Abstract
Introduction
Background & Objectives
Despite several interventions implemented for the improvement of infant survival, the pace of decline in infant mortality in the State of Andhra Pradesh during the last two decades has been rather slow. This paper examines determinants of infant mortality in a rural population of about 45000 in Medchal region of Andhra Pradesh, India.
Methods
Data obtained through continuous (longitudinal) enumeration of household population and also from the cross-sectional survey of households carried out during 2008–09 in the study area were analyzed. A univariate analysis was carried out and followed by an application of binary logistic regression model to identify significant factors associated with infant mortality.
Results
Despite a substantial increase in institutional deliveries in the study area, infant mortality rate remained relatively constant at 43±1. Socioeconomic variables such as education and household economic status and environmental variables such as access to safe drinking water and sanitation facility and use of clean cooking fuel emerged as significant predictors of infant survival.
Interpretation & Conclusions
Promoting institutional deliveries by providing cash assistance to women by itself cannot be expected to bring down infant mortality to a low level in the absence of an improvement in socioeconomic and environmental conditions of the households.
Keywords: Determinants, infant mortality, relative risk (odds ratio)
Introduction
India has the highest number of infant deaths (1.45 million annually), contributing about 23% to the global burden of infant deaths1. Despite several interventions implemented for the improvement of infant survival, the pace of decline in infant mortality rate (IMR) during the last two decades has been rather slow. It declined from 94 in 1988 to 70 in 1998 and 44 in 2011, representing an annual decline of only 2.3% during this period 2. The data generated from the three rounds of National Family Health Survey (NFHS) also showed similar pattern of decline. The IMR declined from 79 in 1992–93 (NFHS-1) to 57 in 2005–06 (NFHS-3), amounting to a decline of just 2.1% per year in 13 years 3. Early neonatal deaths contributed to 53.2% of total number of infant deaths in 2010 4. As per Millennium Development Goals (MDGs) set by the United Nations, India was committed to reduce infant mortality by two-thirds between 1990 and 20155. Achieving the 2015 target demands a higher rate of decline: an average decline of 9.8% per year between 2011 and 2015 would enable the attainment of a rate of 26.7 set as goal by 2015. If the rate of decline experienced during 2000–2011, is continued, the country’s IMR can best be about 35 by 2015 and thereby the MDG cannot be achieved. The Tenth Plan Document observes that the above goal set for IMR could be achieved only with simultaneous efforts towards bringing the neonatal mortality rate (NNMR) to below 19 per 1000 live births by 2010 6. National Population Policy (NPP 2000)7 as well as the National Rural Health Mission (NRHM 2005)8 have underscored the importance of institutional deliveries for significantly reducing maternal mortality ratio (MMR) and NNMR. With a view to increasing the institutional delivery, the government of India, as part of NRHM, launched a safe motherhood scheme called Janani Suraksha Yojana (JSY), a countrywide conditional cash transfer scheme 9. Implementation of JSY in Andhra Pradesh enabled an increase in the proportion of deliveries in health facilities from 59% in 2002–04 to 72% in 2007–0810. However, in spite of this NNMR in Andhra Pradesh has been hovering around 33 since 2003. At national level NNMR has declined very marginally from 37 in 2003 to 35 in 2008 11.
The present study examines the impact of institutional deliveries on infant mortality and its determinants in a population of about 45,000 in a developing region in rural Andhra Pradesh.
Material and Methods
Ethical approval
The study was approved by the Ethics Committee of the MediCiti Institute of Medical Sciences, Hyderabad.
Study Setting
The study was done in Medchal Mandal, Rangareddy district, Andhra Pradesh. Medchal Mandal has a town with 40 villages and 25panchayats. It had a population of approximately 45,000 in 2008, excluding Medchal town. There were 10176 households.
