Abstract
Spinal cord injury (SCI) is associated with worst outcomes and requires a prolonged rehabilitation. Ayurvedic indigenous methods of rehabilitation are often utilized to treat such conditions. A case of SCI was followed up for 3 months upon an Ayurvedic composite intervention and subsequently reported. The composite treatment plan involved Ayurvedic oral medications as well as a few selected external and internal pancha karma procedures. A substantial clinical and patient centered outcome improvement in existing neurological deficits and quality of life was observed after 3 months of the Ayurvedic treatment given to this case.
Keywords: Practice-based evidence, patient centered outcome, quadriplegia, rehabilitation, spinal cord injury
INTRODUCTION
Traumatic spinal cord injury (SCI) causes severe devastations involving multiple domains affecting a healthy life. Besides ambulatory and occupational deficits as per the injury level and intensity, it also leads to sensory and autonomic deficits affecting the bladder and bowel regulation. As prolonged survival is the rule in most SCI, rehabilitation has been increasingly recognized as an important measure in overall management of such conditions. The primary goal of rehabilitation here is prevention of secondary complications, restoration of physical functioning to the maximum, and adopting appropriate measures to utilize the existing functions to make the activities of daily living (ADL) less dependent. Rehabilitation after SCI usually requires a multidisciplinary approach involving a physician, a physiotherapist, an occupational therapist, a psychiatrist, a social worker, and nursing personnel specialized in SCI care.[1,2] Seeing the limitations of current rehabilitative measures in improving the net outcomes in SCI, a practice-based evidence (PBE) research has been stressed to underscore the practical measures employed in various settings, which are found associated with improved net outcomes. Spinal cord injury rehabilitation (SCIRehab) project and spinal cord Injury rehabilitation evidence (SCIRE) are examples of how a PBE research can successfully be employed to identify the rehabilitation interventions most strongly associated with positive outcomes.[3,4]
Ayurvedic hospitals and particularly the pancha karma units therein are found utilizing some indigenous rehabilitative techniques to intervene in various neurological, muscular, and locomotory deficits. Common conditions where such interventions recommended are neurological deficits caused by cerebrovascular accidents, cerebral atrophy, prolapsed intervertebral disc, and SCIs. The rehabilitative techniques adopted in such conditions are composed of various classical heat and oil treatments done externally, oil and herbal decoction treatments done internally in addition to oral therapies. Neurological, rheumatological, and degenerative joint disease together form a substantial sum of total patients visiting an Ayurvedic hospital in India.[5] An overall satisfaction among patients receiving such therapies has been observed in earlier studies.[6] Some pilot studies, case reports, and case series have also reported the benefits of individual procedures or oral medications as interventions in such conditions. Upon Pub Med search, nevertheless, we did not come across any report where Ayurvedic intervention has been tried in a patient of SCI. Here we report a patient of SCI where an Ayurvedic comprehensive management composed of a few rehabilitative procedures and oral Ayurvedic medications has resulted in improvements identifiable through a SCI outcome measure like modified Barthel index (MBI).[7] The observations noted on various outcome measures related to SCI have further been verified through clinical examination and were endorsed during patient and care giver's interviews.
We presume that the observations as are reported in this case, upon their further substantiation may prove crucial as a PBE substantiating to the management of SCI. Such PBE research may also come as a vital thrust to the efforts made toward scientific substantiation and evidence-based reasoning aiming at effective and dependable clinical practice of Ayurveda. Equally important, in contrast, this method of PBE generation would also be able to mainstream many such interventions from traditional medicine, which remained unnoticed despite of their empirical ability of generating improvements through patient-based outcome observation.
