Abstract
Objective:
Temperature fluctuations and material mixing times are likely to affect the consistency and integrity of the material mixture, and hence the restoration made out of it. The purpose of the present study was to determine the influence of the ambient temperature and the mixing time of glass ionomer cement (GIC) restorative material on the survival rate of proximal atraumatic restorative treatment (ART) restorations placed in primary molars.
Materials and Methods:
A total of 804 restorations were placed in the primary molars of 6-8-year-olds using the ART approach. The restorations were then followed for a period of 2 years and evaluated at given intervals. The data collected were analyzed using SPSS computer statistical program, and the results tested and compared using the Chi-square, Kaplan Meier survival analysis and Cox Proportional hazard statistical tests.
Results:
The cumulative survival rate of the restorations dropped from the initial 94.4% to 30.8% at the end of 2 years. The higher survival rate of the restorations was associated with the experienced operators and assistants when using the rubber dam isolation method. However, there was no statistically significant difference in the survival rate of the restorations when related to the room temperature and the mixing time of the GIC materials used in spite of the variations in the temperature recoded and the methods used in mixing the materials.
Conclusion:
The ambient temperature and mixing time of GIC did not have a significant effect on the survival of the proximal ART restorations.
Keywords: Glass ionomer cement, mixing time, primary molars, proximal atraumatic restorative treatment restorations, survival rate, temperature
Introduction
Thousands of dental restorations are placed everyday in children by dentists, dental students and ancillary personnel with reasonable clinical background knowledge in the management of dental caries. These restorations are performed at any time and place on the planet earth, yet it is well known that the earth does not have uniform climatic conditions. What might not be so clear to the operators involved in restoring the teeth is whether the different climatic conditions are able to influence the survival outcomes of these restorations. Changes in environmental temperatures and humidity, among other changes, could have a potential influence on the restorative material used and subsequently on the survival results of the restorations made out of them. Further, these restorations are placed in the teeth using materials that need mixing. It is, therefore, possible that defective proportionation and mixing process could result in poor material mixture consistency and, consequently, changes in the integrity of the restoration.
Glass ionomer cement (GIC) is a restorative material that is mixed prior to placing it in the prepared cavity. The mixing process can be mechanical or by hand. The material sets through a simple acid–base chemical reaction. During the mixing stage of the material, the powder part is combined with the liquid part thus commencing the setting phase of the material. On exposure to aqueous solution, the cement powder part of the material reacts with the polycarboxylic acid part, setting up an acid–base reaction that ensues in the formation of a bonding matrix. Initially, the polycarboxylic acid dissociates into negatively charged carboxylate anions (RCOO-) and positively charged protons (H+). The H+ reacts with the surface of the glass filling of the GIC material, the cement-forming metal ions, i.e. Al3+ and Ca2+.[1] In the presence of water, these ions activate the primary setting phase of the GIC reaction that forms a salt gel and complexes with the carboxylate residues of the polycarboxylic acid component. The second stage follows with the release of aluminum ions that get incorporated into the pre-formed matrix to result in a three-dimensional, water-insoluble calcium–aluminum–carboxylate gel that is no longer susceptible to moisture or dehydration.[1] Changes in ambient temperature, the presence of water, the powder particle size and powder/liquid ratio of the material, the mode of mixing the material and the presence of other chemicals like fluoride material and tartaric acid are likely to influence the rate of this reaction process.
The use of GIC with the atraumatic restorative treatment (ART) approach for the management of dental caries, especially in the primary dentition, is well documented. The ART approach involves the removal of dental caries with exclusive use of hand instruments and restoring the cavity formed and sealing the adjacent fissures using GIC, an adhesive restorative material.[2] The ease of mixing the GIC material, the self-setting properties, biocompatibility with the oral tissues and fluoride release mechanisms make GIC an ideal material for use with the ART approach in the prevention and management of dental caries.
