Abstract
Hemangiomas are developmental vascular abnormalities and more than 50% of these lesions occur in the head and neck region, with the lips, tongue, buccal mucosa, and palate most commonly involved. They are considered as hamartomas rather than true neoplasms. Here we report a case of hemangioma of the body of the tongue, discussing the diagnostic aspects and treatment modalities of such lesion and emphasizing the role of the color Doppler ultrasonography, especially in the diagnosis and treatment. Factors such as patient's age, size and site of lesion and the proximity of lesion to vital structure are paramount in the determination of the therapeutic approach and surgical excision. Even though radiotherapy, cryotherapy, laser therapy, medical treatment, injection of sclerosing substances and the selective embolization of the lingual artery seem to have some efficacy, the author conclude that surgery is the therapy of choice in the isolated vascular lesions of the body of the tongue.
Keywords: Cavernous hemangioma, hemangioma, tongue hemangioma
Introduction
Hemangiomas are developmental vascular abnormalities characterized by a proliferative growth phase and by very slow inevitable regression (involutive phase), and about 60% to 70% of the lesions are found in the head and neck region.[1]
International Society for the Study of Vascular Anomalies (ISSVA) has recently provided guidelines to differentiate these two conditions, according to the novel classification first published by Mulliken et al., in 1982. Vasoformative tumors are broadly classified into two groups: Hemangioma and vascular malformation. Hemangioma is histologically further classified into capillary and cavernous forms. Capillary hemangioma is composed of many small capillaries lines by a single layer of endothelial cells supported in a connective tissue stroma of varying density, while cavernous hemangioma is formed by large, thin walled vessels, or sinusoids lined by epithelial cells separated by thin layer of connective tissue septa.[2]
Hemangiomas are considered as benign tumors, being characterized by 3 stages: Endothelial cell proliferation, rapid growth and at last spontaneous involution. The pathophysiology of hemangiomas is attributed to genetic and cellular factors, mainly to monocytes, which are considered the potential ancestors of hemangioma endothelial cells. Imbalance in the angiogenesis, which causes an uncontrolled proliferation of vascular elements, associated with substances such as vascular endothelial growth factor (VEGF), basic fibroblast growth factor (BFGF) and indole-amine 2,3-dioxygenase (IDO), which are found in large amount during proliferative stages, are believed to be the cause.[3]
Case Report
A 17-year old female presented with a swelling in the mouth involving the right anterior 2/3rd of the tongue since one and half years. According to the patient, the swelling was present from one and half years and for the past 6 months, the swelling in the tongue gradually increased to the present size. There were no associated features of pain, fever, difficulty in the speech and swallowing. Past medical, dental and family histories were non-contributory and on physical examination, she appeared to be healthy and, with all her vital signs being within normal limit.
Intra-oral examination [Figure 1], revealed a solitary dome-shaped swelling in the right anterior 2/3rd of tongue extending both dorsally and ventrally, measuring about 1.5 x 2 cm in size. The surface appeared to be smooth and granular with well- defined borders. The swelling was bluish purple in color with normal surrounding area. On palpation the swelling was soft to firm in consistency, non mobile, non tender, afebrile with no palpable thrills and blanched on compression (diascopy).
Figure 1.

Intraoral photograps showing dorsal and ventral extension of lesion on tongue
Depending on the clinical features, a working diagnosis of hemangioma with differential diagnosis of a granular cell myoblastoma, angiomyolipoma, angiosarcoma, hemangiosarcoma and Kaposi's sarcoma were made.
The routine blood and urine investigations were normal. Color Doppler ultrasound revealed hypoechoic lesion measuring 1.3 × 0.5 cm seen in the right anterior lateral aspect of the tongue with intermittent color picking suggestive of vascular lesion. Before surgical excision, feeder vessel was identified by Color Doppler ultrasound. Legation of the feeding vessel was done and surgical excision [Figure 2] was carried out under general anesthesia. Histopathological examination [Figure 3] confirmed the definite diagnosis of cavernous hemangioma. Patient follow up [Figure 4] was done for two years and all the tongue movements were normal and there was no recurrence of the similar lesion.
Figure 2.
