Abstract
Background
Mindfulness has been associated with anxiety and depression, but the ways in which specific facets of mindfulness relate to symptoms of anxiety and depression remains unclear. The purpose of the current study was to investigate associations between specific facets of mindfulness (e.g., observing, describing, nonjudging, acting with awareness, and nonreactivity) and dimensions of anxiety and depression symptoms (e.g., anxious arousal, general distress-anxiety, general distress-depression, and anhedonic depression) while controlling for shared variance among variables.
Methods
Participants were 187 treatment-seeking adults. Mindfulness was measured using the Five Facet Mindfulness Questionnaire and symptoms of depression and anxiety were measured using the Mood and Anxiety Symptom Questionnaire.
Results
Bivariate correlations showed that all facets of mindfulness were significantly related to all dimensions of anxiety and depression with two exceptions: describing was unrelated to general distress -anxiety, and observing was unrelated to all symptom clusters. Path analysis was used to simultaneously examine associations between mindfulness facets and depression and anxiety symptoms. Significant and marginally significant pathways were retained to construct a more parsimonious model and model fit indices were examined. The parsimonious model indicated that nonreactivity was significantly inversely associated with general distress anxiety symptoms. Describing was significantly inversely associated with anxious arousal, while observing was significantly positively associated with it. Nonjudging and nonreactivity were significantly inversely related to general distress-depression and anhedonic depression symptomatology. Acting with awareness was not significantly associated with any dimensions of anxiety or depression.
Conclusions
Findings support associations between specific facets of mindfulness and dimensions of anxiety and depression and highlight the potential utility of targeting these specific aspects of mindfulness in interventions for anxiety and mood disorders.
Keywords: Mindfulness, Depression, Anxiety, Adults
Mindfulness, typically defined as the process of attending to present moment experience in a nonjudgmental way (Kabat-Zinn, 1990; Bishop et al., 2004), has been widely integrated into treatments for a variety of psychological symptoms and disorders, particularly anxiety and depression (Evans et al., 2008, Kabat-Zinn et al., 1992; Teasdale et al., 2000). Treatment outcome studies have supported the effectiveness of mindfulness treatments for depression and anxiety (see review by Hofmann et al., 2010). Mindfulness-based treatments include several different techniques drawing from the theorized facets of mindfulness; however, it is not well understood which techniques are most important to the effectiveness of treatment (Holzel et al., 2011). Further, although several researchers have argued for a more targeted application of mindfulness techniques based on specific symptoms of depression and anxiety (see review by Keng et al., 2011), little is known about what particular aspects of mindfulness are associated with different types of symptoms, and thus how to target specific depression or anxiety symptoms with individual mindfulness techniques.
Symptoms of anxiety and depression have been shown to fall reliably into four general clusters (Clark, Steer, & Beck, 1994; Gotlib & Cane, 1989; Watson, 2009). A general distress cluster is found in both depression and anxiety. In depression, this general distress cluster includes negative affect and disorder specific symptoms (such as self-criticism and feelings of worthlessness). In anxiety, the general distress factor includes negative affect and disorder specific symptoms associated with anxious mood (such as worry). A cluster labeled anhedonic depression, characterized by low positive affect/loss of interest, is specific to depression (Watson & Clark, 1991). In contrast, a cluster referred to as anxious arousal, characterized by physiological hyperarousal, is specific to anxiety (Clark & Watson, 1991). Understanding how the individual facets of mindfulness are differentially related to these four symptom clusters of depression and anxiety (i.e., general distress-depression, general distress-anxiety, anhedonic depression, and anxious arousal) could lead to more targeted and effective treatments for patients with different symptom presentations.
In the present study, we investigated the relationships between the different facets of mindfulness and symptoms of general distress-depression, general distress-anxiety, anhedonic depression and anxious arousal in a sample of patients seeking treatment for depressive and anxiety disorders. As we describe below, research on the relationship between mindfulness and depression or anxiety has generally utilized community samples and has examined both mindfulness and depression and anxiety as one-dimensional constructs. We focused on a clinical sample because mindfulness may be related to depression and anxiety differently in patients with severe symptoms when compared to community residents with mild-to-moderate symptoms; knowing the relationships in clinical samples is more informative to clinical practice than knowing the relationships in community samples. We centered our investigation on facets of mindfulness and specific symptoms of anxious arousal, anhedonic depression, and general distress to provide information that could lead to more targeted intervention strategies for patients depending on their symptom presentations.
Facets of Mindfulness
Mindfulness has been theorized to consist of several distinct skills or capacities, including 1) the ability to pay attention and notice experiences in the present, 2) the ability to refrain from judging experience, and 3) the ability to accept positive and negative experience without avoidance or reactivity (Baer, Smith, & Allen, 2004; Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006; Baer et al., 2008; Dimidjian & Linehan, 2003). The multifaceted theoretical conceptualization of mindfulness has also been validated empirically in several studies exploring the factor structure of commonly used scales (Baer et al., 2006; 2008; Christopher, Neuser, Michael, & Baitmangalkar, 2012; Fernandez et al., 2010). Five facets have been identified, including describing, observing, acting with awareness, nonjudging, and nonreactivity (Baer et al., 2006). Describing involves the capacity to label internal experiences with words. Observing refers to the process of noticing or attending to both internal and external experiences. Acting with awareness refers to attending to current activities in the present moment, and is frequently contrasted with operating on ‘auto-pilot’. Nonjudging involves adopting a non-evaluative viewpoint towards thoughts and feelings. Nonreactivity consists of allowing thoughts and feelings to come and go without reacting or fixating on them. This factor structure has provided a foundation for studying mindfulness multi-dimensionally that is derived from both theory and research.
Facets of Mindfulness and General Psychological Distress
Previous studies that have examined the different facets of mindfulness have compared them to symptoms of general psychological distress, which has been characterized by symptoms of both depression and anxiety (rather than as separate constructs). These studies, which have been conducted in non -clinical samples, have typically found that the different facets of mindfulness demonstrate similar relationships to general psychological distress, with the exception of the observing facet. For example, Baer et al. (2006; 2008) found that higher levels of describing, nonjuding, nonreactivity, and acting with awareness were associated with lower levels of psychological distress in both student and community samples, whereas higher levels of observing were associated with more psychological distress. Similarly, Coffey, Hartman and Fredrickson (2010) found that the attentional component of mindfulness (which is conceptually similar to observing) was positively associated with elevated psychological distress. One possible explanation for the positive relationship between observing and symptomatology is that heightened attention to emotions in the absence of a nonjudgmental cognitive stance is characteristic of people with elevated psychological symptoms (Baer et al., 2008; Ingram, 1990; Mor & Winquist, 2002). Aside from observing, mindfulness facets appear to relate uniformly to general psychological distress, but a different picture emerges when symptoms of depression and anxiety are independently measured.
