To the Editor:
Emergency department (ED) use has been affected by insurance patterns over time and will likely be further affected by health reform’s expansions of coverage. Because of their disproportionate use of the ED, uninsured patients are often impugned as high, and frequently inappropriate, ED users.1,2 However, recent studies have shown that insured patients can be more frequent utilizers than the uninsured, particularly those with insurance like Medicaid that still leaves them with difficulties in accessing primary care.2-4
We therefore sought to describe recent trends in the association between insurance coverage and ED use in California for non-elderly adult patients, who have experienced the greatest changes in insurance coverage in recent years and are likely to see the biggest shifts as the result of health reform. Previous studies have considered trends in ED use, but predate the recent economic downturn and related insurance changes.2,5
Methods
We conducted a retrospective analysis of California ED visits by patients 19-64 years old from 2005-2010 using the non-public versions of the California Office of Statewide Health Planning and Development’s Emergency Discharge Data and Patient Discharge Data. We excluded visits with missing sex (0.06%), admissions not from the hospital’s ED (20%), and scheduled admissions (0.05%). We also excluded Medicare patients (7.9%), as Medicare beneficiaries under 65 are severely ill and disabled and therefore not comparable to our remaining sample.
To study variations by insurance coverage, we grouped ED visits into four categories based on expected source of payment: Medicaid, private insurance, self-pay or uninsured, and other. We then constructed visit rates using California population data stratified by insurance coverage from the State Health Access Data Assistance Center, derived from the Census Bureau’s Current Population Survey. Finally, we classified visits for ambulatory care sensitive conditions (ACSCs) using the Agency for Healthcare Research and Quality’s Prevention Quality Indicators.6
We compared the distributions of visits and visit rates per population by payer across years using chi-squared tests. We also tested for differences in trends in visit rates by payer using an ordinary least squares regression that allowed for payer-specific linear trends in rates. Statistical significance was assessed using two-sided tests with a critical value of 0.05. Analyses were done using Stata version 11. The study was approved by the UCSF Committee on Human Research.
Results
Between 2005 and 2010, the number of visits to California EDs by non-elderly adult patients increased 13.2%, from 5.4 to 6.1 million per year (Table). The largest increase in visits occurred in 2009 (383,000 visits, 6.7%). The share of total visits attributable to Medicaid patients and the uninsured grew from 2005-2010, while the share attributable to privately insured patients declined (p<.01).
Table. Characteristics of California ED visits by adult (19-64) patients, 2005-2010a.
Chi-squared test were used to test for differences between the distribution of visits across payer categories by year. In pairwise tests, the distribution in each year 2006-2010 is statistically significantly different from the distribution in 2005 (p<.01 in all cases). The distributions are also jointly significantly different across years (p<.01).
| Year | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | Total | ||
|---|---|---|---|---|---|---|---|---|---|
| Na (%) | Na (%) | Na (%) | Na (%) | Na (%) | Na (%) | Na (%) | % increase in visits 2005-2010 |
||
| Payer | Private | 2324 (43) | 2318 (43) | 2374 (43) | 2416 (42) | 2457 (40) | 2350 (38) | 14239 (41) | 1.2% |
| Medicaid | 1238 (23) | 1246 (23) | 1314 (24) | 1416 (25) | 1608 (26) | 1679 (27) | 8501 (25) | 35.6% | |
| Uninsured | 1230 (23) | 1296 (24) | 1342 (24) | 1387 (24) | 1494 (25) | 1543 (25) | 8293 (24) | 25.4% | |
| Otherb | 626 (12) | 578 (11) | 546 (10) | 497 (9) | 539 (9) | 560 (9) | 3345 (10) | −10.6% | |
| Age | 19-25 years | 1061 (20) | 1070 (20) | 1102 (20) | 1121 (20) | 1230 (20) | 1214 (20) | 6798 (20) | 14.4% |
| 26-34 years | 1170 (22) | 1161 (21) | 1202 (22) | 1235 (22) | 1337 (22) | 1351 (22) | 7456 (22) | 15.5% | |
| 35-44 years | 1302 (24) | 1281 (24) | 1272 (23) | 1267 (22) | 1306 (21) | 1289 (21) | 7717 (22) | −1.0% | |
| 45-54 years | 1155 (21) | 1172 (22) | 1210 (22) | 1258 (22) | 1325 (22) | 1335 (22) | 7454 (22) | 15.6% | |
| 55-64 years | 730 (13) | 755 (14) | 791 (14) | 835 (15) | 900 (15) | 942 (15) | 4952 (14) | 29.1% | |
| Sex | Male | 2439 (45) | 2439 (45) | 2482 (45) | 2526 (44) | 2659 (44) | 2672 (44) | 15217 (44) | 9.5% |
| Female | 2979 (55) | 3000 (55) | 3094 (55) | 3190 (56) | 3439 (56) | 3459 (56) | 19161 (56) | 16.1% | |
| Total Visits | 5418 (100) | 5439 (100) | 5576 (100) | 5716 (100) | 6099 (100) | 6131 (100) | 34378(100) | 13.2% | |
| Increase from previous year |
NA | 21 (0.4) | 137 (2.5) | 140 (2.5) | 383 (6.7) | 33 (0.5) | NA | NA | |
All visit numbers presented in thousands.
