Abstract
We present a rare case of radiopaque lesion with radiolucent rim in the right body of mandible, with history of extraction of involved tooth, which made diagnosis confusing unless pre-extraction intraoral periapical radiography radiograph was recovered, finally diagnosed as benign cementoblastoma. It was surgically managed, with no recurrence of the lesion more than 2 years of follow-up. Benign cementoblastoma is a rare, benign tumor of odontogenic ectomesenchymal origin, usually associated with roots of first mandibular molar.
Keywords: Cementoblastoma, true cementoma, tumor of ectomesenchymal origin
Introduction
Cementoblastoma in the current World Health Organization classification of odontogenic tumor, is in the category of tumors of mesenchyme and/or odontogenic ectomesenchyme with or without odontogenic epithelium.[1] The lesion was first recognized by Noeberg in 1930.[2] The lesion is considered as the only true neoplasm of cementum origin. It generally occurs in young persons, comprises <1-6.2% of all odontogenic tumor and is characterized as being attached to the roots, most frequently associated with first permanent molar.[3] The majority of these tumor are radiopaque, but radiolucent tumor may occur in rare instances. Histologically, it presents as a well-circumscribed tumor composed of cementum like tissue surrounded by a fibrous capsule. The surgical enucleation en masse is the treatment of choice. The recurrence rate is 21.7-37.1%.[4]
Case Report
This was a case report of a 16-year-old male patient who reported to the Department of Oral Medicine, GDC, Ahmedabad with the chief complaint of swelling and mild pain in the right side of the jaw since 6 months, with a history of extraction of 46 because of pain before 6 months in a private dental clinic. On clinical examination, there was diffuse bony hard swelling present in the right body of mandible with normal overlying skin. Intra-orally, there was diffuse bony hard swelling in 46 region with normal overlying mucosa and expanded buccal and lingual cortical plates [Figure 1]. Adjacent teeth were immobile and undisplaced. Radiological examination revealed a well-defined round radiopacity with radiolucent rim in the right body of mandible [Figure 2]. Mandibular occlusal radiograph revealed expansion of buccal and lingual cortical plates. He had pre-extraction intraoral periapical radiography (IOPA) radiograph of 46 region, which showed a well-defined radiopacity surrounded by radiolucent rim attached to roots of 46 [Figure 3]. The typical radiographic presentation of radiopacity attached to root with radiolucent rim suggested of benign cementoblastoma with differential diagnosis of hypercementosis, osteoblastoma, periapical cemental dysplasia and condensing osteitis. The lesion was surgically enucleated and submitted for histopathological examination. Histopathologically it showed a well-circumscribed tumor composed of cementum like tissue surrounded by a fibrous capsule [Figure 4]. The patient was followed-up for 2 years with no recurrence.
Figure 1.
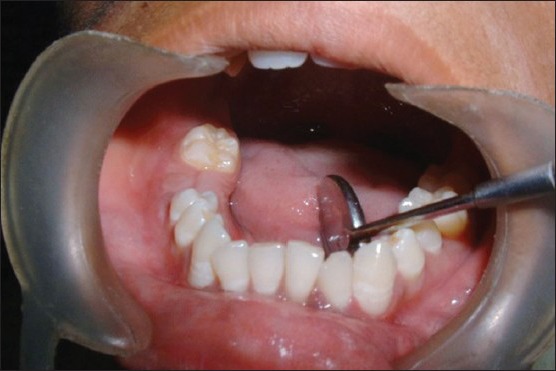
Intra-oral view showing diffuse swelling in right lower quadrant with missing 46 and expansion of buccal and lingual cortical plates
Figure 2.

Right lateral oblique of mandible showing well defined radiopacity surrounded by radiolucent zone in body of mandible with missing 46
Figure 3.

Pre-extraction radiograph showing radiopaque lesion attached to roots of 46
Figure 4.