Study design
The study consists of two parts: A. Longitudinal study (REACH = Rural Effective Affordable Comprehensive Health Care): In 1995 NGO SHARE INDIA initiated REACH project with the prime objective of improving MCH services including immunization provided to rural population of Medchal Mandal. Details of REACH project and results of immunization are reported elsewhere12. Initially REACH project included a few villages but from the year 2000 onwards all villages of Medchal Mandal were covered. A dynamic data base of all households was maintained with the help of 40 community health volunteers, two health supervisors, two coordinators and a project director. The data were updated weekly. Each birth was monitored, site of delivery noted and every infant death, by age at death, was documented. Live births per year varied between 735 and 1061. The electronically available REACH data were analyzed to study the trends in the institutional delivery and various components of infant mortality. B. Cross-sectional survey: In 2008–2009, SHARE INDIA also carried out a cross-sectional survey of all households in all villages of Medchal Mandal. An informed consent for participation in the household survey was obtained from all household heads and currently married women aged 15–49 years who were eligible for individual interview. The household questionnaire was used to collect socio-demographic characteristics of household members, information on household conditions and possession of household items. Questionnaire administered to women obtained data on background characteristics of women, their birth history including survival status of all births, contraceptive use, antenatal care, delivery and postnatal care, child immunization and child health and utilization of Integrated Child Development Services (ICDS). A survey team consisting of 3 supervisors and 12 investigators carried out the fieldwork. The survey staffs were given an intensive training for 2 weeks on survey procedures and conduct of interviews. The questionnaires were pretested on a small sample of households. The number of households surveyed was 10176. The number of live births were 4112 with 182 infant deaths during the five year period preceding the survey. The calculated IMR and NNMR were, respectively, 44.3 & 32.3 per 1000 live births for the five year period preceding the survey.
Analysis
The Longitudinal REACH data (A) were analyzed for assessing the impact of escalating institutional deliveries on IMR. Pearson correlation coefficients between trends in institutional delivery and various components of infant mortality were calculated. Cross-sectional survey data (B) were analyzed to examine the differentials in infant mortality by selected demographic, socioeconomic and household environmental variables (Table 1). Univariate and multivariate logistic regression analyses were performed using the SPSS version 17.0. We used the binary logistic regression model after controlling for the effects of other confounders, for identifying the significant predictors of infant mortality, taking ‘yes’ or ‘no’ response for occurrence of infant death during 0–4 years preceding the survey as the response variable.. The other background variables were taken as covariates in the analysis. The results of logistic regression analysis are expressed in terms of odds ratios (OR) and 95% confidence intervals (CIs).
Table 1.
Infant mortality rates and odds ratios for the five year period preceding the survey by selected background variables, Medchal mandal, 2008–09.
| Variable | IMR | Odds Ratio (95% CI) |
|---|---|---|
| Demographic variables | ||
| Sex of child | ||
| Female# | 42.3 | 1 |
| Male | 46.1 | 1.09 (0.81–1.47) |
| Mother’s age at birth | ||
| 15–19# | 81.1 | 1 |
| 20–29 | 42.9* | 0.69 (0.49–0.98)* |
| 30–39 | 33.2* | 0.90 (0.42–1.95) |
| Birth order: | ||
| 1# | 48.8 | 1 |
| 2 | 30.8* | 0.62 (0.43–0.89)** |
| 3 and above | 58.4 | 1.16 (0.80–1.67) |
| Previous birth Internal | ||
| < 24 months# | 57.3 | 1 |
| 24–47 months | 44.4 | 1.3(1.16–1.41) |
| 48+ months | 42.4 | 1.04(0.89–1.23) |
| Single/Multiple birth | ||
| Single# | 40.2 | 1 |