Ideally, restorations placed in the primary dentition should last until the teeth exfoliate, meaning a maximum period of approximately 8 years. Good survival results have been obtained in single-surface ART restorations,[3] but not in multi-surface ART restorations.[4] Short-term studies (evaluation after 1 year) using the ART approach have indicated success rates of approximately 80-95% for Class I and 30-75% for Class II restorations. Long-term studies (evaluation after more than 2.5 years) have reported success rates of approximately 43.4-86.1% for Class I and 12.2-82.1% for Class II restorations.[4,5,6] The causes of the ART restoration failures have been found to be multi-factorial and include operator factors like improper caries removal, deficiency in proportionation of the material, poor mixing of GIC, material handling time and poor application of the restorative material,[4] the type of cavity to be restored, the experience of the operator/assistant, poor tooth isolation method and the consistency of the food taken soon after placing the restoration.[7]
The aim of the present study was to determine what influence the ambient temperature and the mixing time of GIC material have on the survival rate of proximal ART restorations placed in primary molars.
Materials and Methods
Subjects
A total of 804 children aged 6-8 years from 30 local schools in Matungulu and Kangundo, Machakos County in Kenya, participated in the study that lasted for 2 years (2006-2008).
Procedure
Random numbers were used to select the children who participated in the study, out of a group that had been previously selected on the basis of having appropriate proximal carious lesions restorable using the ART approach. The initial selection was performed within 2 months of restoring them. The selection of teeth was performed by trained, experienced and pre-tested examiners using the criteria described by Kemoli et al.[8] Written consents were obtained from the parents/guardians and the children also assented to it, prior to their inclusion into the study. The study received ethical approval from the University of Nairobi and Kenyatta National Hospital Ethical Committee prior to its commencement. One proximal cavity was restored in each of the participating children, and then followed.
The restoration phase took place in a specially prepared classroom at each of the 30 schools that participated in the study. Fuji IX (GC Europe), Ketac Molar Easymix (3M ESPE, AG) and Ketac Molar Applicap (3M ESPE, AG) were the three GIC materials that were randomly used during the study to restore the carious primary molars. Two tooth isolation methods were randomly applied (Rubberdam; Medium-dark, Hygienic dental dam, HCM-Hygienic Corporation, Malaysia) with a rubber dam clamp (FIT-Kofferdam Klammer, U67, Hager and Werken GmbH and Co., KG Germany) and cotton wool roll (Hartmann Celluron, De-Paul Hartmann AG-89522, Helderheim, Germany). Two sets of operators and assistants categorized as “experienced” and “inexperienced” as described by Kemoli et al.[8] were randomly paired and restored the teeth using the ART approach. Three “experienced” and four “inexperienced” operators assisted by four “experienced” and four “inexperienced” assistants participated in the operative phase. By rotation, one assistant always rested each day of the restorative phase. Before taking part in the study, all the operators and assistants received adequate training and practice for their respective category. The operators were composed of dentists, final-year dental students and community oral health officers, whereas the assistants were community oral health officers and dental assistants.
During the restoration phase, the child lay prone on a table/desk with the head supported with a pillow and the operator sitting on an ordinary chair placed at the head of the table/desk. Using natural sunlight augmented with an artificial battery-powered headlamp, the oral cavity of the child was illuminated. The operator isolated the cavity and widened the cavity access and removed enamel overhangs with a hatchet and the soft dentine within the cavity was removed using a spoon excavator aided by a caries-detector dye. Wet and dry cotton pellets were utilized to clean and dry the prepared cavity before a matrix band (Union Broach Moyco) was applied to the tooth and held interdental with wooden wedges (Sycomore interdental wedges no. 823, Hawe Neos Dental, Switzerland). The cavity size was measured through its center in the mesio-distal and bucco-lingual directions using Michigan O with William's markings periodontal probe in the same manner as described by Kemoli and van Amerongen.[9] For deep cavities, a thin layer of calcium hydroxide (Dycal, Caulk) was applied at the deepest point before pre-treating the dentine surfaces of the tooth for 15 s using the diluted part of the liquid for Fuji IX and the manufacturer's conditioner for the other two materials. Once the assistant had finished mixing the GIC material, either manually (Fuji IX and Ketac Molar Easymix) or mechanically at 4300 oscillations per minute using a Duomat 2 amalgamator, Germany (Ketac Molar Applicap) in accordance with the instructions of the manufacturer, the material was handed to the operator to restore the prepared cavity.
