Abstract
Purpose of review
To assess all the possible differential diagnosis of food protein-induced enterocolitis syndrome (FPIES), both in acute and chronic presentation, reviewing the data reported in published studies.
Recent findings
There is an increase of reported cases of FPIES in recent years. As the disease presents with nonspecific symptoms, it can be misunderstood in many ways. The differential diagnosis includes, in acute presentations, the following: sepsis, other infectious diseases, acute gastrointestinal episodes, surgical emergencies, food allergies. In its chronic forms, FPIES may mimic malabsorption syndromes, metabolic disorders, primary immunodeficiencies, neurological conditions, coagulation defects, and other types of non-IgE-mediated food allergy.
Summary
A thorough clinical evaluation, including symptoms, signs, and laboratory findings, is necessary to lead the clinicians toward the diagnosis of FPIES. The major reason for delayed diagnosis appears to be the lack of knowledge of the disease.
Keywords: chronic diarrhea, dehydration, differential diagnosis, food protein-induced enterocolitis syndrome
INTRODUCTION
Among the mysteries that surround the FPIES, pathogenesis is the most intriguing. Several hypotheses have been proposed, attributing the responsibility to cell-mediated or humoral-specific immunologic alterations, or to neutrophils, platelets, and/or eosinophils dysfunction. Some mediators, such as serotonin, may be involved [1]. Whatever the mechanism(s) is, the presentation of the disease is often explosive and the disease is severely hampering the patient's quality of life [2]. Thus, the condition must not go unnoticed, and a diagnosis is called for. However, because of several reasons, the first diagnosis is seldom the right one [3].
Although the differential diagnosis of FPIES has been considered an important issue for many years [4], a complete review of the conditions possibly confused with FPIES is lacking. Misdiagnoses may delay the identification of FPIES for months, exposing the children to the repetition of acute episodes [5], or even leading to dramatically incorrect diagnostic/therapeutic interventions [6]. Yet, FPIES is indicated as a possible manifestation of food allergy in all the guidelines on the topic [7–9].
The present article aims to review the possible diagnostic hypotheses proposed for FPIES before its correct identification.
THE DIAGNOSIS IS OFTEN DELAYED
The diagnosis of FPIES is often difficult and delayed, and patients may undergo extensive workups for their symptoms. This is very common in non-IgE-mediated food allergies [10], but particularly typical of this syndrome: FPIES does not have an identification biomarker nor an unequivocal, typical symptom.
Box 1.
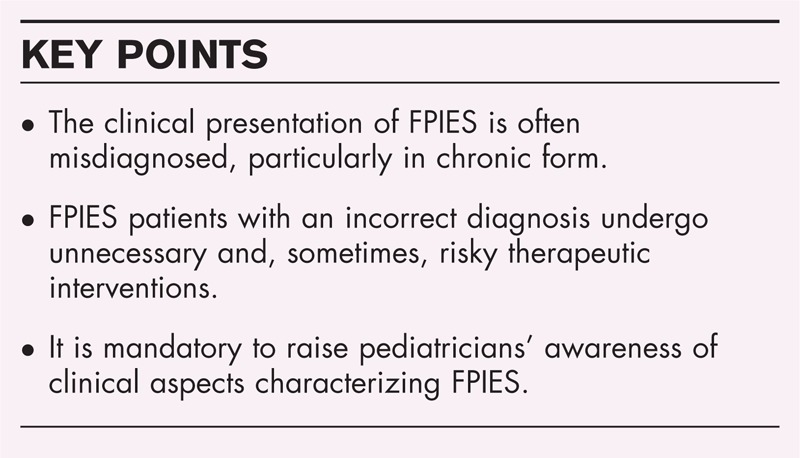
no caption available
In a retrospective study [3] of children with FPIES over the course of 16 years at Children's Hospital in Sydney, 35 children presented with 66 acute episodes of FPIES. Only two of the 19 children who presented to the emergency department with their initial reaction were discharged with the correct diagnosis. Additional tests were common for patients who presented with FPIES in the hospital, with 34% of them undergoing abdominal imaging studies, 28% a septic evaluation, and 22% a surgical consultation. Patients experienced more episodes before the correct diagnosis was made. If this happens in the acute form of the disease, one can imagine that the delayed forms are even less frequently diagnosed.
ACUTE AND CHRONIC FOOD PROTEIN-INDUCED ENTEROCOLITIS SYNDROME
FPIES may present in either acute or chronic form (Bahna [11]). In its acute form, FPIES occurs 1–3 h after every ingestion of the causative food, with somewhat more severe presentation than in the chronic form. FPIES usually presents with profuse diarrhea, vomiting, acute dehydration, and possible episodes of circulatory collapse and shock in about 20% of patients. Other possible symptoms are pallor, hypotension, hypothermia, and abdominal distension. Given its clinical characteristics, acute FPIES often takes the family to the nearest emergency room where the pediatrician is faced with a patient with an acute episode of vomiting, hypotension, and dehydration. Her first diagnostic orientation will assess the gastrointestinal tract for vomiting, diarrhea, or both. Other possible causes are listed in the following paragraphs. Sepsis is the most commonly diagnosed condition in this phase (Table 1[3,6,12–30,31▪▪,32–37]).
Table 1.
