Abstract
Purpose of review
The article discusses the clinical management of patients affected by food protein-induced enterocolitis syndrome (FPIES), focusing on established therapeutic choices and future options.
Recent findings
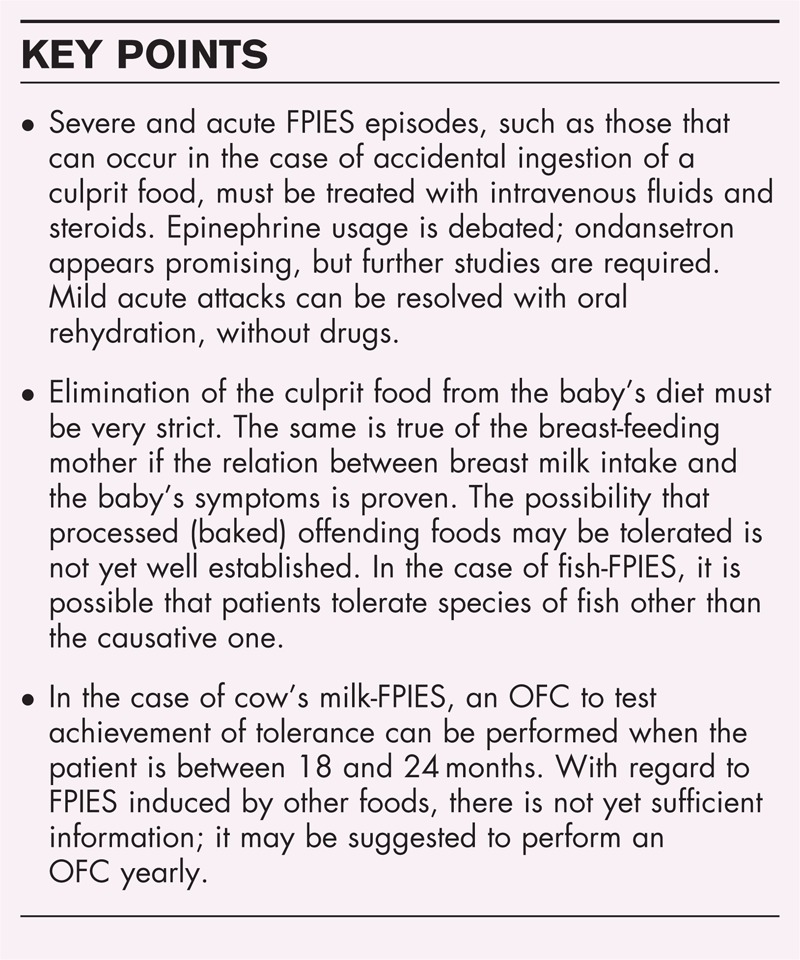
After FPIES has been diagnosed and avoidance of the culprit food prescribed, the most important management needs are as follows. First, recurrence of acute FPIES episodes due to accidental ingestion of culprit food. It may be useful to give patients’ families an action plan. The principal suggested treatments are intravenous fluids and steroids, whereas the use of epinephrine and ondansetron requires further study. In mild-to-moderate cases, oral rehydration should be sufficient. Second, dietary introduction of at-risk foods. In children with FPIES, in addition to that/those identified as culprit(s), some foods may not be tolerated (typically cow's milk, legumes, cereals, poultry). It has been suggested to avoid introducing these foods during the baby's first year. Otherwise, they may be given for the first time in hospital, performing an oral food challenge. Third, acquisition of tolerance. Children affected by cow's milk-FPIES have a good chance of acquiring tolerance by the time they reach age 18–24 months. For other culprit foods, insufficient data are available to indicate the appropriate time, so that it is suggested that an oral food challenge be performed about 1 year after the last acute episode.
Summary
Future clinical management of FPIES must take into account, among other factors, improved understanding of pathogenesis, possible detection of different phenotypes, and the introduction of more effective therapies for acute episodes. These factors will undoubtedly influence management decisions, which will become more diversified and effective.
Keywords: clinical management, food protein-induced enterocolitis syndrome, oral food challenge
INTRODUCTION
The clinical management of a patient who has received a definitive diagnosis of FPIES is a simple matter, comprising a small number of key points. Some clinical cases are reported to exemplify these key points: recurrence of acute episodes due to the accidental ingestion of culprit food; introduction of at-risk foods and long-term dietary management; follow-up and acquisition of tolerance. The current state of knowledge and management of this syndrome is described and compared with future hypotheses and perspectives.
