Abstract
Background
Key sexual and reproductive health milestones typically mark changing life stages with different fertility intentions and family planning needs. Knowing the typical ages at such events contributes to our understanding of changes in family formation and transition to adulthood and helps inform needs for reproductive health services.
Methods
We used data from the 1982–2010 National Surveys of Family Growth and the 1995 National Survey of Adolescent Males and event history methods to examine trends over time for women and men in the median ages at several reproductive and demographic events.
Findings
Women’s reports indicate that age at menarche has changed little since 1951. Women’s and men’s median ages at first sex declined through the 1978 birth cohort, but increased slightly since then, to 17.8 for women and 18.1 for men. The interval from first sex to first contraceptive use has narrowed, although Hispanic women have a longer interval. Age at first union (defined as the earlier of first marriage and first cohabiting relationship) has remained relatively stable, but the time between median age at first sex and median age at first birth has increased to 9.2 years for women and 11.4 for men. For some women and men born in the late 1970s, median age at first birth is earlier than median age at first marriage for the first time in at least the past several decades.
Conclusion
The large majority of the reproductive years are spent sexually active. Thus, women have a lengthy period during which they require effective methods. In particular, the period between first sex and first childbearing has lengthened, but long-acting method use, although increasing, has not kept up with this shift. Moving the contraceptive method mix toward underutilized but highly effective contraceptive methods has the potential to reduce the unintended pregnancy rate.
Introduction
Women’s and men’s lives contain a number of milestones that mark changing life stages with different health and social needs. Specific events, such as the initiation of sexual intercourse and the completion of childbearing, often mark the beginning or end of stages during which different needs predominate. For example, menarche marks the beginning of the biological capacity to bear children, and first intercourse marks the beginning of the period of risk for pregnancy and sexually transmitted diseases (although risk of the latter can be incurred before vaginal intercourse occurs). First marriage closes a period at which an individual is at risk for a nonmarital birth, although risk for STIs still exists if individuals have other partners. Completion of desired childbearing often brings a change in a person’s priorities regarding contraception.
Fussell and Furstenberg (2005) argue that the transition to adulthood is “culturally scripted” and that the sequence of events is constrained by norms that “may be altered” very rapidly. Moreover, reproductive trajectories, particularly during adolescence and young adulthood, are “dense, diverse, blurred, and sometimes out of order,” and the activities on either side of transitions are as important as the transitions themselves (Rindfuss, 1991). Individual lives are certainly more complex and variable than what is implied by a “typical” order and timing of events. Nevertheless, placing in order the median ages at which these events occur can be helpful for understanding how individuals progress through these stages, and also enables us to compare various subgroups on the events of interest. Generational differences in the amount of time between these events, their order, and their frequency are important markers of social change that allow us to track and predict demographic trends, economic and societal inequality, and changes in social norms.
Finally, knowledge of the typical ages at these events is valuable from a service provision perspective (Forrest, 1993). Observing differences in the timing of events between demographic groups can help identify subpopulations who face a higher risk for certain events or who have greater need for specific types of services; when differences in the stability and timing of family formation coincide with indicators such as education or family income, they can provide researchers and policy makers with important clues to the causes and consequences of economic inequality (Musick, 2007; Mincieli et al, 2007; and McLanahan, 2008). Combined with research on the impact of adult behavior on child well-being, data on the timing of key life events and how timing differs by group can even help plan services for future generations, such as children born to couples in cohabiting or noncoresidential unions (Manlove, 2012 and Smock, 2010).
Past research has noted changes in specific demographic transitions. A number of studies have noted declines in age at menarche during the past century. For example, a recent study using the National Health and Nutrition Examination Survey (NHANES) found that women born in the 1980s experienced menarche nearly a year earlier than those born before 1920. However, almost all of the decline took place between the earliest birth cohorts studied and the 1940s cohort (McDowell, Brody, & Hughes, 2007). The rise in age at first intercourse in the 1990s (often described as a decline in proportion of adolescents who have had sex) has received a great deal of attention from researchers (Abma et al, 1997; Kann et al, 2000).
Researchers and the general public have also noted a growing delay of first marriage, which has been offset by increasing levels and duration of nonmarital cohabitation (Bumpass, Sweet, & Cherlin 1991). The trend toward later fertility has long been recognized (Bloom, 1982), while the relatively recent increase in nonmarital fertility has been the subject of much attention from researchers— and no small amount of concern from the general public (Smock, 2010 and DeParle, 2012).
The gap between first sex and first use of contraception is particularly important, for it may represent a period of heightened vulnerability to unintended pregnancy. Research showing continuing increases in the proportion of adolescents using contraception both at first sex and at most recent sex (Kann et al, 1998; Eaton et al, 2006; and Finer et al, 2013) suggests that the gap between first sex and first method use may have narrowed.
Most research in this area has generally focused on single transitions. However, a comprehensive assessment of the full reproductive life cycle has not been performed since data from the 1988 National Survey of Family Growth (NSFG) were available (Forrest, 1993). Stages have shifted; new patterns have emerged, and with them new needs. As a result, an up-to-date examination of the timing of these stages is overdue. The release of the 2006–10 NSFG means that these new data can be used to update past published figures. Moreover, both the 2002 and 2006–10 rounds have data for men that are highly comparable with data for women. The goal of this study was to examine the timing of, and trends in, key reproductive and related events, using nationally representative data.
Methods
The primary source of data for this analysis was the NSFG, an in-home survey conducted by the U.S. National Center for Health Statistics. The NSFG is arguably the best source of data on U.S. women’s and men’s sexual, contraceptive and childbearing behaviors, and contains detailed information on relationship histories as well. Nationally representative data were collected from women aged 15–44 in 1982, 1988, 1995, 2002 and 2006–10; sample size ranged from 7,643 to 12,279. The 2002 data set surveyed 4,926 men aged 15–44 for the first time, and the 2006–10 wave surveyed 10,403 men. A second source of information on men used in this analysis was the National Survey of Adolescent Males (NSAM), which was conducted in 1995 and surveyed 1,729 men 15 to 19 on risk behaviors related to HIV, sexually transmitted diseases and pregnancy (Urban Institute, 1998). The NSAM was designed to parallel the NSFG (Abma, 2001), so the responses should be comparable across the two surveys.
