Summary
Objectives
The number of places available in Ireland for graduate entry to medical school has steadily increased since 2006. Few studies have, however, characterized the motivational factors underlying decision to study medicine via this route. We compared the factors motivating graduate entrants versus undergraduate entry (UGE) students to choose medicine as a course of study.
Design
The present study was a quantitative cross-sectional questionnaire-based investigation.
Setting
The study was conducted in University College Cork and University of Limerick, Ireland.
Participants
It involved 185 graduate entry (GE) and 120 UGE students.
Outcome measures
Questionnaires were distributed to students addressing the following areas: demographic/academic characteristics; factors influencing the selection of academic institution and motivation to study medicine; and the role of career guidance in choice of study.
Results
When asked to list reasons for selecting medicine, both groups listed a wish to help and work with people, and a desire to prevent and cure disease. UGE students were significantly more motivated by intellectual satisfaction, encouragement by family/friends, financial reasons, and professional independence. Approximately half of GE students selected their first degree with a view to potentially studying medicine in the future. GE and UGE students differed significantly with respect to sources consulted for career guidance and source of study information.
Conclusions
This study is the first systematic examination of study and career motivation in GE medical students since the programme was offered by Irish universities and provides insight into the reasons why graduate entrants in Ireland choose to study medicine via this route.
Keywords: medicine, undergraduate entry, graduate entry programme, motivation, career guidance
Background
Two decades ago, several Australian universities initiated a four-year graduate entry (GE) medical programme with a view to broadening the sociodemographic and academic basis for student admission.1 The introduction of UK-based GE programmes in 2000 was based on workforce shortages in the National Health Services and the consequent need to produce more medical graduates. Over 10 years later, there are now 14 universities offering this programme, representing almost 10% of the current UK medical school intake.2 In Ireland, the introduction of GE programmes was prompted by the publication of the Fottrell Report ‘Medical Education in Ireland, a New Direction’,3 which recommended that the intake of European Union (EU) students into Irish medical universities be increased4; four Irish institutions currently offer such programmes of study.
Historically, UK medical school intake has been largely skewed towards those from higher socioeconomic groups, with more females than males.5 The establishment of GE programmes has allowed wider access to students from more diverse academic and social backgrounds.2,6 Age of entry to GE programmes is also higher relative to undergraduate entry (UGE) courses.2,7–10
Research in medical education has focused primarily on measuring early and long-term outcomes in graduate entrants. Studies to date have demonstrated a high completion rate for GE students in medical school, proving that this cohort can perform as well, or even better, than undergraduate students in their academic performance and clinical skills assessments.11–15
Several studies have noted differential cognitive and socioemotional profiles in GE relative to undergraduate students. Graduates have been rated as significantly more conscientious, confident, more self-controlled, more communitarian in moral orientation, co-operative, and less anxious than their undergraduate counterparts,5,9 while others have noted a stronger study commitment and work-life orientation relative to undergraduates.2,16,17
It should be noted, however, that several of these associations are potentially confounded by age at admission and type of course (e.g. problem-based learning vs. traditional curricula).9 Few studies have examined motivational variables in graduate entrants versus undergraduates, with study comparability limited due to use of diverse quantitative and qualitative techniques. In this context, motivation may be viewed as both an independent and dependent variable in medical education, influencing learning and study behaviour, academic performance, career choice in medicine, and likelihood of completing the medical course. While several factors, including age at entry into medical school, have been identified as robust predictors of commitment to completing study and pursuing a career in medicine,9,18 putative motivational factors underlying this predictive relationship have not been explored, particularly in an Irish/British context. A qualitatively based study, based on interviews with 15 non-graduate mature students entering medical school in the UK, noted that the promise of achieving self-fulfilment through the pursuit of a stimulating and rewarding career drove them to surmount all the difficulties associated with securing a place in medical school.19 We wondered whether these were the factors also influencing our students.
