Abstract
Purpose of review
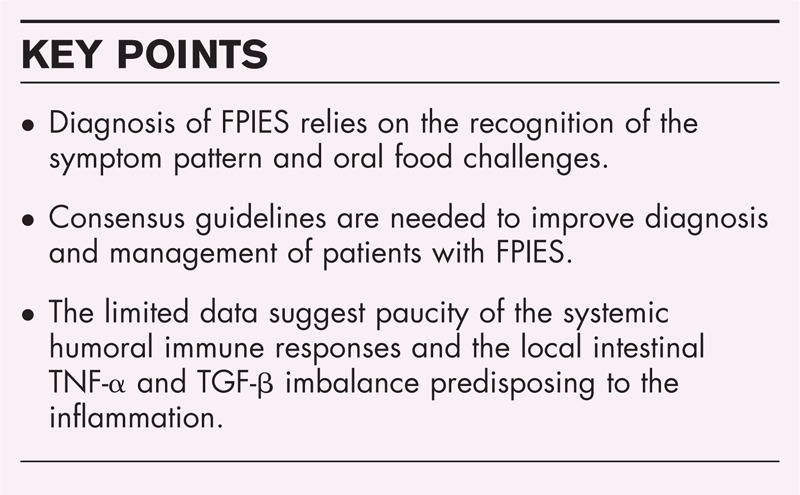
Food protein-induced enterocolitis syndrome (FPIES) is a poorly understood non-IgE-mediated food hypersensitivity, primarily affecting infants and toddlers. There are few data regarding pathophysiology of FPIES that suggest local intestinal imbalance between TNF-α and TGF-β. Patients frequently present with multiple reactions, which are characterized by projectile, repetitive emesis, dehydration, lethargy, and failure to thrive. Despite the severity of presentation, the diagnosis is frequently delayed, and patients often undergo extensive and invasive evaluation prior to reaching the diagnosis.
Recent findings
Reviews published in the last year provide a general approach to diagnosis and management of FPIES and aim to increase awareness and understanding of FPIES among general pediatricians.
Summary
Multicenter studies are necessary to reevaluate and modify the oral food challenge criteria. Research on the pathophysiology of FPIES reactions is necessary to provide insight into the evidence-based approach to diagnosis and management of FPIES. Registries are needed to understand the phenotype, triggers, and prevalence of FPIES.
Keywords: allergic enterocolitis, food allergy, food protein-induced enterocolitis syndrome
INTRODUCTION
Food protein-induced enterocolitis syndrome (FPIES) is a non-IgE-mediated food hypersensitivity that usually presents in infancy with profuse vomiting, sometimes accompanied by diarrhea. In the acute form, when food is ingested on an intermittent basis or following a period of avoidance, FPIES typically presents with profuse vomiting, diarrhea, and dehydration, starting 1–3 h following food ingestion [1]. Increased neutrophil count, increased platelet count, and methemoglobulinemia may be observed. In the chronic form, when food is ingested frequently, FPIES presents with intermittent vomiting, diarrhea, weight loss, and failure to thrive [2▪]. FPIES is diagnosed based on history and typical symptoms that improve with food avoidance, and exclusion of other etiologies. Oral food challenge (OFC) remains the gold standard for FPIES diagnosis. The majority of patients with FPIES because of cow's milk and soy resolve within the first years of life; solid food FPIES or FPIES associated with positive food-specific IgE may have a more protracted course.
HISTORICAL PERSPECTIVE
In 1940, Rubin [3] reported intestinal bleeding due to cow's milk allergy in newborns. Gryboski and Powell et al.[4–7] described infants presenting in the first 6 weeks of life with recurrent vomiting, bloody diarrhea, and abdominal distension while being fed with cow's milk-based formula. They appeared dehydrated and severely ill; sepsis evaluations were negative. Improvement was achieved with intravenous fluids or hydrolyzed casein-based formula, but not with soy-based formula. Feeding with the cow's milk-based formula caused recurrence of severe emesis within 1–3 h and elevation of the peripheral neutrophil count, peaking at about 6 h following food ingestion. Powell [8] characterized major features of the disorder, established criteria for the diagnosis of cow's milk-induced enterocolitis, and established a standard challenge protocol. Reports of series of infants with FPIES by Sicherer et al.[9] (16 patients) and Burks et al.[10] (43 patients) further characterized clinical features and refined food challenge protocols. Additional reports identified solid foods such as cereal grains, vegetables, meats, and fish as triggers for FPIES [11–19].