The 1982 cycle of the NSFG interviewed women 15–44 at that time — in other words, those born between 1938 and 1967; the 2006–10 cycle interviewed women and men born in 1962– 1995. Rather than comparing results from each of the five data sets, we combined them and used a birth cohort approach to look at changes over time in median ages. In the cases where data sets overlapped, women from two, three, four or five datasets were used. (Women born between 1962 and 1967 were represented in all five cycles.) In order to smooth trendlines, figures reported are typically five-year centered moving averages. So, for example, the median age at menarche indicated for the 1949 birth cohort actually represents the experience of women who were born from 1947 to 1951.
The NSFG is a cross-sectional survey that collects retrospective data. Women were asked to report many salient reproductive events,1 including age at menarche, the date of their first sexual intercourse, and the date of their first use of any contraceptive method. If first contraceptive use occurred before first sex, which can occur when methods are initiated for noncontraceptive reasons (Jones, 2011), women were coded as initiating contraception at the same time as sexual activity. Women were also asked the date that their first cohabitation (if any) began, the date of first marriage, and the date of each of their births, if any. Using information on cohabitation and marriage, we calculated the date of first union (defined as the earlier of first cohabitation and first marriage). For men, the NSFG contains information on the dates of first sex (data from the NSAM contributed to this measure as well), first cohabitation, first marriage and first birth. (Although the NSFG has asked men about contraceptive use since 2002, we decided not to examine this information since respondents’ knowledge about their female partners’ method use is likely incomplete.) Respondents reported all ages and dates in years and months except for age at menarche, which was reported in whole years (as it was in the National Health and Nutrition Examination Survey, the source of data for another published report [McDowell et al, 2007]).
The primary statistical technique used was event history analysis (also known as survival analysis), which allows one to incorporate the experience of all respondents, including those who reached the interview without experiencing a particular event. It also allows one to calculate the median age for any event for which at least 50% of individuals in a birth cohort have experienced the event. We used Kaplan-Meier life table techniques to determine the proportion of individuals who had experienced each event by each age and to calculate the median age at each event for the population as a whole and (for selected events) by subgroup. In addition, in order to describe “current” behaviors, we present a timeline of median ages at each event for the most recent birth cohort for whom data are available.
Most Americans initiate sex during their teen years (Abma et al, 2004), and among teens, almost all pregnancies are unintended (Finer & Henshaw, 2006). In addition, contraceptive use at first sex has been recognized as an indicator of later consistency of use (Shafii et al, 2004). Because of this, we paid additional attention to the interval between first sex and first contraceptive use.
In order to look at influences on the timing of reproductive behaviors in a multivariate context, we performed Cox proportional-hazards regression analyses of the likelihood of first sex, contraceptive use after first sex, first marriage and first birth. In such a model, the outcome variable is the “risk” or “hazard” of experiencing the event, and the odds ratios for each independent variable represent the likelihood of experiencing the event for a particular group compared to the reference group.
