption among tea plantation workers of Assam) [63]. A higher prevalence was also noted in Car Nicobar islands as compared with other rural southern regions. One-third of urban Indians from all the four regions of India were hypertensive.
The differences in HTN prevalence between urban and rural areas noted in our study could be explained by the differences in socioeconomic conditions, risk factors, and quality of healthcare services provided. Rural parts of India have lower rates of literacy and have wider disparity in access and quality of health services as compared with urban areas. Recent studies from India have shown that HTN is significantly more prevalent in the lower education group when compared with higher education group [68]. The higher prevalence of HTN in urban areas may have arisen as cardiovascular disease risk factors among the urban poor and middle class are rapidly increasing in India [69]. Lifestyle changes (harmful dietary practices, consumption of tobacco, and sedentary habits) occurring because of rapid urbanization and economic progress in urban areas have also contributed to the growing epidemic of HTN in urban areas of India. Higher rates of salty food consumption in eastern India [63] owing to presence of humid conditions, and presence of cardiometabolic risk factors in southern India (such as central obesity and high BMI) [70] may have been the contributing factors for high prevalence of HTN in both urban and rural parts of east and south India.
Increase in HTN with advancing age was shown by six studies [22,23,33,36,52,63]. We noticed close to a two-fold increase in risk for HTN among Indians when they smoked [8,33,52], orally consumed khaini and tobacco [63], had extra salt intake in their food [63], had a sedentary lifestyle [64], were centrally obese [8,33,42,52,57], had BMI at least 25 [8,23,36,52,57], and consumed alcohol [22,36,63,64]. The awareness levels for HTN in rural parts of India ranged from a low of 12% in Car Nicobar islands [36] to a high of 43% in Kerala [35]. Awareness was above 20% in almost all rural studies except one study [36].
The awareness levels for HTN were consistently above 35% in almost all studies from urban areas. The treated percentage among hypertensive patients showed a great variation in rural southern parts of India, ranging from 0.01% [36] to a high of 47% [17]. Similar variation was also found in urban parts of India for percentage treated for HTN (a low of 18.70% [54] to a high of 80% [21]). However, the small sample size in the study that recorded an 80% treatment rate among hypertensive patients limits the significance of the finding. Overall, close to 38% of urban Indians suffering from HTN are being treated. The BP control among both urban and rural parts of India has been very poor (range of 6.5–15% in rural and 11.6–28.7% in urban). These findings have enormous public health significance for policy makers and physicians alike. The low awareness and treatment levels among hypertensive patients signify a lower knowledge, attitude, and practice levels among patients. Current strategies to control BP among Indian hypertensive patients are not working because less than one fifth of hypertensive patients have their BP under control even in urban areas. Rural hypertensive patients on treatment have even further lower rates, with only a tenth of them having BP under control.
Limitations
There are limitations to our study. First, to summarize and arrive at a common figure for 18% of the world's population having vast variations in geographic, dietary, and cultural practices is difficult owing to the inherent heterogeneity. We attempted to overcome this limitation by dividing India along geographic areas into north, east, west and south India and arriving at region-specific rates. However, the cultural and dietary practices vary state-wise and this may have a bearing on the results. The proportion of variability in a meta-analysis that is explained by differences between the included studies rather than by sampling error (I2) was significant across all urban and rural areas for HTN prevalence, awareness, treatment, and control of BP (I2 above 95%; P <0.001 for all regions). It has been documented that large differences in sample sizes between the included articles, and inclusion of a fewer number of studies produce a pooled estimate that has low power and precision, thereby producing a higher Cochran Q (heterogeneity χ2 test statistic) and a higher I2[71]. The sample size in the included studies ranged from a few hundreds to few thousands in each study and in each region. The number of studies too has been less than eight in most urban and rural regions. Time-dependent biases (time lag, and publication bias – see figure S12, supplemental digital file) [71] and differential presence of risk factors (age, smoking, physical activity and salt intake), both of which were present in the selected studies, have also been known to influence heterogeneity. Unfortunately, because of insufficient data in most of the published studies, it was not possible to perform a subgroup analysis and deduce the effect of these variations on the pooled prevalence of HTN. Future studies using alternative approaches such as disease mapping, Bayesian, and hierarchical modeling techniques can better discriminate and explore the regional differences that have been shown in our study.