Differential diagnosis in reported cases of acute food protein-induced enterocolitis syndrome
| Year | Ref. | Gastrointestinal | Surgical | Infectious | Allergic | Other |
| 1963 | [12] | Volv | ||||
| 1992 | [13] | GE | Se | FPois, Munch | ||
| 1996 | [14] | GE | Se | Ana | ||
| 1998 | [15] | APC | Se | |||
| 2000 | [16] | GE | Se | Isch | ||
| 2003 | [17] | Se | NeS | |||
| 2003 | [18] | GE | I | Se | ||
| 2005 | [19] | GE, APC | NEC, I, HD | Se | ||
| 2005 | [20] | GE | Se | |||
| 2006 | [21] | GE | Se | |||
| 2006 | [22] | Se | Ep | |||
| 2007 | [23] | Se | ||||
| 2007 | [6] | GE, APC | I | Se | ||
| 2008 | [24] | Se | ||||
| 2009 | [3] | GE | I | Se | ||
| 2010 | [25] | PS | Ana | |||
| 2010 | [26] | Se | ||||
| 2011 | [27] | APC | ||||
| 2011 | [28] | Se | ||||
| 2011 | [29] | GE | I | Se | ||
| 2011 | [30] | Ana | ||||
| 2012 | [31▪▪] | GE | AA | Se | ||
| 2012 | [32] | GE | Ana | |||
| 2012 | [33] | GE | Ana | |||
| 2012 | [34] | GE | I | Se | ||
| 2013 | [35] | GE | ||||
| 2013 | [36] | GE | ||||
| 2013 | [37] | Se |
AA, acute abdomen; Ana, anaphylaxis; APC, allergic proctocolitis; Ep, epilepsy; FPois, food poisoning; GE, gastroenteritis; HD, Hirschsprung disease; I, intussusception; Isch, ischemia; Munch, Munchausen's syndrome; NEC, necrotizing enterocolitis; NeS, neurologic etiologies of recurrent shock; PS, pyloric stenosis; Se, Sepsis; Volv, volvulus.
Chronic FPIES is an ill-defined condition characterized by intermittent vomiting, watery or mucous diarrhea, poor weight gain, and dehydration. The differential diagnosis is particularly important in chronic FPIES, as this is an ‘exclusion’ diagnosis. Thus, in order to label a child with ‘chronic’ FPIES, a huge diagnostic workload is necessary.
Differential diagnosis of acute food protein-induced enterocolitis syndrome
When presenting at an emergency room, the patient with acute FPIES is most often misdiagnosed with sepsis. This diagnosis has been considered in 20 publications of case series or reports, more frequently at younger ages (mean age at presentation: 11 months, range 0.5–48 months; Table 1). Sepsis and acute FPIES may share a sudden onset of weakness, vomiting, hyperpnea, tachycardia, neurological impairment, oliguria, and hypotension. Although fever is a cardinal symptom of sepsis, not present in acute FPIES, it can happen that in sepsis – particularly when severe – the body temperature falls below normal values. Laboratory features in acutely presenting FPIES may also mislead to sepsis, as they include extreme leukocytosis, elevated neutrophil count, thrombocytosis, metabolic acidosis, and methemoglobinemia. However, inflammatory indices are normal or slightly elevated, differentiating the two conditions. Faced with a clinical suspicion of a septic status, the emergency room physician will treat the child promptly and aggressively, as indicated in such cases [38]. The treatment will include antibiotics – even before test results confirm the etiologic diagnosis – intravenous fluids to sustain blood pressure, dopamine or epinephrine, oxygen, and sometimes plasma infusion. Of these treatments, the only really effective therapy for FPIES is fluid infusion. However, no complaints by patient parents are reported for overtreatment in the published case series. In our opinion, treating as sepsis an acute presentation of FPIES in an undiagnosed patient, based on the worst case scenario, is wise – at least until rapid diagnostic tests, FPIES-specific, can be developed.
Such ‘therapeutically aggressive’ approaches can become dangerous when the suspicion is an acute surgical abdominal condition. At least two FPIES children are reported being mistakenly diagnosed as having intussusception, which led to nondiagnostic laparotomies [6,12].
The second reported differential diagnosis is acute dehydration from gastroenteritis (16 publications). This condition again occurs normally with fever, starts with vomiting, and ends in diarrhea. Etiologic agents can be identified in the stools [39]. In FPIES there is no fever, sometimes no diarrhea, and stool studies for viruses and bacteria are negative. The clinical evolution of acute FPIES is much more serious and rapid, leading to a severe impairment of the general conditions in a short time. Supportive treatment is all that is needed for most gastrointestinal patients, with oral or intravenous rehydration in particular in infants.
When FPIES occurs in neonates in the first weeks of life, the differential diagnosis with necrotizing enterocolitis (NEC) has been reported. Common symptoms include instability, lethargy, vomiting, diarrhea, and acidosis. In the most severe cases of NEC, the infant develops shock and DIC [40]. As NEC must be treated aggressively with parenteral nutrition, wide-spectrum antibiotics and surgical resection in case of perforated or necrotic intestine, it is important to distinguish it from FPIES. Epidemiologic considerations can be of help: NEC is more common in premature, low birth weight infants; other risk factors include respiratory distress, congenital heart disease, and formula-milk feeding. The pathognomonic sign of NEC is the radiologic finding of pneumatosis intestinalis.
Another condition occasionally reported in the FPIES caseloads is pyloric stenosis, suspected when symptoms of projectile and repetitive vomiting, eventually leading to dehydration and shock, occur in the first week of life [41]. Sometimes pyloric stenosis is associated, at physical examination, with the presence of a firm and nontender mass in the right upper quadrant, described as an ‘olive’. The diagnostic confirmation derives from a noninvasive technique, as ultrasonography scan. After hydroelectrolytic resuscitation, surgical correction is considered the standard of care of pyloric stenosis.
