Abstract
Background: Seriously ill hospitalized patients and their loved ones are frequently faced with complex treatment decisions laden with expressions of emotional distress during palliative care (PC) consultations. Little is known about these emotional expressions or the compassionate responses providers make and how common these are in PC decision-making conversations.
Objectives: To describe the types and frequency of emotional distress that patients and loved ones express and how providers respond to these emotions during PC decision-making consultations with seriously ill hospitalized patients.
Methods: We used a quantitative descriptive approach to analyze 71 audio-recorded inpatient PC decision-making consultations for emotional distress and clinicians' responses to those emotions using reliable and established methods.
Results: A total of 69% of conversations contained at least one expression of emotional distress. The per-conversation frequency of expressions of emotional distress ranged from 1 to 10. Anxiety/fear were the most frequently encountered emotions (48.4%) followed by sadness (35.5%) and anger/frustration (16.1%). More than half of the emotions related to the patient's feelings (53.6%) and 41.9% were related to the loved ones' own emotions. The majority of emotions were moderate in intensity (65.8%) followed by strong (20.7%) and mild (13.5%). Clinicians responded to a majority of emotions with a compassionate response (75.7%) followed by those with medical content (21.9%) and very few were ignored (1.3%).
Conclusions: Expressions of emotional distress are common during PC consultations and are usually met with compassionate responses by the clinician.
Introduction
Treatment decision making in serious illness can be profoundly difficult for patients and families.1 Patients and loved ones often find relief when discussing their concerns and worries with their medical team.2,3 When clinicians respond to a patient's distressing emotions with compassion,4–9 patients are more satisfied with care and more willing to further disclose their feelings.1,10,11 Despite this, seriously ill patients and families often experience clinical encounters where their distressing emotions are not addressed.
Palliative care (PC) is emerging rapidly in the United States,12 and PC consultation leads to improved satisfaction with care and quality of life among seriously ill patients.13 Responding to distressing emotion is fundamental to PC education, yet little is known about expression and response to distressing emotions in the setting of PC consultation. Therefore, the aim of this study was to examine the frequency and types of a) expressions of emotional distress and b) responses to those emotions that occur during PC decision-making consultations.
Methods
Setting
This observational study was conducted at a 750-bed academic medical center in the northeastern United States, with a mature inpatient PC consultation service completing more than 1,000 consultations annually. Details are reported elsewhere.14
Participants
The PC team comprises attending physicians, nurse-practitioners (NPs), PC fellows, 2-week trainees (residents and fourth-year medical students), a clinical ethicist, a clinical social worker, chaplains, a massage therapist, and a music therapist. Two consultation teams, each with three to five members (always an attending physician and usually an NP, resident, and fellow), are available at any given time. All patient participants were English-speaking, were at least 21 years of age (or surrogates were if a patient's decisional capacity was impaired), and were referred for “goals-of-care” or “end-of-life decision making.”
Data sources
With prior informed consent from all study participants, we placed digital recorders in unobtrusive locations in the hospital rooms. After the visit, we extracted data from a two-page PC consultation form for: patient age, gender, primary diagnoses, referral reason, Palliative Performance Scale (PPS) and Edmonton Symptom Assessment System scores. For nine participants, the PPS was not completed; however, the medical record provided sufficient information to accurately categorize their PPS scores. From the medical record and hospital administrative data, we collected reported race, insurance type, hospital admit date, consultation date, and any advance directives.
Coding
Audio recordings were analyzed by two trained coders (SL and MM). Training consisted of 30 hours over a 2-week period of time. Twenty percent of the conversations were double-coded for reliability. Disagreements were discussed and final decisions made by consensus. Coders demonstrated strong agreement for Emotional Distress (Cohen's Kappa=0.78; 95% confidence interval [CI] 0.57–0.98) and Clinician Responses (Kappa=0.84; 95% CI 0.72–0.97).15 Emotional Distress was further coded into subcategories: directness, type of emotion, and intensity of emotion. Intensity was a magnitude subcode that had a threshold criteria (from least to highest). The lowest threshold (mild) was any emotion expressed that hints at, or makes passing reference to a distressing emotion. This might include references to a recurrent distressing emotion without clarifying its presence at the moment (e.g., “At home, his anxiety is as such that if he is not feeling well, he gets agitated.”). The middle threshold (moderate) was current emotional expressions where the person maintained composure (i.e., “Again, I am riddled with guilt because the kids are not here to help make the decision. I am scared to do this.”). The highest threshold (strong) consisted of emotional expressions where persons are experiencing a profound or deeply felt emotion and are unable to compose themselves (e.g. [yelling], “What the hell difference does it make if they were mean to her or not? They treated her like shit!”; a loved one crying and saying, “I am not ready. Dad? Dad? Is this what you want? Oh, God!”).