Facets of Mindfulness and Depression or Anxiety
In the few studies exploring associations between specific facets of mindfulness and symptoms of depression and anxiety (rather than overall psychological distress), which again were all in non-clinical samples, differential relationships have been found. Higher non judging was related to lower depression in several studies (Barnhofer, Duggan, & Griffith, 2011; Cash & Whittingham, 2010; Christopher et al., 2012; Desrosiers, Donalds, Anderson, Itzoe, & Britton, 2010), but to lower anxiety in only one study (Cash & Whittingham, 2010). The relationship between nonjudging and depression is consistent with well -validated theories of depression in which self-criticism and negative cognitions are a hallmark of the disorder (see review by Abramson et al., 2002).
In a longitudinal study of college students, increases in observing were related to increases in anxiety, but not depression (Desrosiers et al., 2010). Observing has also been unrelated to depression in other studies (Barnhofer et al., 2011; Cash &Whittingham, 2010). The positive relationship between observing and anxiety, coupled with the positive relationship between observing and psychological distress reviewed above, suggests that higher levels of observing may be associated with heightened attention to internal and external anxiety symptoms.
Acting with awareness was significantly inversely related to symptoms of depression in two community samples (Cash & Whittingham, 2010; Christopher et al., 2012) but not to symptoms of anxiety (Cash & Whittingham, 2010). Describing has been mostly unrelated to depression and anxiety (Cash & Whittingham, 2010; Desrosiers et al., 2010) though one study found an inverse relationship between describing and depression (Barnhofer et al., 2011). Nonreactivity has also been inconsistently related to depressive symptoms, with some studies showing no relationship (Cash & Whittingham, 2010; Desrosiers et al., 2010) and some studies showing that lower nonreactivity is associated with higher depression (Barnhofer et al., 2011; Bohlmeijer et al., 2011; Christopher et al., 2012). Nonreactivity has been associated with worry, a defining characteristic of anxiety (Delgado et al., 2010; Fiask et al., 2012), but it has only been associated with overall anxiety in one study (Bohlmeijer et al., 2011).
A small number of studies have sought to investigate how mindfulness relates to specific symptom clusters in anxiety and depression, particularly anhedonic depression and anxious arousal. Unfortunately, these studies have not also examined mindfulness as a multifaceted construct. Low levels of overall mindfulness have been found to correlate with higher levels of both anxious arousal symptoms and anhedonic depression symptoms in community samples (Bernstein, Tanay, & Vujanovic, 2011; Gonzalez, Vujanovic, Johns, Leyro, & Zvolensky, 2009; Zovlensky et al., 2006). Findings such as these suggest that overall mindfulness may be integrally related to both anxious arousal and anhedonic depression, but in the absence of multi -faceted measurement of mindfulness, the ways in which specific facets of mindfulness relate to anxious arousal symptoms, anhedonic depression symptoms, and general distress anxiety and depression symptoms is still unclear.
In sum, findings generally suggest that mindfulness facets do not operate homogeneously across symptoms of depression and anxiety. Where findings differ across studies, in consistencies could be due to facets of mindfulness relating differently to specific types of depressive or anxiety symptoms. This highlights the importance of understanding the unique relationships of different facets of mindfulness to specific types of symptoms, which is the primary goal of the current study. In consistencies might also have occurred because certain facets of mindfulness relate differently to symptoms of depression or anxiety when they are considered individually compared to when they are considered simultaneously (i.e., when the relationship of one facet to depression and anxiety symptoms is examined while accounting for variance in other facets). This could occur because the facets are intercorrelated, and a bivariate relationship between a given facet and symptoms is actually due to the covariance between that facet and other facets (i.e., a third variable problem). For this reason, we examined relationships between mindfulness facets and symptom clusters through both bivariate correlations (allowing for covariance) and path analysis (controlling for covariance in both symptom clusters and mindfulness facets).
Proposed Differential Relationships between Mindfulness Facets and Symptom Clusters
Although previous studies provide no information on how the different facets of mindfulness are related to the symptom clusters of general distress-depression, general distress-anxiety, anxious arousal, and anhedonic depression, we generated some hypotheses based on theories of mindfulness and/or theories of depression and anxiety. First, we hypothesized that observing would be most likely to be associated with anxious arousal compared to other symptom clusters. As noted earlier, the pattern of results from previous studies suggests that observing (particularly when not combined with a nonjudging stance) may be associated with heightened attention to internal anxiety cues, sometimes referred to as heightened interoceptive (bodily) awareness (Baer et al., 2008; Craig, 2002). The anxious arousal factor of anxiety has been associated with heightened interoceptive awareness (Dunn et al., 2010; Vanden Bogaerde, Derom, & De Raedt, 2011), thus observing may contribute to heightened interoceptive awareness, and thereby to anxious arousal.
Second, we hypothesized that nonjudgment would be associated with both anhedonic depression and general distress-depression subscales because it taps into self-critical thought, which is a cardinal feature of depression (Abramson et al., 2002). Based on the theoretical underpinnings of mindfulness, developing a nonjudgmental, compassionate attitude towards the self is essential to mitigate feelings of guilt or poor self-worth typical of depression (Teasdale, 1999; Teasdale et al., 2000). Additionally, cultivating nonjudgment and compassion may also help generate more positive emotion (Hofmann, Grossman, & Hinton, 2011), which may be particularly pertinent for addressing symptoms of anhedonic depression.
Third we hypothesized that nonreactivity would be associated with general distress-anxiety and general distress-depression subscales because the process of allowing thoughts and feelings to pass through awareness without reacting or fixating on them may be particularly beneficial for reducing negative, repetitive thoughts processes common to both depression and anxiety (i.e, worry, rumination). Also, nonreactivity has been associated with symptoms of general psychological distress (Baer et al., 2006; 2008), and with overall symptoms of anxiety and depression (Barnhofer et al., 2011; de Bruin et al., 2012; Delgado et al., 2010; Fisak et al., 2012), suggesting that it relates to symptoms broadly rather than discriminately (i.e., to anhedonia or anxious arousal).
Fourth, we hypothesized that describing would be associated with anhedonic depression because anhedonia reflects difficulty in the experience or identification of typical feelings in response to situations (Berenbaum, Bredemeier, Thompson, & Boden, 2012). Describing has previously been associated with alexithymia (Baer et al., 2006; de Bruin et al., 2012; Stasieqicz et al., 2012), which is characterized by difficulties identifying and describing feelings and distinguishing between emotions and physical sensation (Bagby, Parker, & Taylor, 1994). In turn, alexithymia has been related to anhedonia and low positive affect (Deary, Scott, & Wilson, 2004; De Gucht, Fischler, & Heiser, 2004).
