Abstract
Aim:
To assess the impact of dental fear on different domains of oral health-related quality of life (OHRQoL) among school going and non-school going children in the Indian scenario.
Materials and Methods:
The study sample consisted of 279 school children and 257 non-school going children thus making a total sample of 536 children. The sampling frame comprised of 12-15-year-old children attending two upper primary public schools and non-school going children working at shops or not working in Udaipur city, India. Information on dental fear and OHRQoL was obtained by personal interviews by a single trained and calibrated examiner through a structured questionnaire. Intercooled STATA version 9.2 was employed to perform statistical analysis. The level of significance was set at 5%.
Results:
Mean dental fear scores among school going (35.41 [11.79]) and non-school going (47.59 [3.80]) children revealed that dental fear was significantly (P ≤ 0.05) higher among non-school going than among school going children. In school going children, the likelihood of having poor oral symptoms, functional limitation and poorer social and emotional well being were significantly (P ≤ 0.05) lesser as compared with non-school going children.
Conclusions:
Fear has a significant impact on different domains of OHRQoL, except emotional well being, among non-school going children.
Keywords: Dental fear, non-school going, oral health-related quality of life, school going
Introduction
For successful implementation and evaluation of oral health care services for children, dental fear holds a significant concern as it interferes both with the provision and with the acceptance of oral health care services and ultimately affects the oral health-related quality of life (OHRQoL). Data exploring these issues are scanty in the Indian scenario and hence there is an urgent need to consider the impact of dental fear on the functional, emotional and psychosocial dimensions of oral health in children.
Despite a sea change in dental procedures, paraphernalia and anesthetic technology to reduce dental fear among children, the prevalence of dental fear remains almost the same in different parts of the world.[1] This could be attributed to the fact that dental fear is a complex phenomenon, precisely because numerous factors are involved in its prevalence, causes and maintenance.
If a child does not cooperate or is upset during dental treatment, it becomes important for the dentist to look upon the possible reasons for the uncooperative behavior as a child's behavior in later sessions will be influenced by his experience in earlier ones.[2]
Fear is described as an apprehensive and uncomfortable feeling.[3] Dental fear refers to the fear of dentistry. It is not unusual to detect dental fear among patients, which represents a barrier for seeking dental care.[4,5] This leads to avoidance of dental treatment, which may lead to severe general health problems such as fever, septicemia, skin problems, joint and heart problems, facial osteo-myelitis and many more. Failing dental and general health may become a serious source of diffidence and declining self-respect, which negatively affect the OHRQoL in terms of its different dimensions, such as phonetics, chewing efficiency, appearance and, subsequently, social interaction.[6]
Dental fear may affect quality of life. Research revealed that adults suffering from dental fear more often have poorer quality of life than those who do not have dental fear.[7,8]
The United States Surgeon General's report on oral health defines OHRQoL as “a multidimensional construct that reflects (among other things) people's comfort when eating, sleeping, and engaging in social interaction; their self-esteem; and their satisfaction with respect to their oral health”.[9]
Socioeconomic inequalities without fail affect most of the indicators of oral health.[10] Street children (non-school going) represent subjects who are lowest in the social gradient as compared with their counterparts who are school going.[11] Poorer dental health has been seen in lower socioeconomic groups than in higher socioeconomic groups. Similarly, it was found that consistent education and income gradients in both clinical and subjective oral health status have an impact, which are similar to the respective social gradients in general health.[12]
Low socioeconomic status coupled with high dental fear in the non-school going children may lead to dental avoidance, which can critically impede and hamper the very fabric of life and ultimately OHRQoL. Early research on OHRQoL focused on adults, largely because of their better communicative abilities. Studies have shown that adults with dental anxiety/fear suffer from impaired OHRQoL.[13]
As understanding and bewildering of children is difficult because of their developing mental skills and functions; hence, children's assessment is slow to materialize and there is a severe dearth of information that could discover interaction of education (school), dental fear and OHRQoL in children at the international and Indian levels. Hence, the aim of the present study was directed toward investigating the impact of dental fear on OHRQoL between the school going and non-school going children in Udaipur city and other factors influencing the OHRQoL.