Box 1.
no caption available
CLINICAL MANIFESTATIONS
FPIES may present in either acute or chronic form, as discussed in detail in another article in this issue of Current Opinion in Allergy and Clinical Immunology[20–25,26▪▪]. There are no classic allergic symptoms from the skin or respiratory tract in either form of FPIES.
INCITING FOODS
The most common triggers are cow's milk and soy formulas and rice in young infants. FPIES may also occur upon ingestion of solid foods, including grains (rice, oats, barley, corn), meat and poultry (beef, chicken, turkey), egg white, vegetables (white potato, sweet potato, squash, string bean), fruit (tomato), legumes (peanut, green pea, lentil), seafood (fish, crustaceans, molluscs, usually with onset in older children and adults), and the probiotic Saccharomyces boulardii[7,9,14,16,17,19,22,27–30].
It is generally accepted that ingestion of a food is necessary for sensitization and reaction to a food protein. Recently, a 5.5-month-old infant, exclusively breast-fed, who developed emesis and lethargy after chewing on the wrapper of a rice cake was reported [31]. After reoccurrence of symptoms with introduction of rice into his diet, he was diagnosed with rice FPIES. The case suggests that sensitization in FPIES can occur through breast milk alone and that the food amount required to trigger FPIES reaction can be quite low.
PATHOPHYSIOLOGY OF FOOD PROTEIN-INDUCED ENTEROCOLITIS SYNDROME
The mechanisms through which FPIES develops are as yet unclear. FPIES is often considered to be a T-cell-mediated disorder; however, only a handful of studies [32–38] have investigated T cells in FPIES with inconclusive results (Table 1). Humoral responses in FPIES are not well understood.
Table 1.
Studies that investigated T-cell responses in food protein-induced enterocolitis syndrome and non-IgE-mediated food allergy
| Study | Findings |
| Van Sickle et al. [32] | In children with confirmed FPIES, peripheral blood mononuclear cell (PBMC) stimulation by the causal antigen induced greater cell proliferation than in children with negative oral food challenge |
| Hoffman et al. [33] | Higher lymphocyte proliferative response in affected children was observed, but the stimulation index was not significantly different compared with the control group |
| Heyman et al. [34] | The high level of TNF-α released by antigen-specific T cells acts synergistically with IFN-γ to increase intestinal permeability. This may contribute to the influx of antigens into the submucosa with further activation of antigen-specific T cells |
| Benlounes et al. [35] | Intact rather than intestinally processed proteins stimulate PBMC to release TNF-α. The threshold for PBMC reactivity to milk antigens decreases considerably during active cow's milk allergy with intestinal symptoms compared with patients whose sensitivity resolved or with those with skin rather than intestinal manifestation of cow's milk hypersensitivity. In-vitro kinetic studies differed in these groups, with those having active disease showing two peaks in TNF-α elaboration. The second peak occurred after 5 days of culture |
| Chung et al. [36] | There was higher staining for TNF-α in infants with FPIES and with villous atrophy compared with those without villous atrophy, and with the control group. Type 1, but not type 2, receptor for TGF-β was decreased in duodenal biopsy specimens in FPIES patients compared with controls |
| Mori et al. [37] | In a case of FPIES to rice, authors described an increase in IL-4 and decrease in IFN-γ expression in T cells after a positive oral challenge with rice. After the patient had acquired tolerance, there was an increase in IL-10 expression in CD3+ cells, as well as an increase in IFN-γ before and after the challenge |
| Karlsson et al. [38] | Children outgrowing non-IgE-mediated hypersensitivity to cow's milk following a period of dairy-free diet were compared to children with active non-IgE-mediated hypersensitivity to cow's milk protein. The results revealed a higher frequency of circulating CD4+CD25+ Treg cells specific for cow's milk protein in children outgrowing non-IgE-mediated hypersensitivity to cow's milk protein. The suppressive action of cow's milk-specific Treg cells was exerted partly by direct cell–cell contact and partly by production of TGF-β |
Cell-mediated immune responses
While there is some evidence of T-cell proliferation upon stimulation with food antigens, the stimulation index is not consistently different from control, nonallergic subjects [39]. It is hypothesized that T-cell activation by food allergens may mediate local intestinal inflammation through release of proinflammatory cytokines, causing increased intestinal permeability and fluid shifts [39,40]. This local inflammation may be mediated by activated peripheral mononuclear cells, increased TNF-α, and decreased expression of TGF-β receptors in the intestinal mucosa [23]. However, baseline antigen absorption is normal and does not predispose to FPIES [41]. Methomoglobinemia described in case of severe acute FPIES have been attributed to the local intestinal inflammation [24].