Analytic approach
Our primary analyses define the frequency and distribution of all Emotional Distress and Clinician Responses. Because conversations differed in duration, we standardized the quantity of Emotional Distress segments by calculating rates (i.e., segment counts per hour). We then stratified Emotional Distress and Clinician Responses on key demographic and clinical factors. For stratification variables with many potential thresholds (e.g., PPS), we created trichotomous categories based on the observed distributions to explore potential dose-response relationships. Based on observed distributions, we used nonparametric statistical tests (Wilcoxon rank-sum) for rates of expressions of emotional distress and clinician responses and parametric tests (Student's t test, analysis of variance [ANOVA]) for mean differences.
Human subjects
All clinician and patient participants (or their surrogates) completed written informed consent, and the University of Rochester Research Subjects Review Board approved this study.
Results
During the 4-month enrollment period, 11 attending physicians, 2 NPs, and 2 PC fellows actively participated in at least one observed consultation. Among the 15 PC clinicians (attending MDs, NPs, fellows), 6 were women, 12 were board certified in PC, 7 had >5 years of PC experience, and 11 had been in clinical practice for >10 years at the time of enrollment.
Three hundred and six patients were referred for PC consultations to address “goals of care” or “end-of-life decision making.” We approached 100 patients (78 consented to participate). Among consented participants, we missed three consultations because they occurred either at night or simultaneously with another participant's consultation. Four recorded consultations did not contain sufficient conversation for analyses. Thus, the final sample includes 71 conversations.
The demographics of the patient participants and the composition of the PC team for each consultation are described in Table 1. Approximately one-half of the consultations were with female patients and approximately one-third involved patients younger than 60 years of age. Approximately one-half of the participants were referred because of complications related to cancer. The remaining were referred due to heart failure, chronic obstructive pulmonary disease (COPD), or stroke. Forty-one percent of patient-participants were experiencing severe symptoms of pain, nausea, dyspnea, anxiety, or depression, and 41% were bedbound.
Table 1.
Sample Description
| Study sample (n=71) | Historical samplea (n=2043) | ||
|---|---|---|---|
| N | % | % | |
| Patient/Family Participants | |||
| Age | |||
| <60 years | 23 | 32 | 36 |
| 60 to <80 years | 26 | 37 | 39 |
| ≥80 years | 22 | 31 | 25 |
| Gender | |||
| Women | 33 | 46 | 47 |
| Men | 38 | 54 | 53 |
| Reported race | |||
| Black | 5 | 7 | 14 |
| White | 66 | 93 | 79 |
| Main diagnosis | |||
| Cancer | 35 | 49 | 46 |
| CHF/COPD | 9 | 13 | 17 |
| CVA | 7 | 10 | 6 |
| Other | 20 | 28 | 30 |
| Patient/Family Verbal Participation | |||
| Patient only | 18 | 25 | Unavailable |
| Patient and family | 24 | 34 | |
| Family only | 29 | 41 | |
| Severe symptoms? | |||
| Yes | 29 | 41 | 37 |
| No | 42 | 59 | 63 |
| Palliative Performance Score | |||
| ≤30 | 30 | 42 | 46 |
| 40–50 | 23 | 32 | 31 |
| ≥60 | 18 | 26 | 23 |
| Composition of PC team | |||
| Participating membersb | |||
| Attending physician only | 30 | 42 | Unavailable |
| Attending physician+NP/fellow | 25 | 35 | |
| Attending physician, NP+fellow | 16 | 23 | |
“Goals of care” or “end-of-life decision-making” consultations (January 2006 to January 2010), no statistically significant differences in comparisons to study sample characteristics.
Internal medical residents and medical students trainees were present for many conversations but did not contribute substantively.
CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; CVA, other; NP, nurse practioner; PC, palliative care.