Two reports indicate that FPIES came into the differential diagnosis with allergic proctocolitis. This disease of infancy usually presents by 2 months, can show thrombocytosis [42], and can occur in the early neonatal period, even in preterm infants after the first feed [43]. Infants with allergic proctocolitis may present with rectal bleeding, but are otherwise well and thriving. Their symptoms may be caused by cow's milk, sometimes transferred via the breast milk. The typical presentation is the emission of stools containing mucus and flecks of blood rather than as frank rectal bleeding. Other systemic features (such as failure to thrive or anemia) are usually absent [44]. After some time, this condition vanishes so this is usually a temporary disorder of early childhood. The diagnosis is made on the basis of a response to the exclusion of the offending food, either from the lactating mother's diet or by substitution by extensively hydrolyzed formula. After this, bleeding should resolve in a few days. From these considerations, it is clear that allergic proctocolitis can be easily differentiated from acute FPIES.
Not always an acute presentation of FPIES comes to the attention of an allergist. As indicated in Table 1, anaphylaxis and food allergy are not the most frequently suspected conditions. This is due to the fact that the relation among the ingestion of food and the symptoms can be unclear. The presentation of an anaphylactic reaction in the emergency room can vary widely, but the reaction usually occurs within 1–15 min of exposure to the allergen. Less frequently, reactions can begin after 30 min or even after 1 h, as in FPIES. The anaphylactic patient may feel uneasy and become agitated, with tachycardia and tachypnea. Blood pressure may fall, causing fainting. Other symptoms – including itchy and flushed skin, throbbing in the ears, coughing, sneezing, hives, and swelling (angioedema) – clearly differentiate anaphylaxis from FPIES, which never involves skin [45].
An anaphylactic reaction may progress so rapidly that it leads to collapse, cessation of breathing, seizures, and loss of consciousness within 1–2 min. The reaction may be fatal unless treatment is given immediately. At presentation in the emergency room, anaphylaxis may not be recognized if it is triggered by a novel agent, if it is an individual's first episode, or if it occurs in an infant or young child or in an aphonic, dyspnoeic, or unconscious individual [46].
When the history links it to the ingestion of a specific food, FPIES can be misdiagnosed as IgE-mediated food allergy. To differentiate the two conditions, the main tool is the sensitization test, indicating the presence of specific IgE to foods. FPIES is by definition a non-IgE-mediated food allergy, occasionally evolving to IgE-mediated food allergy [47].
A specific IgE determination and a skin prick test with foods form the basic diagnostic procedure for food allergy, and are necessary in FPIES. An oral food challenge (OFC), an inescapable diagnostic procedure in food allergy, is also recommended for FPIES [7]. However, as for anaphylaxis, an OFC carries intrinsic risks. Thus, in the current clinical practice a clinical history of delayed vomiting with hypotensive episodes after ingestion of a particular food can be considered sufficient to diagnose FPIES [1].
Differential diagnosis of chronic food protein-induced enterocolitis syndrome
In cases of ‘chronic’ FPIES, the differential diagnosis is even more difficult. The diagnostic boundaries, in particular with other non-IgE-mediated gastrointestinal food allergies are blurred, and it is difficult to differentiate this condition from them. This underlines the need for a precise definition. In any case, in the literature the most frequently involved conditions are gastrointestinal and food allergy (Table 2[12–19,21,22,24,26,27,29,30,31▪▪,32,34,36,48,49,50▪,51▪]).
Table 2.
Differential diagnosis in reported cases of chronic food protein-induced enterocolitis syndrome
| Year | Ref | Gastrointestinal | Metabolic | PIDs | Allergic | Other |
| 1963 | [12] | CD | FA | |||
| 1982 | [48] | CD | ||||
| 1992 | [13] | MD | FA | dα-1AT | ||
| 1996 | [14] | FA | ||||
| 1998 | [15] | CD, EoEC, EoG | ||||
| 2000 | [16] | CD, IBD, GEF, EoG | ||||
| 2003 | [17] | MD | NeS | |||
| 2003 | [18] | Hy, UCD | PID | |||
| 2004 | [49] | CD, EoE, EoG | FA | |||
| 2005 | [19] | EoEC, EoG, MIR | MD | |||
| 2006 | [21] | |||||
| MD | ||||||
| 2006 | [22] | MD | ||||
| 2007 | [6] | EoG | CoaD | |||
| 2008 | [24] | HFI | ||||
| 2009 | [3] | FA | ||||
| 2010 | [26] | EoG, EoEC | ||||
| 2011 | [27] | EoE, EoG, EoEC | ||||
| 2011 | [29] | MD | FA | Ht | ||
| 2011 | [30] | FA | ||||
| 2012 | [31▪▪] | MD | ||||
| 2012 | [32] | FA | ||||
| 2012 | [34] | FA | ||||
| 2013 | [36] | FAv | ||||
| 2014 | [50▪] | HFI | ||||
| 2014 | [51▪] | TMAU |
CD, celiac disease; CoaD, coagulation defect; dα-1AT, α-1 antitrypsin deficiency; EoE, eosinophilic esophagitis; EoEC, eosinophilic enterocolitis; EoG, eosinophilic gastritis; FA, food allergy; FAv, food aversion; GEF, gastroesophageal reflux; HFI, hereditary fructose intolerance; Hy, hyperammonemia; Ht, hypotension; IBD, inflammatory bowel disease; MD, metabolic disorders; NEC, necrotizing enterocolitis; PID, primary immunodeficiency; TMAU, trimethylaminuria; UCD, urea cycle defect.