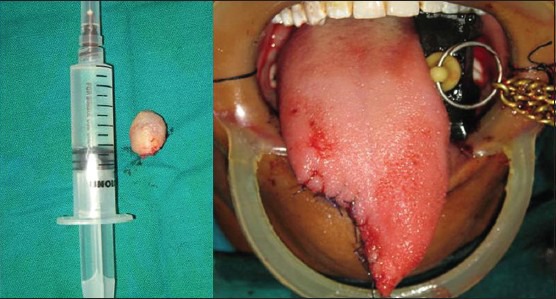
Photograph showing gross specimen of the lesion and intra oral view after surgical excision
Figure 3.
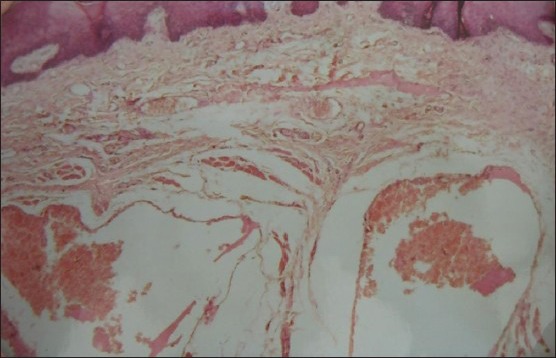
Photomicrograph (H and E ×40) revealing cavernous hemangioma
Figure 4.

Images showing postoperative follow up after (a) 3 months (b) 6 months (c) 1st year (d) 2nd year
Discussion
Hemangiomas show a notorious higher prevalence in females. The head and neck region is more commonly affected especially the face, oral mucosa, lips, tongue and trunk.[4]
The term cavernous hemangioma has traditionally been applied when lesional vascular channels are considerably enlarged.[3] Cavernous hemangiomas consist of deep, irregular, dermal blood-filled channels. They are composed of tangles of thin walled cavernous vessels or sinusoids that are separated by a scanty connective tissue stroma.[5]
With regard to the location and the number of lesions, a similarity with cases reported in the literature was observed, since approximately 80% of the patients present a single lesion, and the head and neck region is the most commonly affected.[3]
Clinically hemangiomas are characterized as a soft, smooth or lobulated, sessile or pedunculated and may be seen in any size from a few milli-meters to several centi-meters. The color of the lesion ranges from pink to red purple and tumor blanches on the application of pressure, and hemorrhage may occur either spontaneously or after minor trauma. They are generally painless.[5]
Although hemangioma is considered one of the most common soft tissue tumors of the head and neck, it is relatively rare in the oral cavity and uncommonly encountered by the clinicians. Radiographic imaging is indicated preoperatively in selected cases where large lesions may impinge on vital anatomical structures, such as the facial nerve or orbit. Computed tomography (CT) and magnetic resonance imaging (MRI) can also be used for volumetric analysis of hemangiomas and vascular malformations.[4] Imaging resources can also be useful in both diagnostic differentiation and analysis of lesion features with regard to its size, extension and location, as well as for follow up of lesions treated under a systemic therapy. In the present case as the biopsy and fine needle aspiration cytology was contraindicated, we used Color Doppler ultrasound to identify the feeding vessel, which helped to legate during surgical procedure. Differential diagnosis between vascular and non-vascular lesions is based on clinical findings and semiotic maneuvers, such as diascopy or glass slide pressure.[3] Baba and Kato reported a case of hemangioma with pleboliths in the floor of the mouth and Doppler ultrasonography, CT, MRI was used to diagnose the lesion.[1]
Management of hemangioma depends on a variety of factors, and most true hemangioma requires no intervention. However, 10-20% requires treatment because of the size, exact location, stages of growth or regeneration. There are many treatment modalities reported in the literature for head and neck hemangiomas, including wait and watch policy, for spontaneous involution, intralesional and systemic corticosteroid treatment, embolization, excision, electrolysis and thermocautery, immunomodulatory therapy with interferon alfa-2a, and laser photocoagulation.[6] Recent interest has centered on interstitial delivery of laser energy to photocoagulate vascular lesions. Currently, sclerotherapy is employed largely because of its efficiency and ability to conserve the surrounding tissues.[4]
Among the sclerosing agents available, excellent results have been reported for sodium morrhuate, sodium sulfate tetradecyl, polidocanol and ethanolamine oleate, and hypertonic glucose solution.[1,3] Growing hemangioma can be treated effectively by systemic drug therapy, sclerotherapy, laser therapy or combined therapy. Transcutaneous and contact applications of laser energy have been studied with the argon and Nd: YAG lasers while the 585-nm flashlamp - pulsed dye laser can be used in cutaneous and subcutaneous hemangiomas.[7] Vesnaver[8] applied photocoagulation with interstitial Nd: YAG laser in 111 patients with vascular lesions in the head and neck region and he concluded that, Nd: YAG laser is a safe and effective tool for treating vascular lesions.