Second, there was a paucity of studies that reported on awareness and control of BP from all over India. Hence, it was not feasible to generate region-wise data for awareness and control of BP. However, because 10 studies were from urban and rural areas each, we estimated the pooled percentage aware, treated, and controlled for BP among Indians. Third, only 50% of studies mentioned at least three out of the four criteria for quality assessment (eligibility criterion, sources and methods of selection of participants, reported numbers of outcome events or summary measures and limitations). Finally, the differences in the age range (20–70 years) in the included studies may have a bearing on the prevalence of HTN as increasing age has shown a consistent positive correlation with prevalence of HTN in many studies.
In conclusion, one-third of urban adult Indians and close to one fourth of rural adult Indians are hypertensive. Regional differences exist in rural areas of India for prevalence of HTN. Urban areas of India show no significant differences in HTN prevalence. Only a quarter of rural Indians suffering from HTN are aware of and are being treated for HTN. Forty-two percent of urban Indian hypertensive patients are aware of their hypertensive status. Thirty-eight percent of urban Indians are being treated for their HTN. Only one-tenth of rural Indians and one-fifth of urban Indians suffering from BP have their BP under control. In view of these findings, urgent steps to improve health education and health promotion (specifically on modifiable risk factors and awareness of BP) measures have to be made by the policy makers on a large scale. Existing interventions should look at incorporating multicomponent and multilevel approaches for better managing BP among Indians, as current rates for awareness, treatment of BP, and control of BP among those on treatment are very low.
ACKNOWLEDGEMENTS
The present work was supported by a Wellcome Trust Capacity Strengthening Strategic Award to the Public Health Foundation of India and a consortium of UK universities.
Conflicts of interest
There are no conflicts of interest.
Supplementary Material
Reviewer's Summary Evaluation
Reviewer 2
Strengths: The authors performed a comprehensive systematic review of available literature on prevalence, burden, awareness, and control of blood pressure among Indian patients from 1950 to 30 April 2013. Analysis and reporting was done in keeping with MOOSE (Meta-Analysis of Observational Studies: A Proposal for Reporting) guidelines. All included studies were scored for quality.
Weaknesses: Despite thoughtful attempts to investigate potential sources, large and unexplained heterogeneity remains. The effect of the study design and quality scores on the pooled estimates has not been assessed. As noted, further studies using alternative approaches such as disease mapping, Bayesian and hierarchical modelling techniques can better discriminate and explore the regional differences that emerged in the present study.
Footnotes
Abbreviations: BP, blood pressure; GBD, global burden of disease; HTN, hypertension; NCD, noncommunicable disease; NEWS, north, east, west, and south
REFERENCES
- 1.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380:2224–2260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leeder S, Raymond S, Greenberg H, Liu H. A race against time. The challenge of cardiovascular disease in developing economies. New York:Columbia University; 2004 [Google Scholar]
- 3.Srinath Reddy K, Shah B, Varghese C, Ramadoss A. Responding to the threat of chronic diseases in India. Lancet 2005; 366:1744–1749 [DOI] [PubMed] [Google Scholar]
