Abstract
Objectives
To (1) evaluate educational needs of clinical students at Al-Quds University Medical School in the West Bank; (2) address these needs where possible using synchronous distance learning, with clinicians in Oxford providing case-based tutorials to undergraduates in the West Bank via an online platform (WizIQ) and (3) assess the impact of this education.
Design
Review of online OxPal Medlink database for tutorials held between March 2012 and April 2013. Needs assessment and evaluation of student and tutor experiences through online questionnaires, focus groups and semi-structured interviews.
Setting
Oxford University Hospitals, Oxford, UK, and Al-Quds University Medical School, Abu Dies, Palestine.
Participants
Doctors at Oxford University Hospitals and fourth-, fifth- and sixth-year medical students and faculty members at Al-Quds Medical School.
Main outcome measures
Number of tutorials, student participation, student-rated satisfaction and qualitative feedback from tutors and students.
Results
Students demonstrated strong theoretical knowledge but struggled to apply this in presentation-based scenarios. Between March 2012 and April 2013, 90 tutorials were delivered to 60 students. Feedback: >95% respondents rated tutorials as ‘Excellent’ or ‘Good’ and ‘Very’ or ‘Fairly’ relevant to their future practice in Palestine. Students reported the programme had modified their approach to patients but requested better synchronization with concurrent attachments and clarification of learning outcomes.
Conclusions
OxPal Medlink is a novel, web-based distance-learning partnership designed to overcome some of the challenges to local medical education in the occupied Palestinian territories. Evaluation of the first year indicates teaching is relevant to local practice and of high quality. This approach may have the potential to strengthen local capacity for medical education.
Keywords: distance learning, education, Internet, teaching
Introduction
Building sustainable and collaborative partnerships between health communities in different parts of the world remains a key component in the drive to improve global health. Paucity in generating and applying knowledge is a fundamental obstacle to achieving positive health outcomes.1 As a result, there have been repeated calls for initiatives to bridge educational and information gaps between developing and developed countries.2–4
The current geopolitical context of the occupied Palestinian territories presents unique challenges to healthcare and medical education, which were outlined in 2009 by The Lancet-Palestinian Health Alliance.5,6 The separation wall between Israel and the West Bank and the presence of numerous checkpoints prevents many students from accessing clinical learning environments; in a survey of 50 students from Al Quds Medical School (AQMS) conducted by OxPal in 2012, 37% of students stated that they experienced disruption whilst travelling to classes at least once per week on average. Furthermore, frequent economic sanctions and punitive retention of tax revenues by occupying authorities mean that private clinical practice is often prioritized over the teaching and education of medical students. Additionally, a lack of dedicated teaching hospitals and learning spaces in wards and other clinical settings has stunted the growth of a robust teaching culture in many Palestinian hospitals.
Thus far, international medical education initiatives have not utilized modern global communication resources to their full potential, despite the evolution of digital web-based technologies that can facilitate exchange capable of crossing physical and geographical barriers in real time and at low cost.
The OxPal Medlink was established in March 2012, building upon a 10-year history of collaboration and partnership between clinicians based in Oxford and students and faculty at AQMS in Jerusalem. The project draws inspiration from MedicineAfrica (www.medicineafrica.com), an online platform connecting healthcare professionals in the UK with their counterparts in several African countries including Somaliland, Ghana and Sierra Leone.7,8 Using virtual classroom-based technology (www.wiziq.com), doctors based in Oxford University Hospitals meet with AQMS students in the West Bank weekly to participate in real-time tutorials. Medical and surgical cases from the students’ own clinical experiences in Palestine act as the focus. Tutorials involve discussion of these cases in order to develop and refine skills in clinical reasoning and the formulation of diagnoses and management plans. The virtual classroom incorporates both audio- and text-based discussion, and an interactive white-board facilitates a multimedia learning environment requiring only low-bandwidth internet connectivity.
One year into the partnership, we seek to analyse the educational needs of clinical students at AQMS. Whilst students receive sufficient academic teaching, access to clinical learning environments, patient contact and small-group bedside teaching opportunities is restricted by the current financial and geopolitical situation. This may limit experience of the approach to diagnosis and patient management. We aim to address this deficit where possible, supplementing current AQMS teaching with case-based discussions focussing on diagnostic approach. With restrictions on travel and access to online medical journals, interaction with the international professional community is also limited. The partnership aims to connect students and junior clinicians with doctors in the UK and thereby foster educational exchange and mentorship.