Neutrophils, platelets, and eosinophils
Powell reported leukocytosis with a left shift as a common finding for patients presenting with acute FPIES and included it as one of the diagnostic criteria. In the Powell study, peripheral blood neutrophil counts were elevated in all positive challenges, peaking at 6 h with a mean increase of 9900 cells/μl. These results were confirmed by subsequent studies [8]. Neutrophils have also been found in stool mucous of FPIES patients. This increase in peripheral neutrophils is likely due to the secretion of different cytokines (TNF-α) and chemokines during the inflammatory reaction. Thrombocytosis was recorded in 63% of episodes in one recent Australian report [42]. One possible explanation for this acute thrombocytosis is a response to epinephrine induced by stress, which can shift platelets from the spleen into the circulation. The potential contribution of neutrophils and platelets in FPIES pathophysiology requires further investigation.
Eosinophils are present throughout the gastrointestinal tract under physiologic conditions, except in the esophageal squamous mucosa. Eosinophil accumulation in the gastrointestinal tract is commonly found in many gastrointestinal disorders, including classic IgE-mediated food allergy, eosinophilic gastroenteropathies, food-induced proctocolitis, as well as inflammatory bowel diseases and gastroesophageal reflux [43]. Clusters of eosinophils have been found in intestinal biopsies from infants with FPIES. In FPIES with chronic diarrhea, eosinophils and Charcot-Leyden crystals were detected with Hansel's stain. These findings are not specific for FPIES.
Humoral immune responses
Humoral responses are poorly characterized in FPIES. Jejunal biopsies reveal increased numbers of IgM- and IgA-containing plasma cells [36,44]. Elevated serum IgA and IgG antibodies to food proteins have been described in FPIES patients compared with a control group [45]. A recent study [23] showed similar results with a trend for higher specific IgA antibody levels in children with milk FPIES. These studies demonstrated near absence of allergen-specific IgG4 in FPIES. IgG4 antibodies fix complement poorly and could have a protective role in competing with other antibody subclasses that activate complement. The relative lack of IgG4 in FPIES patients may be involved in the pathogenesis of the disease.
Systemic specific IgE antibody responses are generally absent in FPIES [9,23,37,40]. However, if skin tests are positive to the causal food, case series suggest that these patients have a decreased probability of developing tolerance [9]. The relationship between IgE and non-IgE mechanisms in FPIES requires further study. The gastrointestinal inflammation caused by FPIES might enhance penetrability of food proteins and their presentation to the immune system with subsequent generation of food-specific IgE antibodies. Conversely, local intestinal mucosal IgE antibodies may facilitate antigen uptake and intestinal inflammation [43].
A recent case series of children with FPIES successfully treated with ondansetron during the supervised OFC raised questions about the role of serotonin signaling in FPIES [46]. Ondansetron is a serotonin 5-HT3 receptor antagonist used mainly to treat nausea and vomiting, often following chemotherapy but also in viral gastroenteritis. It affects both peripheral and central nerves. Ondansetron reduces the activity of the vagus nerve, which deactivates the vomiting center in the medulla oblongata, and blocks serotonin receptors in the chemoreceptor trigger zone. The effectiveness of ondansetron suggests the potential for neural component in FPIES reactions and warrants further study.
DIAGNOSIS
The NIAID Food Allergy Guidelines recommend using the medical history and OFC to establish a diagnosis of FPIES [1]. However, when history indicates that infants or children have experienced hypotensive episodes or multiple reactions to the same food, a diagnosis may be based on a convincing history and absence of symptoms when the causative food is eliminated from the diet. The original diagnostic criteria as proposed by Powell were as follows: exposure to the incriminating food elicits repetitive vomiting and/or diarrhea within 4 h, without any other cause for the symptoms; symptoms are limited to the gastrointestinal tract; avoidance of the offending protein from the diet results in resolution of symptoms; and a standardized OFC or isolated reexposure elicits the typical symptoms [8]. In a review published in 2013, Miceli Sopo et al.[47▪] proposed criteria to aid the clinician in diagnosis, which include the following: less than 2 years of age at first presentation (not mandatory); exposure to trigger food elicits repetitive vomiting, pallor, and lethargy within 2–4 h, and usually last less than 6 h; absence of symptoms that suggest an IgE-mediated reaction; avoidance of offending protein from the diet results in resolution of symptoms; and recurrence of typical symptoms within 2–4 h of reexposure.