Other includes workers compensation, other government programs, automobile medical, CHAMPUS (TRICARE), Title V, Veteran’s Affairs, and Other.
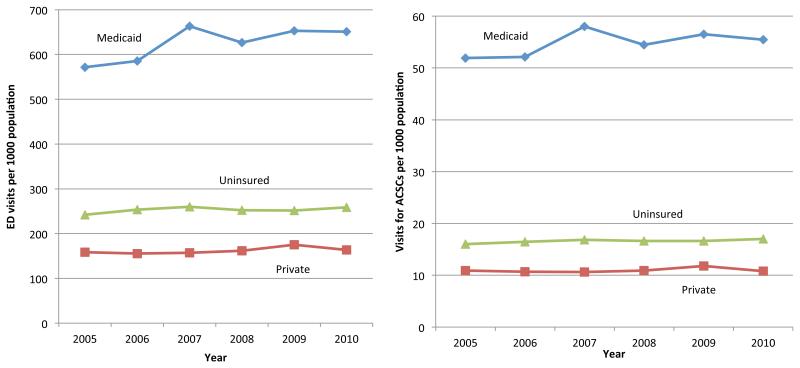
Total visits per 1000 non-elderly adult Californians rose 8.3%, from 252 to 274, between 2005 and 2010 (p<.01). ED visit rates among Medicaid beneficiaries were significantly higher than uninsured and privately insured patients (Figure; p<.01 in all years). Visits per population rose significantly for all payer groups (p<.01 in all cases). ED visit rates among Medicaid beneficiaries rose 13.9%, from 572 to 651 visits per 1000, significantly faster than the privately insured (158 to 164 per 1000), or uninsured (242 to 259 per 1000) (p<.01).
Figure. Overall ED visit rates and ED visit rates for ambulatory care sensitive conditions (ACSCs) among adults (19-64) by payer, 2005-2010.
Legend: Chi-square tests were used to test for differences in the rates of use per population across payers within years, and to test for differences in rates of use by year within payer. In both cases, all differences shown are statistically significant (p<.01). In addition, an analysis of linear trend was conducted to compare changes in rates over time across payers. Differences in the trends in rates for payers shown are statistically significant (p<.01).
Finally, non-elderly adult Medicaid patients consistently had the highest rate of visits for ACSCs (54.76 per 1000 enrollees on average) compared with the privately insured (10.93 per 1000) and uninsured (16.60 per 1000) (Figure; p<.01). Rates of ED use for ACSCs increased from 2005-2010 among Medicaid beneficiaries (6.8%) and the uninsured (6.2%), but declined among the privately insured (−0.7%).
Discussion
ED visit rates by non-elderly adults increased in California from 2005-2010, particularly among Medicaid patients. Growing ED utilization by Medicaid beneficiaries could reflect decreasing access to primary care,2,4 which our findings of high and growing rates of ED use for ACSCs by Medicaid patients support. Overall, the rise in ED visits was highest in 2009, likely due to the H1N1 pandemic and the influence of the economic downturn on coverage transitions, access to care, and thus ED use.
Our analysis is limited in that it uses administrative data and is only generalizable to California. As major changes in insurance coverage approach with the implementation of healthcare reform, continued monitoring of changes in ED use is needed.
Acknowledgements
Drs. Hsia and Baker had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. This study was primarily funded by a grant from the California HealthCare Foundation. Additional support was provided by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number KL2 TR000143 (R.Y.H.), and the Robert Wood Johnson Foundation Physician Faculty Scholars Program (R.Y.H.). The sponsors had no role in the design and conduct of the study; collection, analysis, and interpretation of data; or preparation, review, or approval of the manuscript.
Footnotes
The authors have no conflicts of interest to report.
References
- 1.Freeman HE, Aiken LH, Blendon RJ, Corey CR. Uninsured working-age adults: characteristics and consequences. Health Serv Res. 1990;24(6):811–823. [PMC free article] [PubMed] [Google Scholar]
- 2.Cunningham P, May J. Insured Americans Drive Surge in Emergency Department Visits. Center for Studying Health System Change; Washington DC: 2003. [PubMed] [Google Scholar]
- 3.California HealthCare Foundation . Overuse of Emergency Departments Among Insured Californians. Oakland, CA: 2006. [Google Scholar]
- 4.Decker SL. In 2011 nearly one-third of physicians said they would not accept new medicaid patients, but rising fees may help. Health Aff (Millwood) 2012;31(8):1673–1679. doi: 10.1377/hlthaff.2012.0294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of U.S. emergency department visits, 1997-2007. JAMA. 2010;304(6):664–670. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agency for Healthcare Research and Quality [Accessed March 5, 2013];Prevention Quality Indicators Overview. 2012 http://www.qualityindicators.ahrq.gov/modules/pqi_overview.aspx.