- 4.Gupta R. Trends in hypertension epidemiology in India. J Hum Hypertens 2004; 18:73–78 [DOI] [PubMed] [Google Scholar]
- 5.Mackay J, Mensah G. Atlas of heart disease and stroke. Geneva:World Health Organization; 2004 [Google Scholar]
- 6.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006; 367:1747–1757 [DOI] [PubMed] [Google Scholar]
- 7.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet 2005; 365:217–223 [DOI] [PubMed] [Google Scholar]
- 8.Thankappan KR, Sivasankaran S, Sarma PS, Mini G, Khader SA, Padmanabhan P, et al. Prevalence-correlates-awareness-treatment and control of hypertension in Kumarakom, Kerala: baseline results of a community-based intervention program. Indian Heart J 2006; 58:28–33 [PubMed] [Google Scholar]
- 9.Gupta R. Meta-analysis of prevalence of hypertension in India. Indian Heart J 1997; 49:450. [PubMed] [Google Scholar]
- 10.Das SK, Sanyal K, Basu A. Study of urban community survey in India: growing trend of high prevalence of hypertension in a developing country. Int J Med Sci 2005; 2:70–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Noncommunicable diseases country profiles 2011. http://www.who.int/nmh/countries/ind_en.pdf [Accessed 10 May 2013] [Google Scholar]
- 12.Hypertension Study Group Prevalence, awareness, treatment and control of hypertension among the elderly in Bangladesh and India: a multicentre study. Bull World Health Organ 2001; 79:490–500 [PMC free article] [PubMed] [Google Scholar]
- 13.Devi P, Rao M, Sigamani A, Faruqui A, Jose M, Gupta R, et al. Prevalence, risk factors and awareness of hypertension in India: a systematic review. J Hum Hypertens 2013; 27:281–287 [DOI] [PubMed] [Google Scholar]
- 14.Gupta R, Guptha S, Sharma KK, Gupta A, Deedwania P. Regional variations in cardiovascular risk factors in India: India Heart Watch. World J Cardiol 2012; 4:112–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaur M. Blood pressure trends and hypertension among rural and urban Jat women of Haryana, India. Coll Antropol 2012; 36:139–144 [PubMed] [Google Scholar]
- 16.Bansal SK, Saxena V, Kandpal SD, Gray WK, Walker RW, Goel D. The prevalence of hypertension and hypertension risk factors in a rural Indian community: a prospective door-to-door study. J Cardiovasc Dis Res 2012; 3:117–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bhardwaj R, Kandori A, Marwah R, Vaidya P, Singh B, Dhiman P, Sharma A. Prevalence, awareness and control of hypertension in rural communities of Himachal Pradesh. J Assoc Physicians India 2010; 58:423–424429 [PubMed] [Google Scholar]
- 18.Gupta S, Kapoor S. Sex differences in blood pressure levels and its association with obesity indices: who is at greater risk. Ethn Dis 2010; 20:370–375 [PubMed] [Google Scholar]
- 19.Malhotra P, Kumari S, Kumar R, Jain S, Sharma BK. Prevalence and determinants of hypertension in an un-industrialised rural population of North India. J Hum Hypertens 1999; 13:467–472 [DOI] [PubMed] [Google Scholar]
- 20.Goel NK, Kaur P. Dr P. C. Sen Memorial Award – 1994. Role of various risk factors in the epidemiology of hypertension in a rural community of Varanasi district. Indian J Public Health 1996; 40:71–76 [PubMed] [Google Scholar]
- 21.Joshi A, Puricelli Perin DM, Arora M. Using Portable Health Information Kiosk to assess chronic disease burden in remote settings. Rural Remote Health 2013; 13:2279. [PubMed] [Google Scholar]
- 22.Borah PK, Shankarishan P, Hazarika NC, Mahanta J. Hypertension subtypes and angiotensin converting enzyme (ACE) gene polymorphism in Indian population. J Assoc Physicians India 2012; 60:11.15–17 [PubMed] [Google Scholar]