An International Working Group on Consensus Guidelines for FPIES has been formed under the auspices of the AAAAI Adverse Reactions to Food Committee and the International Association of Food Protein-induced Enterocolitis in 2013. The Expert panel is working on evidence-based guidelines for diagnosis and management of FPIES to improve the care provided for the patients with FPIES.
Though there are no pathognomomic laboratory or radiographic findings specific to FPIES, findings of an elevated white blood cell count with left shift and methemoglobinemia following food ingestion are consistent with FPIES.
Food-specific IgE and skin prick testing may be performed to provide complete evaluation for food sensitization, particularly when considering a food challenge. Though the majority of patients with FPIES have undetectable serum IgE at the time of diagnosis, 18–30% of FPIES patients may develop IgE-mediated food sensitivity to the same food at some point during their course [9,48], with some developing immediate-type symptoms of classic IgE-mediated food allergy.
In research studies, gastric juice analysis showing more than 10 leukocytes/hpf 3 h after a food challenge [49] and atopy patch testing (APT) have been evaluated in FPIES patients [50,51]. Diagnostic utility of these tests remains unclear. Jarvinen et al.[52] evaluated APT in 38 children with FPIES and undergoing OFC. They estimated sensitivity of 11.8% and specificity of 85.7%; at this time APT is not recommended for routine diagnosis of FPIES.
Infants with FPIES often present with multiple reactions and extensive evaluations before the diagnosis of FPIES is considered [24,27]. Delays in diagnosis of infants with FPIES may be due to nonspecific nature of symptoms and lack of classic allergic skin and respiratory symptoms, broad differential diagnosis (discussed in another article of this Current Opinion in Allergy and Clinical Immunology issue by Fiocchi [53]), relative lack of knowledge among physicians [54,55], and in the case of FPIES to solid foods, the perception that grains and vegetables are hypoallergenic.
ORAL FOOD CHALLENGE IN FOOD PROTEIN-INDUCED ENTEROCOLITIS SYNDROME
The OFC remains the gold standard for an initial diagnosis of FPIES as well as for monitoring the resolution of FPIES. The OFC is usually done in an open manner under physician supervision in a facility equipped for managing dehydration and allergic reactions (Table 2). In our practice, a peripheral intravenous line is placed before the challenge to secure immediate access for rapid intravenous fluid rehydration. Baseline complete blood count with differential is obtained immediately before the challenge. The challenge food amount is based on the food protein content and administered in three equal portions over 30 min, followed by minimum 4 h of observation prior to discharge. Patients who tolerated the challenge without any symptoms are usually discharged after 4 h from completing the ingestion of the food; a postchallenge blood sample is obtained for complete blood count with differential. Patients who reacted to the challenge are usually discharged when 6 h have passed since ingestion of the food and their symptoms have resolved. A postchallenge blood sample is obtained for complete blood count with differential at 6 h postchallenge to calculate the increase in peripheral blood neutrophils, which is one of the major criteria for challenge positivity, as proposed by Powell (Table 3). In recent experience, diarrhea during the acute reaction is seen in 20–40% of the patients and may be less common during the food challenge [42,48,56]. In addition, the magnitude of neutrophil count increase during the challenge seems to be less than 3500/mm3. These observations suggest that criteria for challenge positivity should be updated and revised based on these observations from a large number of the food challenges. The initial criteria were established based on the outcomes of 14 challenges in 9 infants with median age 36 days who had just recently removed the offending food from their diet and who were clearly at the peak of their disease [7]. In our clinical practice, we do not perform challenges in infants. The challenge is usually delayed by 12–18 months from the most recent FPIES reaction; therefore, the magnitude of the inflammatory response could be lower. Cooperative efforts among the centers providing the challenges for patients with FPIES are needed to standardize the challenge criteria.
Table 2.