CASE REPORT
A 52-year-old previously healthy male suffered from a fall from stairs (about 10 feet height) (November 30, 2011 evening). He remained unconscious for about 1.5 hours following the fall and regained consciousness subsequently. After getting awake he reported severe giddiness while raising the head and inability to move the upper and lower limbs. He was attended by a family physician next morning and was prescribed a few symptomatic medicine (prescription not available). On December 05, 2011 a noncontrast computed tomography (CT) scan of head was performed, which revealed no significant finding. Failing to get any response from the treatment, the patient was consulted with a neurosurgeon (December 22, 2011). Upon a detailed clinical neurological examination done this time, he was noted for a quadriparesis with upper motor neuron (UMN) involvement more on the right side comparing to the left side. He was advised a hard collar, bowel and bladder, and back care along with supportive therapy as may be recommended in the case from the point of view of conventional medicine. Magnetic resonance imaging (MRI) cervical spine was advised this time and revealed (January 02, 2012) straightening of cervical spine with desiccated intervertebral discs along with a fracture at C4 vertebral body. An intramedullary T2 hyper intensity was seen at C4 level, which was suggestive of cord contusion. A disc bulge was observed at C3-4 level producing mild extradural compression over ventral aspect of thecal sack with mild compromise of bilateral lateral races.
The conventional therapy continued for about 3 months following the injury, however, remained unrewarding. Observing this, he was further consulted with another neurosurgeon and continued with subsequently recommended therapy for another month. Failing to get any response he stopped taking the medicine. For next 3 months, the patient remained away from any direct medical supervision.
Ayurvedic intervention
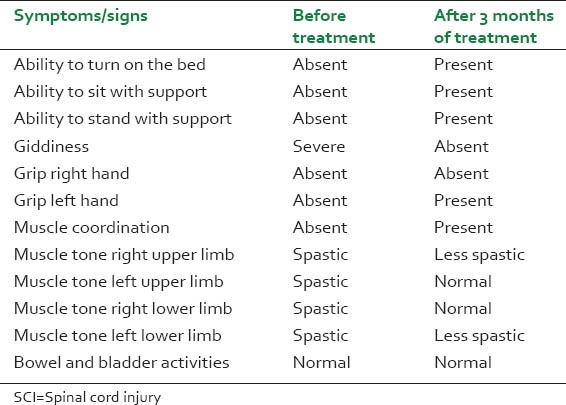
On September 07, 2012 the patient was consulted by an Ayurvedic physician (SR) at State Ayurvedic College, Lucknow. Upon this examination, it was revealed that he was unable to move either of the upper or lower limbs and severe giddiness upon lifting the head. He was fully conscious and awake except that he was not able to move any part of his body. His spine was stiff and so he was unable to turn on the bed or to sit even with support. There was no autonomic dysfunction and the patient was able to feel the urge for micturition and defecation. There was no added sensory loss anywhere in the body [Table 1]. A MBI was found to be 4 this time.
Table 1.
Neurological finding in a case of SCI before and after the ayurvedic therapy
Seeing the consistent request of the patient for Ayurvedic intervention in his case and considering his poor socio-economic status rendering him unable to opt for any other conventional therapy, which might have been offered in his case, the patient was taken up for Ayurvedic therapy. As there were no previous records of treating such patients of SCI with Ayurvedic management, the patient and the relatives were explained about the experimental nature of the therapy and the eventual uncertainty of the outcomes.
Considering the spastic condition of the whole body including spine and considering trauma to the cervical spine and subsequent features pathognomonic to vata nanatmaja disease, the patient was recommended for a set of Ayurvedic therapies comprising of Pinda Sweda (PS), Greeva Vasti (GV) with mahanarayana oil and Sarvanga Sweda (SS). In addition to these local therapies, the patient was also recommended a few oral Ayurvedic drugs aiming at the control of vata in such clinical conditions [Table 2]. The whole treatment package was provided to the patient in the indoor setting of State Ayurvedic College Hospital, Lucknow. The patient was kept under continuous observation and was followed up on periodic basis. After one month of the therapy, little improvement was observed in neurological deficits. Most remarkably the patient was able to raise his head without complaint of giddiness as was noticed prior to the Ayurvedic treatment. After one month of therapy, to maximize the therapeutic effects of the whole therapy the prescription was added with a periodic Kaala Vasti (KV) with mahanarayana oil for 16 days and Shiro Vasti (SV) with brahmi ghrita [Tables 2 and 3]. The same treatment continued for another 2 months and the patient was followed up after the completion of the therapy. Upon a subsequent follow-up after 3 months of Ayurvedic therapy, the patient was found to have substantial recovery to his neurological deficits. He was able to turn on the bed unaided, able to sit unaided for 15-20 minutes and was able to walk with major support. He was able to move all the joints of all the four limbs except the fine finger movements at right hand. He was able to grip from the left hand and was able to eat with this hand. By this time he was also able to stay out on wheel chair carried by some caregiver. A 10-item MBI score, which was reported to be 4 before the start of Ayurvedic intervention, was improved to 10 at the end of 3 month Ayurvedic therapy. The 10-item MBI is intended to establish the degree of independence of the patient from any help, however, minor and for whatever purpose. This is an index that records what the patient does rather than what the patient can do.