The symptomatic similarities of allergic eosinophilic esophagitis (EoE) with chronic FPIES are postprandial vomiting, diarrhea, occasional blood loss, iron deficiency anemia, and possible protein-losing enteropathy [52]. This allergic inflammatory condition of the esophagus is characterized also by swallowing difficulty, food impaction, refusal of food, difficulty in infant feeding, poor weight gain, and poor response to standard antireflux treatment; dietetic management is important [53]. Practically, all the clinical features of infants with allergic enteropathy are common to ‘chronic’ FPIES. Diarrhea, failure to thrive, various degrees of vomiting, and, sometimes, hypoproteinemia, and anemia can be present in children emitting stools that contain not only blood but also neutrophils [54]. Mild anemia may progress to significant anemia associated with hypoproteinemia due to protein-losing enteropathy; this is confirmed by increased fecal α-1 antitrypsin. These clinical characteristics are present with different grades both in eosinophilic enterocolitis (EoC) and in eosinophilic gastritis (EoG) and the offending foods are the same as for FPIES. In our opinion, despite the fact that EoC and EoG are listed in the differential diagnosis of FPIES, there is no clear distinction among these allergic entheropaties and chronic FPIES.
In some cases, celiac disease came into differential diagnosis with FPIES (Table 2). Common features of celiac disease may include diarrhea, abdominal distention, symptoms of malnutrition such as short stature, anemia, defects in dentition, failure to thrive, or developmental delay. Some of these are common to chronic forms of FPIES; IgA antitransglutaminase is the standard of diagnosing and screening for celiac disease [55].
The inborn errors of metabolism are frequently reported in the differential diagnosis of FPIES. Urea cycle defects, organic acidemias, certain disorders of amino acid metabolism, and some inherited disorders of energy metabolism may present in infancy with general malaise and/or with sudden neurological deterioration [56]. Symptoms such as lethargy, apnea or tachypnea, and vomiting are the result of toxic effects of accumulating metabolites on the central nervous system; they represent an acute presentation of a chronic condition. In such cases, a handful of routine laboratory tests can give a rapid clinical indication:
Blood: Blood count, serum glutamic oxaloacetic transaminase, serum glutamic pyruvic transaminase, creatine kinase, electrolytes, uric acid, blood urea nitrogen and creatinine, glucose, phosphate, acid-base status, bicarbonate, anion gap, lactate ammonia determination;
Urine: Specific gravity, ketones.
If the clinician is oriented toward a metabolic condition, these few simple tests, combined with the list of metabolic diseases that may present with clinical and biochemical features resembling those of FPIES provided in Table 3, should give an indication at the onset. In case of strong suspicion, a metabolic specialist should be alerted without delay.
Table 3.
Differential diagnosis between inborn errors of metabolism in patients presenting with acute clinical deterioration
| Parameter | FPIES | UCD | PA/MMA | HMG | KT | MSUD | β-OX | HI-HA | PDH | MITO |
| Ammonia | ↑ | ↑ | ↑ | ↑ | ↑ | ±↑ | ||||
| Acidosis | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ||||
| Glucose | ±↑ | ↓ | ±↓ | ↓ | ↓ | ±↓ | ||||
| Lactate | ↑ | ↑ | ↑ | ↑ | ↑ | |||||
| SGOT/SGPT | ↑ | ↑ | ±↑ | |||||||
| CK | ↑ | ±↑ | ||||||||
| Uric acid | ↑ | ↑ | ↑ | ↑ | ↑ | ±↑ | ↑ | |||
| WBC | ↑ | ↓ | ||||||||
| Ketonuria | ↑ | ↑ | ↑ | ↑ |
β-OX, beta oxidation defects; CK, creatine kinase; FPIES, food protein-induced enterocolitis syndrome; HI-HA, hyperinsulinism hyperammonemia syndrome; HMG, hydroxymethylglutaric aciduria; KT, ketothiolase deficiency; MITO, mitochondrial disorders; MSUD, maple syrup urine disease; PA/MMA, propionic/methylmalonic aciduria; PDH, pyruvate dehydrogenase deficiency; SGOT, Serum Glutamic Oxaloacetic Transaminase; SGPT, Serum Glutamic Pyruvic Transaminase; UCD, urea cycle defects; WBC, white blood cell.
Recently, a specific metabolic differential diagnosis emerged. When FPIES is due to fruit, acute symptoms after fruit consumption are generally interpreted as hereditary fructose intolerance (HFI). The clinical presentation of the two conditions can be similar, so a careful evaluation of laboratory data is necessary. When atypical cases of HFI do not fulfil the ‘canonical’ diagnostic criteria, it has been suggested to involve an allergist [51▪].
Another metabolic disease involved in FPIES is trimethylaminuria (TMAU), an autosomal recessive disorder caused by excessive excretion into body fluids and breath of unoxidized trimethylamine (TMA) derived from the enterobacterial metabolism of dietary precursors. A case was described in which FPIES episodes (from rice, oat, and banana) produced a fish-like odor, typical of superfluous excretion of TMA [52].
In one report, FPIES in the chronic phase generated a clinical suspicion of primary immunodeficiency disease (PID) [18].
In our experience, such a differential diagnosis is not exceptional (see infra). Considering that the gastrointestinal tract is the largest lymphoid organ in the body, continuously exposed to antigen derived from food and bacteria [57], it is not surprising that many children with primary immunodeficiencies develop gastrointestinal symptoms [58]. Note the gastrointestinal manifestations may be the initial presentation of PID. Therefore, a careful history and evaluation should be carried out to exclude an underlying immunologic disorder.
A detailed list of the main gastrointestinal disorders reported in these patients is described in Table 4. From all these considerations, it appears that the possible differential diagnosis of chronic FPIES is very wide. It also includes psychosocial (Munchausen by proxy syndrome, food aversion), neurological, and infectious (e.g. HIV, Salmonella, Yersinia) conditions. Although the clinical definition is vague, chronic FPIES is a factual entity in children not recognized for the syndrome, when they freely consume the offending food(s). In this situation, infants may incur the odyssey of FPIES.