CLINICAL CASE NUMBER 1
When Gabriele was 1 year old, he received a diagnosis of egg-FPIES; he had already experienced three severe acute episodes. Rigorous avoidance of dietary egg was prescribed, and the parents were given an action plan of instructions to be followed in case of accidental egg ingestion; this could be shown to the medical personnel in case of emergency. Some months later, Gabriele accidentally ate a small piece of omelet at nursery school, without anyone noticing. Two hours later his fourth acute FPIES episode occurred. The child presented with repetitive and profuse vomiting, pallor, and severe lethargy. He was immediately taken to the emergency department, where his parents produced the action plan; intravenous fluids and steroids were immediately administered. Six hours after the onset of symptoms, he had recovered fully.
Box 1.
no caption available
RECURRENCE OF ACUTE EPISODES DUE TO ACCIDENTAL INGESTION OF CULPRIT FOOD
Case number 1 exemplifies an acute and severe FPIES episode and its official pharmacological management. However, as for other aspects of this syndrome, no randomized trials have been carried out that support the actual efficacy of this management protocol. As Sicherer [1] has pointed out, these therapeutic measures are indicated on the basis of the symptoms of FPIES, and on current knowledge of its immunopathogenesis, which is still far from complete. Intravenous fluids and steroids should be administered in acute and severe episodes consisting of repetitive and profuse vomiting, severe and bloody diarrhea, pallor, lethargy, hypotonia, and hypotension (Table 1).
Table 1.
Treatment of food protein-induced enterocolitis syndrome
| Acute | Chronic |
| Oral rehydration fluids, if mild | Removal of causative food from diet |
| Intravenous fluids, if moderate to severe: 20 ml/kg boluses of isotonic saline | Intravenous fluids if dehydrated |
| Intravenous steroids: methylprednisolone 1 mg/kg (max 60–80 mg) | For cow's milk-FPIES: use soy alternative (following a supervised oral food challenge), casein hydrolysate, or elemental formula |
| Vasopressors for hypotension if severe or unresponsive to fluids | Bicarbonate for acidemia |
| Bicarbonate for acidemia | Methylene blue for methemoglobulinemia |
| Methylene blue for methemoglobulinemia |
Reproduced with permission from Leonard et al. [2].
The role of epinephrine has not yet been fully clarified. Some studies [1,2,3▪] highlight its importance in treating hypotension when intravenous fluids and steroids fail; their experience having shown that epinephrine usage is not favorable on all other symptoms. Others [4▪] document the efficacy of epinephrine in cases with severe lethargy and without hypotension. However, the reliability of these reports is debatable, because the studies enrolled few patients without any controls. In an interesting study, Holbrook et al.[5▪] report using ondansetron hydrochloride, a serotonin 5-HT3 receptor antagonist used mainly as an antiemetic. Five patients above 3 years of age with FPIES, who had an adverse reaction during the OFC, received intravenous ondansetron (0.2 mg/kg/dose); their symptoms resolved within 10–15 min. The drug was reported to be effective not only on vomiting, but also on all other symptoms, including lethargy. This casts new light on the pathogenesis of FPIES, and on its treatment in the acute phase. We have administered ondansetron intramuscularly to three girls with FPIES, below the age of 3, who had an acute adverse reaction during OFC; resolution of symptoms was very rapid (unpublished data). Conversely, two other studies [6,7] reported that most acute episodes after OFC were resolved with oral rehydration alone, or even without any treatment. It is also well known that most acute episodes take place at home and are resolved without medical assistance or treatment. Lastly, there are no reports of death caused by FPIES. We thus think that, during an acute but mild FPIES episode (mild vomiting, without lethargy or hypotension, after accidental ingestion of the culprit food), a ‘wait and see’ approach could be warranted, provided that, if it becomes necessary, a venous line for fluids and steroids is immediately available. The same approach can be used during OFC, provided that the patient has no history of severe acute episodes. In our view, this ‘wait and see’ management should not be applied in the case of infants younger than 12 months, because of the greater difficulty of rapidly placing a venous line. An acute FPIES episode rarely requires bicarbonates to correct acidosis, nor methylene blue for methemoglobulinemia; these treatments are more frequently necessary in chronic FPIES with dehydration (see Table 1). Patients suffering from chronic FPIES sometimes receive the diagnosis when they are in a critical condition, and should be rehydrated with either oral or intravenous fluids. Bicarbonate and methylene blue can be administered as needed; temporary bowel rest and parenteral nutrition may be necessary in the most severe cases.