We present here an evaluation of the programme to date and discuss possible future directions of the partnership. The online distance-learning model can be expanded to engage increasing numbers of clinicians in disparate geographical locations; it is low cost and has potential to be applied in other resource-limited settings. Starting from a small nucleus of participants, the current programme has already expanded considerably. As it continues to grow, OxPal aims to determine need on an ongoing basis and thereby evolve to become increasingly impactful and relevant to local deficits in clinical education.
Methods
A field visit to the West Bank in April 2013 was conducted to:
Perform a needs assessment of students’ abilities, both in terms of clinical skills and baseline theoretical knowledge. Tutors delivered, in total, 100 hours of student contact time in bedside clinical teaching within government hospitals, observed by OxPal’s evaluation team to ascertain the students’ areas of relative strength and weakness and to record feedback;
Evaluate the teaching programme. Focus groups and semi-structured interviews were held separately with fourth-, fifth- and sixth-year medical students who had been involved in the OxPal programme during the past year. All students who had participated (or been invited to participate) were invited by email or in person. Questions with desired evaluation outcomes were developed in advance and sought to explore students’ experiences of the programme, barriers to participation and difficulties encountered. This method of evaluation also provided students with the opportunity to voice additional comments and suggestions for the programme. Several interviews were recorded with consent for transcription and later analysis. Students who had not been involved in the project were interviewed in order to identify ways to improve future participation;
Build relationships with student participants and gain the support of the AQMS faculty, including the Dean and speciality leads in rheumatology, paediatrics, obstetrics and gynaecology and psychiatry. A meeting was hosted by the Palestinian Minister of Health to discuss the potential for building postgraduate links between Oxford-based specialists and Palestinian speciality trainees.
Format, content and logistics of programme delivery
Registrars based at Oxford University Hospitals and fourth-, fifth- and sixth-year students at AQMS were invited to the programme by email; those who responded to the initial correspondence were then sent a more detailed sign-up form. A series of pilot tutorials were held in March–April 2012, prior to launching of the programme. The aim of these was to (1) gauge initial interest in the project from both tutors in Oxford and students in the West Bank, (2) gain familiarity with the technical aspects of the online interface and ensure sufficient bandwidth for running of the programme and (3) refine practicalities, such as length of tutorials and days and times of the week which would be most convenient for both tutors and students.
All participating students were then divided into groups of four to six, each of which was assigned tutors for internal medicine and for general surgery. Tutorials alternated on a weekly basis between the two specialties; coordinators for the programme would liaise with tutors in Oxford and students in Palestine to schedule the online sessions at times of mutual convenience. Tutorials were run, recorded and stored online using the WizIQ online teaching platform (www.wiziq.com).
Tutorials were invariably case based, using cases provided by the students from their local hospitals. Cases were emailed to the OxPal programme coordinators in advance; these were edited and supplemented by the tutors and uploaded to the teaching platform in Powerpoint format. During tutorials, tutors used their own personal computers with microphone facilities activated; students interacted with the case via a text-based instant messaging panel, visible to all participants. The online teaching platform incorporates a smartboard with drawing capability, links to YouTube videos and a poll to quiz students’ knowledge. Tutors can designate microphone and/or drawing control to individual or selected groups of students, enabling them to respond verbally to questions or to annotate the case on the interactive whiteboard.