Oral food challenge in food protein-induced enterocolitis syndrome
| Basic requirements | Physician supervision |
| Secure intravenous (i.v.) access | |
| Immediate availability of fluid resuscitation | |
| Baseline laboratory tests | Peripheral neutrophil count (CBC with differential) |
| Challenge administration | Food amount is calculated as 0.06–0.6 g/kg body weight in three equal doses, generally not to exceed total 3 g protein or 10 g of total food (100 ml of liquid) for an initial feedinga |
| Food is divided in three equal portions and fed over 30 min if food-specific IgE is negative | |
| Modification of the challenge and more incremental dosing is used for patients with positive food-specific IgE | |
| Treatment of the reaction | Fluid resuscitation: 20 ml/kg i.v. boluses of 0.9% sodium chloride (NaCl) |
| Steroids: methylprednisolone 1 mg/kg IV, max 60–80 mg | |
| A majority (>50%) of positive challenges require treatment with i.v. fluids and steroids | |
| The role of intravenous ondansetron in the management of acute FPIES reactions is being currently evaluated | |
| Epinephrine and antihistamines are not effective in FPIES | |
| Postchallenge laboratory tests | Peripheral neutrophil count (CBC with differential): at 6 h if the patient reacted or at discharge if the patients tolerated the challenge |
| If stool sample available: test for occult blood and stool smear for leukocytes | |
| Postchallenge observation | About 6 h after the resolution of symptoms or 4 h after feeding in case of no symptoms |
CBC, complete blood count.
aIf no reaction in 2–3 h, administer an age appropriate serving of the food followed by several hours of observation.
Table 3.
Interpretation of the food protein-induced enterocolitis syndrome oral food challenge results
| Symptoms | 1. Emesis (onset 1–3 h) |
| 2. Diarrhea (onset 2–10 h, mean 5 h) | |
| Laboratory | 3. Elevated neutrophil count (>3500 cells/ml, peaks at 6 h) |
| 4. Fecal leukocytes | |
| 5. Fecal eosinophils | |
| Positive challenge | Three of five criteria met |
| Equivocal challenge | Two of five criteria met |
WHEN IS ADDITIONAL DIAGNOSTIC WORK UP NECESSARY?
In any doubtful situation, a confirmatory OFC should be performed to document the diagnosis of FPIES. Children who experience ongoing symptoms or failure to thrive despite progressive food restrictions and/or being exclusively fed with an elemental amino acid-based formula should be evaluated by a pediatric gastroenterologist to rule out other disorders in the gastrointestinal tract. If symptoms appear to be triggered by febrile illness and or there are any developmental delays, a metabolic work up may be advisable.
There appears to be confusion among the providers and the parents of children with chronic gastrointestinal symptoms regarding diagnosis of chronic FPIES. Based on our experience from a referral population, the diagnosis of chronic FPIES is considered when all other diagnostic labels do not fit; it is sometimes given to children with ongoing gastrointestinal symptoms that persist despite extensive dietary eliminations or while the child is exclusively fed with an amino acid-based formula. In such cases, supervised OFCs are necessary to confirm the diagnosis of FPIES and to avoid misdiagnosing other conditions (e.g. metabolic disorders, eosinophilic gastroenteropathies or gastrointestinal inflammatory diseases) as chronic FPIES. The FPIES phenotype had been originally defined in young infants reacting to milk or soy proteins. They had chronic symptoms of vomiting, diarrhea, sometimes with failure to thrive, and/or bloody stools while being fed with milk- or soy-based formulas in the first months of life. Following removal of the formula due to severe symptoms requiring hospitalization, symptoms resolved within a few days. However, subsequent reintroduction of the formula resulted in the typical pattern of acute FPIES, with the onset of emesis in 2–4 h following a feeding. While a recent study [26▪▪] reported a large subset presenting predominantly with chronic diarrhea without vomiting, the diagnosis of FPIES had not been confirmed by an oral challenge in these subjects. Chronic diarrheal phenotype of FPIES requires further validation by rigorous studies.
CONCLUSION
FPIES appears to be a more common condition than previously appreciated. Any food can cause FPIES, with the most common triggers being cow's milk, soy, and rice. Registries are needed to understand the phenotype, triggers, and prevalence of FPIES. OFC remains the gold standard for FPIES diagnosis. Multicenter studies are needed to validate the challenge procedure and positivity criteria. Research on the pathophysiology of FPIES reactions is necessary to develop an evidence-based approach to diagnosis and management of FPIES.
Acknowledgements
ANW reports receiving grant support from NIAID, FARE, Nestle, and Nutricia, royalties from UpToDate, honoraria from speaking engagements from Nestle and Thermofisher Scientific, and for advisory board activities from Merck and Stallergens.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Boyce JA, Assa’ad A, Burks AW, et al. Guidelines for the diagnosis and management of food allergy in the united states: Summary of the NIAID-sponsored expert panel report. J Allergy Clin Immunol 2010; 126:1105–1118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2▪.Jarvinen KM, Nowak-Wegrzyn A. Food protein induced enterocolitis syndrome: Current management strategies. Journal of Allergy and Clinical Immunology: In Practice 2013; 1:317–322 [DOI] [PubMed] [Google Scholar]; This is a comprehensive review of the current empirical approach to diagnosis and management of FPIES.