Microphotograph showing sheet of cementum like tissue with intervening loose fibrovascular connective tissue stroma
Discussion
The presentation of this case was unusual as the patient presented with missing 46. The pre-extraction IOPA clearly showed the tumor attached to the roots. The presented case met the radiographic, surgical and histological criteria of benign cementoblastoma. The male to female ratio of the prevalence has been reported to be 2.1:1 with a mean age of 20.7 years.[5] Benign cementoblastoma is also reported in the maxillary sinus[6] and associated with deciduous[5] and unerupted permanent tooth[7] and multiple teeth.[8] Clinical sign and symptoms include expansion of bone, swelling and pain. The radiographic appearance of benign cementoblastoma is well-defined radiopacity with radiolucent zone.[5] Though it is a benign tumor, but aggressive behavior has been also reported.[2] Some cases reported in the literature exhibited signs of local aggressiveness and destruction, including bony expansion, erosion of cortical plates, displacement of adjacent teeth, maxillary sinus involvement, invasion of the pulp chamber and root canals and extension to and incorporation of adjacent teeth. Expansion, pain and erosion or perforation of bony cortex were seen in a higher percentage of recurrent tumors, but were also seen in non-recurrent tumors. The growth rate for cementoblastoma is estimated to be 0.5 cm/year.[4] The differential diagnosis for a periapical radiopacity include cementoma, osteoblastoma, periapical cemental dysplasia, condensing osteitis and hypercementosis.[2] Histologically, this tumor presents sheets of cementum like tissue, which may contain a large number of reversal lines with active cementoblasts. The irregularly mineralized trabeculae of cementum are fused to the root of the tooth. A band of fibrous connective tissue at the periphery resembling capsule may be present.[9] Cementoblastoma and osteoblastoma are essentially identical histologically and the only distinguishing feature is attachment of cementoblastoma to the root of a tooth. Histologically, the cementoblast in cementoblastoma may be plump with pleomorphic and hyperchromatic nuclei, however, mitotic figures are not seen in cementoblastoma.[10] In contrast to osteoblastoma, the cementoblastoma is an odontogenic tumor that recapitulates cementum deposition similar to that during root formation in the later stages of odontogenesis. Furthermore, the cementoblastoma is continuous with the cemental layer of the apical third of the tooth root and remains separated from bone by a continuation of the periodontal ligament, all of which supports an odontogenic origin.[11] Whereas osteoblastoma arises in the medullary cavity of bones.[2] The treatment of choice is complete removal of the lesion with extraction of associated tooth, followed by thorough curettage and peripheral ostectomy.[4] Cases have been also reported of endodontically preserving the tooth while surgical removal of benign cementoblastoma is done.[12]
Conclusion
We presented a rare case of benign cementoblastoma in mandible and it should be considered in differential diagnosis of bony swellings of mandible. When extraction is attempted in such cases leaving the lesion behind makes the clinical diagnosis difficult. Though the patient had pre-extraction records, which helped in formulating the diagnosis. The patient was followed-up for 2 years with no recurrence.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Huber AR, Folk GS. Cementoblastoma. Head Neck Pathol. 2009;3:133–5. doi: 10.1007/s12105-008-0099-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pynn BR, Sands TD, Bradley G. Benign cementoblastoma: A case report. J Can Dent Assoc. 2001;67:260–2. [PubMed] [Google Scholar]
- 3.Sumer M, Gunduz K, Sumer AP, Gunhan O. Benign cementoblastoma: A case report. Med Oral Patol Oral Cir Bucal. 2006;11:E483–5. [PubMed] [Google Scholar]
- 4.Brannon RB, Fowler CB, Carpenter WM, Corio RL. Cementoblastoma: An innocuous neoplasm? A clinicopathologic study of 44 cases and review of the literature with special emphasis on recurrence. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:311–20. doi: 10.1067/moe.2002.121993. [DOI] [PubMed] [Google Scholar]
- 5.Lemberg K, Hagström J, Rihtniemi J, Soikkonen K. Benign cementoblastoma in a primary lower molar, a rarity. Dentomaxillofac Radiol. 2007;36:364–6. doi: 10.1259/dmfr/58249657. [DOI] [PubMed] [Google Scholar]
- 6.Infante-Cossio P, Hernandez-Guisado JM, Acosta-Feria M, Carranza-Carranza A. Cementoblastoma involving the maxillary sinus. Br J Oral Maxillofac Surg. 2008;46:234–6. doi: 10.1016/j.bjoms.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 7.Dinakar J, Senthil Kumar M, Mathew Jacob S. Benign cementoblastoma associated with an unerupted third molar-A case report. Oral Maxillofac Pathol J. 2010;1:76–78. [Google Scholar]
- 8.Ohki K, Kumamoto H, Nitta Y, Nagasaka H, Kawamura H, Ooya K. Benign cementoblastoma involving multiple maxillary teeth: Report of a case with a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:53–8. doi: 10.1016/j.tripleo.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 9.Napier Souza L, Monteiro Lima S, Júnior, Garcia Santos Pimenta FJ, Rodrigues Antunes Souza AC, Santiago Gomez R. Atypical hypercementosis versus cementoblastoma. Dentomaxillofac Radiol. 2004;33:267–70. doi: 10.1259/dmfr/30077628. [DOI] [PubMed] [Google Scholar]
- 10.Slootweg PJ. Cementoblastoma and osteoblastoma: A comparison of histologic features. J Oral Pathol Med. 1992;21:385–9. doi: 10.1111/j.1600-0714.1992.tb01024.x. [DOI] [PubMed] [Google Scholar]
- 11.Sapp JP, Eversole LR, Wysocki GP. St. Louis: Mosby; 1997. Contemporary Oral and Maxillofacial Pathology; pp. 144–5. [Google Scholar]
- 12.Biggs JT, Benenati FW. Surgically treating a benign cementoblastoma while retaining the involved tooth. J Am Dent Assoc. 1995;126:1288–90. doi: 10.14219/jada.archive.1995.0365. [DOI] [PubMed] [Google Scholar]