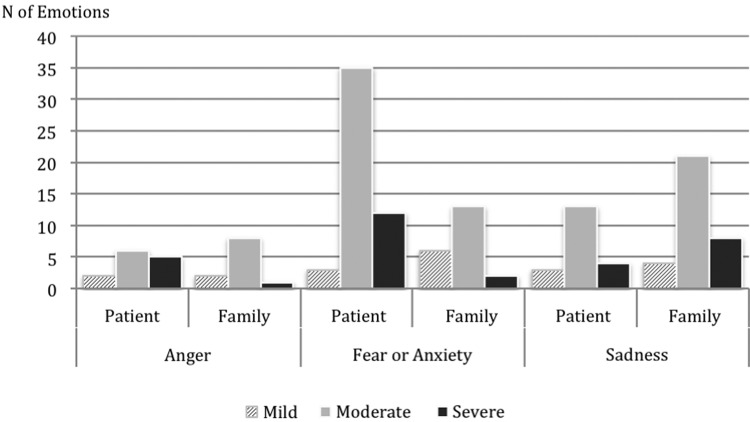
Emotional distress was equally expressed directly (49.7%) and indirectly (50.3%), but this varied by the type (majority of sadness was expressed indirectly, whereas the majority of fear was directly expressed). A total of 69% (49/71) of conversations contained at least one expression of emotional distress (averaging between 1 and 10 emotions per conversation). Anxiety was the most frequent emotion (48.4%), then sadness (35.5%), and anger/frustration (16.1%) (Fig. 1). Expressions split evenly between patient's feelings (53.6%), and loved ones' emotions. The majority were moderate in intensity (65.8%), then strong (20.7%), and mild (13.5%).
FIG. 1.
Patients' and loved ones' expressions of emotional distress: anger, fear/anxiety, and sadness.
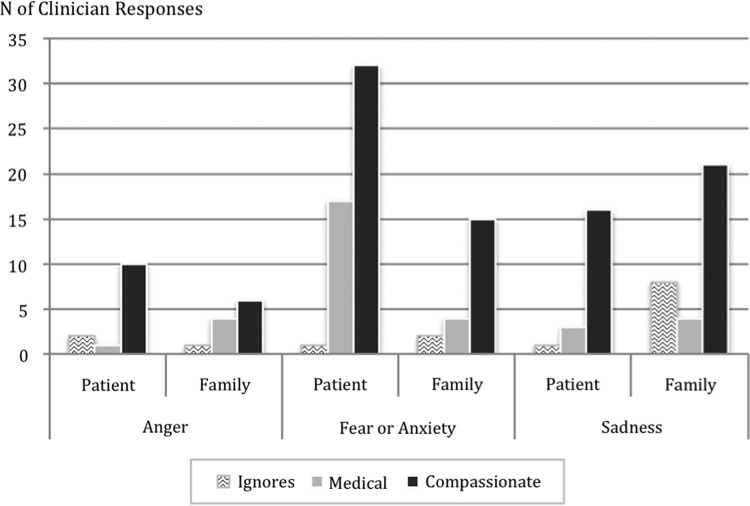
The majority of emotional expressions received a compassionate response (75.7%), followed by medical content (21.9%) and very few were ignored (1.3%) (Fig. 2). Compassionate responses to family members were mostly about fear/anxiety, whereas compassionate responses to patients were mostly about sadness/grief (see Table 2 for examples of compassionate responses).
FIG. 2.
Clinician responses to expressions of emotional distress.
Table 2.