Once the operator had placed adequate GIC material into the cavity and slightly overfilling the cavity, the operator applied petroleum jelly over the gloved finger and pressed the material firmly into the cavity and over the adjacent fissures in a technique referred to as “finger press”. The excess GIC material was removed using the applier before the occlusion was corrected with the use of a spoon excavator and with the aid of articulating paper (Bausch articulating paper, Nashua, NH03060, USA). The assistant then recorded the time taken to mix the material and the time taken by the operator to complete restoring the cavity. For the mechanical mixing, although the time was constant, it was still recorded. The ambient temperature at the time of completing the restoration was also recorded by the assistant. Afterwards, the child was released with specific instructions not to eat within the next hour.
Evaluations
The restorations were clinically evaluated soon after placement (within 2 h), after 1 week, 1 month, 5 months and then 6-monthly for the remaining period of 2 years using the criteria described in Table 1.
Table 1.
The criteria used to evaluate the survival of the proximal restorations

The evaluators, who were final year dental students, were trained and calibrated in the manner described by Kemoli et al.[8] During the evaluation, the principal investigator (PI) was initially calibrated by an experienced dentist versed with the ART technique. The results of the calibrations showed a mean Kappa value of Kappa 0.92 (n = 20). The PI then calibrated the groups of examiners who evaluated the restorations. The mean Kappa values for the evaluations ranged from 8.4 to 0.86 (n = 52-63), with the mean inter-evaluator consistency of Kappa 0.82-0.92 (n = 48-52). The daily intra-examiner agreements on 10% of the restorations evaluated ranged from Kappa 0.80 to 1.0.
Statistical analysis
SPSS (SPSS Inc, Chicago, IL, USA) data entry computer program was used to process the data collected in the study. Chi-square, Kaplan–Meier survival analysis and Cox Proportional hazard tests with the significant value pegged at P < 0.05 were used for comparison of the survival rate of the restorations in relation to the type of GIC material, operator and dental assistant experience, the method of tooth isolation, the mixing time for the material and temperature at the time of finishing the restoration.
Results
The restoration phase of the study lasted 3 weeks, spread over a period of 1.5 months. From the initial number of participants of 804 aged 6-8 years, at the end of 2 years, a total of 648 participants aged 8-10 years could be evaluated, with the rest having fallen out due to various reasons ranging from absenteeism, truancy and one death. Most of the restored teeth were in the mandibular arch (66.8%), with the rest drawn from the maxillary arch. The initial evaluation of the proximal restorations in the study showed an initial cumulative survival rate of 94.4%, which dropped to 30.8% after 2 years.
During the 2 years when the restorations were followed, no significant differences were noted in the survival rates of the restorations in relation to the type of GIC material used. However, a higher survival rate of the restorations was associated with “experienced” operators when related to the “inexperienced” operators, and the difference was statistically significant (Log-rank, Chi-square 92.04, 1 df, P = 0.15). The cumulative survival of the restorations placed using rubber dam were much higher when related to those where cotton wool rolls were used, and the difference was statistically significant irrespective of the jaw in which the restoration was placed, the operator and the assistant experience used in placing the restorations (Cox PH model, P > 0.05).
In the present study, the assistants did all the mixing of the GIC materials that were used in restoring the cavities besides documenting the mixing and restoration times. Analysis of the survival rate of the proximal restorations in relation to the experience of the assistant indicated that “experienced” assistants were associated with significantly higher survival rate of the restorations they helped place when related to the “inexperienced” assistants (Log-rank, Chi-square 12.41, 1 df, P = 0.0004). Further, the results indicated that there was a significant interaction (Log-rank = chi-square of 15.8181, 3 df, P = 0.0012) between the assistant and the operator experience, and that the inexperience of both the operator and the assistant increased the failure rate of the restorations.