Table 4.
Gastrointestinal manifestations in primary immunodeficiencies [58]
| Immunodeficiency | Evaluation with clinically significant result | Gastrointestinal manifestation |
| Common variable immunodeficiency | Quantitative immunoglobulins → reduced serum IgG and IgA and/or IgM; antibody response (IgG) to vaccination → poor, nonprotective; lymphocyte subsets → normal or reduced B cell numbers | Diarrhea, nodular lymphoid hyperplasia, flat villous lesions, IBD-like disease, pernicious anemia |
| Selective IgA deficiency | Quantitative immunoglobulins → serum IgA absent or near absent usually <10 mg/dl; normal IgG and IgM levels though IgG2 subclass deficiency may be present | Diarrhea, celiac sprue, nodular lymphoid hyperplasia |
| Agammaglobulinemia, X-linked or autosomal recessive | Quantitative immunoglobulins → reduced serum levels of all immunoglobulins; antibody response (IgG) to vaccination → poor, nonprotective; lymphocyte subsets → normal numbers of pro-B cells; reduced/absent B cells | Gastrointestinal disorders rare, chronic diarrhea, malabsorption |
| X-linked hyper IgM syndrome | Quantitative immunoglobulins → normal to elevated IgM levels; low IgG and IgA; antibody response (IgG) to vaccination → poor, nonprotective; lymphocyte subsets → normal T cell numbers; B cell numbers are normal or slightly reduced | Diarrhea, progressive liver disease, sclerosing cholangitis |
| Severe combined immunodeficiency | Lymphocyte subsets → markedly diminished T cells; variable B cell and natural killer cell numbers depending on functional deficiency; in vitro assay of lymphocyte function → diminished response to mitogens-PHA, ConA, PWM | Diarrhea, oral candidiasis |
| DiGeorge syndrome | Quantitative immunoglobulins → immunoglobulins are usually normal though occasionally IgE is elevated and IgA may be reduced; lymphocyte subsets → variable decreases in T lymphocytes; B and natural killer cells are normal or elevated; in vitro assay of lymphocyte function → variable lymphocyte response to mitogens depending on thymic deficiency | Mucocutaneous candidiasis |
| Immune dysregulation, polyendocrinopathy, enteropathy syndrome | Complete blood count → eosinophilia; quantitative immunoglobulins → may have increased serum IgE and IgA; lymphocyte subsets → CD4+CD25+ T cells are reduced most patients with FOXP3 mutations have markedly decreased or absent FOXP3+ Tregs; otherwise normal T cell and B cell subsets; in vitro assay of lymphocyte function → specific antigens are normal or slightly decreased | Severe enteropathy with watery often bloody diarrhea associated with eosinophilic inflammation |
| Bare lymphocyte syndrome | Quantitative immunoglobulins → variable reductions; antibody response (IgG) to vaccination → poor, nonprotective; lymphocyte subsets → low numbers of CD4+ T cells with proportional increases in CD8+ T cells; flow cytometry-diminished expression of MHC; in vitro assay of lymphocyte function → impaired antigen specific responses | Progressive liver disease, sclerosing cholangitis |
| Chronic granulomatous disease | Dihydrorhodamine reductase or nitroblue tetrazolium → diminished respiratory burst in neutrophils | Colitis, hepatic abscess, gastric outlet obstruction, small bowel obstruction, granulomatous stomatitis, oral ulcers, esophageal dysmotility |
| Wiskott–Aldrich syndrome | Complete blood count → platelet numbers are reduced and small in size; quantitative immunoglobulins → variable concentrations secondary to accelerated synthesis and catabolism of Igs (usually low IgM, elevated IgA and IgE, and normal or slightly low IgG); antibody response (IgG) to vaccination → impaired antibody response; lymphocyte subsets → moderate reductions in percentages of CD3+, CD4+, and CD8+ bearing T cells; in vitro assay of lymphocyte function → impaired lymphocyte response to mitogens | Colitis, bloody diarrhea, malabsorption |
| Hermansky–Pudlak syndrome | Complete blood count → normal platelet count; coagulation studies → prolonged bleeding time, with abnormal platelet function assays | Granulomatous colitis |
IBD, inflammatory bowel disease; ConA, concanavalin A; FOXP3, forkhead box P3; MHC, major histocompatibility complex; PHA, phytohaemagglutinin; PWM, pokeweed mitogen.
Adapted from [58].
THE ODYSSEY OF FOOD PROTEIN-INDUCED ENTEROCOLITIS SYNDROME CHILDREN
To exemplify the difficulties in the differential diagnosis of FPIES, we performed a retrospective evaluation of clinical records of children diagnosed with FPIES [59]. Between August 2012 and April 2013, three patients were diagnosed with FPIES from rice, apple, and fish. They had been admitted with acute symptoms including vomiting, pallor, and asthenia. One had dehydration and diarrhea, none had fever. Two were admitted with a suspicion of sepsis, treated with antibiotics, steroids, and plasma. They had two, three, and four episodes, respectively, before diagnosis. After their stay in the emergency room, each child was admitted in a different ward: immunology, metabolic diseases, and general pediatrics. During their hospital stay, diagnostic evaluations included the specialists reported in Table 5. The table also includes the suspected conditions for which the specialists ordered supplemental diagnostic tests.
Table 5.