| Multiple | 226.2* | 7.22 (4.22–12.35)** |
| Socioeconomic variables | ||
| Mother’s education | ||
| Illiterate# | 53.2 | 1 |
| Litrateup to middle school | 46.6 | 0.85 (0.59–1.23) |
| High school and above | 35.4* | 0.65 (0.46–0.93)** |
| Father’s Education | ||
| Illiterate# | 62.6 | 1 |
| Lit. up to middle school | 34.1* | 0.60 (0.45–0.81) |
| High school and above | 37.4* | 0.58 (0.42–0.82)* |
| Mother’s Work status | ||
| Not working# | 37.5 | 1 |
| Working | 60.8* | 1.63 (1.20–2.02)** |
| Father’s Occupation | ||
| Agriculture & related# | 44 | 1 |
| Service (govt. & private) | 40.5 | 0.96 (0.61–1.51) |
| Other | 47.7 | 1.12 (0.72–1.76) |
| Religion | ||
| Hindu# | 43.1 | 1 |
| Muslim | 61.4 | 1.45 (0.87–2.43) |
| Christian | 38.4 | 0.89 (0.32–2.44) |
| Caste/Tribe | ||
| SC & ST# | 57.4 | 1 |
| Other backward castes | 39.4* | 0.67 (0.48–0.98)** |
| Other castes | 40.8* | 0.54 (0.54–0.83) |
| Standard of Living Index (SLI)a | ||
| Low# | 56.8 | 1 |
| Medium | 44.5 | 0.77 (0.55–1.09) |
| High | 32.3* | 0.55 (0.37–0.83)** |
| Household Environment | ||
| Type of House | ||
| Pucca# | 39.3 | 1 |
| Non-pucca | 50.6 | 1.04(0.97–1.76) |
| Electricity | ||
| Available# | 42.7 | 1 |
| Not available | 98.9* | 2.25 (1.07–4.74)* |
| Cooking fuel | ||
| Clean fuel# | 40.4 | 1 |
| Unclean fuel | 47.4 | 1.54 (1.12–2.11)* |
| Separate room for Kitchen | ||
| Available# | 33.7 | 1 |
| Not available | 50.6* | 1.61 (1.07–2.41)* |
| Source of drinking water | ||
| Bottled water# | 32 | 1 |
| Piped water | 51.5* | 1.62(1.16–2.26)** |
| Toilet facility | ||
| Hygienic# | 45.1 | 1 |
| Unhygienic | 35.3 | 1.09 (0.60–2.00) |
| No facility/bush | 44.1 | 5.89 (4.19–8.30)** |
| Total | 44.3 | |
IMR: Infant mortality rate is defined as the number of infant deaths per 1000 live births for the five-year period preceding the survey.
The standard of living in a household is defined in terms of ownership of household goods. Following the procedure adopted in National Family Health Survey (NFHS-2), different scores were given to various household goods and a summary household measure called the standard of living index (SLI) was computed by adding the scores of the individual items. Index scores range from 0–20 for low SLI, 21–31 for medium SLI and 32+ for high SLI.
Flush or pour flush are considered as a hygienic toilet & pit latrine/dry toilet is considered as a unhygienic toilet. Note: Subgroup differences in infant mortality rate were tested for statistical significance using a test of proportions of two samples.
Reference category used in logistic regression analysis.
p< .01;
p< .05
Source: Cross-sectional survey in Medchal Mandal, 2008–09.
Results
Institutional Delivery and Infant Mortality
The proportion of institutional deliveries in the study area has increased steadily from 81% in 2001 to 96% in 2010, and as a result, the share of home deliveries has gone down steeply from 19% to 4% during this period. It is interesting to observe that a significant proportion of deliveries have occurred in the private medical sector and this share has steadily increased over the years. It is clear from Figure 1 that an upward trend in the proportion of institutional births during the period 2001–2010 has not been accompanied by a downward trend in the components of infant mortality. For example, the IMR has remained almost constant at 40–43 during the period despite a substantial increase in the proportion of institutional births. Similarly, early neonatal mortality rate (ENMR) and neonatal mortality rate (NNMR) also remained almost stagnant during this period. The Pearson correlation coefficients between institutional delivery and ENMR; institutional delivery and NNMR; and institutional delivery and IMR are, respectively, −0.31, 0.08 and −0.32. All the correlation coefficients are weak and statistically insignificant, suggesting that an increasing trend in the institutional deliveries in the study area has not had any significant lowering effect on any of the components of infant mortality.
Figure 1. Trends in institutional deliveries, early nenonatal mortality rate, and other components of infant mortality, Medchal mandal, 2001 to 2010.