Materials and Methods
A cross-sectional descriptive study was conducted in Udaipur city by permission from the Darshan Dental College and Hospital, Udaipur. Ethical clearance was obtained from the Ethical Review Committee of the Institutional Review Board. Udaipur city was divided into five parts: North, south, west, east and central. From each part, two schools - one private and one government - were randomly selected and from them students were selected by simple random sampling. For non-school going children, a convenience sampling strategy was applied and they were singled out from the streets or working at shops from the same area.
The study sample consisted of 207 school children and 193 non-school going children, thereby making a total sample of 400 children who were in the age group of 12–15 years.
Members of the research team had made preliminary contact with the authorities in the targeted school, shopkeepers and families of non-school going children and were explained about the purpose and nature of the study, including the children over there. Permission to carry out the survey was obtained from school authorities, families and shopkeepers. Written informed consent was obtained from all the participating children taking due care to maintain the confidential integrity. All the children present on the days of the survey were included and those unwilling to participate were excluded. Data on OHRQoL were collected by personal interviews, which were conducted by a single trained and calibrated investigator. The study was carried out from January to April 2012, and the investigator visited the school and shops everyday to collect data. Additionally, age, gender and dental visiting habits and socioeconomic status (Kuppuswamy scale of Socio economic status) of each subject were recorded.
Dental fear instrument
The questionnaire for assessing dental fear is the Children's Fear Survey Schedule - Dental Subscale (CFSS-DS[14]) introduced by Scherer and Nakamura,[15] the Fear Survey Schedule for Children (FSSFC) as an inventory for assessment for fear in children. Cuthbert and Melamed[14] used this instrument in their research and modified it to assess dental fear. The instrument has been translated into several languages.[16,17,18,19,20,21,22,23] It has good internal and test-retest reliability in English and several other languages.
The criterion validity of the CFSS-DS has been assessed in several ways, including observing a child's behavior during dental treatment,[17,22] comparing chart records of behavioral problems[24,25] and asking the dentist to rate the child's fear.[20,24,26] In these studies, children with higher CFSS-DS scores have been found to display more disruptive and fearful behavior during dental treatment and also were more likely to have histories of disruptive treatment. Children rate their level of fear on a five-point scale, ranging from “not at all afraid” to “very afraid.” Examples of the items are “dentist drilling ‘injections’” and “people in white uniforms.” The dental items are summed to create an index of child's dental fear that ranges from 15 to 75.
OHRQoL instrument
The OHRQoL instrument proposed by Jokovic[27] was used, which consists of four domains: Oral symptoms, functional limitations, emotional well-being and social well-being, and, as with other quality of life measures, assesses the frequency and impact of oral health problems in these domains. Oral symptoms was the first domain that consisted of five questions, such as whether in the last 3 months children had pain in the mouth or bad breath, bleeding gums and mouth sores, etc., The second domain had eight questions about functional limitations, which included questions about difficult in chewing firm foods, in eating/drinking hot/cold food, restricted diet, etc., The third domain was about emotional well being, which had seven questions about feeling shy/embarrassed, anxious/fearful and irritated/frustrated. The fourth domain was about social well being. The responses ranged from 5, “never,” 4 “once or twice,” 3 “sometimes,” 2 “often,” 1 “everyday or almost every day.” Thus, altogether, the least score recorded would be 31 and the highest score recorded would be 155.
Statistical analysis
The data were entered into MS Excel (MS Office version 2007 developed by Microsoft, Redmond, WA, USA) and Intercooled STATA version 9.2 (StataCorp, Lakeway Dr, College Station, TX 77845, USA) was employed to perform statistical analysis. The level of significance was set at 5%.
Mean scores for dental fear among school going children and non-school going children were determined by applying the Chi-square test. The same test was applied for determining the association between dental fear and domains of OHRQoL. A binary logistic regression model was performed to explore the impact of various independent variables taking the OHRQoL as the dependent variable among school going and non-school going children.