- 23.Dutta A, Ray MR. Prevalence of hypertension and prehypertension in rural women: a report from the villages of West Bengal, a state in the eastern part of India. Aust J Rural Health 2012; 20:219–225 [DOI] [PubMed] [Google Scholar]
- 24.Biswas M, Manna CK. Prevalence of hypertension and sociodemographic factors within the scheduled caste community of the District Nadia, West Bengal, India. High Blood Press Cardiovasc Prev 2011; 18:179–185 [DOI] [PubMed] [Google Scholar]
- 25.Borah PK, Hazarika NC, Biswas D, Kalita HC, Mahanta J. Population-specific left ventricular hypertrophy in three groups from the northeastern region of India. Natl Med J India 2010; 23:336–339 [PubMed] [Google Scholar]
- 26.Hazarika NC, Biswas D, Mahanta J. Hypertension in the elderly population of Assam. J Assoc Physicians India 2003; 51:567–573 [PubMed] [Google Scholar]
- 27.Bhagyalaxmi A, Atul T, Shikha J. Prevalence of risk factors of noncommunicable diseases in a district of Gujarat, India. J Health Popul Nutr 2013; 31:78–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gupta R, Sharma AK. Prevalence of hypertension and subtypes in an Indian rural population: clinical and electrocardiographic correlates. J Hum Hypertens 1994; 8:823–829 [PubMed] [Google Scholar]
- 29.Kokiwar PR, Rao JG, Shafee MD. Prevalence of coronary risk factors in a rural community of Andhra Pradesh. Indian J Public Health 2009; 53:52–54 [PubMed] [Google Scholar]
- 30.Kokiwar PR, Gupta SS, Durge PM. Prevalence of hypertension in a rural community of central India. J Assoc Physicians India 2012; 60:26–29 [PubMed] [Google Scholar]
- 31.Chinnakali P, Mohan B, Upadhyay RP, Singh AK, Srivastava R, Yadav K. Hypertension in the elderly: prevalence and health seeking behavior. N Am J Med Sci 2012; 4:558–562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haddad S, Mohindra KS, Siekmans K, Màk G, Narayana D. Health divide’ between indigenous and nonindigenous populations in Kerala, India: population based study. BMC Public Health 2012; 12:390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sathish T, Kcannan S, Sarma PS, Razum O, Thankappan KR. Incidence of hypertension and its risk factors in rural Kerala, India: a community-based cohort study. Public Health 2012; 126:25–32 [DOI] [PubMed] [Google Scholar]
- 34.Kaur P, Rao SR, Radhakrishnan E, Rajasekar D, Gupte MD. Prevalence, awareness, treatment, control and risk factors for hypertension in a rural population in south India. Int J Public Health 2012; 57:87–94 [DOI] [PubMed] [Google Scholar]
- 35.Prince MJ, Ebrahim S, Acosta D, Ferri CP, Guerra M, Huang Y, et al. Hypertension prevalence, awareness, treatment and control among older people in Latin America, India and China: a 10/66 cross-sectional population-based survey. J Hypertens 2012; 30:177–187 [DOI] [PubMed] [Google Scholar]
- 36.Manimunda SP, Sugunan AP, Benegal V, Balakrishna N, Rao MV, Pesala KS. Association of hypertension with risk factors & hypertension related behaviour among the aboriginal Nicobarese tribe living in Car Nicobar Island, India. Indian J Med Res 2011; 133:287–293 [PMC free article] [PubMed] [Google Scholar]
- 37.Thrift AG, Evans RG, Kalyanram K, Kartik K, Fitzgerald SM, Srikanth V. Gender-specific effects of caste and salt on hypertension in poverty: a population-based study. J Hypertens 2011; 29:443–450 [DOI] [PubMed] [Google Scholar]
- 38.Kar SS, Thakur JS, Virdi NK, Jain S, Kumar R. Risk factors for cardiovascular diseases: is the social gradient reversing in northern India? Natl Med J India 2010; 23:206–209 [PubMed] [Google Scholar]
- 39.Singh RB, Fedacko J, Pella D, Macejova Z, Ghosh S, de Amit K, et al. Prevalence and risk factors for prehypertension and hypertension in five Indian cities. Acta Cardiol 2011; 66:29–37 [DOI] [PubMed] [Google Scholar]