Reactions to accidental exposure can be severe, and instructions for emergency management should be provided. If ingestion is known to have occurred, the patient should be instructed to present to medical attention for observation [1]; if symptoms begin when medical assistance is unavailable, we recommend that caregivers administer fluids and steroids orally (prescribed for this eventuality by a physician). Because the clinical presentation and management of FPIES are generally unfamiliar in urgent care centers, it is helpful to provide patients with an action plan [1], explaining symptoms and recommending management of acute reactions. The same information should be given to the child's general practitioner and school staff. A template for a letter can be accessed online at http://download.journals.elsevierhealth.com/mmcs/journals/0091–6749/PIIS0091674904024881.mmc1.pdf[1].
CLINICAL CASE NUMBER 2
Carmen suffers from atopic eczema; she has been exclusively breast-fed. From her second month of life she presented frequent episodes of vomiting and diarrhea, sometimes watery; her growth was normal. When she was 5 months, she drank 70 ml of cow's milk formula; 2 h later she presented with repetitive and profuse vomiting, pallor, lethargy, and watery stools. Two hours later the symptoms resolved, and this episode was diagnosed as a viral gastroenteritis. After 2 weeks, she again drank 90 ml of cow's milk formula, and 2 h later suffered a similar acute episode. After the symptoms had improved, she still had episodes of regurgitation, colic, and occasional diarrhea. When Carmen reached the age of 6 months, her mother, who was still breast-feeding the baby, exceptionally drank a larger than usual quantity of cow's milk (500 ml) as she had to take a breath test. Twelve hours later, Carmen presented with a worsening of her chronic symptoms: increased regurgitation, diarrhea with bloody stools, and colic. An allergist now formulated a diagnosis of FPIES and eliminated cow's milk proteins from the diet of both the child and the mother. Gradually, regurgitation, colic, and diarrhea disappeared. Carmen started to eat other foods but, when she ate cream of rice (that does not contain cow's milk), the diarrhea reappeared; this occurred twice, and rice was eliminated from her diet.
LONG-TERM DIETARY MANAGEMENT AND INTRODUCTION OF AT-RISK FOODS
Carmen's story clearly exemplifies the chronic FPIES phenotype, which is rare. This case can be considered even rarer, because the culprit food affected her after passing through the breast milk. Although chronic FPIES is less frequent than acute FPIES, its long-term management is very similar: both require the culprit food to be eliminated from the patient's diet, a point on which all experts agree.
Whereas in the case of IgE-mediated food allergies management is moving toward decreasing dietary restrictions, albeit with great caution (e.g. administration of baked milk or egg, oral immunotherapy), and although the current standard of care continues to entail strict avoidance of the food allergen for food allergy patients [8], in the case of FPIES patients, avoidance of culprit foods is compulsory, and surrounded by little or no doubt. This certainty is due to at least three reasons: first, most FPIES patients achieve tolerance spontaneously before their fifth year of life, an important reason making oral immunotherapy less attractive; second, for the individual patient, it is difficult to know the minimal dose of culprit food that may cause an adverse reaction; it may even be infinitesimal. This is due to the latency of symptoms; the child can finish the meal before any symptoms appear. It is thus very difficult to formulate an oral immunotherapy program with an initial dose that will almost certainly be tolerated; third, although the immunopathogenic mechanisms are not as yet fully clear, the most convincing hypothesis assigns an important role to the T lymphocytes and their inflammatory cytokines [9]; this would mean that pathogenic chemical bonds involve sequential peptides that are so small that any heating process, as for example in baking food, will be irrelevant in terms of the immune system's recognition of epitopes.
In the case of cow's milk-FPIES, if breast milk is lacking, the use of an extensively hydrolyzed casein formula is usually recommended, whereas soy milk should be avoided. These recommendations were developed on the basis of studies observing some clinical cohorts some years ago in the USA; the studies showed that 50% of children affected by cow's milk-FPIES had adverse reactions to soy. More recently, Ruffner et al.[10▪] confirmed these data in a study likewise conducted on U.S. children. However, Israeli [6], Italian [7], and Australian [11] reports have not found the same association between cow's milk-FPIES and soy-FPIES. Soy milk may thus be considered as a cow's milk substitute, but only after having performed an OFC, to ensure that no adverse events will occur [3▪]. In rare cases, it may be necessary to use an amino-acid formula.