Results
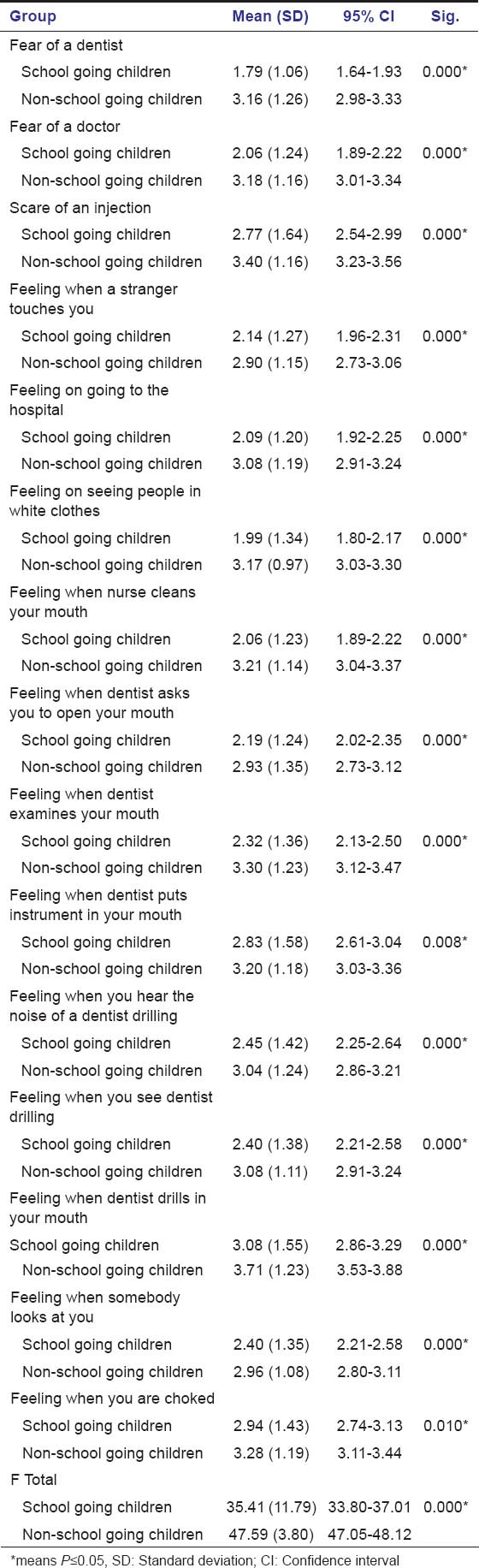
The mean dental fear scores among school going and non-school going children state that dental fear is significantly (P ≤ 0.05) higher among non-school going than among school going children [Table 1].
Table 1.
Mean scores for dental fear among school going children and non-school going children
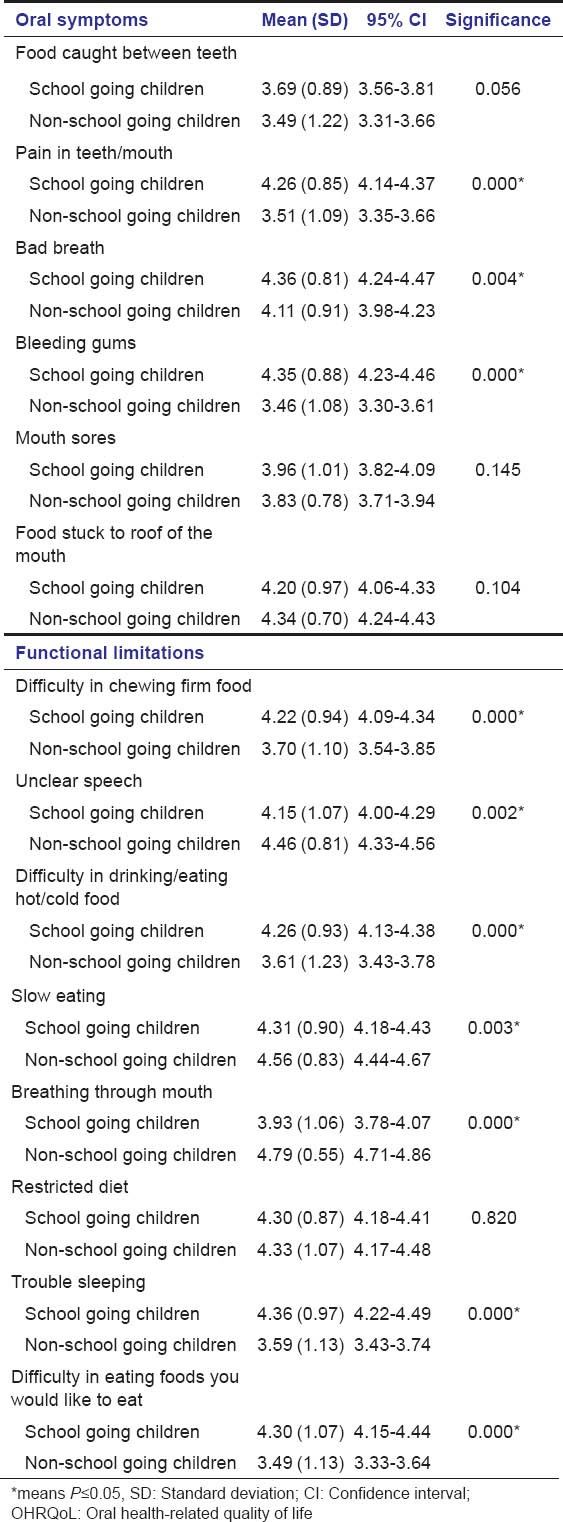
In relation to oral symptoms, school going children recorded significantly higher mean scores for all the items; however, an insignificant difference was observed for question related to food stuck to the roof of the mouth and mouth sores. Non-school going children reported significantly poorer functional status than the comparison group [Table 2a].
Table 2a.