In each case, we grouped all the NSFG birth cohorts into three sets based on observed changes in the timing of events, which allowed us to examine shifts over a period of time more substantial than just one year. We included as independent variables a variety of demographic characteristics that were time-invariant or preceded most of these events: race/ethnicity, mother’s completed level of education, family structure when the respondent was 14, respondent’s religious attendance at age 14, and age at first sex. To look at changes over time, we estimated a second set of models including interactions between birth cohort and demographic characteristics; most of these interactions were significant, but to facilitate interpretation, we instead show a separate model for each group of birth cohorts. Finally, in order to assess the amount of time spent in each reproductive “stage,” we used an NSFG variable summarizing each woman’s current sexual activity, pregnancy status, fecundity, and use of contraception. We performed cross-tabulations by age in order to create synthetic cohorts that would represent the experience of a woman throughout her reproductive life if her contraceptive use each year was equivalent to that of women of each age in 1982, 1995 and 2008.
All analyses were conducted using Stata statistical software version 13.0, and account for the NSFG’s complex multistage sampling design.
Results
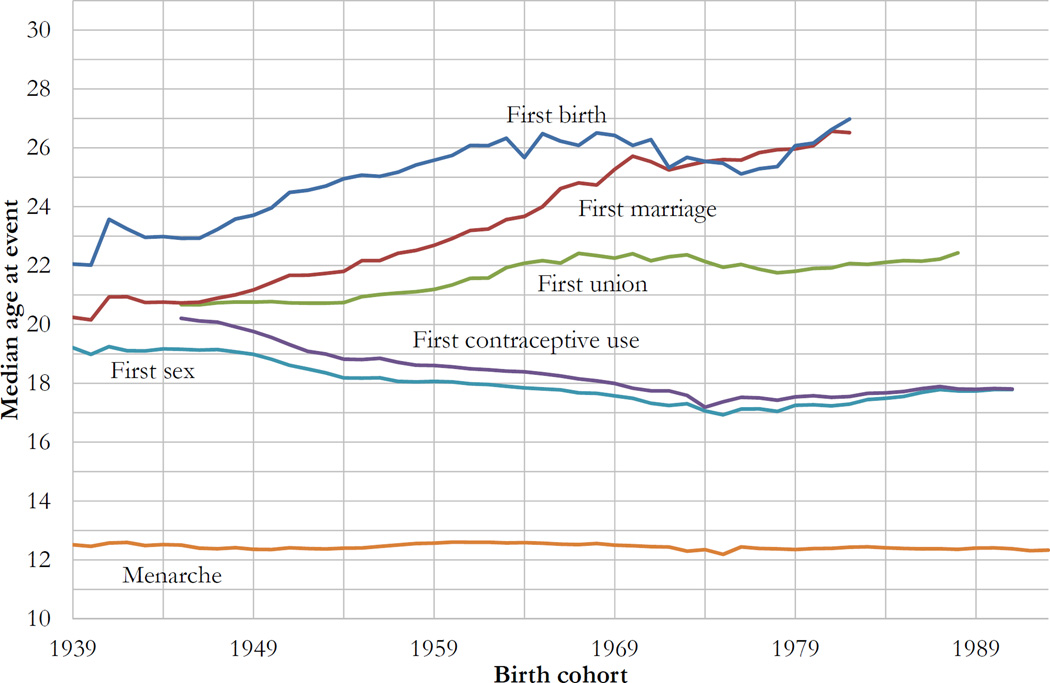
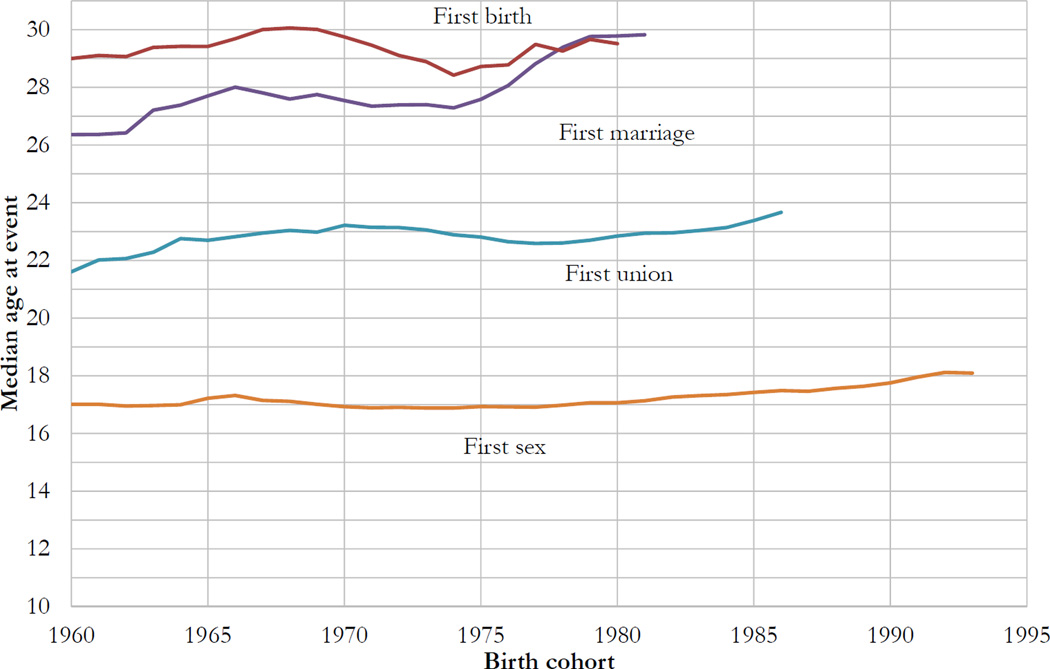
In Figures 1 and 2, each set of points that can be connected by a vertical line represents the typical experience of a single-year birth cohort.
Figure 1.
Women’s median ages at various reproductive events
Figure 2.
Men’s median ages at various reproductive events
Age at Menarche
Women’s reports indicate that age at menarche has changed little since 1939 (Figure 1). The median age of onset of menses for women born in 1939 (and turning 15 in 1954) was 12.5; it peaked at 12.6 for the 1963 birth cohort and declined to 12.3 for women born in 1993 (and turning 15 in 2008) (Figure 3). The 1963–93 decline represented about .01 years of age per cohort year. The 25th percentile (not shown) was also stable over the period studied, ranging from 11.2 to 11.6 with no discernible trend, and the 75th percentile ranged from 13.1 to 13.6, also with no clear trend.
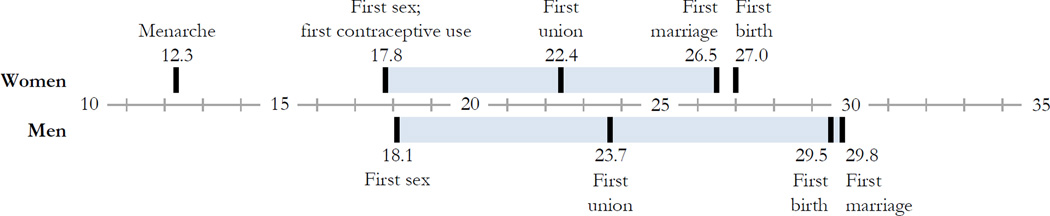
Figure 3.
“Current” median ages at reproductive events (i.e., median age at event for most recent cohort for whom data are available)
Shaded area represents period of high risk for nonmarital birth.
Birth cohort for each estimate:
Women: Menarche 1993, first sex and first contraceptive use 1991, first union 1988, first marriage and first birth 1982.
Men: First sex 1993, first union 1986, first marriage 1981, first birth 1980.
Age at First Sex
The median age at first sex declined among women born in the 1950s and 1960s, but beginning with women born in the 1970s, this trend halted at about 17.0 years of age, and the median age actually increased by almost a year among cohorts coming of age in the late 1990s. Accordingly, the “current” median age (i.e., the median for the most recent cohort for which a median can be calculated) at first sex is 17.8 for women.
A similar increase beginning with the 1982 birth cohort was seen for men (Figure 2), although median age at first sex was stable for those born between 1960 and 1985, at about 17.0. The “current” median age at first sex for men is 18.1.
In multivariate models, compared to white women, black women initiate sex sooner (Table 1). The propensity of Hispanic women to initiate sex later appears to have diminished over time. Family structure, adolescent religious attendance, and mother’s education all are significantly associated with sexual initiation, and the magnitude of family structure’s relationship with age at first sex appears to have increased.
Table 1.