The present study, employing a quantitative survey-based approach, sought to examine (a) the factors influencing students’ decisions to study medicine via the GE versus UGE route; (b) motivational variables influencing choice of medicine as a career in GE versus UGE students; and (c) the use of career guidance services and other information sources in their selection of specific medical programmes in GE versus UGE students, in two Irish medical schools.
Methods
Subjects
This study was a quantitative cross-sectional study conducted at the School of Medicine, University College Cork (UCC), and Graduate Entry Medical School, University of Limerick (UL), Ireland. Study participants were medical undergraduate students enrolled in either direct entry undergraduate programme (UGE; years 1–5) or the graduate entry medicine programme (GE; years 1–4) during the academic year 2011–2012. A convenience sampling method was employed.
Instrument
The authors developed a questionnaire, adapted from a previous study which examined the motivation to study medicine in GE students in Australian medical schools.8 Specifically, questions were amended and additional items were included (see areas 2 and 4 below). The questionnaire contained both closed and open-ended questions; the majority of the former response type containing binary yes/no response options. The survey content addressed the following four areas:
Demographic and academic characteristics: Age, sex, year of study, background degree subject, and awarding university (where applicable).
Selection of GE programme (GE only): timing of decision to study medicine, factors involved in the selection of undergraduate degree.
Motivational variables related to the study of medicine: participants provided a yes/no answer beside a list of reasons for choosing medicine; the list of variables was adapted from a survey developed by Rolfe et al.8
Role of career guidance: perceived quality of career advice received, sources of information consulted concerning medical school programmes.
Procedures
For UCC students, paper questionnaires were distributed to GE and UGE students in a lecture theatre at the end of a tutorial in October/November 2011. Students were instructed that the goal of the study was to examine the factors influencing decision to choose medicine as a course of study. They were provided with instructions for completion of the questionnaire, along with assurances that they were free to withdraw consent to participation at any point. The completed questionnaires were then collected after a 15- to 20-min period. UL GE students were sent, via email, a link to the survey instrument, hosted on surveymonkey.com (Portland, Oregon, USA) during February 2012. Instructions for completion and issues related to consent were identical to the paper version.
Data analysis
All data are summarized as percentages and are illustrated in the figures and tables. To examine differences between both groups of respondents (GE vs. UGE) with respect to demographic and motivational variables, chi-square or Fisher’s exact tests were used, as appropriate. Statistical analyses were carried out using PASW Statistics 18 (IBM, New York, NY, USA). As outcomes were addressed by several questions in the survey, Bonferroni adjustment for multiple comparisons was used to ensure that the overall alpha level of the simultaneous comparisons was 0.05. For analysis of responses to open-ended questions, analysis was restricted to a thematic analysis and constant comparison of written comments provided by students, as described previously.20
Results
In total, 305 completed questionnaires from 185 GE medical students and 120 undergraduate medical students were analysed. The response rate across the various groups was as follows: UL GE students – 57% (80/140); UCC GE students – 53% (105/200); and UCC UGE students – 23% (120/520).
Demographic and academic characteristics
Although there was considerable overlap in age between GE and UGE students, graduate entrants were generally older than their undergraduate colleagues (χ 2 = 40.91, p < 0.0001; Table 1). Less than half (42.2%) of the GE students were aged between 21 and 25 years old, while in the UGE medical programme, approximately 90% of the students were 25 years old or younger. There were a higher proportion of students aged 31 or over in GE (11.3%) compared to the undergraduate medical programme (2.5%). In relation to the latter statistic, at the present point in time, older or mature students who are not eligible to enter via the GE route may apply for a small number of mature entry places in the 5-year undergraduate programme in UCC. Among study respondents, the male:female ratio differed across both programmes (see Table 2), but this difference was not statistically significant (χ 2 = 1.50, p = 0.47). In the case of both GE and UGE students, the greatest number of respondents (41.7% and 46.5%, respectively) were currently in year 1 of their studies. Among GE respondents, the majority of students had completed their first degree in the areas of science (56.2%) or medicine and health sciences (14.1%), with the remaining students possessing degrees in the areas of arts and social sciences, business, engineering, and law.
Table 1.