- 40.Midha T, Idris M, Saran R, Srivastava A, Singh S. Isolated systolic hypertension and its determinants: a cross-sectional study in the adult population of Lucknow district in north India. Indian J Community Med 2010; 35:89–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chaturvedi S, Pant M, Yadav G. Hypertension in Delhi: prevalence, awareness, treatment and control. Trop Doct 2007; 37:142–145 [DOI] [PubMed] [Google Scholar]
- 42.Ganguli D, Das N, Saha I, Chaudhuri D, Ghosh S, Dey S. Risk factors for hypertension in a population-based sample of postmenopausal women in Kolkata, West Bengal, India. Asia Pac J Public Health 2013; 5:388–397 10.1177/1010539511420703 [DOI] [PubMed] [Google Scholar]
- 43.Gupta R, Sharma KK, Gupta A, Agrawal A, Mohan I, Gupta VP, et al. Persistent high prevalence of cardiovascular risk factors in the urban middle class in India: Jaipur Heart Watch-5. J Assoc Physicians India 2012; 60:11–16 [PubMed] [Google Scholar]
- 44.Gupta R, Guptha S, Gupta VP, Prakash H. Prevalence and determinants of hypertension in the urban population of Jaipur in western India. J Hypertens 1995; 13:1193–1200 [DOI] [PubMed] [Google Scholar]
- 45.Gupta PC, Gupta R, Pednekar MS. Hypertension prevalence and blood pressure trends in 88 653 subjects in Mumbai, India. J Hum Hypertens 2004; 18:907–910 [DOI] [PubMed] [Google Scholar]
- 46.Gupta R, Gupta VP, Sarna M, Bhatnagar S, Thanvi J, Sharma V, et al. Prevalence of coronary heart disease and risk factors in an urban Indian population: Jaipur Heart Watch-2. Indian Heart J 2002; 54:59–66 [PubMed] [Google Scholar]
- 47.Gupta R, Kaul V, Bhagat N, Agrawal M, Gupta VP, Misra A, Vikram NK. Trends in prevalence of coronary risk factors in an urban Indian population: Jaipur Heart Watch-4. Indian Heart J 2007; 59:346–353 [PubMed] [Google Scholar]
- 48.Gurav RB, Kartikeyan S, Jadhav BS. Biochemical profile of hypertensive individuals in an urban community. Indian J Med Sci 2001; 55:663–668 [PubMed] [Google Scholar]
- 49.Bharucha NE, Kuruvilla T. Hypertension in the Parsi community of Bombay: a study on prevalence, awareness and compliance to treatment. BMC Public Health 2003; 3:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pednekar MS, Gupta R, Gupta PC. Association of blood pressure and cardiovascular mortality in India: Mumbai cohort study. Am J Hypertens 2009; 22:1076–1084 [DOI] [PubMed] [Google Scholar]
- 51.Thankappan KR, Shah B, Mathur P, Sarma PS, Srinivas G, Mini GK, et al. Risk factor profile for chronic noncommunicable diseases: results of a community-based study in Kerala, India. Indian J Med Res 2010; 131:53–63 [PubMed] [Google Scholar]
- 52.Mohan V, Deepa M, Farooq S, Datta M, Deepa R. Prevalence, awareness and control of hypertension in Chennai: the Chennai Urban Rural Epidemiology Study (CURES-52). J Assoc Physicians India 2007; 55:326–332 [PubMed] [Google Scholar]
- 53.Shanthirani CS, Pradeepa R, Deepa R, Premalatha G, Saroja R, Mohan V. Prevalence and risk factors of hypertension in a selected South Indian population: the Chennai Urban Population Study. J Assoc Physicians India 2003; 51:20–27 [PubMed] [Google Scholar]
- 54.Deepa R, Shanthirani CS, Pradeepa R, Mohan V. Is the ’rule of halves’ in hypertension still valid? Evidence from the Chennai Urban Population Study. J Assoc Physicians India 2003; 51:153–157 [PubMed] [Google Scholar]
- 55.Reddy NK, Kumar DN, Rayudu NV, Sastry BK, Raju BS. Prevalence of risk factors for coronary atherosclerosis in a cross-sectional population of Andhra Pradesh. Indian Heart J 2002; 54:697–701 [PubMed] [Google Scholar]
- 56.Joseph A, Kutty VR, Soman CR. High risk for coronary heart disease in Thiruvananthapuram city: a study of serum lipids and other risk factors. Indian Heart J 2000; 52:29–35 [PubMed] [Google Scholar]