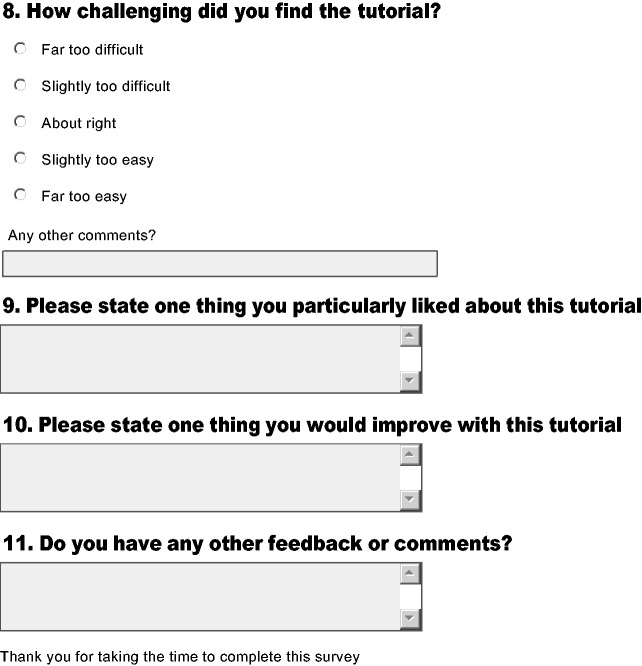
Evaluation and feedback questionnaires
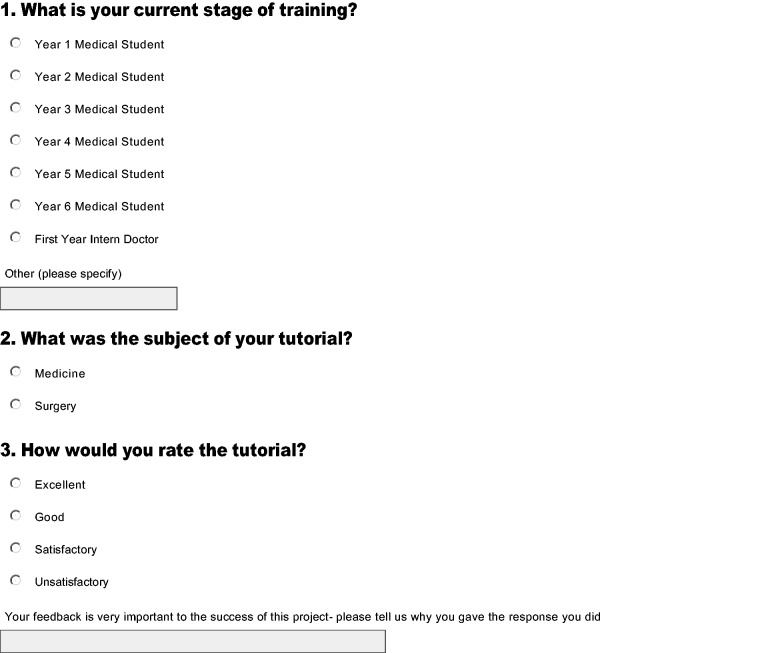
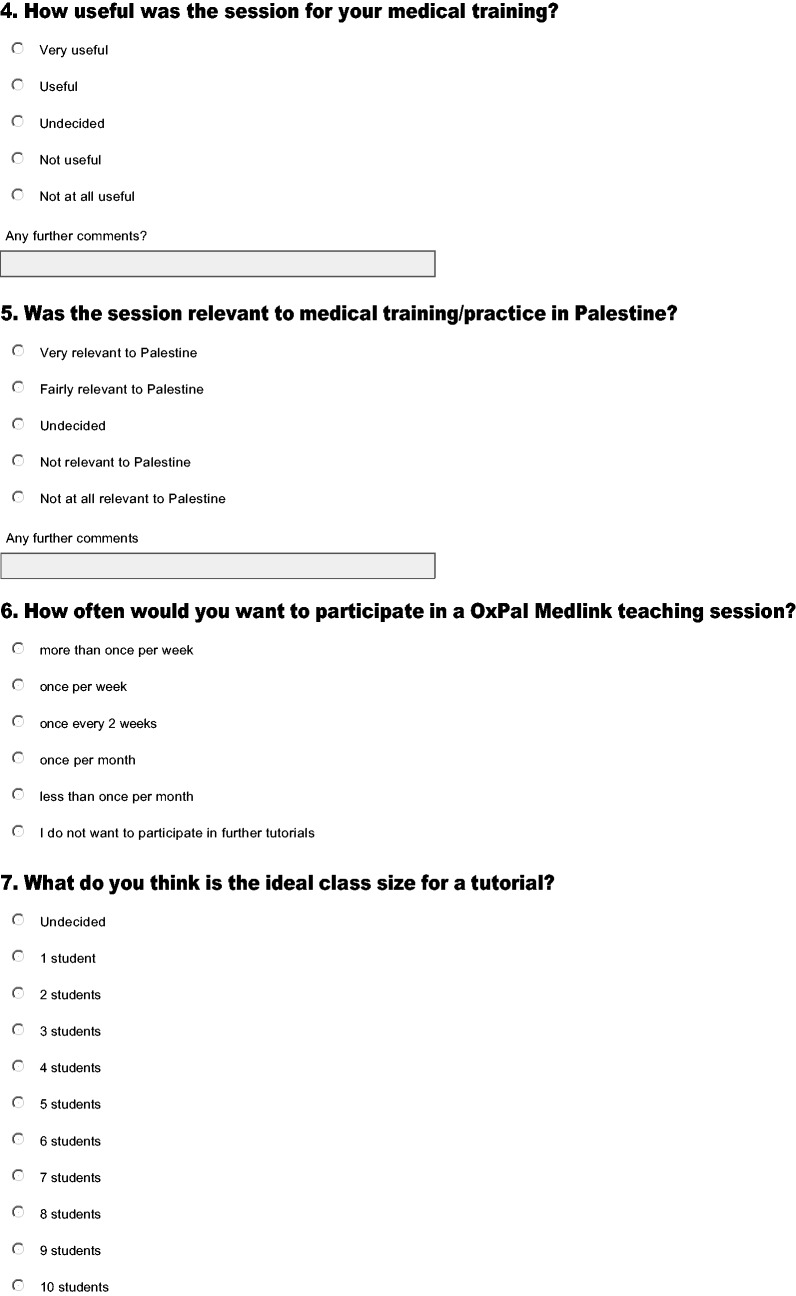
The OxPal records were reviewed in April 2013 for number of students and tutors, number of tutorials delivered and number of cases uploaded within the first year of the teaching programme. At the end of each teaching term, both students and tutors were invited to complete feedback questionnaires. These collected both quantitative and qualitative data to evaluate the teaching programme and provided an opportunity for further comments and suggestions (please see Appendix 1 for example).
Results
Needs assessment
This was conducted as part of a field visit to the West Bank in April 2013. The students demonstrated particular strengths in theoretical (book) knowledge but often struggled to apply this in dynamic clinical scenarios. This may reflect the nature and challenges of extant medical education and difficulties in accessing clinical learning environments. Students struggled with diagnostic approach (e.g. identifying the diagnosis in a patient presenting with chest pain, or shortness of breath) more so than management-based problems (e.g. ‘what is the management of myocardial infarction?’). The medical faculty cited students’ inability to withstand critical challenges to their clinical reasoning and diagnostic formulations, whilst students reported few opportunities from local faculty for constructive feedback, with examples of tutors whose teaching style was interrogative or even aggressive. At times, female students were out-sounded by more vocal male members of the group and occasionally lacked the confidence to participate fully in group discussion.
Professionalism and professional competence are difficult concepts to define and even harder to assess.9 However, there is scope to refine the students’ approach to patients, notably in communication and gaining proper consent for examination. During the examination itself, students’ interactions with patients at times lacked sensitivity – for example, manually turning the face rather than asking the patient to look to the side, retracting patients’ eyelids without warning. Whether this is a socialized or cultural practice is not clear, but when prompted students saw the value in forewarning the patient and seeking permission and consent prior to examination.