Hemangiomas of the tongue are rare lesions which can cause distressing problem to the patients, producing cosmetic deformity, recurrent hemorrhage, and functional problems with speaking, mastication and deglutition. The treatment depends on lesion location, size and evolution stage, and the patient's age. Due to its side effects, radiotherapy and chemotherapy would not be suitable as a treatment choice for tongue lesion. Swallowing, chewing and speaking function disabilities were seen in the cases where CO2 laser was applied.[1,9]
Surgery is usually indicated when there is no response to systemic treatments, or even for aesthetic reasons, being performed as a simple excision in combination or not with plastic surgery. Conservative or further aggressive forms of treatment may be tried for the hemangiomas of the tongue. Both treatment methods have disadvantages. In the conservative treatment, recurrences may be frequent. On the other hand, aggressive treatment could also cause function loss.[4,5] However, the results of cryotherapy have been reported to have high success rates. Kutluhan[10] used plasma knife surgery for excision of hemangioma of tongue.
Conclusion
The hemangioma is a benign proliferation of endothelial cells common in the head, neck and relatively rare in the oral cavity. In the oral region, the most common location is the lip. Most congenital hemangioma regresses spontaneously without treatment. However we conclude that surgery is the therapy of choice in the isolated vascular lesions involving the body of the tongue.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Okoji VN, Alonge TO, Olusanya AA. Intra-tumoral ligation and the injection of sclerosant in the treatment of lingual cavernous hemangioma. Niger J Med. 2011;20:172–5. [PubMed] [Google Scholar]
- 2.Neville BW, Damm DD, Allen CM, Bouqot . 2nd ed. Philadelphia: WB Saunders; 2002. Oral and Maxillofacial Pathology. [Google Scholar]
- 3.Avila ED, Molon RS, Conte Neto N, Gabrielli MA, Hochuli- Vieira E. Lip Cavernous hemangioma in a young child. Braz Dent J. 2010;21:370–4. doi: 10.1590/s0103-64402010000400015. [DOI] [PubMed] [Google Scholar]
- 4.Bonet- Coloma C, Mínguez-Martínez I, Palma-Carrió C, Galan-Gil S, Penarroche-Diago M, Minguez-Sanz JM. Clinical characteristics, treatment and outcome of 28 oral hemangiomas in pediatric patients. Med Oral Patol Oral Cir Bucal. 2011;16:e19–22. doi: 10.4317/medoral.16.e19. [DOI] [PubMed] [Google Scholar]
- 5.Slaba S, Braidy C, Sader RB, Hokayem N, Nassar J. Giant venous malformation of the tongue: The value of surgiflo. J Mal Vasc. 2010;35:197–201. doi: 10.1016/j.jmv.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 6.Atkins JH, Mandel JE, Mirza N. Laser ablation of a large tongue hemangioma with remifentanil analgosedation in the ORL endoscopy suite. ORL J Otorhinolaryngol Relat Spec. 2011;73:166–9. doi: 10.1159/000328341. [DOI] [PubMed] [Google Scholar]
- 7.Zheng JW, Wang YA, Zhou GY, Zhu HG, Ye WM, Zhang ZY. Head and neck hemangiomas: How and when to treat. Shanghai Kou Qiang Yi-Xue. 2007;16:337–42. [PubMed] [Google Scholar]
- 8.Vesnaver A, Dovsak DA. Treatment of vascular lesions in the head and neck using Nd: YAG laser. J Craniomaxillofac Surg. 2006;34:17–24. doi: 10.1016/j.jcms.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 9.Qureshi SS, Chaukar DA, Pathak KA, Sanghavi VD, Sheth T, Merchant NH, et al. Hemangioma of base of tongue. Indian J Cancer. 2004;41:181–3. [PubMed] [Google Scholar]
- 10.Kutluhan A, Bozdemir K, Ugras S. The treatment of tongue hemangioma by plasma knife surgery. Singapore Med J. 2008;49:e312–4. [PubMed] [Google Scholar]