- 3.Rubin MI. Allergic intestinal bleeding in the newborn; a clinical syndrome. Am J Med Sci 1940; 200:385–390 [Google Scholar]
- 4.Gryboski JD, Burkle F, Hillman R. Milk induced colitis in an infant. Pediatrics 1966; 38:299–302 [PubMed] [Google Scholar]
- 5.Gryboski JD. Gastrointestinal milk allergy in infants. Pediatrics 1967; 40:354–362 [PubMed] [Google Scholar]
- 6.Powell GK. Enterocolitis in low-birth-weight infants associated with milk and soy protein intolerance. J Pediatr 1976; 88:840–844 [DOI] [PubMed] [Google Scholar]
- 7.Powell GK. Milk- and soy-induced enterocolitis of infancy. clinical features and standardization of challenge. J Pediatr 1978; 93:553–560 [DOI] [PubMed] [Google Scholar]
- 8.Powell GK. Food protein-induced enterocolitis of infancy: Differential diagnosis and management. Compr Ther 1986; 12:28–37 [PubMed] [Google Scholar]
- 9.Sicherer SH, Eigenmann PA, Sampson HA. Clinical features of food protein-induced enterocolitis syndrome. J Pediatr 1998; 133:214–219 [DOI] [PubMed] [Google Scholar]
- 10.Burks AW, Casteel HB, Fiedorek SC, et al. Prospective oral food challenge study of two soybean protein isolates in patients with possible milk or soy protein enterocolitis. Pediatr Allergy Immunol 1994; 5:40–45 [DOI] [PubMed] [Google Scholar]
- 11.Cavataio F, Carroccio A, Montalto G, Iacono G. Isolated rice intolerance: Clinical and immunologic characteristics in four infants. J Pediatr 1996; 128:558–560 [DOI] [PubMed] [Google Scholar]
- 12.Borchers SD, Li BU, Friedman RA, McClung HJ. Rice-induced anaphylactoid reaction. J Pediatr Gastroenterol Nutr 1992; 15:321–324 [DOI] [PubMed] [Google Scholar]
- 13.Vitoria JC, Camarero C, Sojo A, et al. Enteropathy related to fish, rice, and chicken. Arch Dis Child 1982; 57:44–48 [PMC free article] [PubMed] [Google Scholar]
- 14.Vandenplas Y, Edelman R, Sacre L. Chicken-induced anaphylactoid reaction and colitis. J Pediatr Gastroenterol Nutr 1994; 19:240–241 [DOI] [PubMed] [Google Scholar]
- 15.Nowak-Wegrzyn A, Sampson HA, Wood RA, Sicherer SH. Food protein-induced enterocolitis syndrome caused by solid food proteins. Pediatrics 2003; 111 (4 Pt 1):829–835 [DOI] [PubMed] [Google Scholar]
- 16.Zapatero Remon L, Alonso Lebrero E, Martin Fernandez E, Martinez Molero MI. Food-protein-induced enterocolitis syndrome caused by fish. Allergol Immunopathol (Madr) 2005; 33:312–316 [DOI] [PubMed] [Google Scholar]
- 17.Hojsak I, Kljaic-Turkalj M, Misak Z, Kolacek S. Rice protein-induced enterocolitis syndrome. Clin Nutr 2006; 25:533–536 [DOI] [PubMed] [Google Scholar]
- 18.Gray HC, Foy TM, Becker BA, Knutsen AP. Rice-induced enterocolitis in an infant: TH1/TH2 cellular hypersensitivity and absent IgE reactivity. Ann Allergy Asthma Immunol 2004; 93:601–605 [DOI] [PubMed] [Google Scholar]
- 19.Levy Y, Danon YL. Food protein-induced enterocolitis syndrome – not only due to cow's milk and soy. Pediatr Allergy Immunol 2003; 14:325–329 [DOI] [PubMed] [Google Scholar]
- 20.Mane SK, Bahna SL. Clinical manifestations of food protein-induced enterocolitis syndrome. Curr Opin Allergy Clin Immunol 2014; 14:217–221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lake AM. Dietary protein enterocolitis. Immunol Allergy Clin North Am 1999; 19:553–561 [Google Scholar]
- 22.Jenkins HR, Pincott JR, Soothill JF, et al. Food allergy: the major cause of infantile colitis. Arch Dis Child 1984; 59:326–329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shek LP, Bardina L, Castro R, et al. Humoral and cellular responses to cow milk proteins in patients with milk-induced IgE-mediated and non-IgE-mediated disorders. Allergy 2005; 60:912–919 [DOI] [PubMed] [Google Scholar]
- 24.Murray KF, Christie DL. Dietary protein intolerance in infants with transient methemoglobinemia and diarrhea. J Pediatr 1993; 122:90–92 [DOI] [PubMed] [Google Scholar]
- 25.Hwang JB, Lee SH, Kang YN, et al. Indexes of suspicion of typical cow's milk protein-induced enterocolitis. J Korean Med Sci 2007; 22:993–997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26▪▪.Ruffner MA, Ruymann K, Barni S, et al. Food protein-induced enterocolitis syndrome: insights from review of a large referral population. J Allergy Clin Immunol Pract 2013; 1:343–349 [DOI] [PubMed] [Google Scholar]; This is the largest series of FPIES patients reported from a single center in the United States.