Beyond clinical skills, students also cited interest in developing a better understanding of research methods through critical analysis of published literature and even through conducting their own primary research.
Format, content and logistics of programme delivery
Between March 2012 and April 2013, OxPal hosted three eight-week terms of tutorials. 60 students (40 fourth-year and 20 fifth-year students) initially registered interest in the programme; of these, 13 did not continue, citing problems with Internet access (1 student) or commitments of other work (12). Twelve Oxford-based tutors taught on a weekly basis. A typical group size was four to six students. Approximately 90 online tutorials covering cases in internal medicine and surgery were held during this period, amounting to 750 student contact hours of online teaching.
Pilot tutorials
Several modifications were made to the logistics of the online programme following the series of pilot tutorials held in March–April 2012. The majority of tutors and students suggested that tutorials be held once weekly, of 60–90 min maximum duration; evenings between 6 and 9 pm GMT were most convenient for those both in Oxford and in Palestine. Tutors observed that activation of the students’ microphone facilities (so that they replied verbally to questions posed by tutors) led to some signal interference and slowed the pace of the teaching. The online classroom functioned better when tutors had their microphone activated whilst students typed responses in the text-based discussion panel provided, as the discussion was able to progress more rapidly without the added complication of cross-talk. Bandwidth was found to be sufficient for use of the programme.
Focus groups and semi-structured interviews
Fifty fourth-, fifth- and sixth-year medical students at AQMS participated in focus groups and interviews. Standardized scripts were used to transcribe comments and several interviews were recorded with permission for subsequent analysis. Transcripts and recordings were analysed by OxPal’s evaluation team, comprising clinical tutors and programme coordinators, to identify consensus statements and points of disagreement. Keyword analysis and thematic categorization techniques were used. Statements are presented below where there was a clear consensus of opinion, with issues raised by a minority of students presented in the discussion.