Detail of differential diagnoses considered for three children admitted after an acute episode of food protein-induced enterocolitis
| Specialist | Suspect | Number of patients | Specialist | Suspect | Number of patients |
| Gastrointestinal | Meckel's diverticulum, intussusception, congenital microvillus atrophy, pyloric stenosis | 2/3 | Anesthetist | Hypotension, tachycardia, arrhythmia, hyperpnea | 2/3 |
| Pediatric surgeon | Pyloric stenosis | 2/3 | Metabolic disease specialist | Metabolic acidosis, Hereditary fructose intolerance | 2/3 |
| Immunologist | IPEX, primary immunodeficiency | 1/3 | Endocrinologist | Adrenal insufficiency | 1/3 |
| Cardiologist | Congenital cardiopathy | 1/3 | Hematologist | Anemia, methemoglobinemia | 2/3 |
| Neurologist | Seizures, intracranial hemorrhage | 1/3 | Dietician | Enteral nutrition | 1/3 |
| Allergist | Anaphylaxis | 3/3 | Infectious disease specialist | Sepsis | 3/3 |
| HIV | 1/3 |
IPEX, immune dysregulation, polyendocrinopathy, enteropathy, X-linked.
The time lapse between the first episode and the diagnosis was 8 ± 2 months (with a median of three acute events before reaching the diagnosis). This illustrates how wide the spectrum of possible differential diagnoses can be, when a relatively simple clinical history could solve the problem. For this reason, we share the vision that educational interventions on FPIES are needed for hospital-based pediatricians to shorten the time lapse between the first episode and the diagnosis [2].
CONCLUSION
The risks of a late diagnosis are concrete for FPIES. The longer the delay, the greater the risk of unuseful diagnostic evaluations and erroneous treatments. These will entail costs and risks. FPIES is relatively easy to treat, and its diagnosis is relatively easy: knowing it is all that is needed. The effect of appropriate informative interventions has been described [60]. Thus, educational interventions on FPIES are needed for hospital-based pediatricians and general practitioners to shorten the time lapse between the first episode and the diagnosis [2].
Acknowledgements
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Feuille E, Nowak-Węgrzyn A. Definition, etiology, and diagnosis of food protein-induced enterocolitis syndrome. Curr Opin Allergy Clin Immunol 2014; 14:222–228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schultz F, Westcott-Chavez A. Food protein-induced enterocolitis syndrome from the parent perspective. Curr Opin Allergy Clin Immunol 2014; 14:263–267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehr S, Kakakios A, Frith K, Kemp AS. Food protein-induced enterocolitis syndrome: 16-year experience. Pediatrics 2009; 123:e459–e464 [DOI] [PubMed] [Google Scholar]
- 4.Powell GK. Food protein-induced enterocolitis of infancy: differential diagnosis and management. Compr Ther 1986; 12:28–37 [PubMed] [Google Scholar]
- 5.Leonard SA. Food protein-induced enterocolitis syndrome: an update on natural history and review of management. Ann Allergy Asthma Immunol 2011; 107:95–101 [DOI] [PubMed] [Google Scholar]
- 6.Jayasooriya S, Fox AT, Murch SH. Do not laparotomize food protein-induced enterocolitis syndrome. Pediatr Emerg Care 2007; 23:173–175 [DOI] [PubMed] [Google Scholar]
- 7.Boyce JA, Assa’ad A, Burks AW, et al. Guidelines for the diagnosis and management of food allergy in the United States: summary of the NIAID-sponsored expert panel report. J Allergy Clin Immunol 2010; 126:1105–1118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sackeyfio A, Senthinathan A, Kandaswamy P, et al. Guideline Development Group Diagnosis and assessment of food allergy in children and young people: summary of NICE guidance. BMJ 2011; 342:d747. [DOI] [PubMed] [Google Scholar]
- 9.Fiocchi A, Brozek J, Schunemann H, et al. World Allergy Organization (WAO) Diagnosis and Rationale for Action against Cow's Milk Allergy (DRACMA) Guidelines. Pediatr Allergy Immunol 2010; 21 Suppl 21:1–125 [DOI] [PubMed] [Google Scholar]
- 10.Meyer R, Fleming C, Dominguez-Ortega G, et al. Manifestations of food protein induced gastrointestinal allergies presenting to a single tertiary paediatric gastroenterology unit. World Allergy Organ J 2013; 6:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mane SK, Bahna SL. Clinical manifestations of food protein-induced enterocolitis syndrome. Curr Opin Allergy Clin Immunol 2014; 14:217–221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ikola RA. Severe intestinal reaction following ingestion of rice. Am J Dis Child 1963; 105:281–284 [DOI] [PubMed] [Google Scholar]
- 13.Borchers SD, Li BU, Friedman RA, McClung HJ. Rice-induced anaphylactoid reaction. J Pediatr Gastroenterol Nutr 1992; 15:321–324 [DOI] [PubMed] [Google Scholar]
- 14.Cavataio F, Carroccio A, Montalto G, Iacono G. Isolated rice intolerance: clinical and immunologic characteristics in four infants. J Pediatr 1996; 128:558–560 [DOI] [PubMed] [Google Scholar]
- 15.Sicherer SH, Eigenmann PA, Sampson HA. Clinical features of food protein-induced enterocolitis syndrome. J Pediatr 1998; 133:214–219 [DOI] [PubMed] [Google Scholar]