- 27.Caubet JC, Nowak-Wegrzyn A. Food protein-induced enterocolitis to hen's egg. J Allergy Clin Immunol 2011; 128:1386–1388 [DOI] [PubMed] [Google Scholar]
- 28.Hwang JB, Kang KJ, Kang YN, Kim AS. Probiotic gastrointestinal allergic reaction caused by saccharomyces boulardii. Ann Allergy Asthma Immunol 2009; 103:87–88 [DOI] [PubMed] [Google Scholar]
- 29.Bruni F, Peroni DG, Piacentini GL, et al. Fruit proteins: another cause of food protein-induced enterocolitis syndrome. Allergy 2008; 63:1645–1646 [DOI] [PubMed] [Google Scholar]
- 30.Monti G, Viola S, Tarasco V, et al. A case of severe allergic reaction to cooked potato. Acta Paediatr 2011; 100:e236–e238 [DOI] [PubMed] [Google Scholar]
- 31.Mane SK, Hollister ME, Bahna SL. Food protein-induced enterocolitis syndrome to trivial oral mucosal contact. Eur J Pediatr 2013 2013; [Epub ahead of print] 10.1007/s00431-013-2051-2 [DOI] [PubMed] [Google Scholar]
- 32.Van Sickle GJ, Powell GK, McDonald PJ, Goldblum RM. Milk- and soy protein-induced enterocolitis: evidence for lymphocyte sensitization to specific food proteins. Gastroenterology 1985; 88:1915–1921 [DOI] [PubMed] [Google Scholar]
- 33.Hoffman KM, Ho DG, Sampson HA. Evaluation of the usefulness of lymphocyte proliferation assays in the diagnosis of allergy to cow's milk. J Allergy Clin Immunol 1997; 99:360–366 [DOI] [PubMed] [Google Scholar]
- 34.Heyman M, Darmon N, Dupont C, et al. Mononuclear cells from infants allergic to cow's milk secrete tumor necrosis factor alpha, altering intestinal function. Gastroenterology 1994; 106:1514–1523 [DOI] [PubMed] [Google Scholar]
- 35.Benlounes N, Candalh C, Matarazzo P, et al. The time-course of milk antigen-induced TNF-alpha secretion differs according to the clinical symptoms in children with cow's milk allergy. J Allergy Clin Immunol 1999; 104 (4 Pt 1):863–869 [DOI] [PubMed] [Google Scholar]
- 36.Chung HL, Hwang JB, Kwon YD, et al. Deposition of eosinophil-granule major basic protein and expression of intercellular adhesion molecule-1 and vascular cell adhesion molecule-1 in the mucosa of the small intestine in infants with cow's milk-sensitive enteropathy. J Allergy Clin Immunol 1999; 103:1195–1201 [DOI] [PubMed] [Google Scholar]
- 37.Mori F, Barni S, Cianferoni A, et al. Cytokine expression in CD3+ cells in an infant with food protein-induced enterocolitis syndrome (FPIES): case report. Clin Dev Immunol 2009; 2009:679381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Karlsson MR, Rugtveit J, Brandtzaeg P. Allergen-responsive CD4+CD25+ regulatory T cells in children who have outgrown cow's milk allergy. J Exp Med 2004; 199:1679–1688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Caubet JC, Nowak-Wegrzyn A. Current understanding of the immune mechanisms of food protein-induced enterocolitis syndrome. Expert Rev Clin Immunol 2011; 7:317–327 [DOI] [PubMed] [Google Scholar]
- 40.Chung HL, Hwang JB, Park JJ, Kim SG. Expression of transforming growth factor beta1, transforming growth factor type I and II receptors, and TNF-alpha in the mucosa of the small intestine in infants with food protein-induced enterocolitis syndrome. J Allergy Clin Immunol 2002; 109:150–154 [DOI] [PubMed] [Google Scholar]