Two hypothetical liberalization in the diet
It has been reported that culprit foods (in particular, cow's milk and hen's egg) may be tolerated if baked [12▪]; this runs counter to the theory of an exclusively cell-mediated pathogenesis of FPIES, and provides support for a role played by specific IgEs, as has been hypothesized [4▪,9]. However, very few studies have addressed this point, so that in expectation of further research, the current recommendation is still to avoid culprit food even if baked. In this case, too, possible tolerance of baked culprit food should be verified by means of an OFC.
In the case of fish-FPIES, which is the commonest form of solid-food-induced FPIES in Italy [7], it may not be necessary to eliminate all kinds of fish from the diet. Sopo et al.[7] reported that three of eight children who reacted to one or more types of fish tolerated other fish (e.g. tuna, swordfish, salmon). It is known that cross-reactivity between species of fish is not absolute in IgE-mediated fish allergy [13]; this may also be true for fish-FPIES. Be that as it may, tolerance to other types of fish must in all cases be verified via an OFC.
Should a restrictive diet be prescribed to breast-feeding mothers?
Based on Carmen's story, other therapeutic options, about which there is less certainty, may also be examined. The elimination of cow's milk from her breast-feeding mother's diet was certainly useful to improve her condition: there was undoubtedly a clear association between the child's chronic FPIES symptoms and the breast-feeding mother's cow's milk intake. But what of the case of a child who has a diagnosis of acute FPIES caused by the direct ingestion, for example, of egg? Should we also prescribe a restrictive diet to his breast-feeding mother? Opinions differ on this point. Monti et al.[14], who were the first to describe a case of FPIES caused by the proteins of a culprit food that had passed through the breast milk, propose eliminating the culprit food from the mother's diet if the baby's FPIES episodes are severe. Conversely, Tan et al.[15] suggest eliminating the culprit food from the maternal diet only if there are documented adverse reactions occurring as a result of the child's intake of breast milk. The latter position is also supported by Järvinen and Nowak-Wegrzyn [3▪], who suggest that the culprit food should only be removed from the mother's diet if reactions after breast-feeding have occurred, or if the infant fails to thrive. Considering the rarity of FPIES passing through breast milk, this more tolerant approach is currently preferable.
When should it be suggested that other foods, apart from the culprit food, should be eliminated from the diet?
Carmen ate rice, and subsequently presented with diarrhea; could it have been prevented? Sicherer [1] has proposed eliminating other foods from the diet in addition to the culprit food. In the case of cow's milk-FPIES, he suggests avoiding soy and cereals, and delaying the introduction of other solid foods, at least until the baby is 1 year old. In cases of FPIES induced by solid food, he proposes avoiding the ingestion of cow's milk, cereals, legumes, and poultry, at least until the baby reaches 1 year. Clearly, the preventive diet will only be implemented if, at the time of diagnosis of FPIES, the child has not already eaten the foods in question without problems. This suggestion arose from observations in two U.S. series comprising 30−50 children; children with cow's milk-FPIES or with solid-food FPIES showed clinical reactivity to these foods. More recently, studies on cohorts of patients outside the USA [6,7,11] have reported a very low prevalence of children suffering from multiple culprit food FPIES. Based on these findings, it could be of interest to perform OFC tests with a mixture of those ‘at-risk’ foods (cow's milk, legumes, cereals, poultry) that have not yet been introduced into the baby's diet at the time of FPIES diagnosis. If this approach is followed, as we do regularly and with good results, it is unnecessary to eliminate at-risk foods preemptively: if the patient passes the OFC, he or she can then eat them without giving rise to concern, even before 1 year of age. Similarly, in patients with IgE-mediated food allergies, but only in cases in which the risk of an adverse reaction is low, the American Academy of Allergy, Asthma & Immunology (AAAAI) [16] recommends that OFC be performed with a mix of other foods potentially cross-reactive with the food that is demonstrably the culprit, in order to save human and economic resources. Conversely, if the risk of an adverse reaction is thought to be high, they recommend performing a series of OFCs with one food at a time. Moreover, the fact that some foods are considered at risk for children with FPIES is not based on a mechanism of cross-reactivity, as might be the case of a child with an IgE-mediated allergy to hazelnut having an increased risk of adverse reaction to walnuts. There is no cross-reactivity among cow's milk, legumes, cereals, and poultry. Cross-reactivity among foods, which undoubtedly plays a central role in IgE-mediated food allergies, has not yet been described in FPIES. In this connection, no reports have been published of patients suffering from cow's milk-FPIES who have a high risk of experiencing an acute episode of FPIES induced by goat's milk, although there are some anecdotal accounts (Yitzhak Katz, personal communication). In our own clinical experience, a baby who was affected by cow's milk-FPIES did not tolerate beef (which is not considered an at-risk food), whereas other children suffering from cow's milk-FPIES tolerated donkey's milk (unpublished data).