Mean scores for OHRQoL (domain oral symptoms and functional limitation) among school going children and non-school going children
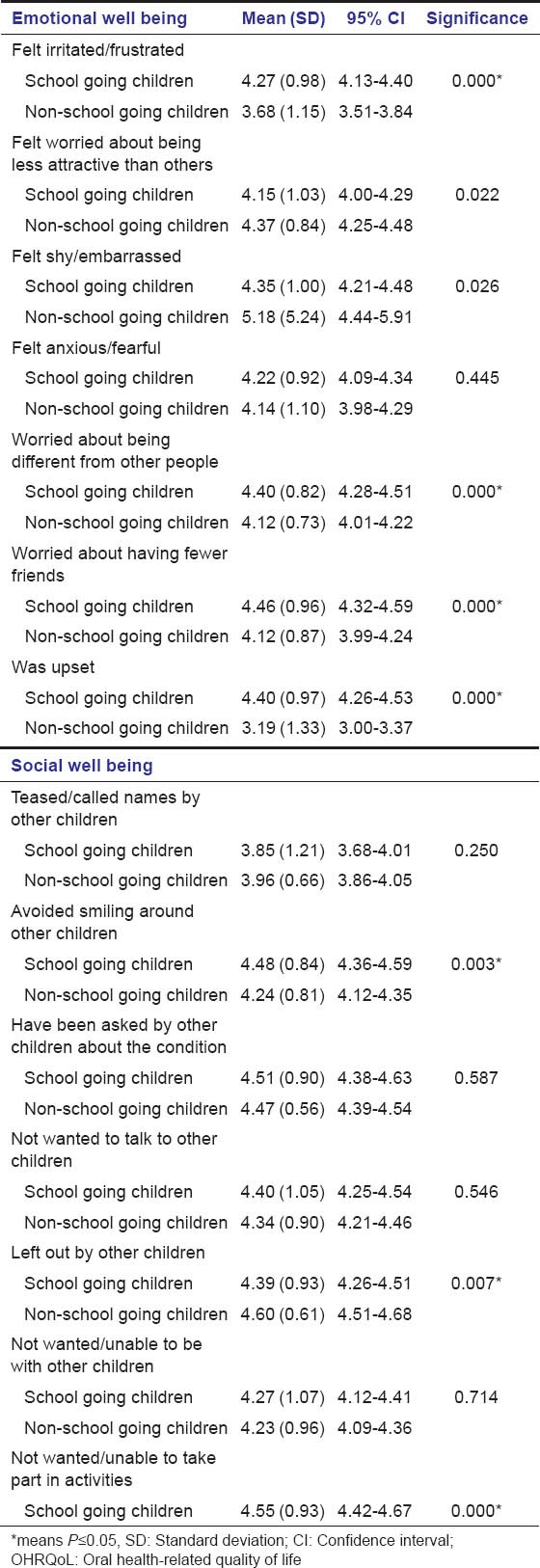
For questions about emotional well being, significant differences in the mean scores were observed for items like “felt irritated,” “worried about being different from other people” and “having fewer friends,” which were 4.27, 4.40 and 4.46 for school going children and 3.68, 4.12 and 4.12 for the other group, respectively. In questions related to social well being, mean scores for items like avoided smiling around other children and not wanted/unable to take part in activities were significantly higher among school going than among non-school going children [Table 2b].