- 41.Powell GK, McDonald PJ, Van Sickle GJ, Goldblum RM. Absorption of food protein antigen in infants with food protein-induced enterocolitis. Dig Dis Sci 1989; 34:781–788 [DOI] [PubMed] [Google Scholar]
- 42.Mehr S, Kakakios A, Frith K, Kemp AS. Food protein-induced enterocolitis syndrome: 16-year experience. Pediatrics 2009; 123:e459–e464 [DOI] [PubMed] [Google Scholar]
- 43.Rothenberg ME. Eosinophilic gastrointestinal disorders (EGID). J Allergy Clin Immunol 2004; 113:11–28 [DOI] [PubMed] [Google Scholar]
- 44.Fontaine JL, Navarro J. Small intestinal biopsy in cows milk protein allergy in infancy. Arch Dis Child 1975; 50:357–362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McDonald PJ, Goldblum RM, Van Sickle GJ, Powell GK. Food protein-induced enterocolitis: altered antibody response to ingested antigen. Pediatr Res 1984; 18:751–755 [DOI] [PubMed] [Google Scholar]
- 46.Holbrook T, Keet CA, Frischmeyer-Guerrerio PA, Wood RA. Use of ondansetron for food protein-induced enterocolitis syndrome. J Allergy Clin Immunol 2013; 132:1219–1220 [DOI] [PubMed] [Google Scholar]
- 47▪.Miceli Sopo S, Greco M, Monaco S, et al. Food protein-induced enterocolitis syndrome, from practice to theory. Expert Rev Clin Immunol 2013; 9:707–715 [DOI] [PubMed] [Google Scholar]; This article proposes revising the diagnostic criteria for FPIES.
- 48.Hwang JB, Sohn SM, Kim AS. Prospective follow-up oral food challenge in food protein-induced enterocolitis syndrome. Arch Dis Child 2009; 94:425–428 [DOI] [PubMed] [Google Scholar]
- 49.Nowak-Wegrzyn A, Muraro A. Food protein-induced enterocolitis syndrome. Curr Opin Allergy Clin Immunol 2009; 9:371–377 [DOI] [PubMed] [Google Scholar]
- 50.Fogg MI, Brown-Whitehorn TA, Pawlowski NA, Spergel JM. Atopy patch test for the diagnosis of food protein-induced enterocolitis syndrome. Pediatr Allergy Immunol 2006; 17:351–355 [DOI] [PubMed] [Google Scholar]
- 51.Scaparrotta A, Di Pillo S, Consilvio NP, et al. Usefulness of atopy patch test on a child with milk protein-induced enterocolitis syndrome: a case report. Int J Immunopathol Pharmacol 2013; 26:795–800 [DOI] [PubMed] [Google Scholar]
- 52.Jarvinen KM, Caubet JC, Sickles L, et al. Poor utility of atopy patch test in predicting tolerance development in food protein-induced enterocolitis syndrome. Ann Allergy Asthma Immunol 2012; 109:221–222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fiocchi A, Claps A, Dahdah L, et al. Differential diagnosis of food protein-induced enterocolitis syndrome. Curr Opin Allergy Clin Immunol 2014; 14:246–254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Coates RW, Weaver KR, Lloyd R, et al. Food protein-induced enterocolitis syndrome as a cause for infant hypotension. West J Emerg Med 2011; 12:512–514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jayasooriya S, Fox AT, Murch SH. Do not laparotomize food-protein-induced enterocolitis syndrome. Pediatr Emerg Care 2007; 23:173–175 [DOI] [PubMed] [Google Scholar]
- 56.Sopo SM, Giorgio V, Dello Iacono I, et al. A multicentre retrospective study of 66 Italian children with food protein-induced enterocolitis syndrome: different management for different phenotypes. Clin Exp Allergy 2012; 42:1257–1265 [DOI] [PubMed] [Google Scholar]