The mixing times for all the assistants during the restoration phase ranged from 11 s to 2 min, with a mean value of 30 s (SD ±0.25). The mixing times, recorded by the assistants, were categorized as less than 30 s, 30-60 s and more than 60 s. The majority of the mixing times were found within either the less than 30 s or the 30-60 s categories. The grouped times were related to the survival rate of the restorations as shown in Figure 1. When the survival rate of the restorations was related to the mixing times as grouped, no statistical significant difference was detected (Cox Proportional hazards model, Est = -0.112, SE = 0.607, Chi-square = 0.034, P = 0.853). However, the highest survival rate of the restorations was associated with the mixing times between 30 and 60 s, followed by those where the mixing times were below 30 s. The “experienced” assistants were also associated with a higher survival rate of the restorations, and their mixing times fell between 30 and 60 s [Figure 1]. The majority of the “inexperienced” assistants inched toward achieving these times toward the end of the restorative phase of the study [Figure 1], when the survival rate of the restorations they helped in placing became closer or equal to those of the “experienced” assistants. The time taken for the assistant to deliver the material to the operator and for the operator to restore the tooth was also considered and related to experience of the assistant. There was no significant statistical difference (Chi-square, P > 0.05). However, the survival rate of the restorations restored by “experienced” operators assisted by “experienced” assistants was higher and statistically significant (Chi-square, P < 0.05) when related to those by “inexperienced” operators and assistants paired together.
Figure 1.
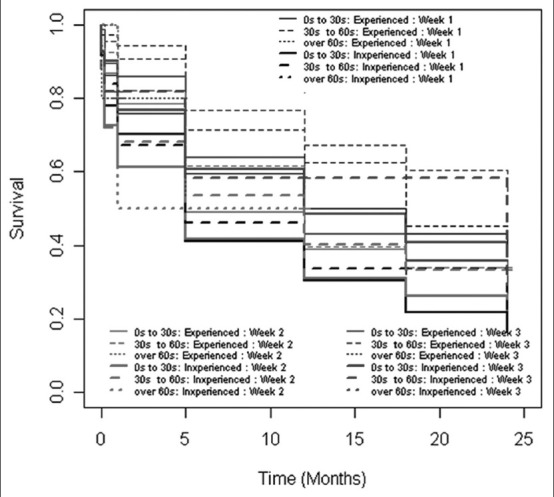
Kaplan–Meier survival analysis for 2 years with regard to the assistant experience, the week of the restoration and the time taken in seconds to mix the glass ionomer cement material during the restoration phase of the study
Multiple logistic model with backward selection for the best model of dichotomized restoration survival in relation to factors as size of restoration, GIC material, isolation method, mixing time, the week when restoration was done and the assistant used showed that there was a significant intercept (DF = 1, Est = -1.0516, SE = 0.2907, Chi-square = 13.086, P = 0.0003). The survival rate of the restorations in relation to the these factors was statistically significant with regard to restoration size DF = 1, Est =0.017, SE = 0.00611, Chi-square = 7.7033, P = 0.0055), rubber dam isolation method (DF = 1, Est = -0.1673, SE = 0.0850, Chi-square = 3.8694, P = 0.0492) and assistant experience (DF = 1, Est = 0.2028, SE = 5.6875, P = 0.0171) and the week when restored (DF = 1, SE = 0.2954, Chi-square = 0.1136, Wald = 0.2954, P = 0.0093). However, this model for predicting the best survival of the proximal ART restorations found that the mixing time did not significantly affect the survival of these restorations (DF = 1, SE = -0.0875, Chi-square = 0.3337, Wald test = 0.0612, P = 0.8046).
During the restoration phase, the temperature at the time of placing the restoration ranged from 19°C to 31°C, with a mean temperature of 24.5°C (±5). The temperatures were grouped as less than 20°C, 20-30°C and above 30°C. When the survival rate of the proximal restorations was related to the ambient temperatures as grouped, there was no significant statistical difference noted. However, those restorations placed when the ambient temperatures were close to the manufacturer's recommended temperature that was within the group 20-30°C, had the highest survival rate. When the tooth isolation method, assistant experience, dental arch, temperature and mixing time as factors were again fitted in the Cox Proportional hazards model test, the results were as shown in Table 2.
Table 2.