Finally, we hypothesized that acting with awareness would be associated with general distress-anxiety and general distress-depression, as staying focused on present moment experience is antithetical to cardinal features of generalized psychological distress, such as rumination about past events (i.e., depression) or worry about future events (i.e., anxiety; Holzel et al., 2011; Watkins, 2009). Further, acting with awareness has been associated with general psychological distress (Baer et al., 2006; 2008), depression (Barnhofer et al., 2011), rumination (de Bruin et al., 2012), and worry (de Bruin et al., 2012; Fisak & von Lehe, 2012), indicating that it may relate most to areas of overlap between depression and anxiety rather than to anxious arousal or anhedonic depression specifically.
The Current Study
The current study aimed to address gaps in the literature by investigating the unique associations between each of the five facets of mindfulness (FFMQ; describing, observing, acting with awareness, nonjudging, and nonreactivity) and distinct symptom clusters of depression and anxiety (general distress-anxiety, general distress-depression, anhedonic depression, anxious arousal) in a clinical sample of adults. Considering the multidimensional nature of anxiety and depression symptoms, utilizing measures of specific symptom clusters (i.e., anxious arousal) rather than broad measures of total scores may illuminate important information for differential diagnosis and intervention development. Furthermore, facets of mindfulness may demonstrate unique patterns of associations with specific dimensions of anxiety and depression, both in bivariate correlations and when considered simultaneously, thus providing pertinent information for development and implementation of mindfulness-based interventions for specific populations as well as generation of theoretical models. Examining the relationships between facets of mindfulness and specific symptom clusters in a clinical sample more directly informs clinical practice and intervention development than examining these relationships in non-clinical samples.
Methods
Participants
Participants were 187 adults ages 18–71 (M= 38, SD = 14.2) who were seeking treatment at a mood and anxiety disorders clinic in Connecticut. Participants identified as white (78.8%), African-American (7.4%), Hispanic (8.5%), and ‘other’ (3.7%), and 64.6% of the sample were female. The study was approved by an Institutional Review Board and informed consent was obtained from all participants before inclusion in the study.
Procedure
Prospective participants were excluded if they reported clinically significant symptoms of psychosis, current substance abuse or dependence, or any organic mental disorders. At intake, participants completed a series of self-report measures and were administered a structured clinical interview for DSM-IV Axis I disorders (SCID-I; First, Spitzer, Gibbon, & Williams, 2002) by advanced doctoral student clinicians. All diagnoses were reviewed for reliability by psychologists with expertise in anxiety and mood disorders and determined by consensus diagnosis using clinician severity ratings (CSR), as suggested by the Anxiety Disorders Interview Schedule (ADIS; Dinard, O’Brien, Barlow, Waddell, & Blanchard, 1983). The most prevalent primary Axis I diagnoses among participants were generalized anxiety disorder (42.9%), major depressive disorder (20.1%) and socialphobia (12.2%). A large percentage of the sample (74.1%) also met criteria for a secondary Axis I diagnosis, the most prevalent of which were major depressive disorder (23.3%) and generalized anxiety disorder (14.3%).
Measures
The Five Facet Mindfulness Questionnaire (FFMQ; Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006) is a 39-item self-report questionnaire measuring general proclivity towards mindfulness in daily life. The FFMQ consists of five subscales reflecting the five facets of mindfulness: non-reactivity to inner experiences, observing, acting with awareness, nonjudging of inner experiences, and describing. The Observing subscale measures capacity for noticing or attending to internal and external stimuli (α=.80; e.g., “I pay attention to sensations, such as the wind in my hair or the sun in my face”). The Describing subscale measures the ability to label feelings with words (α=.88; e.g., “I am good at finding words to describe my feelings”). The Nonreactivity subscale assesses capacity to allow feelings to come and go without getting caught up in them (α=.76; e.g., “I perceive my feelings and emotions without having to react to them”). The Nonjudging subscale measures ability to adopt a non-evaluative stance towards thoughts and feelings (α=.91; e.g., “I criticize myself for having irrational or inappropriate emotions”). The Acting with Awareness subscale assesses ability to sustain focused attention on activities in the present moment, in contrast to operating on ‘autopilot’ (α=.89; e.g., “I am easily distracted). Items are rated on a 5-point Likert-type scale, ranging from 1 (never or very rarely true) to 5 (very often oral ways true) where higher scores are indicative of higher levels of mindfulness.
The Mood and Anxiety Symptom Questionnaire (MASQ; Watson& Clark, 1991) short form is a 62-item measure designed to discriminate between symptoms of anxiety and depression as well as to assess symptoms common to both anxiety and depression. The MASQ is divided into four subscales: General Distress-Depression (GD-D), General Distress-Anxiety (GD-A), Anxious Arousal (AA), and Anhedonic Depression (AD). The GD-D subscale consists of 12 items reflecting symptoms of negative affect and distress related to depression (α=.92; e.g., “Felt worthless”, “Was disappointed in myself”). The GD-A subscale consists of 11 items reflecting symptoms of negative affect and distress related to anxiety (α=.82; e.g., “Felt nervous”, “Felt keyed up or on edge”). The AD subscale consists of 22 items measuring symptoms of anhedonia and low positive affect specific to depression (α=.87; e.g., “Felt hopeful about the future”, “felt optimistic”). The AA subscale consists of 17 items assessing symptoms of physiological tension and hyperarousal specific to anxiety (α=.87; e.g., “Startled easily”, “Hands were shaky”). Participants are asked to rate how much they have experienced a given symptom during the past month on a five-point Likert scale ranging from 1 (not at all) to 5 (extremely).
Data Analytic Strategy
The data analysis for this study was conducted in several steps. First, regression imputation was used to replace all missing data (Rubin, 1987). Bivariate correlations were computed to examine the associations between facets of mindfulness and anxiety and depression symptom clusters before controlling for intercorrelations. Next, path analysis was used to simultaneously regress the four mental health outcome variables (e.g., general distress-anxiety, anxious arousal, general distress-depression, anhedonic depression) onto the five mindfulness variables (e.g., describing, observing, acting with awareness, nonjudging, nonreactivity), controlling for the intercorrelations between variables. This approach allowed for a more thorough evaluation of the simultaneous relationships between facets of mindfulness and facets of anxiety and depression than individual regression analyses conducted on each anxiety and depression variable. It also allowed us to distinguish the unique contribution of each facet of mindfulness to anxiety and depression symptom clusters apart from the other facets, thus facilitating a more fine-grained analysis of associations between mindfulness and symptom clusters. As this step of the analysis was focused on the regression analysis and produced a saturated model, model fit was not examined.
As a secondary analysis, results from the first path analysis were used to construct a parsimonious model of the relationships between facets of mindfulness and anxiety and depression. Relationships between mindfulness variables and anxiety or depression variables that had a p value of .10 or less were retained in the second, more parsimonious path model. This model was then tested for fit to study data using the goodness of fit χ2, the root mean square error of approximation (RMSEA), the Comparative Fit Index (CFI), and the Tucker-Lewis Index (TLI). Modification indices were also examined, and additional paths were sequentially added to the model as suggested and evaluated, until no further improvements of model fit were possible. All analyses were conducted using SPSS 18.0 and AMOS 18.0.