Examples of Compassion
| Clinician: One of my jobs here, while we are getting the chance to know each other, however long that time is, is to help make sure all of your energies and all your fight is going in the direction you want them to go in. As your doctor, I am here for you. From what you told me, I know your struggle has been hard and I want to help in whatever way I can for you. |
| Loved One: But, there is going to be a day when she says, “It's enough,” but, we will wait (starts crying). |
| Clinician: We will walk along with you for however long that is—and along the way, our job is that we are attentive to your comfort as well as hers. |
| Clinician: I wish I could tell you there was more that we could do. But, he's still very much here and we are very much here to do as much as we can to make sure he stays as peaceful and comfortable as possible. |
| Loved One: OK. |
| Clinician: We are also here for you all—sometimes that might mean answering questions—this is not something people go through every day—we understand if you don't know what to expect. But, we are here to try and help out. Anytime you have a question, I want you to ask me. |
| Clinician: Anxiety or depression ever been a problem for you in the past? |
| Patient: Yeah, yeah, yeah. |
| Clinician: How's it now? |
| Patient: It is better; I mean earlier I was crying. |
| Clinician: You have a lot on your plate. |
| Patient: Yeah (crying). |
| Clinician: Other things that you've found helpful for that? |
| Patient: (sobs) Huh? |
| Clinician: Other things that you have found help for some of the sadness or some of the nerves? |
| Patient: (crying still) No. I just thought I was getting better. |
| Clinician: What are some of the things you are hoping to do? |
| Patient: Get the pain under control so I could go shopping and stuff. |
| Clinician: OK. |
| Patient: I want to see my son—I don't want my son to see my on the couch all the time. He's got anxiety, he's got disabilities, he's got behavioral problems. |
| Clinician: So, getting the pain better so you can move around a bit and appear more comfortable for your son is one thing to hope for. |
| Patient: Yeah. |
Discussion
We report three important findings. First, patients and loved ones expressed emotional distress frequently during PC consultations. Second, fear/anxiety were the predominant emotions expressed. Third, clinicians tended to respond to distressing emotions with compassionate language.
Emotions were quite common in our sample, with more than two-thirds of the conversations containing at least one expression of emotional distress. The frequency of distress was significantly higher compared with other studies on emotions in oncology and end-of-life care.2,7,8,16,17 One possible reason for the higher frequency is that the spiritual, existential, and relationship issues facing many patients and loved ones become even more salient to patients as their illness progresses and they approach the end of life.
The predominant expressions of emotional distress were fear/anxiety. This is not surprising given the nature of a patient's illness when PC becomes important. Anger was frequently expressed, with more than 16% of the conversations containing at least one overt expression of anger, with the intensity of patients' anger being more severe than family members' anger. In previous research, anger has been reported at a much lower level in oncology and end of life.17,18 In PC settings, patients and families often express anger,19,20 whether directed at the disease, at the limits of current medical science, at previous unsettling experiences with medical care, or other sources. Expressing anger can open space for therapeutic relationships and productive goal-setting conversations.
Clinician expressions of compassion in response to distressing emotions were very common in our study, and seemingly more common than other clinical encounters with seriously ill patients in oncology.2,8,16,17,21,22 This study was not designed to compare communication practices across different clinical settings, so the reasons for our comparatively high rates of compassionate responses remain unknown. However, our findings highlight the need to understand how best to sustain the level of presence and compassion in the practice of PC.
There are several limitations to our study. These observations reflect PC practice in one large medical center with a mature PC program and institutional expertise in patient-centered communication.23,24 Restricting the scope to “expert” communicators in established clinical contexts can be of great value as a starting place and catalyst for the subsequent research required to ultimately define “best practices.” The variability in our sample highlights the need to understand how PC practices vary more broadly across the micro and macro cultures represented by institutional, geographic, clinical, and demographic contexts.
The results of this study are encouraging for PC—compassion is at the forefront of clinicians' responses to patients' and loved ones' negative emotions. In our study, providers did not shy away from attending to patients' and loved ones' emotions. On the contrary, we demonstrate that PC providers are very attuned and responsive to spontaneous emotional expression from their patients and families, even when the elicited emotions are challenging and demanding or even uncomfortable to discuss.