The parameter estimates from the cox Proportional hazards model for survival of the restorations in relation to the isolation method, assistant experience, dental arch in which restoration was placed, ambient temperature and mixing time as risk factors
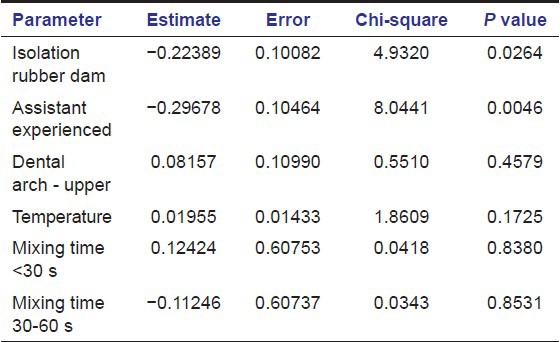
From Table 1, the “experienced” assistants and the use of the rubber dam isolation method appeared to reduce the risk of failure of the restorations. The phenomenon was more pronounced during the third week of the restoration phase and less during the first and second weeks.
Discussion
The longevity of the retention of dental restorations is the most important parameter for determining the success of a dental restorative material. For a long time, amalgam has been the dental restorative material of choice for the treatment of cavitated posterior primary or permanent teeth. However, there has been a recent surge in the number of alternative dental restorative materials. These new materials have been developed to fulfill certain characteristics that amalgam was found to lack, for example, adhesion to the tooth surface, aesthetics, etc. GIC is one of the newer restorative materials first developed in 1972 by Wilson and Kent. Studies conducted to determine the survival rate of restorations placed using GIC have reported varied results. The longevity of ART occlusal restorations in the permanent teeth have been reported to be equal to or greater than the amalgam restorations placed in the same teeth, but in the primary dentition the studies have shown no difference in their survival rate.[10] The failure of these restorations has been attributed to the poor material strength, experience of the operator, the type of cavity, etc.[8,9] However, being a tooth-colored material with tooth adhesive properties, GIC continues to be a preferred restorative material for cavitated primary teeth. Further, GIC has been used in situations where a more conservative cavity preparation is followed (minimal destruction of the tooth) and where its fluoride release characteristics provide further benefits to the affected tooth. In the present study, the GIC materials used were tested for the longevity of the restorations made out of them in relation to the ambient temperature and the mixing time for the material during the restoration phase of the study.
Temperature as a factor
Changes in the ambient temperature would be expected to affect the chemical reaction of GIC. There are countries where temperature fluctuates from the very lowest during the winter season or cold season to the very highest in the summer season or hot season. The open air environment in which the ART approach is carried out might have some effects on the material, considering the seasonal changes for some places. This might be particularly noticeable when the working area is poorly air-conditioned with the temperature not constantly maintained. The possibility that the setting reaction of GIC material will be affected becomes likely in such conditions, by taking a longer or shorter period to set at lower or higher temperatures, respectively. The possibility of the operator leaving the material in the cavity before it is fully set or placing the material in the cavity in its advanced stages of setting is yet another very likely scenario. In the present study, the changes in temperature ranged between 19°C and 31°C during the restoration phase. The temperature range of 12 appears large, yet the results in the present study indicated that there was no significant statistical difference in the survival rate of the restorations in the study. This could have been be due to the varied number of restorations within the two extreme temperatures, compensating for (canceling the effect of each other) what could have probably shown a statistical difference in the survival of the restorations. The manufacturer's recommended ambient working temperature was 23°C for Ketac Molar Aplicapat, 20-25°C for KME and 23°C for Fuji IX. It was evident that restorations that had been placed at temperatures recommended by the manufacturer for the material used in the study had a higher survival rate when related to those placed with temperatures further away from that recommended by the manufacturer. However, the difference between the survival rates was not statistically significant, implying that for the best survival results the material should be mixed at a temperature close to or within that recommended by the manufacturer. Outside the recommended levels, the survival rate of the restorations could be negatively affected.
Mixing time as a factor
Quality mixture of the restorative material (an assistant-dependent factor) should be expected to enhance the survival rate of the restorations made out of the material.[11] It would be reasonable to imagine that the proportionation of the GIC material (powder and liquid) might not be consistent for the hand-mixed type of GIC compared with that already pre-portioned by the manufacturer. In turn, variations in the mixture of the GIC material mixture produced could arise, leading to possible variations in the survival rate of the restorations placed using the material. Mechanical mixing is likely to produce a mixture of GIC with good consistency and results in better survival rate of the restorations. For the materials used in the study, the manufacturer's recommended mixing times were 10, 30 and 20 s, respectively, for KMA, KME and Fuji IX. In the study, the assistants hand-mixed Fuji IX and Ketac Molar Easymix, but the Ketac molar Applicap material had already been pre-portioned by the manufacturer and only mixed by the assistant using the Duomat machine. Yet, there were no significant differences noted between the survival rate of the restorations made out of the hand-mixed and the mechanically mixed GIC. This could imply that the assistants proportioned the two hand-mixed materials rather well.