Results
Descriptive statistics and bivariate correlations for all study variables are presented in Table 1. Significant inverse relationships were found between each facet of mindfulness and each symptom cluster of anxiety and depression with two exceptions: describing was unrelated to general distress-anxiety, and observing was unrelated to all symptom clusters.
Table 1.
Summary of Means, Standard Deviations, and Intercorrelations for Mindfulness Facets, Depression, and Anxiety
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Observe | - | ||||||||
| 2. Describe | .29** | - | |||||||
| 3. ActAware | .22** | .21** | - | ||||||
| 4. Nonjudge | .16** | .36** | .47** | - | |||||
| 5. Nonreact | .43** | .29** | .27** | .42** | - | ||||
| 6. Anhedonic Dep | −.11 | −.19* | −.28** | −.34** | −.34** | - | |||
| 7. Gen Distress Dep | −.13 | −.23* | −.29* | −.42** | −.31* | .67** | - | ||
| 8. Anxious Arousal | .03 | −.22** | −.18* | −.17* | −.17* | .26** | .36** | - | |
| 9. Gen Distress Anx | −.08 | −.13 | −.21** | −.20** | −.23** | .28** | .48** | .70** | - |
| M | 25.97 | 26.81 | 24.20 | 22.67 | 17.93 | 76.39 | 36.62 | 30.84 | 29.80 |
| SD | 4.26 | 4.90 | 4.92 | 5.93 | 3.78 | 12.95 | 10.69 | 10.82 | 7.59 |
Note.
p < .05,
p < .01
Results of the first path analysis controlling for intercorrelations revealed a differential pattern of associations between mindfulness facets and symptoms of anxiety and depression. Standard Estimates are displayed in Table 2. Higher levels of describing were associated with lower anxious arousal (β = −.44, p = .011). In contrast, higher levels of observing were associated with higher anxious arousal (β = .47, p = .020). Higher nonreactivity was significantly associated with lower general distress-anxiety (β = −.36, p = .034), general distress-depression (β = −.44, p = .049), and anhedonic depression (β = −.87, p = .001). Higher levels of nonjudging were significantly associated with lower levels of general distress-depression (β = − .50, p = .000) and marginally associated with lower anhedonic depression (β = −.35, p = .055) Finally, acting with awareness was marginally inversely related to anxious arousal (β = −.30, p = .090), general distress -anxiety (β = −.21, p = .089), and anhedonic depression (β = −.37, p = .067). Taken together, mindfulness facets accounted for a notable 21% of the total variance in general distress-depression symptoms, 18% of the variance in anhedonic depression symptoms, 10% of the variance in symptoms of anxious arousal symptoms, and 8% of the l variance in general distress-anxiety symptoms.
Table 2.
Standard Estimates for Facets of Mindfulness Regressed Simultaneously on Anhedonic Depression, Anxious Arousal, General Distress Anxiety, and General Distress Depression
| Estimate (SE)
| ||||
|---|---|---|---|---|
| Gen Distress Anxiety | Anxious Arousal | Gen Distress Depression | Anhedonia | |
| Describing | −.07 (.12) | −.44 (.17)* | −.16 (.16) | −.12 (.19) |
| Observing | .09 (.14) | .47 (.20)* | .05 (.19) | .21 (.23) |
| Acting Aware | −.21 (.13)† | −.30 (.18)† | −.23 (.16) | −.37 (.20)† |
| Nonjudging | −.06 (.11) | .00 (.16) | −.50 (.15)*** | −.35 (.18)† |
| Nonreactivity | −.36 (.17)* | −.44 (.24)† | −.44 (.22)* | −.87 (.27)** |
| R2 | .08 | .10 | .21 | .18 |
Note.
p < .10,
p < .05,
p < .01,
p < .005.
p < .10 estimates were retained for secondary analysis examining the more parsimonious path model.
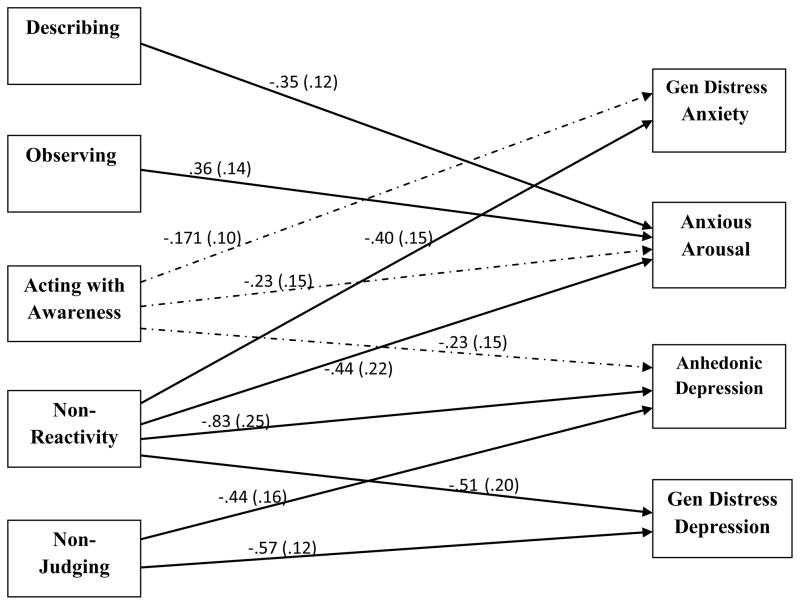
The secondary analysis examined the more parsimonious path model of significant and marginally significant pathways found in the simultaneous regression model (see Figure 1). Results of the more parsimonious model revealed a similar pattern of associations, with the exception that marginally significant paths no longer approached significance. Describing remained significantly inversely associated with anxious arousal (β = −.35, p = .003) and observing remained positively associated with it (β = .36, p = .013). Nonreactivity was significantly inversely associated with symptoms of general distress-anxiety (β = −.40, p = .007) and general distress-depression (β = −.51, p = .011), and anhedonic depression (β = −.83, p = .000). Nonjudging was significantly inversely related to general distress-depression (β = −.57, p = .000) and anhedonic depression (β = −.44, p = .000). Acting with awareness was not significantly associated with any symptom measure of anxiety or depression. Of note, the pathway between nonreactivity and anxious arousal approached significance in the saturated model, but after removing nonsignificant pathways to construct the parsimonious model, the strength of this association increased.
Figure 1.
Final path model describing significant pathways for facets of mindfulness, general distress anxiety, anxious arousal, anhedonic depression, and general distress depression. Error and covariance terms were omitted from this diagram to improve simplicity. Path coefficients and SE indicate above. Boldfaced lines represent significant paths (p < .05) and dotted lines represent nonsignificant paths.