Cox proportional-hazards models predicting women’s risk of first sex by demographic characteristics and birth cohort
| Birth Cohort | ||||||
|---|---|---|---|---|---|---|
| 1937–60 | 1961–71 | 1972–95 | ||||
| Odds ratio |
Sig. | Odds ratio |
Sig. | Odds ratio |
Sig. | |
| Race/ethnicity | ||||||
| White | 1.00 | 1.00 | 1.00 | |||
| Hispanic | 0.70 | *** | 0.77 | *** | 0.91 | |
| Black | 1.38 | *** | 1.21 | ** | 1.29 | *** |
| Other | 0.45 | *** | 0.54 | *** | 0.65 | *** |
| Mother’s education | ||||||
| Less than HS diploma | 1.00 | 1.00 | 1.00 | |||
| HS diploma or GED | 0.93 | 0.94 | 1.01 | |||
| Some college | 0.79 | *** | 0.78 | *** | 0.86 | |
| Bachelor’s degree or more | 0.79 | *** | 0.71 | *** | 0.67 | *** |
| Family structure | ||||||
| Two parents from birth | 1.00 | 1.00 | 1.00 | |||
| Anything else | 1.29 | *** | 1.31 | *** | 1.54 | *** |
| Religious attendance | ||||||
| Never | 1.00 | 1.00 | 1.00 | |||
| Less than once per month | 0.86 | 0.90 | 0.90 | |||
| 1–3 times per month | 0.81 | * | 0.92 | 0.80 | ** | |
| Once per week or more | 0.66 | *** | 0.71 | *** | 0.59 | *** |
Asterisks indicate statistical significance at
p<.05,
p<.01,
p<.001.
Age at First Contraceptive Use; Time From First Sex to First Contraceptive Use
Among women, increases in contraceptive use at first sex are reflected in the convergence of the first-sex and first-contraceptive-use trend lines (Figure 1). The median age at first contraceptive use declined to 17.2 for those who were born in 1978, and then increased (along with age at first sex) to 17.8 for those born in 1991.
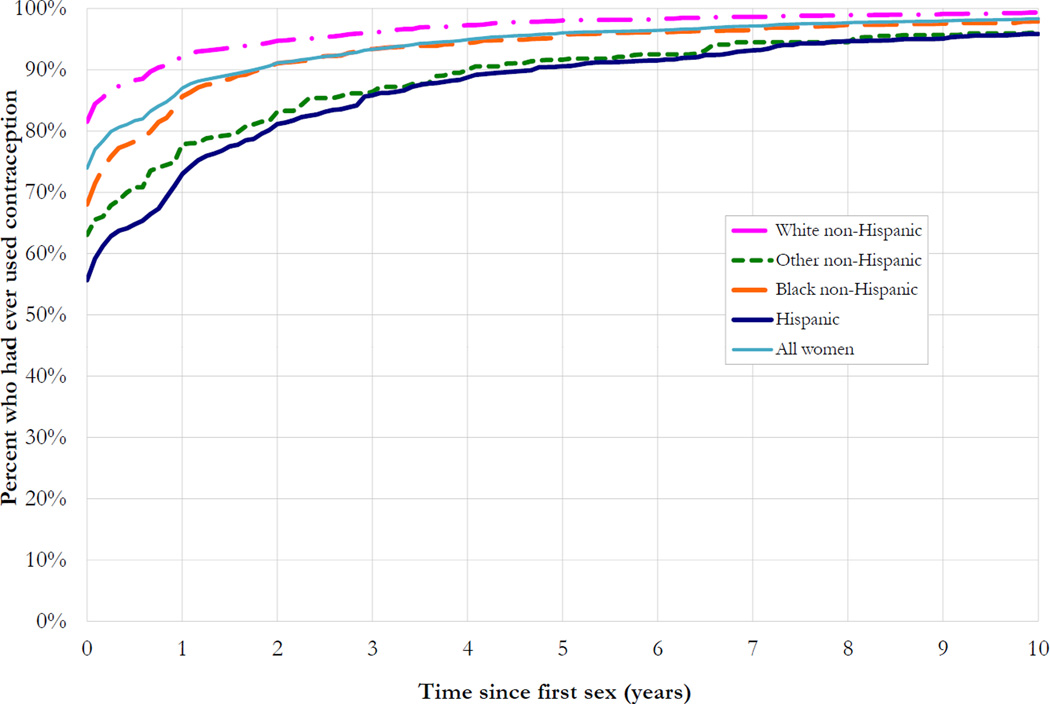
In the 2006–10 NSFG, almost three-quarters of all sexually active women reported using contraception at or before their first sexual encounter (Figure 4), but the percentage varied by race and ethnicity. Hispanic women lagged significantly and substantially behind women of other racial/ethnic groups in their use of contraception at first sex. However, the gap narrowed over time; by 5 years after coitarche, more than 90% of women of all ethnicities had used contraception.
Figure 4.
Time from first sex to first contraceptive use, by race/ethnicity, women, NSFG 2006–10
In a multivariate model, white women, women with more-educated mothers, and women who initiated sex later all begin contracepting sooner than their counterparts (Table 2). While differences in contraceptive uptake persist for nonwhite women and those who begin having sex earlier, these differences have decreased over time. (Recent work on the behavior of the youngest 10 birth-year cohorts in the 2006–2010 NSFG found no significant difference in time to contraceptive use between those who initiated sex at ages 15–16 and those who did so at 19 and older, confirming the trend towards greater contraceptive uptake among teens [Finer & Philbin, 2013].)
Table 2.
Cox proportional-hazards models predicting women’s risk of contraceptive use at or after first sex by demographic characteristics and birth cohort
| Birth Cohort | ||||||
|---|---|---|---|---|---|---|
| 1937–60 | 1961–71 | 1972–95 | ||||
| Odds ratio |
Sig. | Odds ratio |
Sig. | Odds ratio |
Sig. | |
| Race/ethnicity | ||||||
| White | 1.00 | 1.00 | 1.00 | |||
| Hispanic | 0.60 | *** | 0.70 | *** | 0.82 | *** |
| Black | 0.76 | *** | 0.90 | ** | 0.90 | *** |
| Other | 0.55 | *** | 0.59 | *** | 0.93 | |
| Mother’s education | ||||||
| Less than HS diploma | 1.00 | 1.00 | 1.00 | |||
| HS diploma or GED | 1.27 | *** | 1.34 | *** | 1.14 | *** |
| Some college | 1.34 | *** | 1.45 | *** | 1.19 | *** |
| Bachelor’s degree or more | 1.21 | *** | 1.47 | *** | 1.18 | *** |
| Family structure | ||||||
| Two parents from birth | 1.00 | 1.00 | 1.00 | |||
| Anything else | 0.92 | ** | 0.96 | 1.01 | ||
| Religious attendance | ||||||
| Never | 1.00 | 1.00 | 1.00 | |||
| Less than once per month | 1.08 | 1.09 | 1.08 | * | ||
| 1–3 times per month | 1.11 | 1.03 | 1.04 | |||
| Once per week or more | 1.09 | 1.02 | 1.01 | |||
| Age at first sex | ||||||
| >=19 | 1.00 | 1.00 | 1.00 | |||
| 17–18 | 0.94 | 0.96 | 0.98 | |||
| 15–16 | 0.81 | *** | 0.87 | *** | 0.94 | * |
| <15 | 0.58 | *** | 0.77 | *** | 0.79 | *** |
Asterisks indicate statistical significance at
p<.05,
p<.01,
p<.001.