Table 2b.
Mean scores for OHRQL (domain emotional and social well being) among school going children and nonschool going children
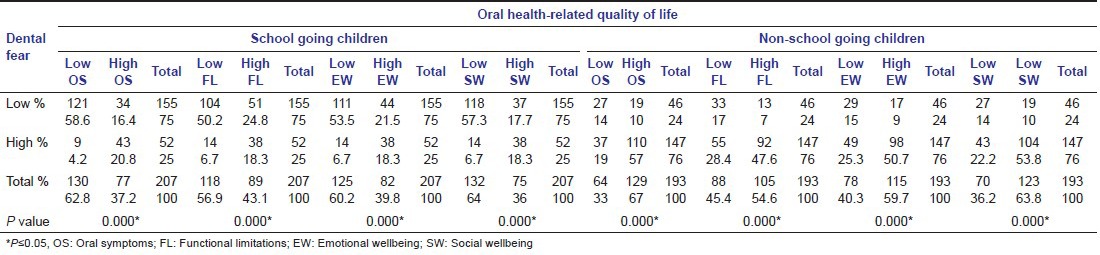
There is a significant association (P ≤ 0.05) between all domains of OHRQoL and dental fear among school going and non-school going children [Table 3].
Table 3.
Association between dental fear and various domains of oral health-related quality of life among school going and non-school going children
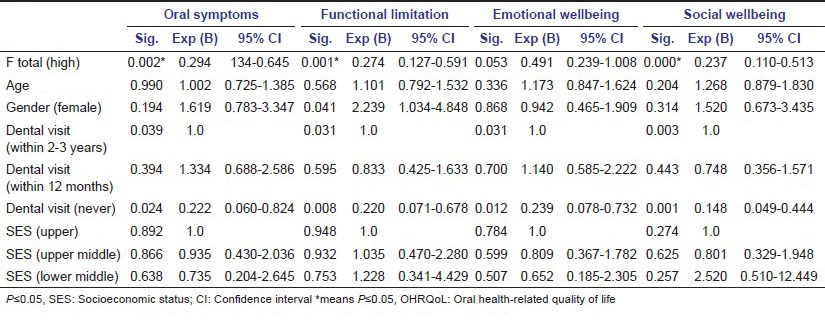
Binary logistic regression has revealed that there is a significant (P ≤ 0.05) impact of dental fear on all domains oral health quality of life except emotional well being in non-school going children [Table 4a].
Table 4a.
Binary logistic regression model to show impact of various independent variables taking OHRQoL as the dependent variable in non-school going children
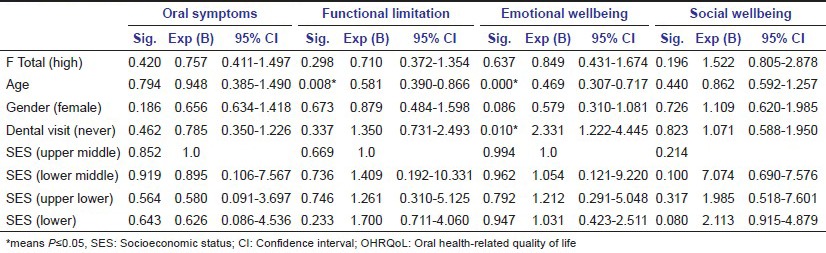
In school going children, age has a significant (P ≤ 0.05) impact on functional limitation and emotional well being. Dental visit has also shown a significant impact on emotional well being [Table 4b].