CLINICAL CASE NUMBER 3
At 4 months, Anna presented with a history of three episodes of profuse and repetitive vomiting, pallor, severe lethargy, and diarrhea, with onset 2–3 h after drinking 30 ml of cow's milk formula. Skin prick tests (SPTs) were weakly positive for pasteurized cow's milk, β-lactoglobulin, and α-lactoalbumin, and she was diagnosed with atypical FPIES [17]. At 16 months, an OFC was performed to test the possible acquisition of tolerance: the child drank 200 ml of cow's milk with no adverse reaction. She tolerated cow's milk for 5 days, apart from developing small areas of urticaria in regions where cow's milk or its derivates come into contact with the skin, for example, the perioral area. During days 6 and 7, 20–30 min after drinking 200 ml of cow's milk, she presented with coughing and vomiting. The front of the child's body became soiled by vomit, and extensive urticaria flared up in that area. Another OFC was performed, with the child taking 200 ml of cow's milk in a single administration, as she had done at home the previous week; the same adverse reaction occurred, again after 20 min.
When should an OFC be administered to test the achievement of tolerance?
Anna's story introduces at least two further points. First, the most appropriate timing for OFC to test achievement of tolerance. Many studies have collected data about cow's milk-FPIES: Nowak-Wegrzyn et al.[18] report that 60% of cow's milk-FPIES patients had regained tolerance within the second year of life. Both Katz et al.[6] and Hwang et al.[19] found that most of their patients regained tolerance between ages 18 and 20 months. Sopo et al.[7] found that cow's milk-FPIES was resolved by the time patients were 18–24 months old. These findings are fairly uniform, so that it can be assumed that the best time to test achievement of tolerance of cow's milk is between 18 months and 2 years of age, when the probability of a positive result is high. For other foods, reports are insufficient, and we personally would endorse Järvinen and Nowak-Wegrzyn's [3▪] suggestion: ‘The culprit food should be considered for reintroduction to the diet 12–18 months after the last reaction, in a physician-supervised setting.’
The second point to emerge from Anna's story concerns how the OFC should be managed. She suffers from atypical FPIES, because IgEs of the culprit food were found; it is known that this particular form tends to last longer than typical forms of FPIES. This is what occurred in her case, although it should be pointed out that her condition was transformed from FPIES to a typical IgE-mediated food allergy [20]. In cases of this sort, the persistence of IgEs of specific culprit foods (which should be tested whenever an OFC is scheduled) means that a typical IgE-mediated food allergy OFC should be adopted, starting with very small doses and with increments every 20–30 min.
CONCLUSION
In 2005, Sicherer [1] wrote: ‘… but much more research is needed to determine the best course of dietary management, develop laboratory tests to avoid the need for oral food challenges, address prevention, and determine specific treatment modalities. These goals will most likely be reached through more intensive laboratory investigation of the immunopathologic basis of the disorder. More work also needs to be done to determine whether disorders with similar symptoms are pathophysiologically distinct from FPIES or part of a spectrum with a similar cause whose clinical expression varies with environmental influences.’ In 2014, we still agree with those conclusions.
Acknowledgements
No funding was received for this work.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Sicherer SH. Food protein-induced enterocolitis syndrome: case presentations and management lessons. J Allergy Clin Immunol 2005; 115:149–156 [DOI] [PubMed] [Google Scholar]
- 2.Leonard SA, Nowak-Węgrzyn A. Clinical diagnosis and management of food protein-induced enterocolitis syndrome. Curr Opin Pediatr 2012; 24:739–745 [DOI] [PubMed] [Google Scholar]
- 3▪.Järvinen KM, Nowak-Wegrzyn A. Food protein-induced enterocolitis syndrome (FPIES): current management strategies and review of the literature. J Allergy Clin Immunol Pract 2013; 1:317–322 [DOI] [PubMed] [Google Scholar]; A very comprehensive review and an excellent update on various aspects of FPIES. The authors have a great experience with this and pass it very well.
- 4▪.Miceli Sopo S, Greco M, Monaco S, et al. Food protein-induced enterocolitis syndrome, from practice to theory. Expert Rev Clin Immunol 2013; 9:707–715 [DOI] [PubMed] [Google Scholar]; This review addresses also management aspects that are not yet fully resolved. Its interesting feature is to exemplify the management aspects with many clinical cases.