- 16.Sicherer SH. Food protein-induced enterocolitis syndrome: clinical perspectives. J Pediatr Gastroenterol Nutr 2000; 30:S45–S49 [DOI] [PubMed] [Google Scholar]
- 17.Nowak-Wegrzyn A, Sampson HA, Wood RA, Sicherer SH. Food protein-induced enterocolitis syndrome caused by solid food proteins. Pediatrics 2003; 111:829–835 [DOI] [PubMed] [Google Scholar]
- 18.Levy Y, Danon YL. Food protein-induced enterocolitis syndrome – not only due to cow's milk and soy. Pediatr Allergy Immunol 2003; 14:325–329 [DOI] [PubMed] [Google Scholar]
- 19.Sicherer SH. Food protein-induced enterocolitis syndrome: case presentations and management lessons. J Allergy Clin Immunol 2005; 115:149–156 [DOI] [PubMed] [Google Scholar]
- 20.Zapatero Remón L, Alonso Lebrero E, Martín Fernández E, Martínez Molero MI. Foodprotein-induced enterocolitis syndrome caused by fish. Allergol Immunopathol 2005; 3:312–316 [DOI] [PubMed] [Google Scholar]
- 21.Anand RK, Appachi E. Case report of methemoglobinemia in two patients with food protein-induced enterocolitis. Clin Pediatr 2006; 45:679–682 [DOI] [PubMed] [Google Scholar]
- 22.Hojsak I, Kljaić-Turkalj M, Misak Z, Kolacek S. Rice protein-induced enterocolitis syndrome. Clin Nutr 2006; 25:533–536 [DOI] [PubMed] [Google Scholar]
- 23.Maloney J, Nowak-Wegrzyn A. Educational clinical case series for pediatric allergy and immunology: allergic proctocolitis, food proteininduced enterocolitis syndrome and allergic eosinophilic gastroenteritis with protein-losing gastroenteropathy as manifestations of non IgE mediated cow's milk allergy. Pediatr Allergy Immunol 2007; 18:360–367 [DOI] [PubMed] [Google Scholar]
- 24.Bruni F. Fruit proteins: another cause of food protein-induced enterocolitis syndrome. Allergy 2008; 63:1645–1646 [DOI] [PubMed] [Google Scholar]
- 25.Chaabane M, Bidat E, Chevallier B. Syndrome d’entérocolite induit par les proteins alimentaires, a‘ propos d’une observation. A new case of food protein-induced enterocolitis syndrome. Arch Pediatr 2010; 17:502–506 [DOI] [PubMed] [Google Scholar]
- 26.Jones KDJ, Noimark L, Osborn M, et al. A case of severe atypical food protein induced enterocolitis syndrome. Allergy 2010; 65:1061–1063 [DOI] [PubMed] [Google Scholar]
- 27.Caubet JC, Nowak-Wegrzin A. Food protein-induced enterocolitis to hen's egg. J Allergy Clin Immunol 2011; 128:1386–1388 [DOI] [PubMed] [Google Scholar]
- 28.Katz Y, Goldberg MR, Rajuan N, et al. The prevalence and natural course of food protein-induced enterocolitis syndrome to cow's milk: a large-scale, prospective population-based study. J Allergy Clin Immunol 2011; 127:647–653e1–e3 [DOI] [PubMed] [Google Scholar]
- 29.Coates RW, Weaver KR, Lloyd R, et al. Food protein-induced enterocolitis syndrome as a cause for infant hypotension. West J Emerg Med 2011; 12:512–514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Onesimo R, Dello Iacono I, Giorgio V, et al. Can food protein induced enterocolitis syndrome shift to immediate gastrointestinal hypersensitivity? A report of two cases. Eur Ann Allergy Clin Immunol 2011; 43:61–63 [PubMed] [Google Scholar]
- 31▪▪.Sopo SM, Giorgio V, Dello Iacono I, et al. A multicentre retrospective study of 66 Italian children with food protein-induced enterocolitis syndrome: different management for different phenotypes. Clin Exp Allergy 2012; 42:1257–1265 [DOI] [PubMed] [Google Scholar]; An Italian collection of FPIES patiens’ data ackowledging the need to define a uniformity in diagnosis and management of the disease.
- 32.Fernandes BN, Boyle RJ, Gore C, et al. Food protein-induced enterocolitis syndrome can occur in adults. J Allergy Clin Immunol 2012; 130:1199–1200 [DOI] [PubMed] [Google Scholar]
- 33.Sopo SM, Filoni S, Giorgio V, et al. Food protein-induced enterocolitis syndrome (FPIES) to corn: a case report. J Investig Allergol Clin Immunol 2012; 22:391–392 [PubMed] [Google Scholar]
- 34.Federly TJ, Ryan P, Dinakar C. Food protein-induced enterocolitis syndrome triggered by orange juice. Ann Allergy Asthma Immunol 2012; 109:472–473 [DOI] [PubMed] [Google Scholar]
- 35.Mane SK, Hollister ME, Bahna SL. Food protein-induced enterocolitis syndrome to trivial oral mucosal contact. Eur J Pediatr 2013; Epub ahead of print [DOI] [PubMed] [Google Scholar]
- 36.Miceli Sopo S, Greco M, Monaco S, et al. Food protein-induced enterocolitis syndrome, from practice to theory. Expert Rev Clin Immunol 2013; 9:707–715 [DOI] [PubMed] [Google Scholar]
- 37.Ranzato C, Piacentini GL, Comberiati P, et al. Unusual shift from IgE-mediated milk allergy to food protein-induced enterocolitis syndrome. Eur Ann Allergy Clin Immunol 2013; 45:209–211 [PubMed] [Google Scholar]
- 38.Kuehn BM. Guideline promotes early, aggressive sepsis treatment to boost survival. JAMA 2013; 309:969–970 [DOI] [PubMed] [Google Scholar]