Table 4b.
Binary logistic regression model to show impact of various independent variables taking OHRQoL as the dependent variable in school going children
Discussion
Dental fear among children, whether school going or non-school going, has all the potential to disrupt OHRQoL. In the Indian scenario, this is the first study that explores the various issues related to impact of dental fear on OHRQoL among school going or non-school going children.
In the present study, the mean dental fear scores were significantly higher among non-school going children as compared with their counterparts. The reason for this finding could be assigned to the fact that certain misconceptions regarding dental treatments run among these low socioeconomic group people, which leads to less exposure to dental treatments; the situation is further complicated by less awareness toward dental procedures, which leads to less utilization. A similar study was carried out by Anni Luoto et al.,[28] revealing poorer OHRQoL in children with cleft lip and palate having dental fear than their counterparts who went to school and had no dental fear.
In the present study, all the domains of OHRQoL were significantly associated with dental fear among school going and non-school going children, but contrasting results have been found in the study done by Anni Luoto et al.,[28] in which associations between Child Perceptions Questionnaire and dental fear were not statistically significant. This may be due to the fact that non-school going children are mainly street children, and among them there is a false impression that dentistry is mainly involved with extraction and is a painful procedure that may be further complicated by wide range of health problems, including malnutrition, communicable and infectious disease, poor oral health, cognitive disorders and learning difficulties.[29] Among school going children, a significant association of dental fear with OHRQoL may be attributed to general fear of dental treatment or unpleasant dental experience in the past.
A higher socioeconomic status in the present study reflected a higher level of education, a higher social status in terms of parental occupation and better living standards in terms of better household conditions. Mean oral symptoms scores of OHRQoL were significantly better in children with higher socioeconomic status. Similar were the observations of Nurelhuda et al.[30] This may be due to their better knowledge, improved accessibility and awareness of superior opportunities for oral health care, which may account for their demand for a better OHRQoL.
In the present study, on applying a logistic regression model, a strong and significant modifying effect of dental fear was seen on all domains of OHRQoL among non-school going children as compared with the study by Anni Luoto et al.,[28] in which a rather strong - although not statistically significant - modifying effect was also observed.
However, this study should be viewed in the light of few limitations, as the role of peers in aggravating or reducing dental fear is not being investigated in the study. Although the sample size is large enough and the findings can be generalized, still, the convenience sampling procedure can be questioned. The present study used self-report questionnaires; the data therefore may be subjected to report bias. Thus, to reduce self-report bias, participants were ensured that all survey responses would be entirely anonymous and would be kept confidential to protect their privacy. Nonetheless, the present study provides an interesting platform for future research to unearth the association between certain multi-factorial concepts. As this study is a new initiative toward understanding of the impact of dental fear on OHRQoL, further multi-centric research will be required to explore this arena and thereby provide a better understanding.
Conclusion
From this study, we conclude that impact of dental fear on OHRQoL was significantly higher among non-school going than school going children due to low socioeconomic status and lack of awareness toward oral health and lack of dental visit. In the future, more research is needed to determine various other factors affecting the impact of dental fear on OHRQoL.