Table 2.
Ayurvedic treatment given to a case of spinal cord injury
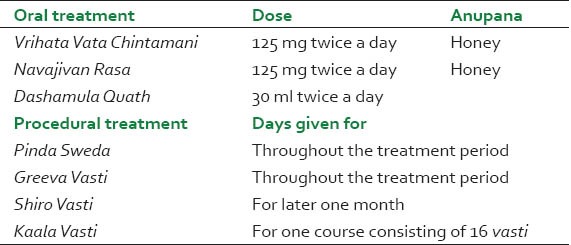
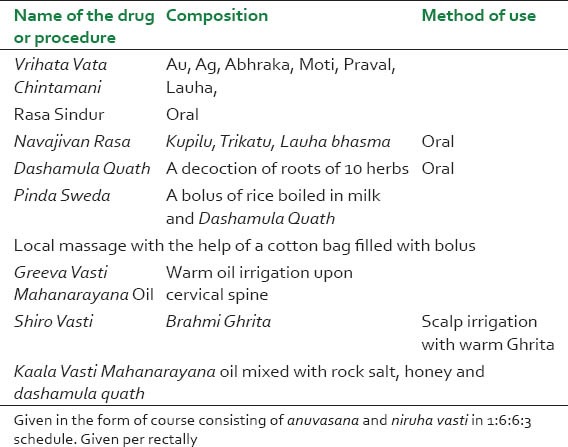
Table 3.
Composition of Ayurvedic therapy utilized for rehabilitation in a case of SCI
It is important to note here that a 20 score at MBI reflects the independence of patient in cases of SCI. An interview with patient and his care givers reflected their satisfaction with the outcome achieved in 3 months of therapy with an expectation to obtain more if the therapy is further continued.
Details of the ayurvedic procedures
Ayurvedic therapy was started with PS for 15 minutes done with the help of a rice bolus made up of rice boiled in milk and dashamula quath. A prior whole body massage with mahanarayana oil was done before PS. A subsequent GV was done with the help of lukewarm mahanarayana oil poured upon cervical spine within a confined area marked through a small well made up of mash flour. Subsequently, a sarvanga swedana for 5 minutes was done with dashamula quath.
In the following month KV was added to the treatment in a schedule of 16 vastis comprised of one anuvasana followed by six anuvasana and six niruha vasti and finally followed by three anuvasana vasti. Anuvasana vasti was given after meal and composed of saindhava salt 5 g, honey 10 g, mahanarayan oil 30 ml, and dashamula quath 30 ml. Niruha vasti was given empty stomach and was composed of saidhava salt 10 g, honey 10 g, mahanarayana oil 30 ml and dashmula quath 150 ml. The vasti components were mixed in order and given as mentioned in the classical texts of Ayurveda. This time the patient was also started with SV with brahmi ghrita to intensify the vata shamaka effects of the whole therapy. SV was done for 30 minutes every day. No other specific therapy either biomedical or physiotherapy was instituted during the trial period.