Regarding curriculum content, the level and breadth of content was appropriate for students’ knowledge and skills; tutorials were considered suitably challenging without being inaccessible. Students appreciated the case-based format. It was occasionally felt that the spectrum of topics covered was rather narrow, with certain common presentations (chest pain, shortness of breath, abdominal pain, etc.) being repeated in subsequent tutorials. As this may reflect the students’ own clinical experience, it was suggested that tutors provide some of the cases to create more variety of content. Respondents also desired tutorials in specialities other than internal medicine and general surgery, to complement clinical rotations in their fifth and sixth year.
Several students commented that OxPal tutors would occasionally assume cultural differences in approaching various pathologies which were in fact not relevant to their teaching. For example, students at AQMS are still taught that alcohol is a leading cause of acute pancreatitis even though levels of alcohol consumption in Palestine are far lower than in the UK. Students at AQMS also access many of the same textbooks and learning resources as students studying in the UK.
Optimal frequency of tutorials was thought to be at least once weekly, with duration between 60 and 90 min. All participants accessed the classes from home, with some collaborating with colleagues to log on in small groups. Connectivity was not generally a problem; students stated said that in cases of dropped internet connections (usually lasting less than 10 min), they would re-join the class when they were able to. Most tutors added extra slides but did not extensively edit student-provided cases in advance; during tutorials, roughly half of the tutors relied on Powerpoint and microphone capabilities alone, with the remainder using the interactive Whiteboard and YouTube video links in addition. The text-based discussion panel was found to be practical and intuitive. Students requested better synchronization of tutorials with their concurrent clinical attachments (e.g. to ensure that medical tutorials took place at the same time as their general medicine attachment) as well as greater clarification of intended learning outcomes and recognition of achievement – for example, certificates of participation. In consultation with the AQMS teaching faculty, it was agreed that the OxPal tutorials would not directly address curricular teaching requirements, as this might penalize students not taking part in the programme.
Faculty at AQMS and the Palestinian Minister of Health (previously Dean at AQMS) remain supportive of the programme as a means of increasing the availability of small-group tutorials for clinical students at AQMS. Tutorials were held in the evenings so as not to conflict with students’ existing academic and clinical commitments and were rearranged if necessary, for example when students had forthcoming examinations. It was emphasized that OxPal tutorials are not intended to replace core teaching, but rather to practise and enhance clinical reasoning skills and the diagnostic approach. The faculty at AQMS provided curricula to help guide choice of topics for future tutorials; whilst interested in verbal and written qualitative feedback from the students, they did not seek to more formally evaluate the programme at this stage. Both parties expressed interest in expanding the partnership, notably through development of a two-way postgraduate teaching programme.
Evaluation and feedback questionnaires
Students
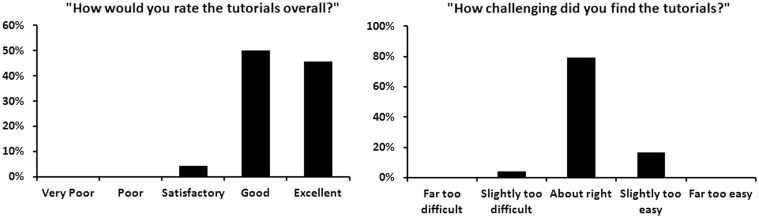
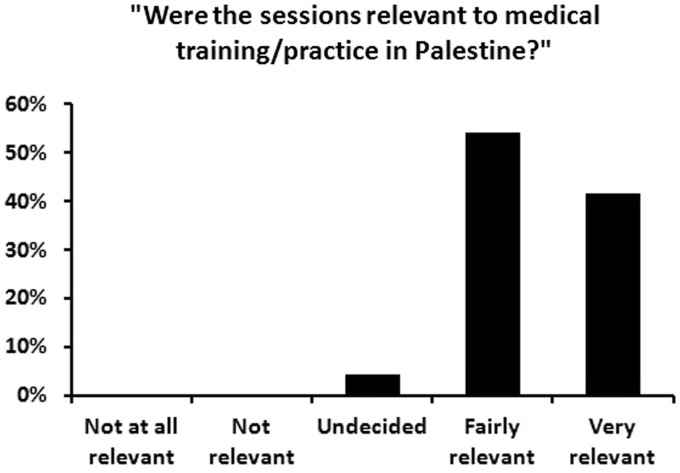
Twenty-four students (40% of those initially registered on the OxPal database and 51% of those actively enrolled in the programme) responded to the end-of-term evaluation questionnaire. Overall feedback was very positive. On a five-point scale, 96% of responders rated tutorials as ‘Excellent’ or ‘Good’ and 79% of students rated the difficulty of tutorials as adequate for their current level of training and experience (Figure 1); 96% believed the tutorials to be ‘Very’ or ‘Fairly’ relevant to medical practice in Palestine (Figure 2).