Model fit indices indicated that the parsimonious model was an excellent fit to the data. The goodness of fit test revealed that the covariance structure of the hypothesized model was not significantly different from the actual covariance of the data (χ2 = 5.94, p = .75). Additionally, the RMSEA indicated good model fit (RMSEA = .000), and the CFI and TLI showed good incremental model fit (CFI = 1.00, TLI = 1.02).
Discussion
Findings of the current study showed that all the facets of mindfulness except for observing were related to symptoms of depression and anxiety when considered in bivariate relationships. When covariance among facets and among symptoms was accounted for, however, unique relationships between different facets and symptom clusters emerged. The facets most strongly related to symptom dimensions were generally consistent with our predictions.
First, nonreactivity was significantly inversely related to general distress-anxiety and general distress-depression, suggesting that high cognitive and emotional reactivity is associated with greater nonspecific anxiety and depressive symptoms. This is consistent with findings from clinical samples that higher cognitive reactivity (i.e., reactivation of intrusive negative thoughts and feelings) was associated with relapse in depression symptoms (Segal et al. 2006), but mindfulness based cognitive therapy that included a nonreactivity component mitigated this effect (Kuyken et al., 2010). Similarly, decreases in emotional reactivity to negative self-beliefs have been demonstrated in a sample of clinically anxious adults undergoing mindfulness based stress reduction (e.g., Goldin & Gross, 2010). Current findings suggest that nonreactivity cultivated through mindfulness is important for treating general distress anxiety and depression symptoms, perhaps through targeting common symptoms such as cognitive and/or emotional reactivity to intrusive, repetitive thoughts.
Though not hypothesized a priori, results of the path model indicated that nonreactivity was also significantly inversely related to anhedonic depression. It has been proposed that mindfulness may target low positive emotion and depressive disorders by enhancing emotion regulatory processes (Brown, Ryan & Creswell, 2007; Jiminez, Niles, & Park, 2010). With respect to nonreactivity, allowing distressing thoughts and feelings to pass through one’s mind without become fixated or reacting may interruptor replace maladaptive emotion regulatory mechanisms typically associated with low positive affect.
Although observing was not related to any symptom types in the bivariate correlations, the path analysis showed that high levels of observing were associated with high anxious arousal when accounting for shared variance among variables. This suggests that the aspect of observing that is distinct from the other mindfulness facets is associated with elevated anxious arousal symptoms. High levels of observing without the benefit of other characteristics of mindfulness may represent heightened attention to internal experiences, or interoceptive awareness to anxiogenic physiological processes (Dunn et al., 2010). This suggests that in clinical practice, focused observation of distressing thoughts and feelings during mindfulness practice without sufficient emphasis on cultivation of the other facets (i.e., developing a nonjudgmental stance towards experience) may exacerbate physiological symptoms of anxiety.
In contrast, describing was significantly inversely related to anxious arousal. Describing, or labeling internal experiences with words, may be associated with lower anxious arousal because the ability to describe reflects decreased experiential avoidance of distressing physiological experiences. In order to describe physiological sensations, one must be capable of tolerating the distress associated with the direct experience of those sensations. Reductions in experiential avoidance have been shown to reduce anxiety symptomatology, including hyperarousal and somatic symptoms of anxiety, in clinical samples and also in healthy controls without any history of anxiety (Feldner, Zvolensky, Eifert, & Spira, 2003; Karelka, Forsyth & Kelly, 2004; Spira, Zvolensku, Eifert & Feldner, 2002). Thus, the ability to label internal experiences may help reduce experiential avoidance and in turn, anxious arousal.
The capacity to describe or label internal experience may also be related to lower anxious arousal because describing or labeling physiological sensations facilitates increased concreteness of these experiences. A central objective of cognitive therapy for anxiety disorders is teaching clients to concretely define (or label) their experiences of anxiety, including anxious arousal symptoms (Beck, 2005). Additionally, increased concreteness has been associated with reduced anxiety symptoms, particularly worry, in clinical and non-clinical samples (Behar et al., 2012; Goldwin & Behar, 2012; Stoeber & Borkovec, 2002), and reductions in perseverative thought processes like worry have been associated with decreased physiological arousal and somatic symptom manifestation (Brosschot, Gerin & Thayer, 2006; Brosshot, Pieper & Thayer, 2005).
We hypothesized that describing would be associated with anhedonic depression. Bivariate correlations showed that describing was significantly inversely associated with anhedonic depression, but when the aspects of anhedonic depression that covary with anxious arousal, general distress-anxiety, and general distress-depression were controlled for in path analysis, the relationship between describing and anhedonic depression was no longer significant. Though previous research has shown that difficulties identifying and labeling emotions (i.e., alexithymia) are associated with anhedonic depression (Deary, Scott, & Wilson, 2004; De Gucht, Fischler, & Heiser, 2004), results of the current study suggest that this association may be accounted for by covariations between describing and other facets of mindfulness and/or covariations between anhedonic depression and other symptoms of depression and anxiety. This has implications for clinical work in that describing and labeling internal experience may be less useful in treating symptoms of low positive affect than other facets of mindfulness.
Finally, as hypothesized, nonjudgment was significantly inversely related to general distress-depression and anhedonic depression, suggesting that adopting a non-evaluative view toward distressing thoughts and feelings is associated with lower nonspecific symptoms of depression and anhedonia. Nonjudgment may also relate to lower levels of general distress depression because it is associated with lower levels of certain core features of depression, like self-criticism or negative repetitive thought. For example, nonjudgment has been shown to reduce rumination, which exacerbates depression, enhances negative thinking, and reduces motivation (Jain et al., 2007; Teasedale, Segal & Williams, 1995; Teasedale, 1999; Baer, 2003; c.f. Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008). Regarding the relationship between nonjudgment and anhedonic depression, as self-compassion has been associated with higher positive affect (Frederickson et al., 2008; Wren et al., 2012), cultivating a nonjudgmental stance contribute to self-compassion and acceptance, which then increase experiences of positive affect.
With respect to the acting with awareness facet, results approached significance for general distress-anxiety, anxious arousal, and general distress-depression in the saturated model, which is consistent with previous research demonstrating associations between higher levels of awareness and lower levels of global depression (e.g., Bohlmeijer et al., 2011; Baer et al., 2006; Cash & Whittingham, 2008). However in the final, more parsimonious model, awareness was no longer significantly related to any dimension of anxiety and depression. Thus, when examining how multiple facets of mindfulness simultaneously relate to multiple dimensions of anxiety and depression, the strength of the relationship for acting with awareness is somewhat attenuated due to the salience of other associations. Similar findings have been reported previously in that the inverse association between present moment awareness and anxiety and depression symptoms became non-significant when controlling for other components of mindfulness, like acceptance or nonjudgment (Kohls, Sauer, & Walach, 2009). Paying attention to present moment experience may be necessary to cultivate other aspects of mindfulness, such as nonjudgment or nonreactivity, which then impact symptom levels more directly.