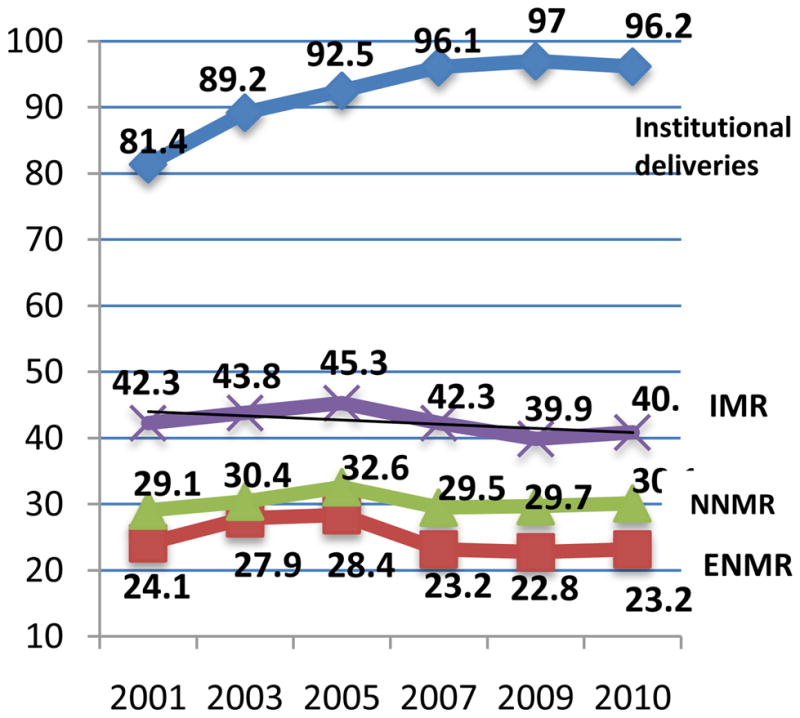
Note: ENMR (early neonatal mortality rate), NNMR (neonatal mortality rate) and IMR (infant mortality rate) are expressed per 1000 live births. All rates are shown as 3-year moving averages.
Demographic Differentials
Both univariate & multivariate analyses of data obtained in the cross-sectional survey revealed that multiple births were associated with higher IMR. Highest IMR was associated with maternal age less than 20 years. Maternal age of 20–29 was ideal for low IMR by both the analytical methods. Gender of the child & previous birth interval did not have significant effect by either analytical method. However, second birth order had significantly lower IMR as compared to first order births. This was revealed by both univariate and multivariate analyses (Table 1).
Socioeconomic Differentials
High standard of living was associated with lower IMR by univariate and multivariate analyses. Mother’s & father’s education (high school &above), working status of the mother and other backward caste (OBC) were associated with lower IMR by both the analytical methods. Other castes compared to SC & ST had a lower IMR which was significant by univariate but not by multivariate analysis. In cases where father was educated up to middle school IMR was lower as compared to illiterate fathers as when tested by univariate but not so by multivariate method. Although Muslim religion tended to be associated with higher IMR, statistical significance was not established (Table 1).
Household Environment
Availability of electricity & a separate room for kitchen and access to bottled water were associated with lower IMR as revealed by both the analytical methods. However, unclean cooking fuel, and lack of toilet facility were significant predictors for high IMR by multivariate but not by univariate analysis. The type of house did not show any significant effect on IMR by either statistical techniques (Table 1).
Discussion
Analysis of our data reveals that a few socioeconomic variables such as woman’s age, education, caste status, woman’s work status and household standard of living index, have statistically significant effects on infant mortality. Several studies have shown that teenage childbearing13,14,15 and mother’s employment16,17 are associated with pre-term birth, low birth weight, high incidence of pregnancy wastage and high infant mortality. Among household environmental factors, use of clean cooking fuel, access to bottled water, availability of electricity and a separate room for kitchen and household access to adequate sanitation facilities are found to have statistically significant positive effects on infant survival. Similar findings were observed by Vinod Mishra et al in 1997 18, NFHS-1 & NFHS – 3 19 & National Human Development Report in 200120. These findings have several policy implications. Since it is not possible to raise the living standards of the households in a short period of time, it is important that government interventions should focus by targeting families at high risk.