- 39.Parashar UD, Nelson EA, Kang G. Diagnosis, management, and prevention of rotavirus gastroenteritis in children. BMJ 2013; 347:f7204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Neu J, Walker WA. Necrotizing enterocolitis. N Engl J Med 2011; 364:255–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pandya S, Heiss K. Pyloric stenosis in pediatric surgery: an evidence-based review. Surg Clin North Am 2012; 92:527–539 [DOI] [PubMed] [Google Scholar]
- 42.Fretzayas A, Moustaki M, Priftis KN, et al. Thrombocytosis as an overt sign of cow's milk allergic proctocolitis. Allergol Immunopathol (Madr) 2011; 39:381–383 [DOI] [PubMed] [Google Scholar]
- 43.Faber MR, Rieu P, Semmekrot BA, et al. Allergic colitis presenting within the first hours of premature life. Acta Paediatr 2005; 94:1514–1515 [DOI] [PubMed] [Google Scholar]
- 44.Fiocchi A, Brozek J, Schunemann HJ, et al. World Allergy Organization (WAO) Diagnosis and Rationale for Action against Cow's Milk Allergy (DRACMA) Guidelines. WAO Journal 2010; 3:57–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Simons FE, Ardusso LR, Bilò MB, et al. World Allergy Organization World Allergy Organization guidelines for the assessment and management of anaphylaxis. World Allergy Organ J 2011; 4:13–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Martelli A, Ghiglioni D, Sarratud T, et al. Anaphylaxis in the emergency department: a paediatric perspective. Curr Opin Allergy Clin Immunol 2008; 8:321–329 [DOI] [PubMed] [Google Scholar]
- 47.Katz Y, Goldberg MR. Natural history of food protein-induced enterocolitis syndrome. Curr Opin Allergy Clin Immunol 2014; 14:229–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vitoria JC, Camarero C, Sojo A, et al. Enteropathy related to fish, rice, and chicken. Arch Dis Child 1982; 57:44–48 [PMC free article] [PubMed] [Google Scholar]
- 49.Gray HC, Foy TM, Becker BA, Knutsen AP. Rice-induced enterocolitis in an infant: TH1/TH2 cellular hypersensitivity and absent IgE reactivity. Ann Allergy Asthma Immunol 2004; 93:601–605 [DOI] [PubMed] [Google Scholar]
- 50▪.Fiocchi A, Dionisi-Vici C, Cotugno G, et al. Fruit-induced FPIES masquerading as Hereditary Fructose Intolerance. Pediatrics 2014; in press [DOI] [PubMed] [Google Scholar]; The clinical story of an infant boy offers a clinical lesson suggesting the pediatricians do modify their diagnostic standards in the field of metabolic diseases. When a suspect of hereditary fructose intolerance comes out, pediatricians are advised to also consider FPIES in the differential diagnosis.
- 51▪.Miller NB, Beigelman A, Utterson E, Shinawi M. Transient massive trimethylaminuria associated with food protein-induced enterocolitis syndrome. JIMD Rep 2014; 12:11–15 [DOI] [PMC free article] [PubMed] [Google Scholar]; This clinical case illustrates the possible interplay between a metabolic condition, the so-called ‘fish odor syndrome’, and FPIES. It suggests that the metabolic aspects of FPIES could be of importance.
- 52.Rothenberg ME, Aceves S, Bonis PA, et al. Working with the US Food and Drug Administration: progress and timelines in understanding and treating patients with eosinophilic esophagitis. J Allergy Clin Immunol 2012; 130:617–619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Davis BP, Rothenberg ME. Emerging concepts of dietary therapy for pediatric and adult eosinophilic esophagitis. Expert Rev Clin Immunol 2013; 9:285–287 [DOI] [PubMed] [Google Scholar]
- 54.Ingle SB, Hinge Ingle CR. Eosinophilic gastroenteritis: an unusual type of gastroenteritis. World J Gastroenterol 2013; 19:5061–5066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Husby S, Koletzko S, Korponay-Szabó IR, et al. ESPGHAN Working Group on Coeliac Disease Diagnosis; ESPGHAN Gastroenterology Committee; European Society for Pediatric Gastroenterology, Hepatology, and Nutrition European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease. J Pediatr Gastroenterol Nutr 2012; 54:136–160 [DOI] [PubMed] [Google Scholar]
- 56.Grünewald S, Davison J, Martinelli D. Blau N, Duran M, Gibson KM, Dionisi-Vici C, et al. Emergency Diagnostic Procedures and Emergency Treatment. Physician's guide to the diagnosis, treatment, and follow-up of inherited metabolic diseases. Berlin Heidelberg:Springer-Verlag; 2014. 709–718 [Google Scholar]
- 57.Agarwal S, Mayer l. Gastrointestinal manifestations in primary immune disorders. Inflamm Bowel Dis 2010; 16:703–711 [DOI] [PubMed] [Google Scholar]
- 58.Guerriero A, Frischmeyer-Guerriero PA, Lederman HM, Hemker MO. Recognizing gastrointestinal and hepatic manifestations of primary immunodeficiency diseases. J Pediatr Gastroenterol Nutr 2010; 51:548–555 [DOI] [PubMed] [Google Scholar]
- 59.Fiocchi A, Dahdah L, Mazzina O, et al. The odyssey of FPIES children. Abstract, European Academy of Allergy and Clinical Immunology 2014 Annual Congress, Copenhagen 7–11th June 2014 [Google Scholar]
- 60.Dahdah L, Fiocchi A, Mazzina O, et al. FPIES: effects of educational intervention in an Italian children hospital. Abstract, European Academy of Allergy and Clinical Immunology 2014 Annual Congress, Copenhagen 7–11th June 2014 [Google Scholar]