Clinical Implications
Mindfulness-based treatments typically incorporate a range of techniques to cultivate various aspects of mindfulness, including mindful breathing, body scan, and meditation practice (c.f., Kabat-Zinn, 1990; Segal, Williams, & Teasdale, 2002). Though results of the current study should be replicated in a more controlled experiment using both subjective and objective measures, findings suggest the possibility that some techniques may be especially important for patients presenting with particular symptoms. For patients with high anxious arousal, techniques that focus more deliberately on developing the attentional component of mindfulness through observing or noticing internal experience (e.g., mindful eating, body scan) may be less effective, while working on describing or labeling those experiences may be more helpful. Patients with elevated symptoms of anhedonic depression may benefit most from techniques that foster nonreactivity and nonjudgment. For example, loving-kindness meditation and compassion meditation emphasize increasing self-compassion and decreasing judgment (Feldman, 2005; Salzberg, 1995), thus these practices may be particularly effective for alleviating anhedonic depression symptoms. As nonjudgment was also inversely related to general distress -depression, loving-kindness and compassion meditation exercises may be beneficial for reducing these symptoms as well. For patients with high general distress-anxiety or with combinations of high general distress-anxiety and general distress-depression, cultivating nonreactivity through distress tolerance exercises like “urge-surfing” (e.g., see Marlatt, 1994) or breath awareness (c.f., Linehan, 1993; Segal, 2002) may be particularly helpful. While these suggestions are clearly not exhaustive, they illustrate the clinical utility of study findings when delivering mindfulness-based approaches. Considering that patients attend on average less than four sessions before dropping out (Carey, 2006), fine-tuning treatment approaches to have maximum impact in minimal time is pertinent.
Strengths, Limitations, and Conclusions
While our use of a clinical sample was optimal, few limitations to this study warrant mention. Primarily, the cross-sectional and correlational nature of the data precludes any causal inferences and alternate models are possible (e.g., higher levels of physiological arousal may increase frequency of attention and focus on physical sensations, perhaps due to difficulty tolerating pain or discomfort, leading to higher levels of observing). As we were unable to assess change over time, it is possible that associations between certain facets of mindfulness and negative symptoms are more accurately represented by a non-linear or curvilinear relationship in which some symptoms may initially increase before beginning to decrease, and this type of trajectory may further be related to extent of mindfulness practice. Another limitation of our study is that data collection relied exclusively on self-report; therefore, scores may reflect certain self-presentation biases. Important limitations of self -report mindfulness scales in particular have been noted. For example, personal meaningfulness of items may conflate self-ratings, semantic understanding of items may differ across individuals, and self-ratings of mindfulness may differ from actual/observed mindfulness (Grossman, 2008; 2011). Including other measures of mindfulness and anxiety and depression, particularly objective measures, may be helpful in further elucidating distinctive associations between these constructs. Our study also did not access current or past meditation practice. As associations between mindfulness facets and psychological symptoms have been shown to differ slightly as a function of meditation experience (i.e., observing has been positively correlated with psychological symptoms in non-meditators; Baer et al., 2006; 2008; de Bruin et al., 2012), future research in clinical samples should consider frequency and duration of meditation practice. Finally, further research with multiple types of empirically validated measures of mindfulness and symptom clusters of anxiety and depression as well as use of experimental and/or longitudinal designs is encouraged.
Despite these limitations, finding from our study contribute to a developing literature on the association between mindfulness and anxiety and depression. Future studies might attempt to further elucidate the precise nature of this relationship through examining dimensions of mindfulness and dimensions of anxiety and depression at multiple time points within different contexts and populations. The current study provides support for unique associations between specific facets of mindfulness (i.e., nonreactivity, describing, observing, and nonjudgment) and dimensions of anxiety and depression and highlights the potential utility of targeting these specific aspects of mindfulness in interventions for anxiety and mood disorders and related pathology. Results also highlight the importance of the developing literature on mindfulness- and acceptance-based treatments for discrete anxiety and mood disorders as well as non-specific overlapping symptoms of both classes of disorders.
References
- Abramson LY, Alloy LB, Hankin BL, Haeffel GJ, MacCoon DG, Gibb BE. Cognitive vulnerability-stress models of depression in a self-regulatory and psychobiological context. In: Gotlib IH, Hammen CL, editors. Handbook of depression. New York: Guilford Press; 2002. pp. 268–294. [Google Scholar]
- Arch JJ, Craske MG. Mechanisms of mindfulness: Emotion regulation following a focused breathing induction. Behaviour Research and Therapy. 2006;44:1849–1858. doi: 10.1016/j.brat.2005.12.007. [DOI] [PubMed] [Google Scholar]
- Baer RA. Mindfulness training as a clinical intervention: Conceptual and empirical review. Clinical Psychology: Science and Practice. 2003;10(2):125–143. [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self- report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Kreitemeyer J, Sauer, Williams J. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15:329–342. doi: 10.177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Bagby RM, Parker JD, Taylor GJ. The twenty-item Toronto Alexithymia Scale: I. Item selection and cross-validation of the factor structure. Journal of Psychosomatic Research. 1994;38:23–32. doi: 10.1016/0022-3999(94)90005-1. [DOI] [PubMed] [Google Scholar]
- Barnhofer T, Duggan DS, Griffith JW. Dispositional mindfulness moderates the relation between neuroticism and depressive symptoms. Personality and Individual Differences. 2011;51:958–962. doi: 10.1016/j.paid.2011.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A. Anxiety disorders and phobias: a cognitive perspective. Cambridge, MA: Basic Books; 2005. [Google Scholar]
- Behar E, McGowan SK, McGlaughlin KA, Borkovec TD, Goldwin M, Bjorkquist O. Concreteness of positive, negative, and neutral repetitive thinking about the future. Behavior Therapy. 2012;43:300–312. doi: 10.1016/j.beth.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berenbaum H, Bredemeier K, Thompson RJ, Boden MT. Worry, anhedonic depression, and emotional styles. Cognitive Therapy Research. 2012;36:72–80. doi: 10.1007/s10608-010-9329-8. [DOI] [Google Scholar]