Three demographic variables, namely age of the woman, birth order and occurrence of multiple births have significant effects on infant mortality. The chances of infant death in the case of mothers aged 20–29 years are 30% lower than that of infants born to younger mothers under 20 years. The first order births are more likely to experience an elevated risk of dying during infancy as compared to second order births. The higher order births (3+) had higher IMR as compared to first order births and second order births. By reducing the higher order births, the overall level of infant mortality could be reduced. On the other hand, as a result of rapid decline in fertility, the proportion of first order births has increased to 45% in the study area. The larger proportion of first order births tends to increase the level of neonatal mortality because first order births have an elevated risk of dying during neonatal period. This may be one of the reasons for the stagnancy of NNMR during the period 2001–2010 in the study area. However, a substantial reduction in infant mortality could be achieved by reducing or eliminating births to women below 20 years of age because these births have a particularly high risk of infant mortality. Although multitude of health and medical factors affect infant mortality, for logistic reasons, all factors could not taken into account in this study.
One of the interesting findings of this study concerns the relationship between institutional delivery and infant mortality. Government of India perceives that institutional delivery is potentially an important intervention for saving the lives of the newborns, which is the guiding principle behind the Janani Suraksha Yojana (JSY) programme under NRHM. However, our data in the study area and also NFHS data for the state of Andhra Pradesh reveal that an increasing trend in institutional delivery has not been accompanied by a significant decline in either neonatal or infant mortality. The results of the three rounds of NFHS carried out in Andhra Pradesh showed that although institutional deliveries increased substantially from 32.9% in NFHS-1 to 64.4% in NFHS-3, the NNMR has declined only by 5 points, from 45.3 to 40.3 and IMR declined from 70.4 to 53.5 during this 13-year period. Further, a detailed analysis of NFHS-1 data, using multivariate techniques, revealed that after controlling for the effects of such confounding variables as mother’s literacy and household economic status, NNMR for India was found to be higher for children delivered in a medical facility than for children delivered at home 19. However, this should not be taken as grounds for diluting the importance of institutional delivery for saving the lives of mothers and the newborns. Available data for other Indian states need to be examined before arriving at firm conclusions on the effect of an increasing trend in institutional births on infant mortality reduction. Since early neonatal mortality constitutes a significant component of infant mortality, preventing newborn deaths and improving health of the newborn should be the main focus in the intervention programme to bring down IMR to a low level. Increased availability and utilization of antenatal care and subsidization of institutional delivery are just not enough to bring down infant mortality. These measures have been successful in reducing IMR to a certain level, but the rate has been stagnant in recent years even in areas where institutional deliveries are high. This calls for an alternative type of approach to achieve tangible and quick results. A comprehensive and coordinated approach with focus on the promotion of mother-baby package of interventions at various stages of pregnancy, during and after birth are the types of interventions needed to accelerate decline in maternal and neonatal mortality. Access to potable water, improved sanitation facilities, safe cooking fuel with added overall socioeconomic development of the high risk population are the measures warranted to accelerate decline in IMR as per the expectations of MDG and sustain the momentum of decline.
Since the present study was based on one mandal with a population of about 45000, it is not the intention of the authors to generalize the results of the study as pertaining to the state of Andhra Pradesh altogether. However, the findings of the study on the determinants of infant mortality assume policy relevance for formulating suitable intervention programmes to accelerate the tempo of reduction in infant mortality in Andhra Pradesh.
Conclusion
Promoting institutional deliveries by providing cash assistance to women by itself cannot be expected to bring down infant mortality to a low level in the absence of an improvement in socioeconomic and environmental conditions of the households.
Acknowledgments
We express our thanks to Dr. Clareann H. Bunker, Associate Professor, University of Pittsburgh for her help in preparation of this manuscript.