- 57.Gupta R, Deedwania PC, Achari V, Bhansali A, Gupta BK, Gupta A, et al. Normotension, prehypertension, and hypertension in urban middle-class subjects in India: prevalence, awareness, treatment, and control. Am J Hypertens 2013; 26:83–94 [DOI] [PubMed] [Google Scholar]
- 58.Jeemon P, Prabhakaran D, Goenka S, Ramakrishnan L, Padmanabhan S, Huffman M, et al. Sentinel Surveillance in Industrial Populations Study Group Impact of comprehensive cardiovascular risk reduction programme on risk factor clustering associated with elevated blood pressure in an Indian industrial population. Indian J Med Res 2012; 135:485–493 [PMC free article] [PubMed] [Google Scholar]
- 59.Pandey RM, Gupta R, Misra A, Misra P, Singh V, Agrawal A, et al. Determinants of urban-rural differences in cardiovascular risk factors in middle-aged women in India: a cross-sectional study. Int J Cardiol 2013; 163:157–162 [DOI] [PubMed] [Google Scholar]
- 60.Gupta R, Pandey RM, Misra A, Agrawal A, Misra P, Dey S, et al. High prevalence and low awareness, treatment and control of hypertension in Asian Indian women. J Hum Hypertens 2012; 26:585–593 [DOI] [PubMed] [Google Scholar]
- 61.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008; 61:344–349 [DOI] [PubMed] [Google Scholar]
- 62.Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strobe Initiative Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med 2007; 4:e297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hazarika NC, Biswas D, Narain K, Kalita HC, Mahanta J. Hypertension and its risk factors in tea garden workers of Assam. Natl Med J India 2002; 15:63–68 [PubMed] [Google Scholar]
- 64.Meshram II, Arlappa N, Balkrishna N, Rao KM, Laxmaiah A, Brahmam GN. Prevalence of hypertension, its correlates and awareness among adult tribal population of Kerala state, India. J Postgrad Med 2012; 58:255–261 [DOI] [PubMed] [Google Scholar]
- 65.Samuel P, Antonisamy B, Raghupathy P, Richard J, Fall CH. Socio-economic status and cardiovascular risk factors in rural and urban areas of Vellore, Tamil Nadu, South India. Int J Epidemiol 2012; 41:1315–1327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zaman MJ, Patel A, Jan S, Hillis GS, Raju PK, Neal B, Chow CK. Socio-economic distribution of cardiovascular risk factors and knowledge in rural India. Int J Epidemiol 2012; 41:1302–1314 [DOI] [PubMed] [Google Scholar]
- 67.Joshi SR, Saboo B, Vadivale M, Dani SI, Mithal A, Kaul U, et al. SITE Investigators Prevalence of diagnosed and undiagnosed diabetes and hypertension in India: results from the Screening India's Twin Epidemic (SITE) study. Diabetes Technol Ther 2012; 14:8–15 [DOI] [PubMed] [Google Scholar]
- 68.Reddy KS, Prabhakaran D, Jeemon P, Thankappan KR, Joshi P, Chaturvedi V, et al. Educational status and cardiovascular risk profile in Indians. Proc Natl Acad Sci U S A 2007; 104:16263–16268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jeemon P, Reddy KS. Social determinants of cardiovascular disease outcomes in Indians. Indian J Med Res 2010; 132:617–622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kinra S, Bowen LJ, Lyngdoh T, Prabhakaran D, Reddy KS, Ramakrishnan L, et al. Sociodemographic patterning of noncommunicable disease risk factors in rural India: a cross sectional study. BMJ 2010; 341:c4974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Thorlund K, Imberger G, Johnston BC, Walsh M, Awad T, Thabane L, et al. Evolution of heterogeneity (I2) estimates and their 95% confidence intervals in large meta-analyses. PLoS One 2012; 7:e39471. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