- Bernstein A, Tanay G, Vuanovic AA. Concurrent relations between mindful attention and awareness and psychopathology among trauma-exposed adults: Preliminary evidence of transdiagnostic resilience. Journal of Cognitive Psychotherapy: An International Quarterly. 2011;25:99–113. doi: 10.1891/0889-8391.25.2.99. [DOI] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson NC, Carmody J, Devins G. Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice. 2004;11:230–241. doi: 10.1093/clipsy/bph077. [DOI] [Google Scholar]
- Bohlmeijer E, ten Klooster PM, Fledderus M, Veehof M, Baer R. Psychometric properties of the five facet mindfulness questionnaire in depressed adults and development of a short form. Assessment. 2011;18:308–320. doi: 10.1177/1073191111408231. [DOI] [PubMed] [Google Scholar]
- Brosschot JF, Gerin W, Thayer JF. The perseverative cognition hypothesis: A review of worry, prolonged stress-related physiological activation, and health. Journal of Psychosomatic Research. 2006;60:113–124. doi: 10.1016/j.jpsychores.2005.06.074. [DOI] [PubMed] [Google Scholar]
- Brosschot JF, Pieper S, Thayer JF. Expanding stress theory: Prolonged activation and perseverative cognition. Psychonueroendocrinology. 2005;30:1043–1049. doi: 10.1016/j.psyneuen.2005.04.008. [DOI] [PubMed] [Google Scholar]
- Brown KW, Ryan RM, Creswell JD. Addressing fundamental questions about mindfulness. Psychological Inquiry. 2007;18:272–281. [Google Scholar]
- Carey T. Estimating treatment duration for psychotherapy in primary care. Journal of Public Mental Health. 2006;5:23–28. [Google Scholar]
- Cash M, Whittingham K. What facets of mindfulness contribute to psychological well-being and depressive, anxious, and stress-related symptomatology? Mindfulness. 2010;1:177–182. doi: 10.1007/s12671-010-0023-4. [DOI] [Google Scholar]
- Christopher MS, Neuser NJ, Michael PG, Baitmangalkar A. Exploring the psychometric properties of the five fact mindfulness questionnaire. Mindfulness. 2012;3:124–131. doi: 10.1007/s12671-011-0086-x. [DOI] [Google Scholar]
- Clark DA, Steer RA, Beck AT. Common and specific dimensions of self-reported anxiety and depression: Implications for the cognitive and tripartite models. Journal of Abnormal Psychology. 1994;103:645–654. [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Coffey KA, Hartman M, Fredrickson BL. Deconstructing mindfulness and constructing mental health: Understanding mindfulness and its mechanisms of action. Mindfulness. 2010;1:235–253. doi: 10.1007/s1267-010-0033-2. [DOI] [Google Scholar]
- Craig AD. How do you feel? Interoception: the sense of the physiological condition of the body. Nature Reviews Neuroscience. 2002;3:655–666. doi: 10.1038/nrn894. [DOI] [PubMed] [Google Scholar]
- Deary IJ, Scott S, Wilson JA. Neuroticism, alexithymia and medically unexplained symptoms. Personality and Individual Differences. 1997;22:551–564. [Google Scholar]
- De Bruin EI, Topper M, Muskens JGAM, Bogels SM, Kamphuis JH. Psychometric properties of the five facets mindfulness questionnaire (FFMQ) in a meditating and anon -meditating sample. 2012 doi: 10.1177/1073191112446654. [DOI] [PubMed] [Google Scholar]
- De Gucht V, Fischler B, Heiser W. Neuroticism, alexithymia, negative affect, and positive affect as determinants of medically unexplained symptoms. Personality and Individual Differences. 2004;36:1655–1667. [Google Scholar]
- Delgado LC, Pedro G, Perakakis P, Vera MN, de Paso GR, Vila J. Treating chronic worry: Psychological and physiological effects of a training programme based on mindfulness. Behavior Research and Therapy. 2010;48:873–882. doi: 10.1016/j.brat.2010.05.012. [DOI] [PubMed] [Google Scholar]
- Desrosiers A, Donalds R, Anderson M, Itzoe M, Britton W. School based mindfulness training may offer clinical benefits. Poster presented at the World Congress of Behavioral and Cognitive Therapy (WCBCT); Boston, MA. 2010. Jun, [Google Scholar]
- Dimidjian S, Linehan MM. Mindfulness practice. In: O’Donohuse W, Fisher Je, Hayes SC, editors. Empirically supported techniques of cognitive behavior therapy: A step-by-step guide for clinicians. New York: John Wiley; 2003. [Google Scholar]
- Di Nardo PA, O’Brien GT, Barlow DH, Waddell MT, Blanchard EB. Reliability of DSM-III anxiety disorder categories using a new structured interview. Archives of General Psychiatry. 1983;40:1070–1075. doi: 10.1001/archpsyc.1983.01790090032005. [DOI] [PubMed] [Google Scholar]
- Dunn BD, Iolanta S, Evans D, Oliver C, Hawkins A, Dalgleish T. Can you feel the beat? Interoceptive awareness is an interactive function of anxiety-and depression-specific symptom dimensions. Behaviour Research and Therapy. 2010;48:1133–1138. doi: 10.1016/j.brat.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans S, Ferrando S, Findler M, Stowell C, Smart C, Haglin D. Mindfulness- based cognitive therapy for generalized anxiety disorder. Journal of Anxiety Disorders. 2008;22:716–721. doi: 10.1016/j.janxdis.2007.07.005. [DOI] [PubMed] [Google Scholar]
- Feldman C. Compassion. Berkeley CA: Rodnell Press; 2005. [Google Scholar]
- Feldner MT, Zvolensky MJ, Eifert GH, Spira AP. Emotional avoidance: An experimental test of individual differences and response suppression using biological challenge. Behaviour Research and Therapy. 2003;41:403–411. doi: 10.1016/s0005-7967(02)00020-7. [DOI] [PubMed] [Google Scholar]
- Fernandez AC, Wood MD, Stein LAR, Rossi JSR. Measuring mindfulness and examining its relationship with alcohol use and negative consequences. Psychology of Addictive Behaviors. 2010;24:608–616. doi: 10.1037/a0021742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisak B, von Lehe AC. The relation between the five facets of mindfulness and worry in anon-clinical sample. Mindfulness. 2012;3:15–21. doi: 10.1007/s12671-011-0075-0. [DOI] [Google Scholar]
- Frederickson BL, Cohn MA, Coffeey KA, Pek J, Finkel SM. Open hearts buildlives: Positive emotions, induced through loving-kindness meditation, build consequential personal resources. Journal of Personality and Social Psychology. 2008;95:1045–1061. doi: 10.1037/a0013262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Gross JJ. Effects of mindfulness based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion. 2010;10(1):83–91. doi: 10.1037/a0018441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldwin M, Behar E. Concreteness of idographic periods of worry and depressive rumination. Cognitive Therapy and Research. 2012;36:840–846. doi: 10.1007/s10608-011-9428-1. [DOI] [Google Scholar]
- Gonzalez A, Vujanovic AA, Johnson KA, Leyro TM, Zvolensky MJ. The role of mindful attention in regard to the relation between negative affect reduction outcome expectancies and emotional vulnerability among adult cigarette smokers. Cognitive Therapy Research. 2009;33:645–656. doi: 10.1007/s1068-009-9246-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotlib IH, Cane DB. Self-report assessment of depression and anxiety. In: Kendall PC, Watson D, editors. Anxiety and depression: Distinctive and overlapping features. London: Academic; 1989. pp. 131–169. [Google Scholar]