Sociodemographic and education characteristics in GE versus UGE students.
| Undergraduate (n = 120) | Graduate-entry (n = 185) | p | |||
|---|---|---|---|---|---|
| n | Valid % | n | Valid % | ||
| Age categories | |||||
| 17–20 | 52 | 43.3 | 0 | 0 | <0.001 |
| 21–25 | 57 | 47.5 | 78 | 42.2 | |
| 26–30 | 8 | 6.7 | 85 | 45.9 | |
| 31–35 | 3 | 2.5 | 13 | 7 | |
| Over 35 | 0 | 0 | 8 | 4.3 | |
| Sex | |||||
| Male | 53 | 44.2 | 94 | 51 | 0.46 |
| Female | 65 | 54.2 | 87 | 47 | |
| Year of degree | |||||
| Year 1 | 50 | 41.7 | 86 | 46.5 | – |
| Year 2 | – | – | 49 | 26.5 | |
| Year 3 | 13 | 10.8 | 30 | 16.2 | |
| Year 4 | 38 | 31.7 | 20 | 10.8 | |
| Year 5 | 19 | 15.8 | – | – | |
| Background degree | |||||
| Science | – | – | 104 | 56.2 | – |
| Medicine and health | – | – | 26 | 14.1 | |
| Business | – | – | 12 | 6.5 | |
| Engineering | – | – | 12 | 6.5 | |
| Arts and social sciences | – | – | 23 | 12.4 | |
| Law | – | – | 5 | 2.7 | |
| Background degree: origin | – | – | |||
| Ireland | – | – | 106 | 57.3 | – |
| North America | – | – | 59 | 31.9 | |
| United Kingdom | – | – | 7 | 3.8 | |
| Other | – | – | 6 | 3.2 | |
Selection of GE medicine programme: timing and academic background
Both programmes differed significantly with respect to timing of students’ decisions to study medicine (χ 2 = 73.08, p < 0.0001). Students across both the GE (45%) and UGE (91%) programmes indicated a strong ambition to study medicine since primary- and second-level education. Among GE students, approximately a quarter (25.56%) of students made the decision during their third-level studies in a different discipline, compared to 9.17% of UGE students; 29.44% of GE respondents entered medicine via the GE programme after qualifying in a different discipline (Figure 1a).
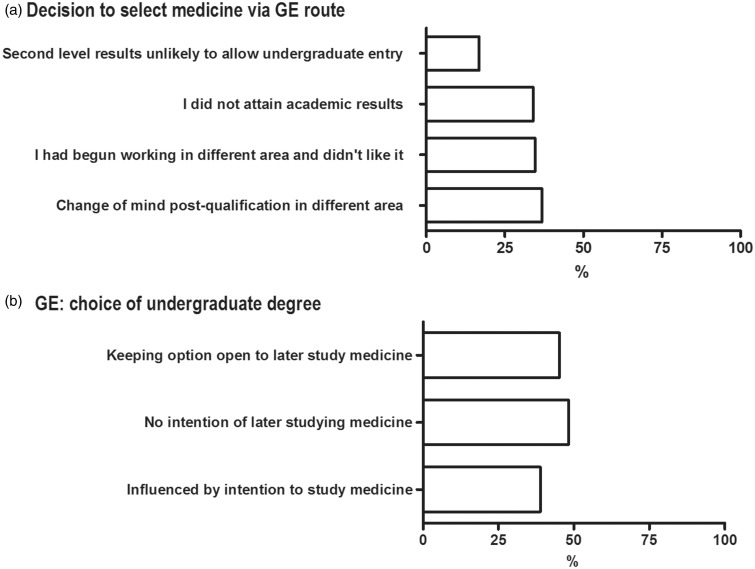
Figure 1.
(a) Percentage of GE respondents’ reasons for selecting medicine via the GE route. (b) Percentage of GE respondents’ reasons for choice of undergraduate degree course in relation to future studies in medicine.