Acknowledgment
The authors sincerely thank all the school authorities who had given the permission for conducting this research study and all school going and non-school going children for their cooperation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Schuller AA, Willumsen T, Holst D. Are there differences in oral health and oral health behavior between individuals with high and low dental fear? Community Dent Oral Epidemiol. 2003;31:116–21. doi: 10.1034/j.1600-0528.2003.00026.x. [DOI] [PubMed] [Google Scholar]
- 2.Versloot J, Veerkamp JS, Hoogstraten J. Children's self-reported pain at the dentist. Pain. 2008;137:389–94. doi: 10.1016/j.pain.2007.09.025. [DOI] [PubMed] [Google Scholar]
- 3.Smith TA, Heaton LJ. Fear of dental care: Are we making any progress? J Am Dent Assoc. 2003;134:1101–8. doi: 10.14219/jada.archive.2003.0326. [DOI] [PubMed] [Google Scholar]
- 4.Pohjola V, Lahti S, Suominen-Taipale L, Hausen H. Dental fear and subjective oral impacts among adults in Finland. Eur J Oral Sci. 2009;117:268–72. doi: 10.1111/j.1600-0722.2009.00631.x. [DOI] [PubMed] [Google Scholar]
- 5.Yoshida T, Milgrom P, Mori Y, Nakai Y, Kaji M, Shimono T, et al. Reliability and cross-cultural validity of a Japanese version of the Dental Fear Survey. BMC Oral Health. 2009;9:17. doi: 10.1186/1472-6831-9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Locker D. Measuring oral health: A conceptual framework. Community Dent Health. 1988;5:3–18. [PubMed] [Google Scholar]
- 7.McGrath C, Bedi R. The association between dental anxiety and oral health-related quality of life in Britain. Community Dent Oral Epidemiol. 2004;32:67–72. doi: 10.1111/j.1600-0528.2004.00119.x. [DOI] [PubMed] [Google Scholar]
- 8.Mehrstedt M, John MT, Tönnies S, Micheelis W. Oral health-related quality of life in patients with dental anxiety. Community Dent Oral Epidemiol. 2007;35:357–63. doi: 10.1111/j.1600-0528.2007.00376.x. [DOI] [PubMed] [Google Scholar]
- 9.Al Shamrany M. Oral health-related quality of life: A broader perspective. East Mediterr Health J. 2006;12:894–901. [PubMed] [Google Scholar]
- 10.Donaldson AN, Everitt B, Newton T, Steele J, Sherriff M, Bower E. The effects of social class and dental attendance on oral health. J Dent Res. 2008;87:60–4. doi: 10.1177/154405910808700110. [DOI] [PubMed] [Google Scholar]
- 11.Lin YL, Yen YY, Chen HS, Liu YC, Chang CS, Chen CM, et al. Child dental fear in low-income and non-low-income families: A school-based survey study. J Dent Sci. 2013;13:1–7. The correction done by you is correct, we are confirming this. [Google Scholar]
- 12.Sabbah W, Tsakos G, Chandola T, Sheiham A, Watt RG. Social gradients in oral and general health. J Dent Res. 2007;86:992–6. doi: 10.1177/154405910708601014. [DOI] [PubMed] [Google Scholar]
- 13.Ng SK, Leung WK. A community study on the relationship of dental anxiety with oral health status and oral health-related quality of life. Community Dent Oral Epidemiol. 2008;36:347–56. doi: 10.1111/j.1600-0528.2007.00412.x. [DOI] [PubMed] [Google Scholar]
- 14.Cuthbert MI, Melamed BG. A screening device: Children at risk for dental fears and management problems. ASDC J Dent Child. 1982;49:432–6. [PubMed] [Google Scholar]
- 15.Scherer MW, Nakamura CY. A fear survey schedule for children (FSS-FC): A factor analytic Comparison with manifest anxiety (CMAS) Behav Res Ther. 1968;6:173–82. doi: 10.1016/0005-7967(68)90004-1. [DOI] [PubMed] [Google Scholar]
- 16.Chellappah NK, Vignehsa H, Milgrom P, Lam LG. Prevalence of dental anxiety and fear in children in Singapore. Community Dent Oral Epidemiol. 1990;18:269–71. doi: 10.1111/j.1600-0528.1990.tb00075.x. [DOI] [PubMed] [Google Scholar]