- Grossman P. On measuring mindfulness in psychosomatic and psychological research. Journal of Psychosomatic Research. 2008;64:405–408. doi: 10.1016/j.jpsychores.2008.02.001. [DOI] [PubMed] [Google Scholar]
- Grossman P. Defining mindfulness by how poorly I think I pay attention during everyday awareness and other intractable problems for psychology’s (re) invention of mindfulness: Comment on Brown et al. (2011) Psychological Assessment. 2011;23:1034–1040. doi: 10.1037/a0022713. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Grossman P, Hinton DE. Loving-kindness and compassion meditation: Potential for psychological interventions. Clinical Psychology Review. 2011;31:1126–1132. doi: 10.1016/j.cpr.2011.07.003. 10.1016.jcpr.2011.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78:169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How Does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science. 2011;6:537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- Ingram RE. Self-focused attention in clinical disorders: Review and a conceptual model. Psychological Bulletin. 1990;107:156–176. doi: 10.1037/0033-2909.107.2.156. [DOI] [PubMed] [Google Scholar]
- Jain S, Shapiro SL, Swanick S, Roesch SC, Mills PJ, Bell I, Schwartz GER. A randomized controlled trial of mindfulness medication versus relaxation training: Effects on distress, positive states of mind, rumination, and distraction. Annals of Behavioral Medicine. 2007;33(1):11–21. doi: 10.1207/s15324796abm3301_2. [DOI] [PubMed] [Google Scholar]
- Jiminez SS, Niles BL, Park CL. A mindfulness model of affect regulation and depressive symptoms: Positive emotions, mood regulation expectancies, and self-acceptance as regulatory mechanisms. Personality and Individual Differences. 2010;49:645–650. doi: 10.1016/j.paid.2010.05.041. [DOI] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your mind to face stress, pain, and illness. New York: Dell Publishing; 1990. [Google Scholar]
- Kabat-Zinn J, Massion AO, Kristeller J, Peterson LG, Fletcher K, Pbert L, Santorelli SF. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. American Journal of Psychiatry. 1992;149(7):936–943. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- Karelka M, Forsyth JP, Kelly MM. Emotional avoidance and panicogenic responding to a biological challenge procedure. Behavior Therapy. 2004;35(4):725–746. [Google Scholar]
- Keng S, Smoski MJ, Robins CJ. Effects of mindfulness on psychological health: A review of empirical studies. Clinical Psychology Review. 2011;31:1041–1056. doi: 10.1016/j.cpr.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohls N, Sauer S, Walach H. Facets of mindfulness-Results of an online study investigating the Freiburg mindfulness inventory. Personality and Individual Differences. 2009;46:224–230. doi: 10.1016/j.paid.2008.10.009. [DOI] [Google Scholar]
- Kuyken W, Watkins E, Holden E, White K, Taylor RS, Byford S, Dalgleish T. How does mindfulness-based cognitive therapy work? Behaviour Research and Therapy. 2010;48:1105–1112. doi: 10.1016/j.brat.2010.02.003. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Skills training manual for treating borderline personality disorder. New York: Guilford; 1993. [Google Scholar]
- Marlatt GA. Addiction, mindfulness, and acceptance. In: Hayes SC, Jacobson NS, Follette VM, Dougher MJ, editors. Acceptance and change: Content and context in psychotherapy. Reno, NV: Context; 1994. pp. 175–197. [Google Scholar]
- Mor N, Winquist J. Self-focused attention and negative affect: A meta-analysis. Psychological Bulletin. 2002;128:638–662. doi: 10.1037/0033-2909.128.4.638. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspectives on Psychological Science. 2008;3(5):1745–6924. doi: 10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: J. Wiley & Sons; 1987. [Google Scholar]
- Salzberg S. Loving-kindness. Boston, MA: Shambhala; 1995. [Google Scholar]
- Segal ZV, Kennedy S, Gemar M, Hood K, Pedersen R, Buis T. Cognitive reactivity to sad mood provocation and the prediction of depressive relapse. Archives of General Psychiatry. 2006;63:749–755. doi: 10.1001/archpsyc.63.7.749. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York, NY: Guilford Press; 2002. [Google Scholar]
- Spira AP, Zvolensky MJ, Eifert GH, Feldner MT. Avoidance-oriented coping as a predictor of panic-related distress: A test using biological challenge. Anxiety Disorders. 2004;18:309–323. doi: 10.1016/S0887-6185(02)00249-9. [DOI] [PubMed] [Google Scholar]
- Stasiewicz PR, Bradizza CM, Gudleski GD, Coffey SF, Schlauch RC, Bailey ST, Bole CW, Gulliver SB. The relationship of alexithymia to emotional dysregulatoin within an alcohol dependent treatment sample. Addictive Behaviors. 2012;37:469–476. doi: 10.1016/j.addbeh.2011.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stober J, Borkovec TD. Reduced concreteness of worry in generalized anxiety disorder: Findings from a therapy study. Cognitive Therapy and Research. 2002;26:89–96. [Google Scholar]
- Teasdale JD. Metacognition, mindfulness, and the modification of mood disorders. Clinical Psychology and Psycho-therapy. 1999;6:146–155. [Google Scholar]
- Teasdale JD, Segal ZV, Williams MG. How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness training) help? Behaviour Research and Therapy. 1995;33:25–39. doi: 10.1016/0005-7967(94)e0011-7. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Williams JM, Soulsby JM, Segal ZV, Ridgeway VA, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology. 2000;68:615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- Vanden Bogaerde A, Derom E, De Raedt R. Increased interoceptive awareness in fear of flying: Sensitivity to suffocation signals. Behaviour Research and Therapy. 2011;49:427–432. doi: 10.1016/j.brat.2011.03.011. [DOI] [PubMed] [Google Scholar]
- Watkins E. Depressive rumination: Investigating mechanisms to improve cognitive behavioural treatments. Cognitive Behaviour Therapy. 2009;1:8–14. doi: 10.1080/16506070902980695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D. Differentiating the mood and anxiety disorders: A quadripartite model. Annual Review of Clinical Psychology. 2009;5:221–247. doi: 10.1146/annurev.clinpsy.032408.153510. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. The Mood and Anxiety Symptom Questionnaire. University of Iowa; Iowa City, IA: 1991. [Google Scholar]
- Wren AA, Somers T, Wright MA, Goetz MC, Leary MR, Fras AM, Huh BK, Rogers LL, Keefe FJ. Self-compassion in patients with persistent musculoskeletal pain: Relationship of self-compassion to adjustment to persistent pain. Journal of Pain Symptom Management. 2012;43:759–770. doi: 10.1016/j.jpainsymman.2011.04.014. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Solomon SE, McLeish AC, Cassidy D, Bernstein A, Bowman CJ, Yartz AR. Incremental validity of mindfulness-based attention in relation to concurrent prediction of anxiety and depressive symptomatology and perceptions of health. Cognitive Behaviour Therapy. 2006;35:148–158. doi: 10.1080/16506070600674087. [DOI] [PubMed] [Google Scholar]