Age at First Union and First Marriage
The trend of women’s increasing age at first marriage has continued through the 1982 birth cohort; the median for that cohort was 26.5 (Figure 1). However, increases in the number and proportion of cohabiting couples over time mean that the median age at first union has not changed much since the cohort of women born in 1965. For the most recent cohort with available data, those who were born in 1988, it was 22.4. Race and mother’s education are important factors associated with women’s likelihood to marry (Table 3), with blacks and women with more-educated mothers being far less likely to marry, associations that have strengthened over time.
Table 3.
Cox proportional-hazards models predicting women’s risk of first marriage by demographic characteristics and birth cohort
| Birth Cohort | ||||||
|---|---|---|---|---|---|---|
| 1937–60 | 1961–71 | 1972–95 | ||||
| Odds ratio |
Sig. | Odds ratio |
Sig. | Odds ratio |
Sig. | |
| Race/ethnicity | ||||||
| White | 1.00 | 1.00 | 1.00 | |||
| Hispanic | 0.81 | ** | 0.83 | 1.00 | ||
| Black | 0.49 | *** | 0.40 | *** | 0.35 | *** |
| Other | 0.59 | *** | 0.50 | ** | 0.71 | |
| Mother’s education | ||||||
| Less than HS diploma | 1.00 | 1.00 | 1.00 | |||
| HS diploma or GED | 0.83 | *** | 0.79 | * | 0.72 | ** |
| Some college | 0.68 | *** | 0.55 | *** | 0.49 | *** |
| Bachelor’s degree or more | 0.56 | *** | 0.39 | *** | 0.38 | *** |
| Family structure | ||||||
| Two parents from birth | 1.00 | 1.00 | 1.00 | |||
| Anything else | 1.09 | 1.23 | * | 1.12 | ||
| Religious attendance | ||||||
| Never | 1.00 | 1.00 | 1.00 | |||
| Less than once per month | 1.12 | 0.71 | * | 0.75 | * | |
| 1–3 times per month | 1.04 | 0.60 | ** | 0.96 | ||
| Once per week or more | 1.00 | 0.69 | ** | 1.15 | ||
Asterisks indicate statistical significance at
p<.05,
p<.01,
p<.001.
The median age at first union for the most recent cohort of men, those born in 1986, was 23.7. There is evidence of an increase in men’s median age at union and marriage, starting with men born around 1975. The most recent median age at marriage for men was 29.8.
Age at First Birth
The median age at first birth increased for women born through the 1960s, reaching a plateau at about age 26. Since then, however, it appears to have declined and then increased again (Figure 1). For women born in 1975, median age at first birth was earlier than median age at first marriage for the first time since these data have been collected.
For men, the median age at first birth has hovered around 29 over the 20-year period examined; the figure was 29.5 for the most recent cohort for whom a median could be calculated. A similar crossing of the marriage and birth lines is evident.
In Table 4, we can see that race/ethnicity, family structure and mother’s education have long been factors in timing of first birth, and the degree of each factor’s influence has increased over time. The difference between white women and black women is especially notable: black women in the latest birth cohorts (1972–95) were more than twice as likely to begin childbearing at any point in time as were white women. While the role of religious attendance was not a significant predictor of “risk” for a first birth in the past, in the latest birth cohorts, women who attended religious services frequently (once per week or more) as adolescents were less likely to have initiated childbearing. Finally, while the role of mother’s education has and continues to be associated with delaying births, the strength of the association with mother’s college education has increased.
Table 4.
Cox proportional-hazards models predicting women’s risk of first birth by demographic characteristics and birth cohort
| Birth Cohort | ||||||
|---|---|---|---|---|---|---|
| 1937–60 | 1961–71 | 1972–95 | ||||
| Odds ratio |
Sig. | Odds ratio |
Sig. | Odds ratio |
Sig. | |
| Race/ethnicity | ||||||
| White | 1.00 | 1.00 | 1.00 | |||
| Hispanic | 1.30 | *** | 1.44 | *** | 1.82 | *** |
| Black | 1.26 | *** | 1.43 | *** | 2.05 | *** |
| Other | 0.79 | * | 0.89 | 1.16 | ||
| Mother’s education | ||||||
| Less than HS diploma | 1.00 | 1.00 | 1.00 | |||
| HS diploma or GED | 0.75 | *** | 0.70 | *** | 0.66 | *** |
| Some college | 0.65 | *** | 0.48 | *** | 0.48 | *** |
| Bachelor’s degree or more | 0.45 | *** | 0.38 | *** | 0.24 | *** |
| Family structure | ||||||
| Two parents from birth | 1.00 | 1.00 | 1.00 | |||
| Anything else | 1.07 | 1.20 | *** | 1.58 | *** | |
| Religious attendance | ||||||
| Never | 1.00 | 1.00 | 1.00 | |||
| Less than once per month | 0.99 | 0.86 | 0.69 | ** | ||
| 1–3 times per month | 0.98 | 0.90 | 0.82 | |||
| Once per week or more | 0.99 | 0.89 | 0.75 | *** | ||
Asterisks indicate statistical significance at
p<.05,
p<.01,
p<.001.