Figure 1.
Adequacy of online teaching, as assessed by student participants.
Figure 2.
Participant perception of the relevance of OxPal teaching.
Qualitative feedback reflected general satisfaction with structure and content, with students describing the programme as ‘informative’ and ‘useful’. Participants said that tutorials had taught them ‘how to think systematically’ and ‘how to think in the right way to reach the most appropriate diagnosis’. When asked what improvements could be made, the consensus was that tutorials were more effective when both the audio- and text-based chat facilities were used (it should be noted here that sound quality was frequently impaired due to limitations of the internet connection) and students felt more confident if they were made aware of topics to be covered in advance of the tutorial.
Tutors
Eight tutors (67%) responded to the questionnaire and qualitative feedback was positive. Regarding logistics, most reported that they were satisfied with the scheduling of tutorials. Some had initial problems using the WizIQ technology, but this was rapidly overcome with experience. The time commitment required to prepare for the tutorials was not considered overbearing, especially in the instances where more than one tutor was assigned to a group. Many tutors commented that students would occasionally provide cases at short notice, leaving inadequate time to prepare the tutorial; this should be addressed in the future. Students were universally acknowledged as keen and enthusiastic and their theoretical knowledge considered particularly strong. Due to the inherent nature of a text-based chat interface, it was sometimes difficult to engage all students simultaneously.
Impact
The majority of students stated that the teaching was relevant to their training and clinical practice in the context of Palestinian healthcare (Figure 2). Students frequently commented that the training in clinical reasoning had modified their practice of medicine, specifically their approach to patients, in both history and examination. Participants in OxPal online sessions were able to cite examples of ways in which the programme had altered their approach to patients: ‘when I ask questions, I think why I am asking the question, and know what to do with the answer’, ‘it is very helpful to discuss what we read in books because… reading alone is boring’ and ‘how to approach a patient, how to narrow the differential diagnoses, which (tests) to order’.
For many students, the current political context in Palestine means they are unable to leave the West Bank; they valued being part of an international professional community, and the sense of collaboration and partnership with their tutors and Oxford.
Discussion
We have presented above the results from the first year of a novel internet-based teaching programme, connecting clinical tutors based in Oxford University Hospitals with medical students in the West Bank. Evaluation through online questionnaires, focus groups and semi-structured interviews has shown teaching to be high quality and relevant to students’ experiences in Palestine.
Encouragingly, the web-based resources used in this programme were not hindered by any discrepancy in technology infrastructure between Oxford and Palestine and, in conjunction with the experiences of MedicineAfrica thus far, can serve as a model for replication in other relatively resource-poor settings.
The OxPal Medlink falls within the context of other organizations using distance-learning tools in resource-limited settings. It draws inspiration from MedicineAfrica’s social networking model, set up in response to the difficulties faced by junior doctors in Somaliland. When this was first piloted in 2008, Internet-based clinical teaching was received enthusiastically, with over 249 users registering on the site over a one-year period and reporting general satisfaction with the regular, live, case-based teaching approach. Another distance-learning programme, set up by The John Hopkins Center for Clinical Global Health Education (CCGHE), aimed to develop a full distance-learning course for HIV providers in Zambia using the open-source LMS programme called Moodle.10 Despite initial difficulties engaging students in the programme, the value and feasibility of the project (even in such a resource-poor setting, with extremely limited internet connectivity) was evidenced by high demand and successful online delivery, with 499 students registered for the third session of the course. There is therefore a growing body of evidence demonstrating the very real potential of the online platform, which can be used to build further North–South partnerships, as well as South–South and even South–North collaborations. However, the challenge comes in nurturing these teaching partnerships so that they are sustainable and ultimately self-reinforcing.