Acknowledgments
This work was funded in part by research grants from the National Palliative Care Research Center and the Greenwall Foundation. Dr. Robert Gramling is funded by a Career Development Award from the National Palliative Care Research Center. No authors have financial or other conflicts to report. We thank the University of Rochester Medical Center Inpatient Palliative Care team, patients, and families for their enthusiasm and dedication to conducting research that will enhance care for people with serious illness.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Heaven CM, Maguire P: Disclosure of concerns by hospice patients and their identification by nurses. Palliat Med 1997;11:283–290 [DOI] [PubMed] [Google Scholar]
- 2.Pollak KI, Arnold RM, Jeffreys AS, et al. : Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol 2007;25:5748–5752 [DOI] [PubMed] [Google Scholar]
- 3.Baile WF, Palmer JL, Bruera E, Parker PA: Assessment of palliative care cancer patients' most important concerns. Support Care Cancer 2011;19:475–481 [DOI] [PubMed] [Google Scholar]
- 4.Baile WF, Walters R: Applying sociodramatic methods in teaching transition to palliative care. J Pain Symptom Manage 2013;45:606–619 [DOI] [PubMed] [Google Scholar]
- 5.Betcher DK: Elephant in the room project: Improving caring efficacy through effective and compassionate communication with palliative care patients. Medsurg Nurs 2010;19:101–105 [PubMed] [Google Scholar]
- 6.Back AL, Arnold RM, Baile WF, et al. : Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med 2007;167:453–460 [DOI] [PubMed] [Google Scholar]
- 7.Alexander SC, Keitz SA, Sloane R, Tulsky JA: A controlled trial of a short course to improve residents' communication with patients at the end of life. Acad Med 2006;81:1008–1012 [DOI] [PubMed] [Google Scholar]
- 8.Tulsky JA, Arnold RM, Alexander SC, Olsen MK, Jeffreys AS, Rodriguez KL, Skinner CS, Farrell D, Abernethy AP, Pollak KI: Enhancing communication between oncologists and patients with a computer-based training program: A randomized trial. Ann Intern Med 2011;155:593–601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baile WF, De Panfilis L, Tanzi S, Moroni M, Walters R, Biasco G: Using sociodrama and psychodrama to teach communication in end-of-life care. J Palliat Med 2012;15:1006–1010 [DOI] [PubMed] [Google Scholar]
- 10.Epstein RM: Making communication research matter: What do patients notice, what do patients want, and what do patients need? Patient Educ Couns 2006;60:272–278 [DOI] [PubMed] [Google Scholar]
- 11.Greisinger AJ, Lorimor RJ, Aday LA, Winn RJ, Baile WF: Terminally ill cancer patients. Their most important concerns. Cancer Pract 1997;5:147–154 [PubMed] [Google Scholar]
- 12.Morrison RS, Augustin R, Souvanna P, Meier DE: America's care of serious illness: A state-by-state report card on access to palliative care in our nation's hospitals. J Palliat Med 2011;14:1094–1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.El-Jawahri A, Greer JA, Temel JS: Does palliative care improve outcomes for patients with incurable illness? A review of the evidence. J Support Oncol 2011;9:87–94 [DOI] [PubMed] [Google Scholar]
- 14.Gramling R, Norton SA, Ladwig S, et al. : Direct observation of prognosis communication in palliative care: A descriptive study. J Pain Symptom Manage 2013;45:202–212 [DOI] [PubMed] [Google Scholar]
- 15.Landis JR, Koch GG: The measurement of observer agreement for categorical data. Biometrics 1977;33:159–174 [PubMed] [Google Scholar]
- 16.Alexander SC, Pollak KI, Morgan PA, et al. : How do non-physician clinicians respond to advanced cancer patients' negative expressions of emotions? Support Care Cancer 2011;19:155–159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kennifer SL, Alexander SC, Pollak KI, et al. : Negative emotions in cancer care: do oncologists' responses depend on severity and type of emotion? Patient Educ Couns 2009;76:51–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anderson WG, Alexander SC, Rodriguez KL, et al. : “What concerns me is…” Expression of emotion by advanced cancer patients during outpatient visits. Support Care Cancer 2008;16:803–811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O'Grady E, Dempsey L, GFabby C: Anger: A common form of psychological distress among patients at the end of life. Int J Palliat Nurs 2012;18:592–596 [DOI] [PubMed] [Google Scholar]
- 20.Phillip J, Gold M, Schwarz M, Komesaroff P: Anger in palliative care: A clinical approach. Intern Med J 2007;37:49–55 [DOI] [PubMed] [Google Scholar]
- 21.Hsu I, Saha S, Korthuis PT, et al. : Providing support to patients in emotional encounters: A new perspective on missed empathic opportunities. Patient Educ Couns 2012;88:436–442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wittenberg-Lyles E, Debra PO, Demiris G, Rankin A, Shaunfield S, Kruse RL: Conveying empathy to hospice family caregivers: Team responses to caregiver empathic communication. Patient Educ Counsel 2012;89:31–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Epstein RM, Franks P, Fiscella K, et al. : Measuring patient-centered communication in patient-physician consultations: theoretical and practical issues. Soc Sci Med 2005;61:1516–1528 [DOI] [PubMed] [Google Scholar]
- 24.Epstein RM, Street RL: Patient-Centered Communication in Cancer Care. Bethesda, MD: National Institutes of Health, 2007 [Google Scholar]