Time Spent in Each Reproductive Stage
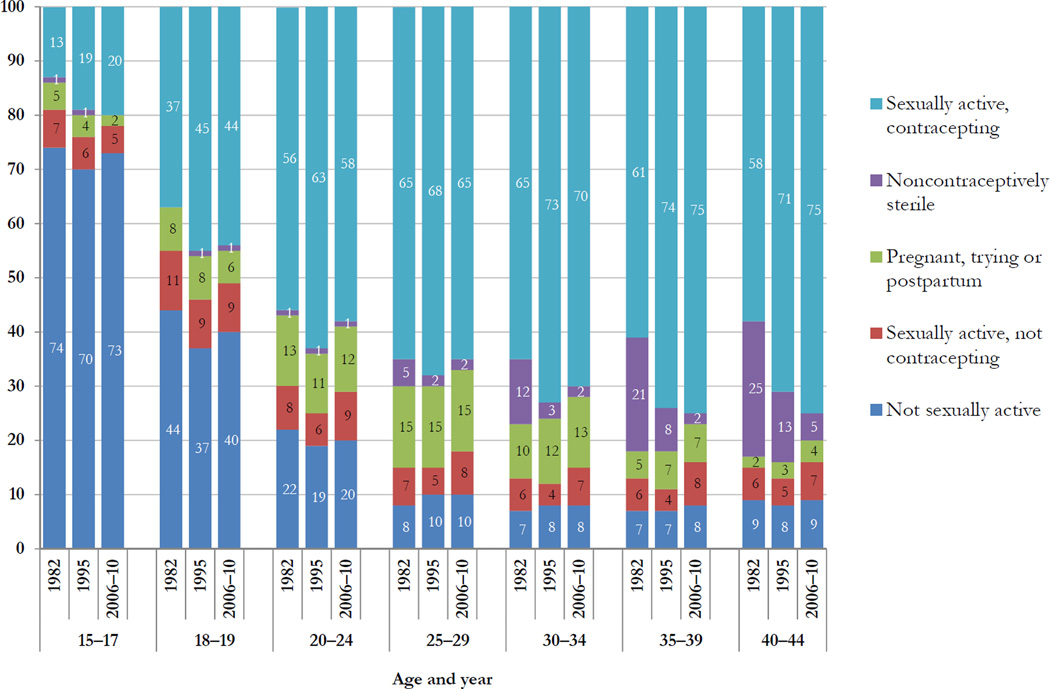
The current sexual activity and contraceptive status of all female respondents in three rounds of the NSFG (i.e., at three points in time) is shown in Figure 5. “Sexually active” is defined as having had sex in the past three months; “contracepting” is defined as having used a form of contraception during the month of interview. Contraception includes both sterilization and all reversible methods, including natural family planning, withdrawal, and male methods. A small proportion of women reported that they were sterile for reasons other than contraceptive use (for example, due to a hysterectomy); these women are shown separately in the figure.
Figure 5.
Percentage of women 15–44 who were in various reproductive stages at each age
At each of the three time points, the large majority of the reproductive years were spent sexually active and using contraception. More than 55% of women in each cohort from age 20 to 44 fell into this category at each time. Slightly less than one in ten women of each age from 25 to 44 were not sexually active, and 5–11% of women 15 and older (and 6–8% of women 25 and older) were sexually active but not using any form of contraception. The proportion pregnant, trying to become pregnant, or postpartum peaks in the 25–29 age group at each time.
A decline in the proportion of young teens who were pregnant was accompanied by an increase in teen contraceptive use. Twice as many 15–17-year-olds were pregnant, trying to become pregnant, or postpartum in 1982 as in 2006–10. In 2006–10, 20% of young teens were sexually active and contracepting, compared to 13% in 1982; the proportion not sexually active was about the same in the two periods. Among all age groups except for teens, declines between 1982 and 1995 in the proportion who were sexually active but not using contraception were offset by increases between 1995 and 2006–10. The proportion of women who report noncontraceptive sterility has decreased substantially over time.
Limitations
The data presented here represent the overall experience of entire cohorts. The timing of these events varies substantially across population subgroups and among individuals, but our aggregate analyses tend to mask these variations. Figures 2 and 3 and the multivariate analyses provide some hints of the heterogeneity.
Since the study is retrospective, recall bias might have influenced the results if any of the events reported were difficult to remember. However, these are highly salient events, which may minimize this concern. Also, men may underreport children they have fathered (Rendall et al, 2006). Assuming they have unreported births, the true median age at first birth for men may be lower than that reported here.
Discussion
Our analysis of representative data from several decades American women’s and men’s lives showed measurable changes in their reproductive life stages over the past quarter century. Several of these have clear implications for reproductive health.
One change we did not see, however, was in age at menarche. Previously published findings using data from NHANES suggested clear decreases in age at menarche between the pre-1920 birth cohorts and the 1930s birth cohort, and smaller declines since then. Our findings, for birth cohorts beginning with 1939, indicate that age at menarche has changed little over the period covered in this analysis. Although our results do not suggest any substantial changes in age at menarche among women as a whole, other studies have noted differences in age at menarche by race (Chumlea et al, 2003). The NHANES study suggested an additional decrease between the 1960s cohort and the 1980s cohort, but the confidence interval for the 1980s cohort was large. We see a small decline of 0.3 years between the 1969 and 1993 birth cohorts, but additional data will be required to determine if this is a real decrease.
While there have been slight declines in age at first sex over the entire time period, median age at first sex for women turning 15 in the mid-2000s was roughly equal to that of women 35 years earlier. More notable is the clear shortening of the time from first sex to first contraceptive use, which bodes well for prevention of unintended pregnancy (and has in fact been reflected in declines in the teen pregnancy rate).
Unlike women, men reported little change in age at first sex over time. As a result, the gap between women’s and men’s sexual initiation has narrowed. Indeed, in the most recent cohorts, age at first sex is now virtually equal across genders. This convergence in men’s and women’s timelines may be attributable to social changes that have delayed marriage for women without causing a similar delay for men, such as expanded labor market and educational opportunities. The wide availability of effective contraception and the acceptability of premarital sex may also have contributed to the lengthier gap between first sex and first union for women.
For recent cohorts of women and men, median age at first birth is earlier than median age at first marriage for the first time in the last several decades. This result is in line with findings from the Current Population Survey and national vital statistics reports. While a majority of births occur to married couples (Hamilton, 2012) and most births still occur in the context of a union, marital or otherwise, this finding nonetheless represents a milestone. Child health and social outcomes are generally more positive when a child is born into a stable two-parent union (Fomby et al, 2007 and Najman et al, 1997), and ordering childbearing first has the potential to affect union stability and the likelihood of subsequent marriage and divorce (Graefe et al, 2002). Thus, this trend warrants additional investigation.