The development of clinical reasoning skills is a difficult outcome to measure and quantify. Thus far, we have relied on student and tutor feedback surveys to measure the impact of the teaching programme. As the project expands, more objective and quantifiable methods to measure clinical reasoning need to be approached. A promising avenue to explore is the script concordance test (SCT), a tool aiming to assess specific elements of clinical reasoning competence.11–13 The SCT consists of vague clinical scenarios presented to respondents, requiring them to choose between several reasonable options. The score generated reflects how closely respondents’ performances concord with those of specialists in that area.
Medical e-learning and so-called telemedicine, with translational case discussions of real individuals using imaging and investigation data, also presents some issues regarding patient confidentiality and privacy.14,15 Participants in the OxPal programme have been given templates for presenting cases which anonymizes patients but, as the project and the case database grows, it is imperative to ensure concordance with legal and ethical requirements.
It is desirable and feasible to expand the social networking function of the OxPal Medlink to facilitate contact between students and tutors outside of scheduled tutorials. This would build upon the foundations already laid by the MedicineAfrica platform to allow students to access clinical cases online and hold clinically orientated discussions with an extensive student and faculty network.
With just over half of actively enrolled students completing the online evaluation questionnaire, it is imperative to increase the feedback response rate in the future. Rather than a separate form emailed to students, tutors will be asked to supply the questionnaire during the final tutorial of the teaching term, whilst participants are still online. Awarding of participation certificates will also be contingent upon completion of a course feedback assessment. The programme is currently being modified to incorporate the student and faculty feedback outlined above. We aim to offer a variety of modular online courses with clearer learning outcomes, better synchronized with students’ clinical schedules, whilst maintaining a case-based approach. Students and tutors will alternate in providing cases for discussion; the student learning objectives provided by the AQMS faculty will be used to guide choice of topics. This more systematic approach should lead to broader coverage of the medical school curriculum. We have approached clinicians in both Oxford and Palestine to increase the range of specialities offered to include paediatrics and psychiatry, data interpretation and non-clinical areas such as research methodology and literature review. Furthermore, we will be engaging Palestinian speciality trainees, initially at Al-Makassed Hospital in East Jerusalem, in similar regular, web-based discussions hosted by UK-based consultants. The aim will be to build postgraduate links between Oxford and Palestine, culminating in shared endeavours such as joint virtual grand rounds and case-based seminars. We would seek to evaluate the impact of such intervention through quantitative and qualitative feedback questionnaires and interview and focus group evaluation.
Long term, with the support of key Palestinian healthcare stakeholders, the partnership aims to strengthen local capacity for medical education by ‘training the trainers’ and supporting near-peer education led by senior students, a model utilized at Oxford University and other medical schools in the UK. This can be achieved through hosting teacher development courses in the occupied Palestinian territories and by providing specialist training for elective students visiting Oxford. The OxPal Medlink can thereby become sustainable and self-reinforcing.
Conclusion
Our experience has shown that web-based distance-learning has the potential to be used to overcome the geopolitical barriers to medical education in the occupied Palestinian territories. Online tutorials by UK clinicians are perceived to be valuable and relevant and may improve students’ clinical reasoning skills.
Appendix 1
An example of the evaluation questionnaire sent to students after each term of tutorials.
Declarations
Competing Interests
None declared
Funding
Travel was supported by funding from MedicineAfrica (of which Alexander Finlayson is a Director), the Al-Quds Foundation for Medical Schools in Palestine and the International Medical Education Trust.
Ethical approval
Following review, ethical approval was not necessary for this study as the program was incorporated into the ongoing educational provision and feedback offered to all medical students by Al Quds Medical School. Consent was obtained at entry into the program, students enrolled in the OxPal program were able to opt in and out of online sessions at their convenience and were informed that feedback on their experiences would be sought at the end of the program.