GE respondents cited the following reasons, in ascending order of importance, for choosing to study medicine via the GE route: awareness that second-level results were not likely to allow access to the undergraduate programme; failure to attain results necessary to enter an undergraduate programme; desire to change occupation; and change of mind following qualification in a different area (Figure 1a).
Figure 1(b) demonstrates the responses of GE students when asked whether they had considered the possibility of studying medicine during the selection of their first degree. Almost half (48%) of GE students indicated that they had no intention of later studying medicine when they selected their undergraduate degree; 45% of students selected their primary degree with a view to keeping open the possibility of studying medicine in the future, while 39% of respondents indicated that the intention to later study medicine had a direct bearing on selection of their first degree.
75.10% of GE students were happy with the subject they chose for their undergraduate degree, with the remaining students (n = 42) unhappy and wishing they had chosen a different topic. Based on the qualitative data provided by the latter group, 33 (79%) students responded that they would have liked to have selected more subjects in the biological sciences at either/both second- and third-level in order to prepare them better for the GE programme. Five (12%) students indicated that they should have selected a more competitive undergraduate programme, or a less competitive university where reduced grade deflation may have helped in obtaining a better first undergraduate degree.
Motivation for studying medicine: GE versus UGE programme
The majority of respondents, regardless of medicine programme, reported that the primary motivating factors for studying medicine were in order of importance the following: wanting to help other people, working with people, and having the desire to cure and prevent disease (see Table 2). Significant differences were observed between graduate entrants and undergraduates across four listed motivational factors: professional independence (χ 2 = 37.80, p < 0.0001), intellectual satisfaction (χ 2 = 22.24, p < 0.0001), financial reasons (χ 2 = 9.21, p = 0.009), and encouragement from family/friends (χ 2 = 42.34, p < 0.0001).
Table 2.
Motivations for studying medicine in GE versus UGE students.
| Motivational variables | Undergraduate (n = 120) | Graduate-entry (n = 185) | p | ||
|---|---|---|---|---|---|
| n | Valid % Responding positively? | n | Valid % | ||
| Friends/relatives studying medicine | 41 | 34.16 | 49 | 26.50 | 0.034 |
| Financial reasons | 47 | 39.16 | 51 | 27.57 | 0.009† |
| Curing and preventing disease | 109 | 90.83 | 158 | 85.41 | 0.083 |
| Helping people | 113 | 94.17 | 166 | 89.73 | 0.122 |
| Working with people | 92 | 76.67 | 130 | 70.27 | 0.057 |
| Intellectual satisfaction | 66 | 55.00 | 55 | 29.73 | <0.0001† |
| Professional independence | 98 | 81.67 | 87 | 47.00 | <0.0001† |
| Parental encouragement | 85 | 70.83 | 62 | 33.50 | <0.0001† |
Significant after Bonferroni correction.
GE students were significantly more likely than UGE students to indicate satisfaction with decision to study medicine (97.18% vs. 88.33%; χ 2 = 17.15, p = 0.001). Analysis of qualitative data in the case of the minority of GEs who indicated some dissatisfaction with their decision to study medicine revealed that this related to uncertainty concerning postgraduate medical career choices and future job opportunities.
Selection of medical programme: role of career advice and guidance
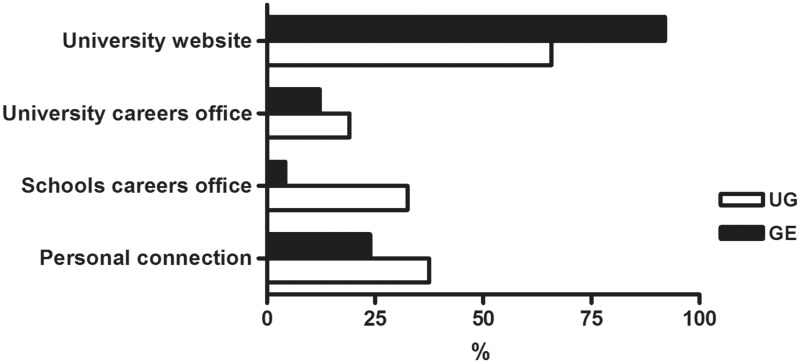
Comparing both programmes with respect to which source of information students accessed before making final programme choices, GEs were significantly more likely than UGE students to consult university and medical school websites (92.00% vs. 65.83%; χ 2 = 36.01, p < 0.0001; Figure 2); the converse pattern was observed for schools career office (4.29% vs. 32.50%; χ 2 = 56.72, p < 0.0001), university careers office (12.27% vs. 19.16%; χ 2 = 17.31, p < 0.0001), and personal connections (23.92% vs. 37.50%; χ 2 = 21.03, p < 0.0001). Only 43.65% of GE respondents were satisfied with the quality of career advice received prior to undertaking their first degree.