The decline in the proportion of women who report noncontraceptive sterility may be due to delayed childbearing, technological advances to correct impaired fecundity, and a documented decrease in sterilization procedures — some of which were done for noncontraceptive purposes — performed through the 1990s and early 2000s (Chan, 2010 and Chandra, 2013).
Implications for Practice and/or Policy
Reproductive health patterns have long been characterized by racial and ethnic disparities, and our data show evidence of this. Black women initiate sex earlier, and Hispanic women in particular lag behind women of other races in terms of initiating contraceptive use. At the same time, a higher proportion of Hispanic teens may desire pregnancy at earlier ages (Braveman, 2011). Educators and health programmers should take these patterns among women of color into account in order to provide the most effective services.
The large majority of women’s and men’s reproductive years are spent sexually active. The increase in the windows between first sex and first marriage, and between first sex and first birth for women, is one of the clearest findings of our study. Although factors contributing to this lengthier interval were beyond the scope of the analysis, other research suggests it is a result of broad societal changes, such as increases in educational attainment and women’s increased participation in the labor force (Goldin 2002). The result is that American adults now face a lengthy period before childbearing during which they require effective contraceptive methods. But despite increases in contraceptive use at first sex, the pill and condoms continue to predominate among women who have not yet had children. Use of long-acting reversible methods — the most effective ways to prevent pregnancy (Winner 2012) —among all women has increased from 2.4% in 2002 to 8.5% in 2009 (Finer 2012), but remains low among teens and underutilized by women in their 20s. Some reproductive health professionals have taken note; the American Congress of Obstetricians and Gynecologists now describes long-acting reversible methods as “first-line options” for young women and those without children (ACOG, 2012). Our findings highlight the importance of dispelling longstanding myths that hinder acceptance of underutilized methods such as the IUD, and of continuing the encouraging pattern of new method development and introduction that has characterized the late 1990s through the current decade, in order to reduce the nation’s continuing high rate of unintended pregnancy.
Acknowledgments
This research was funded by grant R01 HD059896 from the National Institutes of Health. The funder played no role in the design or conduct of the study, the collection, management, analysis, or interpretation of the data, or the preparation, review, or approval of the manuscript.
The authors thank Ward Cates, Jacqueline Darroch and Laura Lindberg for guidance and review of earlier drafts.
Biographies
Lawrence B. Finer, Ph.D., is director of domestic research at the Guttmacher Institute. His research interests include contraceptive use patterns, the demography of unintended pregnancy and abortion, and adolescent sexual health.
Jesse M. Philbin, B.A., is a senior research assistant at the Guttmacher Institute. Her research interests include pregnancy intentions, economic inequality and family formation, social epidemiology, and longitudinal research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Neither author has any conflicts of interest to disclose.
Since most of the women surveyed in the NSFG had not yet experienced menopause, it is impossible to use these data to calculate a median age for this event. Nevertheless, menopause is a key reproductive health event, since it represents the natural end of a woman’s fertile period. Estimates from the published literature (Krailo & Pike, 1983, and Kato et al, 1998) suggest that the median age at menopause is about 51. Fecundity is known to decline with maternal age, particularly after 35 (Leridon, 2004); nonetheless, women are at risk of unintended pregnancy for a substantial period after this age.
Contributor Information
Lawrence B. Finer, Email: lfiner@guttmacher.org.
Jesse M. Philbin, Email: jphilbin@guttmacher.org.
REFERENCES
- Abma JC, Chandra A, Mosher WD, Peterson LS, Piccinino LJ. Fertility, family planning, and women’s health: new data from the 1995 National Survey of Family Growth. Vital and Health Statistics. 1997;23(19):1–114. [PubMed] [Google Scholar]
- Abma JC, Sonenstein FL. Sexual activity and contraceptive practices among teenagers in the United States, 1988 and 1995. Vital and Health Statistics. 2001;23(21):1–79. doi: 10.1037/e304002003-001. [DOI] [PubMed] [Google Scholar]
- Abma JC, Martinez GM, Mosher WD, Dawson BS. Teenagers in the United States: sexual activity, contraceptive use, and childbearing, 2002. Vital and Health Statistics. 2004;23(24):1–48. [PubMed] [Google Scholar]
- American College of Obstetricians and Gynecologists. Adolescents and long-acting reversible contraception: implants and intrauterine devices. 2012 Oct; Committee Opinion No. 539. Retrieved from http://www.acog.org/~/media/Committee%20Opinions/Committee%20on%20Adolescent%20Health%20Care/co539.pdf.