- 5▪.Holbrook T, Keet CA, Frischmeyer-Guerrerio PA, Wood RA. Use of ondansetron for food protein-induced enterocolitis syndrome. J Allergy Clin Immunol 2013; 132:1219–1220 [DOI] [PubMed] [Google Scholar]; In this small experience, the authors propose a pharmacological treatment for acute episodes of FPIES, which looks very promising.
- 6.Katz Y, Goldberg MR, Rajuan N, et al. The prevalence and natural course of food protein-induced enterocolitis syndrome to CM: a largescale, prospective population-based study. J Allergy Clin Immunol 2011; 127:647–653e1–e3 [DOI] [PubMed] [Google Scholar]
- 7.Miceli Sopo S, Giorgio V, Dello Iacono I, et al. A multicentre retrospective study of 66 Italian children with food protein induced enterocolitis syndrome: different management for different phenotypes. Clin Exp Allergy 2012; 42:1257–1265 [DOI] [PubMed] [Google Scholar]
- 8.Wang J, Fiocchi A. Food allergy from an avoidance to a proactive approach: a bridge too far? Curr Opin Allergy Clin Immunol 2012; 12:269–270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caubet JC, Nowak-Węgrzyn A. Current understanding of the immune mechanisms of food protein-induced enterocolitis syndrome. Expert Rev Clin Immunol 2011; 7:317–327 [DOI] [PubMed] [Google Scholar]
- 10▪.Ruffner MA, Ruymann K, Barni S, et al. Food protein-induced enterocolitis syndrome: insights from review of a large referral population. J Allergy Clin Immunol Pract 2013; 1:343–349 [DOI] [PubMed] [Google Scholar]; This case study is, at the time, the largest ever published.
- 11.Mehr S, Kakakios A, Frith K, Kemp AS. Food protein-induced enterocolitis syndrome: 16-year experience. Pediatrics 2009; 123:e459–e464 [DOI] [PubMed] [Google Scholar]
- 12▪.Miceli Sopo S, Buonsenso D, Monaco S, et al. Food protein-induced enterocolitis syndrome (FPIES) and well cooked foods: a working hypothesis. Allergol Immunopathol 2013; 41:346–348 [DOI] [PubMed] [Google Scholar]; This small report is interesting because its confirmation on a large scale would result in an improvement in the quality of life of children with FPIES and shed new light on the immunopathogenetic mechanisms of the syndrome.
- 13.Pascual CY, Reche M, Fiandor A, et al. Fish allergy in childhood. Pediatr Allergy Immunol 2008; 19:573–579 [DOI] [PubMed] [Google Scholar]
- 14.Monti G, Castagno E, Liguori SA, et al. Food protein-induced enterocolitis syndrome by cow's milk proteins passed through breast milk. J Allergy Clin Immunol 2011; 127:679–680 [DOI] [PubMed] [Google Scholar]
- 15.Tan J, Campbell D, Mehr S. Food protein-induced enterocolitis syndrome in an exclusively breast-fed infant-an uncommon entity. J Allergy Clin Immunol 2012; 129:873. [DOI] [PubMed] [Google Scholar]
- 16.Nowak-Wegrzyn A, Assa’ad AH, Bahna SL, et al. Adverse Reactions to Food Committee of American Academy of Allergy, Asthma & Immunology Work Group report: oral food challenge testing. J Allergy Clin Immunol 2009; 123 (6 Suppl):S365–S383 [DOI] [PubMed] [Google Scholar]
- 17.Sicherer SH, Eigenmann PA, Sampson HA. Clinical features of food protein-induced enterocolitis syndrome. J Pediatr 1998; 133:214–219 [DOI] [PubMed] [Google Scholar]
- 18.Nowak-Wegrzyn A, Muraro A. Food protein-induced enterocolitis syndrome. Curr Opin Allergy Clin Immunol 2009; 9:371–377 [DOI] [PubMed] [Google Scholar]
- 19.Hwang JB, Sohn SM, Kim AS. Prospective follow-up oral food challenge in food protein-induced enterocolitis syndrome. Arch Dis Child 2009; 94:425–428 [DOI] [PubMed] [Google Scholar]
- 20.Onesimo R, Dello Iacono I, Giorgio V, et al. Can food protein induced enterocolitis syndrome shift to immediate gastrointestinal hypersensitivity? A report of two cases. Eur Ann Allergy Clin Immunol 2011; 43:61–63 [PubMed] [Google Scholar]