Funding: None
Footnotes
Conflict of interest: None
References
- 1.Population Reference Bureau, Washington. World Population Data sheet. 2010. (computed using data on population, CBR and IMR for India and the world given in the report) [Google Scholar]
- 2.Registrar General, India. Office of the Registrar General, New Delhi, India. Ministry of Home Affairs; and various issues of previous years. SRS Bulletin. 2012 Oct;47(2) [Google Scholar]
- 3.International Institute for Population Sciences and Macro International. National Family Health Survey (NFHS – 3), 2005–06. Mumbai India: 2007. p. 1. [Google Scholar]
- 4.Registrar General, office of the Registrar General, New Delhi, India. Ministry of Home Affairs. Sample Registration System: Statistical Report. 2010. (Report No.1 of 2010) [Google Scholar]
- 5.Government of India. Mid-Term Statistical Appraisal. Central Statistical Organization, Ministry of Statistics and Programme Implementation; New Delhi: 2009. Millennium Development Goals. India Country Report. [Google Scholar]
- 6.Planning Commission. Mid-Term Appraisal of Tenth Five Year Plan (2002–2007) Government of India; New Delhi: 2005. p. 87. [Google Scholar]
- 7.Ministry of Health and Family Welfare. National Population Policy. New Delhi: Department of Family Welfare. MOHFW; 2000. [Google Scholar]
- 8.Ministry of Health and Family Welfare. National Rural Health Mission (2005–2012), Mission Document. New Delhi: MOHFW; 2006. [Google Scholar]
- 9.Ministry of Health and Family Welfare. Janani Suraksha Yojana: Features and Frequently Asked Questions and Answers. Government of India; New Delhi: 2006. [Google Scholar]
- 10.Ministry of Health and Family Welfare, Government of India. Fact Sheets: India, States and Union Territories. IIPS; Mumbai: 2010. District Level Household and Facility Survey 2007–08 (DLHS-3) [Google Scholar]
- 11.Registrar General, Ministry of Home Affairs, Office of the Registrar General. Sample Registration System: Statistical Report 2008. New Delhi, India: 2010. [Google Scholar]
- 12.Tatineni A, Vijayaraghavan K, Reddy PS, Narendranath B, Reddy RP. Health metrics improve childhood immunisation coverage in a rural population of Andhra Pradesh. Indian J Public Health. 2009 Jan-Mar;53(1):41–3. [PubMed] [Google Scholar]
- 13.Olausson Petra Otterblad, Cnattingius Sven, Haglund Bengt. Teenage pregnancies and risk of late fetal death and infant mortality. British Journal of Obstetrics and Gynecology. 1999;106:116–121. doi: 10.1111/j.1471-0528.1999.tb08210.x. [DOI] [PubMed] [Google Scholar]
- 14.Chen Xi-kuan, Wen Shi Wu, Fleming Nathalie, Demissie Kitaw, Rhodes George G, Walker Mark. Teenage pregnancy and adverse birth outcomes: A large population based retrospective cohort study. Int J Epidemiol. 2007;36(2):368–373. doi: 10.1093/ije/dyl284. [DOI] [PubMed] [Google Scholar]
- 15.Olausson PO, Cnattingius S, Haglund B. Teenage pregnancies and risk of late fetal death and infant mortality. British Journal of Obstetrics and Gynaecology. 1999;106(2):116–21. doi: 10.1111/j.1471-0528.1999.tb08210.x. [DOI] [PubMed] [Google Scholar]
- 16.Basu, Malwade Alaka, Basu Kaushik. Women’s economic roles and child survival: The case of India. Health Transition Review. 1991;1(1):83–103. [PubMed] [Google Scholar]
- 17.Kishor Sunitha, Parasuraman Sulabha. Mother’s employment and infant and child mortality in India. International Institute for Population Sciences, Mumbai and Macro International Inc., U.S.A. National Family Health Survey Subject Reports. 1998;8:34–36. [Google Scholar]
- 18.Mishra Vinod, Rutherford Robert. National Family Health Survey Bulletin. Vol. 8. International Institute for Population Sciences; Mumbai: Honolulu: East-West Canter Program on Population; 1997. Cooking smoke increases the risk of acute respiratory infection in children; pp. 1–4. [PubMed] [Google Scholar]
- 19.Pandey Arvind, Choe Minja Kim, Luther Norman Y, Damodarsahu Jagdish Chand. National Family Health Survey subject Reports. Vol. 11. International Institute for Population Sciences; Mumbai: East-West Center Program on population; Hawaii, U.S.A: 1998. Infant and Child Mortality in India; pp. 92–93. [Google Scholar]
- 20.National Human Development Report 2001. Govt. of India; New Delhi: Planning Commission; India: 2002. [Google Scholar]


