Abstract
Objectives
Competency in practical skills is an important aspect of training for medical doctors. This questionnaire survey aimed to investigate if the current Foundation Year trainees have performed several practical procedures of importance and their level of confidence in carrying them out unsupervised.
Design
Questionnaire study.
Setting
Five National Health Service hospitals in England.
Participants
A total of 103 Foundation Year trainees responded to the survey (73 FY1s; 30 FY2s).
Main outcome measures
Percentage of trainees who have performed these skills and their average level of confidence.
Results
The percentage of trainees who have performed these skills and their average level of confidence (scale of 1 to 5) are as follows: intubation (32%, 1); chest drain (33%, 1); central line (26%, 1); femoral line (23%, 1); peripheral line (28%, 1); lumbar puncture (64%, 3); ascitic tap (57%, 3). Only 25% of the trainees have attended certified training courses on these skills during their Foundation Year training. More than half of these trainees (73%) found the courses very useful. Ninety-two per cent of trainees who did not attend practical skill courses are very interested to attend them. All the trainees agreed that these courses should be available for all the Foundation Year doctors, and 92% believe that these courses are most beneficial during the Foundation Year 1 training.
Conclusion
Most Foundation Year trainees have low confidence and exposure to these important practical skills. Certified practical skills courses should be made available to the Foundation Year doctors for the benefit of their training. This will also increase the quality of patient care.
Keywords: invasive procedures, Foundation Year doctor, teaching, clinical skills, structured skills course
Introduction
Foundation Year (FY) doctors are expected to achieve the level of competencies required in various core procedures and basic clinical skills before proceeding to the next stage of their training. These include venepuncture, intravenous cannulation, urethral catheterisation and arterial puncture. The opportunities to perform these core procedures are always available during ward cover and on-call shifts.
Some junior doctors would also have the opportunity to assist or perform more invasive procedures such as lumbar puncture and pleural drainage under the supervision of a trained senior doctor. Although not required as part of the FY training, these skills are important in the later stages of medical training and there is always an advantage to learning them early.
A recent study showed that structured courses aiming to teach junior doctors regarding invasive medical procedures have led to sustained improvements in self-reported confidence.1,2 However, these clinical skills courses are not always widely available to all junior doctors in their hospitals. In addition, some external courses require a fee to attend, which can be particularly difficult for F1 doctors who do not receive any allowance for educational expenses.
In this questionnaire study, we aimed to investigate the availability of opportunities to perform invasive medical procedures amongst the FY doctors in real clinical settings as well as to attend structured courses in this aspect. We also explored the confidence levels of the trainees in performing these procedures.
Design and Setting
A questionnaire survey (Figure 1) was given out by hand to random F1 and F2 doctors of five National Health Service (NHS) hospital trusts in the North West Thames region of London Deanery (Chelsea and Westminster Hospital NHS Foundation Trust, Imperial College Healthcare NHS Trust, North West London NHS Foundation Trust, Hillingdon Hospitals NHS Foundation Trust and West Middlesex University Hospital NHS Trust). The questionnaire study was designed to focus on seven invasive procedures: intubation, chest drain insertion, central line, femoral line, peripheral arterial line, lumbar puncture and ascitic tap.
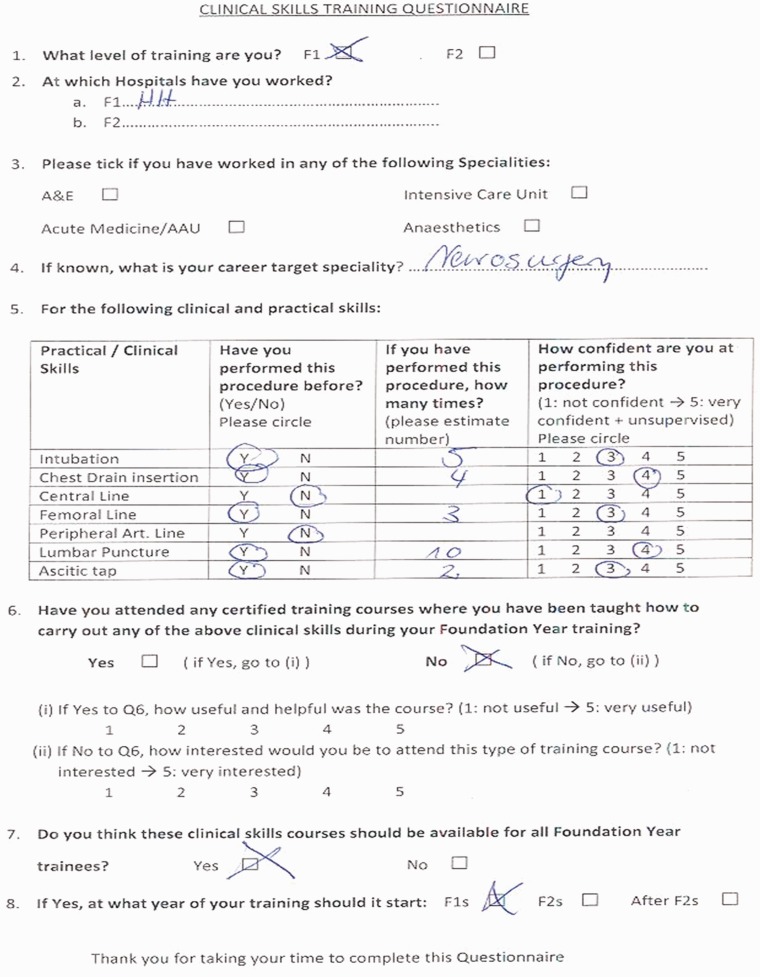
Figure 1.