Guarantor
IM
Contributorship
All authors meet the ICMJE criteria for authorship and contributed to the design of the study, the analysis, the drafting of the article and gave approval of the version to be published. Planning, design and delivery of online teaching: Adam M. Ali, Ishita Patel, Thomas MacGregor, Sushma Shankar, Thomas J. Cahill and Imran Mahmud; Data collection (evaluation of teaching programme, online student and tutor feedback questionnaires): Rose S. Penfold, Mohammad A. Ali, Adam M. Ali, Imran Mahmud; Data collection (needs assessment: West Bank April 2013): Rose S. Penfold, Mohammad A. Ali, Adam M. Ali, Ishita Patel, Thomas MacGregor, Sushma Shankar, Thomas J. Cahill, Alexander E.T. Finlayson and Imran Mahmud; Data Analysis: Adam M. Ali, Imran Mahmud; Drafting of article to be published: Rose S. Penfold, Mohammad A. Ali, Adam M. Ali, Ishita Patel, Thomas MacGregor, Sushma Shankar, Thomas J. Cahill, Alexander E.T. Finlayson and Imran Mahmud; Approval of final article to be published: Rose S. Penfold, Mohammad A. Ali, Adam M. Ali, Ishita Patel, Thomas MacGregor, Sushma Shankar, Thomas J. Cahill, Alexander E.T. Finlayson and Imran Mahmud
Acknowledgements
The authors extend their thanks to MedicineAfrica (www.medicineafrica.com), the Al Quds Foundation for Medical Schools in Palestine (www.fqms.org) and the International Medical Education Trust (www.IMET2000.org) for development grants to support this work and the field visit to the West Bank. Mentorship and guidance in establishing the link was also provided by MedicineAfrica. In addition to the above authors, the OxPal group includes Michael Nguyen and Saleem Lubbad. The authors are grateful to Molly Fyfe for her advice and insight.
Provenance
Not commissioned; peer-reviewed by John Rees
References
- 1. World Health Organization. The World Health Report 1999 – making a difference. Geneva: The World Health Organization, http://www.who.int/whr/1999/en/whr99_en.pdf (1999, accessed 18 August 2013)
- 2.Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet 2010; 376(9756): 1923–1958 [DOI] [PubMed] [Google Scholar]
- 3.Horton R. A new epoch for health professionals’ education. Lancet 2010; 376(9756): 1875–1877 [DOI] [PubMed] [Google Scholar]
- 4.Bhutta ZA, Chen L, Cohen J, Crisp N, Evans T, Fineberg H, et al. Education of health professionals for the 21st century: a global independent Commission. Lancet 2010; 375(9721): 1137–1138 [DOI] [PubMed] [Google Scholar]
- 5.Giacaman R, Khatib R, Shabaneh L, Ramlawi A, Sabri B, Sabatinelli G, et al. Health status and health services in the occupied Palestinian territory. Lancet 2009; 373(9666): 837–849 [Google Scholar]
- 6.Horton R. The occupied Palestinian territory: peace, justice, and health. Lancet 2009; 373(9666): 784–788 [DOI] [PubMed] [Google Scholar]
- 7.Finlayson AET, Baraco A, Cronin N, Johnson O, Little S, Nuur A, et al. An international, case-based, distance-learning collaboration between the UK and Somaliland using a real-time clinical education website. J Telemed Telecare 2010; 16(4): 181–184 [DOI] [PubMed] [Google Scholar]
- 8.Bowen J, Southgate R, Ali A, Little S, Liakos A, Greaves F, et al. Can UK healthcare workers remotely support medical education in the developing world? Focus group evaluation. JRSM Short Reports 2012; 3(7): 47–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA 2002; 287(2): 226–235 [DOI] [PubMed] [Google Scholar]
- 10.Bollinger RC, McKenzie-White J, Gupta A. Building a global health education network for clinical care and research: the benefits and challenges of distance learning tools. Infect Dis Clin North Am 2011; 25(2): 385–398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lubarsky S, Dory V, Duggan P, Gagnon R, Charlin B. Script concordance testing: from theory to practice: AMEE guide no. 75. Med Teach 2013; 35(3): 184–193 [DOI] [PubMed] [Google Scholar]
- 12.Petrucci AM, Nouh T, Boutros M, Gagnon R, Meterissian SH. Assessing clinical judgment using the Script Concordance test: the importance of using specialty-specific experts to develop the scoring key. Am J Surg 2013; 205(2): 137–140 [DOI] [PubMed] [Google Scholar]
- 13.Hornos EH, Pleguezuelos EM, Brailovsky CA, Harillo LD, Dory V, Charlin B. The practicum script concordance test: an online continuing professional development format to foster reflection on clinical practice. J Contin Educ Health Prof 2013; 33(1): 59–66 [DOI] [PubMed] [Google Scholar]
- 14.Stanberry B. The legal and ethical aspects of telemedicine. 1: Confidentiality and the patient’s rights of access. J Telemed Telecare 1997; 3(4): 179–187 [DOI] [PubMed] [Google Scholar]
- 15.Stanberry B. The legal and ethical aspects of telemedicine. 2: Data protection, security and European law. J Telemed Telecare 1998; 4(1): 18–24 [DOI] [PubMed] [Google Scholar]