- Bloom DE. What’s happening to the age at first birth in the United States? A study of recent cohorts. Demography. 1982;19(3):351–370. [PubMed] [Google Scholar]
- Braveman P, Brindis C, et al. Latina Voices: Findings from a Study of Latina Teen Childbearing in the Fresno and Los Angeles Areas. San Francisco, CA: Bixby Center for Global Reproductive Health and Center on Social Disparities in Health; 2011. Retrieved from: http://bixbycenter.ucsf.edu/publications/files/Latina_Teen_Childbearing_March_2011. [Google Scholar]
- Bumpass LL, Sweet JA, Cherlin AJ. The role of cohabitation in declining rates of marriage. Journal of Marriage and the Family. 1991;53(4):913–927. [Google Scholar]
- Chan LM, Westhoff CL. Tubal sterilization trends in the United States. Fertility and Sterility. 2010;94(1):1–6. doi: 10.1016/j.fertnstert.2010.03.029. [DOI] [PubMed] [Google Scholar]
- Chandra A, Copen CE, Stephen EH. National Health Statistics Reports. Vol. 67. Washington, DC: National Center for Health Statistics; 2013. Infertility and impaired fecundity in the United States, 1982 – 2010: Data from the National Survey of Family Growth. [PubMed] [Google Scholar]
- Chumlea WC, Schubert CM, Roche AF, et al. Age at menarche and racial comparisons in US girls. Pediatrics. 2003;111(1):110–113. doi: 10.1542/peds.111.1.110. [DOI] [PubMed] [Google Scholar]
- DeParle Jason. Two classes in America, divided by “I do.“. New York Times. 2012 Jul 14; Retrieved from: http://www.nytimes.com/2012/07/15/us/two-classes-in-america-divided-by-i-do.html. [Google Scholar]
- Eaton DK, Kann L, Kinchen S, et al. Youth Risk Behavior Surveillance — United States, 2005. Journal of School Health. 2006;76(7):353–372. doi: 10.1111/j.1746-1561.2006.00127.x. [DOI] [PubMed] [Google Scholar]
- Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspectives on Sexual and Reproductive Health. 2006;38(2):90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the U.S., 2007–2009. Fertility and Sterility. 2012;98(4):893–897. doi: 10.1016/j.fertnstert.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finer LB, Philbin JM. Sexual initiation, contraceptive use, and pregnancy among young adolescents. Pediatrics. 2013;131(5):1–6. doi: 10.1542/peds.2012-3495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fomby P, Cherlin AJ. Family instability and child well-being. American Sociological Review. 2007;72(2):181–204. doi: 10.1177/000312240707200203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest JD. Contraceptive needs through stages of women’s reproductive lives. Contemporary Ob/Gyn. 1988;32:12–22. [Google Scholar]
- Forrest JD. Timing of reproductive life stages. Obstetrics & Gynecology. 1993;82(1):105–111. [PubMed] [Google Scholar]
- Goldin C, Katz LF. The power of the pill: Oral contraceptives and women’s career and marriage decisions. Journal of Political Economy. 2002;110(4):730–770. [Google Scholar]
- Graefe DR, Lichter DT. Marriage among unwed mothers: whites, blacks and Hispanics compared. Perspectives in Sexual and Reproductive Health. 2002;34(6):286–293. [PubMed] [Google Scholar]
- Hamilton BE, Martin JA, Ventura SJ. National Vital Statistics Reports. 5. Vol. 61. Hyattsville, MD: National Center for Health Statistics; 2012. Births: preliminary data for 2011. [PubMed] [Google Scholar]
- Jones RK. Beyond Birth Control: The Overlooked Benefits of Oral Contraceptive Pills. New York: Guttmacher Institute; 2011. [Retrieved August 18, 2013]. from: http://www.guttmacher.org/pubs/Beyond-Birth-Control.pdf. [Google Scholar]
- Kann L, Kinchen SA, Williams BI, et al. Youth Risk Behavior Surveillance — United States, 1999. MMWR CDC Surveillance Summaries. 2000;49(5):1–32. [PubMed] [Google Scholar]
- Kann L, Kinchen SA, Williams BI, et al. Youth Risk Behavior Surveillance — United States, 1997. MMWR CDC Surveillance Summaries. 1998;47(3):1–89. [PubMed] [Google Scholar]
- Kato IP, Toniolo A, Akhmedkhanov KL. Prospective study of factors influencing the onset of natural menopause. Journal of Clinical Epidemiology. 1998;51(12):1271–1276. doi: 10.1016/s0895-4356(98)00119-x. [DOI] [PubMed] [Google Scholar]
- Krailo MD, Pike MC. Estimation of the distribution of age at natural menopause from prevalence data. American Journal of Epidemiology. 1983;117(3):356–361. doi: 10.1093/oxfordjournals.aje.a113548. [DOI] [PubMed] [Google Scholar]
- Leridon H. Can assisted reproduction technology compensate for the natural decline in fertility with age? A model assessment. Human Reproduction. 2004;19(7):1548–1553. doi: 10.1093/humrep/deh304. [DOI] [PubMed] [Google Scholar]
- McDowell MA, Brody DJ, Hughes JP. Has age at menarche changed? Results from the National Health and Nutrition Examination Survey (NHANES) 1999–2004. Journal of Adolescent Health. 2007;40(3):227–231. doi: 10.1016/j.jadohealth.2006.10.002. [DOI] [PubMed] [Google Scholar]
- McLanahan S, Percheski C. Family structure and the reproduction of inequalities. Annual Review of Sociology. 2008;34:257–276. [Google Scholar]
- Najman JM, Behrens BC, Andersen M, et al. Impact of family type and family quality on child behavior problems. Journal of the American Academy on Child and Adolescent Psychiatry. 1997;36:1357–1365. doi: 10.1097/00004583-199710000-00017. [DOI] [PubMed] [Google Scholar]
- Ranjit N, Bankole A, Darroch JE, Singh S. Contraceptive failure in the first two years of use: differences across socioeconomic subgroups. Family Planning Perspectives. 2001;33(1):19–27. [PubMed] [Google Scholar]
- Rendall MS, Admiraal R, Handcock MS, Joyner K. Early entry to fatherhood estimated from men’s and women’s survey reports in combination. [Retrieved August 18, 2013];National Survey of Family Growth Research Conference. 2006 Oct 19–20; from: ftp://ftp.cdc.gov/pub/health_Statistics/NCHS/Publications/nsfg/confpresentations/S3.Fatherhood/Rendall-Earlyentrytofatherhood.pdf.
- Rindfuss RR. The young adult years: diversity, structural change, and fertility. Demography. 1991;28(4):493–512. [PubMed] [Google Scholar]
- Shafii T, Stovel K, Davis R, Holmes K. Is condom use habit forming?: condom use at sexual debut and subsequent condom use. Sexually Transmitted Diseases. 2004;31(6):366–372. doi: 10.1097/00007435-200406000-00010. [DOI] [PubMed] [Google Scholar]
- Urban Institute. 1995 National Survey of Adolescent Males (NSAM) 1998 Retrieved from: http://www.urban.org/publications/900460.html. [Google Scholar]
- U.S. Census Bureau. Estimated Median Age at First Marriage, by Sex: 1890 to the Present (Table MS-2) 2006 Sep 21; Retrieved from: http://www.census.gov/population/socdemo/hh-fam/ms2.pdf.
- Winner B, Peipert JF, Zhao Q, et al. Effectiveness of long-acting reversible contraception. New England Journal of Medicine. 2012;366(21):1998–2007. doi: 10.1056/NEJMoa1110855. [DOI] [PubMed] [Google Scholar]