The “experienced” assistants, in the present study, were associated with a higher survival rate of the restorations after 2 years. Probably, they were able to accurately proportionate and quickly manipulate the hand-mixed material and quickly avail to the same to the operator, while in the case of the mechanically mixed material the handling process was probably performed expeditiously. It is also probable that the “experienced” assistant also simultaneously helped the operator to allay any anxiety in the child thus allowing the operator to concentrate on the critical areas of the restoration process. The reduction in the mixing times for the “inexperienced” assistants with time to mostly 30-60 s and less than 30 s categories during the third operative week could be a pointer to the gain in skills and competence by the assistant.
Conclusion
The changes in ambient temperature and the mixing time for GIC material during the restorations of proximal cavities in primary molars using the ART approach did not significantly influence the survival rate of the restorations.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Wilson AD, McLean JW. Chicago: Quintessence; 1988. Glass Ionomer Cement; p. 37. [Google Scholar]
- 2.Smales RJ, Yip HK. The atraumatic restorative treatment approach for the management of dental caries. Quintessence Int. 2002;33:427–32. [PubMed] [Google Scholar]
- 3.Taifour D, Frencken JE, Beiruti N, van’t Hof MA, Truin GJ, van Palenstein Helderman WH. Comparison between restorations in the permanent dentition produced by hand and rotary instrumentation - survival after 3 years. Community Dent Oral Epidemiol. 2003;31:122–8. doi: 10.1034/j.1600-0528.2003.00027.x. [DOI] [PubMed] [Google Scholar]
- 4.van Gemert-Schriks MC, van Amerongen WE, ten Cate JM, Aartman IH. Three-year survival of single- and two-surface ART restorations in a high-caries child population. Clin Oral Investig. 2007;11:337–43. doi: 10.1007/s00784-007-0138-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lo EC, Holmgren CJ. Provision of atraumatic restorative treatment restorations to Chinese pre-school children - a 30-month evaluation. Int J Paediatr Dent. 2001;11:3–10. doi: 10.1046/j.1365-263x.2001.00232.x. [DOI] [PubMed] [Google Scholar]
- 6.Roeleveld AC, van Amerongen WE, Mandari GJ. Influence of residual caries and cervical gaps on the survival rate of class II glass ionomer restorations. Eur Arch Paediatr Dent. 2006;7:85–91. doi: 10.1007/BF03320820. [DOI] [PubMed] [Google Scholar]
- 7.Kemoli AM, Opinya GN, van Amerongen WE, Mwalili SM. Two-year survival rates of proximal atraumatic restorative treatment restorations in relation to glass ionomer cements and postrestoration meals consumed. Paediatr Dent. 2011;33:246–51. [PubMed] [Google Scholar]
- 8.Kemoli AM, van Amerongen WE, Opinya GN. Influence of the experience of operator and assistant on the survival rate of proximal ART restorations: Two-year results. Eur Arch Paediatr Dent. 2009;10:227–32. doi: 10.1007/BF03262687. [DOI] [PubMed] [Google Scholar]
- 9.Kemoli AM, van Amerongen WE. The dilemma of selecting suitable proximal carious lesions in primary molars for restoration using ART technique. Community Dent Health. 2011;28:12–6. [PubMed] [Google Scholar]
- 10.Frencken JE, Van’t Hof MA, Van Amerongen WE, Holmgren CJ. Effectiveness of single-surface ART restorations in the permanent dentition: A meta-analysis. J Dent Res. 2004;83:120–3. doi: 10.1177/154405910408300207. [DOI] [PubMed] [Google Scholar]
- 11.Frencken JE, Makoni F, Sithole WD. Atraumatic restorative treatment and glass-ionomer sealants in a school oral health programme in Zimbabwe: Evaluation after one year. Caries Res. 1996;30:428–33. doi: 10.1159/000262355. [DOI] [PubMed] [Google Scholar]