The layout and questions asked in the questionnaire survey.
Main outcome measures
The trainees were asked on the number of times that they have performed the procedures and their level of confidence. The latter was assessed with a scale of one to five, with ‘one’ as ‘not confident’ and ‘five’ as ‘very confident and can perform the skills unsupervised’. Trainees were also asked if they have attended any certified or structured courses that teach them these procedures.
Results
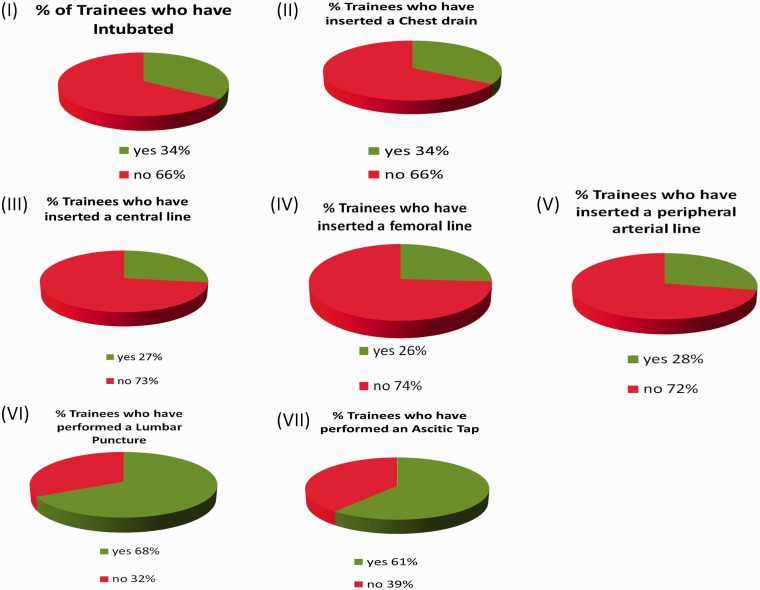
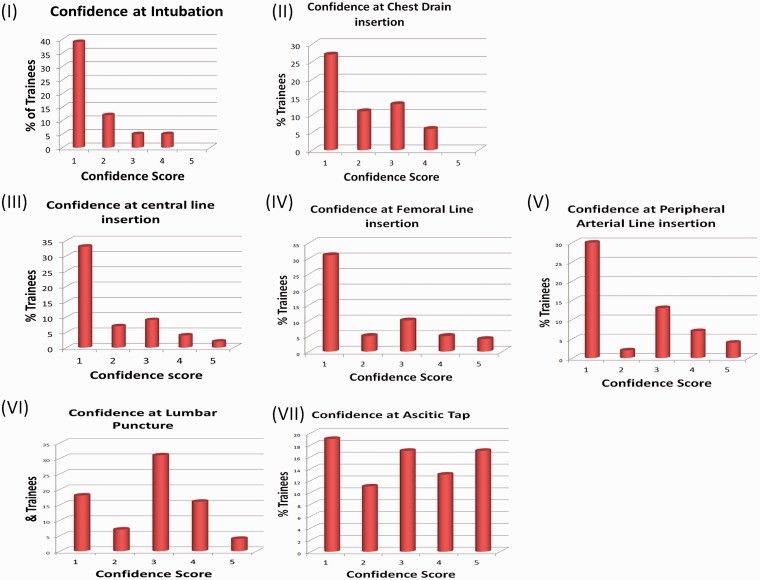
The questionnaire was distributed to 107 trainees in the five hospitals, of which four responses were excluded as the form was not completed by the individual trainees. As for the remaining 103 doctors, 73 were F1 doctors and 30 were F2 doctors. All the trainees had at least six months of clinical training in hospital settings as FY doctors at the time of the questionnaire study. The percentage of trainees who have performed the invasive procedures of interest (Figure 2a) and their average level of confidence (in a scale of 1 to 5) (Figure 2b) were as follows: intubation (34%, 1); chest drain (34%, 1); central line (27%, 1); femoral line (26%, 1); peripheral line (28%, 1); lumbar puncture (68%, 3); ascitic tap (61%, 3).
Figure 2.
The percentage of trainees who have performed these skills (a) and their average level of confidence (in a scale of 1 to 5) (b) are as follows: (I) intubation (34%, 1); (II) chest drain (34%, 1); (III) central line (27%, 1); (IV) femoral line (26%, 1); (V) peripheral line (28%, 1); (VI) lumbar puncture (68%, 3); (VII) ascitic tap (61%, 3).