DISCUSSION
SCI have been one among the most devastating trauma man can suffer. The worst victims of SCI are those suffering with quadriplegia associated with autonomic dysfunction. As long-term survival is the rule in most cases of SCI and as the victims of SCI are prominently the young people in their most productive age, the personal and social impacts of such trauma are extremely deleterious. Immediate surgical decompression is often been recommended as the first measure to minimize the neurological damage caused by vertebral fractures and the results are not found very satisfactory if this decompression is delayed. A substantially high cost of surgical approach in SCI nevertheless is a major limitation in frequent utilization of this option in every SCI case. Absence of definitive conservative therapy to intervene and high cost associated with surgical approaches makes rehabilitative approach crucial for SCI sufferers in making them less dependent and improving their performance level of primary ADL. Any neurological improvement following the immediate or delayed conservative intervention after the spinal cord trauma is also something which is being desperately looked in such conditions. Ayurvedic treatment as an advent of orient with its global outreach offers substantial help to deal with such situations through its own indigenous treatment models. Various oil and ghrita therapies of Ayurveda have been able to give substantial improvement in many intractable neurological conditions as are reported in various single case reports and series published from time to time.[8,9] This case of SCI presented with severe neurological deficits and a MBI score of 4 has demonstrated the clinical and patient centered outcome improvements after 3 months of a comprehensive Ayurvedic therapy. MBI scoring is used as a dependable index to know about the qualitative improvements in SCI patient's life by observing the level of independence achieved after the therapy. A 10 item MBI has a range of scores 0-20 where 0 denotes a complete dependence and 20 denotes a complete independence. Any shift in the net score favoring toward the higher scores is indicative of decreasing dependence and increasing independence as it was observed in this case. Although the treatment was not able to bring a complete independence of functions in the case it certainly had reduced the level of dependence as was observable with the improved MBI score. This case offers two important bearings to current medical practice pertaining to SCI. First it offers a novel approach of managing the neurological deficits of patients suffering with SCI once it is stabilized. Either alone or in conjunction with conventional rehabilitative measures, this approach upon its further substantiation, holds a promise of adding benefits into the currently utilized protocol of SCI management. Second and equally important bearing of this case report is to express the utility of Ayurveda as a composite intervention for the purpose of clinical practice and research. The case presented here has been treated with a comprehensive and composite management plan as per the convenience of Ayurveda. As the treatment was able to make improvements in existing conditions, this approach should be taken into consideration while making any further trial to treat similar or new conditions with the help of Ayurveda.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Sadowsky CL, McDonald JW. Activity-based restorative therapies: Concepts and applications in spinal cord injury-related neurorehabilitation. Dev Disabil Res Rev. 2009;15:112–6. doi: 10.1002/ddrr.61. [DOI] [PubMed] [Google Scholar]
- 2.van Langeveld SA, Post MW, van Asbeck FW, Ter Horst P, Leenders J, Postma K, et al. Reliability of a new classification system for mobility and self-care in spinal cord injury rehabilitation: The Spinal Cord Injury-Interventions Classification System. Arch Phys Med Rehabil. 2009;90:1229–36. doi: 10.1016/j.apmr.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 3. [Last accessed on 2013 Apr 10]. Available from: http://www.scireproject.com/about-scire .
- 4.Whiteneck G, Dijkers M, Gassaway J, Lammertse DP. The SCIRehab Project: Classification and quantification of spinal cord injury rehabilitation treatments. J Spinal Cord Med. 2009;32:249–50. [PMC free article] [PubMed] [Google Scholar]
- 5.Rastogi S, Singh RH. Identifying the stress area for future research in Ayurveda-A demographic study. New Approaches Med Health. 1999;6:20–8. [Google Scholar]
- 6.Rastogi S. Effectiveness, safety and standard of service delivery: A patient based survey at a Pancha Karma therapy unit in a secondary care Ayurvedic hospital. J Ayurveda Integr Med. 2011;2:197–204. doi: 10.4103/0975-9476.90767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McDowell I, Newell C. 2nd ed. Oxford: Oxford University Press; 1996. Measuring health-a guide to rating scales and questionnaires; pp. 56–63. [Google Scholar]
- 8.Rastogi S, Chawla S, Singh RK. Ayurvedic management of unilateral loss of vision following a blunt injury to eye: A case report. Complementary Health Pract Rev. 2009;14:84–92. [Google Scholar]
- 9.Rastogi S. Management of tension-type headache with Ayurveda: A case series. Altern Complementary Ther. 2009;15:113–8. [Google Scholar]