- 17.Milgrom P, Jie Z, Yang Z, Tay KM. Cross-cultural validity of a parent's version of the Dental Fear Survey Schedule for children in Chinese. Behav Res Ther. 1994;32:131–5. doi: 10.1016/0005-7967(94)90094-9. [DOI] [PubMed] [Google Scholar]
- 18.Klingberg G, Berggren U, Norén JG. Dental fear in an urban Swedish child population: Prevalence and concomitant factors. Community Dent Health. 1994;11:208–14. [PubMed] [Google Scholar]
- 19.Milgrom P, Mancl L, King B, Weinstein P. Origins of childhood dental fear. Behav Res Ther. 1995;33:313–9. doi: 10.1016/0005-7967(94)00042-i. [DOI] [PubMed] [Google Scholar]
- 20.Ten Berge M, Veerkamp JS, Hoogstraten J, Prins PJ. Childhood dental fear in the Netherlands: Prevalence and normative data. Community Dent Oral Epidemiol. 2002;30:101–7. doi: 10.1034/j.1600-0528.2002.300203.x. [DOI] [PubMed] [Google Scholar]
- 21.Alvesalo I, Murtomaa H, Milgrom P, Honkanen A, Karjalainen M, Tay KM. The Dental Fear Survey Schedule: A study with Finnish children. Int J Paediatr Dent. 1993;3:193–8. doi: 10.1111/j.1365-263x.1993.tb00083.x. [DOI] [PubMed] [Google Scholar]
- 22.Klingberg G. Reliability and validity of the Swedish version of the Dental Subscale of the Children's Fear Survey Schedule, CFSS-DS. Acta Odontol Scand. 1994;52:255–6. doi: 10.3109/00016359409029055. [DOI] [PubMed] [Google Scholar]
- 23.Ten Berge M, Hoogstraten J, Veerkamp JS, Prins PJ. The Dental Subscale of the Children's Fear Survey Schedule: A factor analytic study in the Netherlands. Community Dent Oral Epidemiol. 1998;26:340–3. doi: 10.1111/j.1600-0528.1998.tb01970.x. [DOI] [PubMed] [Google Scholar]
- 24.Ten Berge M, Veerkakmp JS, Hoogstraten J. The etiology of childhood dental fear: The role of dental and conditioning experiences. J Anxiety Disord. 2002;16:321–9. doi: 10.1016/s0887-6185(02)00103-2. [DOI] [PubMed] [Google Scholar]
- 25.Wogelius P, Poulsen S, Sørensen HT. Prevalence of dental anxiety and behavior management problems among six to eight years old Danish children. Acta Odontol Scand. 2003;61:178–83. doi: 10.1080/00016350310003468. [DOI] [PubMed] [Google Scholar]
- 26.Ten Berge M, Veerkamp JS, Hoogstraten J, Prins PJ. The Dental Subscale of the Children's Fear Survey Schedule: Predictive value and clinical usefulness. J Psychopathol Behav Assess. 2002;24:115–8. [Google Scholar]
- 27.Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G. Validity and reliability of a questionnaire for measuring child oral-health-related quality of life. J Dent Res. 2002;81:459–63. doi: 10.1177/154405910208100705. [DOI] [PubMed] [Google Scholar]
- 28.Luoto A, Lahti S, Nevanperä T, Tolvanen M, Locker D. Oral-health-related quality of life among children with and without dental fear. Int J Paediatr Dent. 2009;19:115–20. doi: 10.1111/j.1365-263X.2008.00943.x. HYPERLINK “http://www.ncbi.nlm.nih.gov/pubmed/19250394” \o. “International journal of paediatric dentistry/the British Paedodontic Society and] the International Association of Dentistry for Children”. [DOI] [PubMed] [Google Scholar]
- 29.Reading J. Victoria, BC: University of Victoria, Centre for Aboriginal Health Research; 2009. The crisis of chronic disease among Aboriginal Peoples: A challenge for public health, population health and social policy. [Google Scholar]
- 30.Nurelhuda NM, Ahmed MF, Trovik TA, Åstrøm AN. Evaluation of oral health-related quality of life among Sudanese schoolchildren using Child-OIDP inventory. Health Qual Life Outcomes. 2010;8:152. doi: 10.1186/1477-7525-8-152. [DOI] [PMC free article] [PubMed] [Google Scholar]