Only 25% of the trainees had attended certified or structured training courses on these procedures during their FY training (21% FY1s; 33% FY2s). More than half of these trainees (73%) found the courses very useful. Ninety-two per cent of trainees who did not attend structured training courses would like to be given the opportunity to attend one. All the trainees agreed that these courses should be available for all the FY doctors, and 92% of them believe that these courses are most beneficial during the FY1 training year.
Discussion
The FY program is designed to guide and train newly qualified doctors, ensuring that they achieve the competencies required before proceeding to the next stage of their training. The core procedure skills expected from the trainees at this stage are chosen carefully and realistically. The aim is to make sure that by the end of their FY training, the trainees would be able to perform these procedures safely, independently and unsupervised.
Recent study has shown that pressure on working hours has led to a decrease in opportunities for training in invasive medical procedures for junior doctors.2 As shown from this study, one out of five of the junior doctors had the opportunity to perform at least one of the seven invasive procedures of interest, either by assisting the seniors or performing it under their supervision. More than half of the trainees (68%) have performed or assisted in lumbar puncture at this stage of their training, and the average level of confidence was an impressive three out of a scale of five. A similar pattern was observed for ascitic tap, which most of the trainees have either completed or are doing Gastroenterology specialty and acute medicine in their training (data not shown).
As expected, less than half of the trainees have performed or assisted in intubation (34%), central line insertion (27%), femoral line insertion (26%) and peripheral arterial line insertion (28%). The level of confidence of the trainees corresponds to the low exposure to these skills, with an average of one out of a scale of five. These procedures are often deemed ‘more complex’ and usually performed by the Registrars, Anaesthetists or Intensivists. Junior doctors are definitely not expected to be able to perform this independently at this stage of training. Thirty-four per cent of the trainees have performed or assisted in chest drain insertion with a low average level of confidence of 1. Interestingly, less than half of the trainees who have performed or assisted in chest drain insertion had done a respiratory placement during their training (data not shown).
Although these skills are not required in the core curriculum of FY programme, the FY doctors are keen to learn and perform them if given the opportunity. This is also reflected in the fact that all the trainees would like to have the opportunity to attend structured or certified courses that teach them invasive medical procedures. As expected, these courses are not widely available to the FY doctors and only one out of four of the trainees (25%) had attended them. There are more F2 doctors who have attended these structured courses than F1 doctors (F2, 34%; F1, 21%), but the numbers are still not significant. Some hospital trusts organise these courses for their trainee doctors but priorities are given to the doctors in core training levels, of which competency in these skills is expected at the end of their training. In addition, spaces are usually limited to ensure that the participants are able to benefit and get the most out from the skill courses. Some courses are available equally to all trainees but they will have to pay fees to attend them. The cost varies depending on the subjects covered and the facilities provided in the skills lab. This can prove difficult for junior doctors particularly the F1 doctors who do not receive any allowance for education during their first year of clinical training.
The majority of the trainees (92%) agreed that these structured courses are most beneficial during the F1 training year. This is further supported by a study that showed that the first postgraduate year is particularly significant for the development of clinical skills.3 However, a more recent study has shown that despite the significant increase in confidence amongst the junior doctors to perform these skills after attending a structured course, it only sustained for a short term and the level of confidence decreased unless there was ongoing clinical experience with the procedure.1 The benefit of short courses is eroded by the lack of reinforcement through continuing experience. Moreover, these courses require the availability of skills lab facilities, carefully structured and planned teaching as well as the supervision and input from Specialists or qualified trainees. Thus, the time at which these courses are most beneficial to the trainees is debatable but nevertheless, they should be made available to the trainees as early as possible in their training stages if feasible.
In conclusion, most FY trainees have low confidence and exposure to these invasive procedures. Certified or structured courses should be made available to the FY doctors whenever feasible for the benefit of their training and learning. This will also potentially increase their level of confidence and the quality of patient care.
Declarations
Competing interests
None declared
Funding
None declared
Ethical approval
Not required based on the research ethic agreement and policy.
Guarantor
CTL
Contributorship
CTL and VG have contributed equally to the questionnaire study.
Acknowledgements
The authors are very grateful towards all the FY doctors who took part in this questionnaire survey.
Provenance
Not commissioned; peer-reviewed by Tanzeem Raza.
References
- 1. Patel M, Oosthuizen G, Child S, Windsor JA. Training effect of skills courses on confidence of junior doctors performing clinical procedures. N Z Med J 2008; 121: 37–45 [PubMed] [Google Scholar]
- 2. Garrood T, Iyer A, Gray K, Prentice H, Bamford R, Jenkin R, et al. A structured course teaching junior doctors invasive medical procedures results in sustained improvements in self-reported confidence. Clin Med 2010; 10: 464–467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Marel GM, Lyon PM, Barnsley L, Hibbert E, Parise A. Clinical skills in early postgraduate medical trainees: patterns of acquisition of confidence and experience among junior doctors in a university teaching hospital. Med Educ 2000; 34: 1013–1015 [DOI] [PubMed] [Google Scholar]