Figure 2.
Percentage of responses according to source of information consulted regarding medicine course in GE versus UGE students.
Discussion
In the present study, GE programme students presented with a different motivational profile compared to their undergraduate colleagues in terms of reasons for studying medicine. Notably, GE students were significantly less likely than UGE students to report choosing medicine on the basis of financial reasons, family encouragement, intellectual satisfaction, and professional independence. In contrast, GE students were overwhelmingly motivated by desire to work with, and help, people, along with a desire to cure and prevent disease. This profile was accompanied by a higher degree of satisfaction with the decision to study medicine relative to UGE students. The majority of students, regardless of their programme, had developed an interest in studying medicine while completing second-level education; this has to be viewed as an important determinant of motivation to study medicine via the GE route, particularly for students who had applied but failed due to unattainable required results during second level.
Interestingly, in a finding which may have outreach implications for potential students on both programmes, GE students were significantly more likely to consult university websites when deciding on their preference of specific medical programme. Schools offering GE medicine programmes should note this and ensure that relevant and appropriate information is accessible electronically. In contrast, UGE students showed a reliance on one-to-one contact with schools or university career office and personal contacts. Additionally, the majority of GE students were not satisfied with the quality of careers advice received before embarking on their first degree, suggesting that there is an increased need for these services to be prepared for advice on preparing to study medicine via the GE route.
The present data are in agreement with the Australia-based study by Rolfe et al.,8 where the most cited motivation for studying medicine among both undergraduate and GE students related to a desire for working with people and helping others. In both studies, UGE respondents were more likely to be driven by parental expectations. This is perhaps not surprising. However, in direct contrast with this earlier study, our UGE students were more likely to be motivated by both the need for intellectual satisfaction and professional independence than our GE students. This is a surprising finding but is perhaps consistent with the observation that the majority of GE students were in retrospect still happy with their first undergraduate course choice and thus they had achieved intellectual satisfaction in other pursuits. It would appear to be a consistent finding that GE students focus on working with and helping people. These findings are in agreement with reports of increased skills related to co-operation in GE students,9 and a report that GE interns felt better prepared in terms of interpersonal and collaborative skills relative to UGE counterparts.21
With respect to study limitations, while the size and multi-centre nature of the GE sample compares favourably with existing studies, the UGE sample size in relation to total cohort of UGE is limited. Additionally, it may be argued that self-reported outcome measures relating to motivations may be affected by recall bias or other confounding variables. However, in the present study, the majority of both GE and UGE respondents were first year students. Hence, it may be proposed that they still have a fresh and clear remembrance of their motivations while applying to the programme. A previous interview-based study conducted in Iran demonstrated that students who were already two to three years into the curriculum were unlikely to hold the same motivations relative to when they initially applied to the programme.22
GE medical programmes provide an important opportunity to many people who had a long-life ambition of doing medicine, but failed to attain necessary second-level results, to explore related areas with a view to eventually realising their ambitions. As also observed in previous studies,8 the majority of GE students held background degrees in a science subject or related to medicine and health sciences. Previous studies have shown that academic background is a significant predictor of progress in certain aspects of the GE curriculum,23,24 although this advantage diminishes as the course progresses.23 Employing a multivariate analysis of factors impacting on overall course performance, a recent study demonstrated that educational background (subject of first degree) had little relationship with the final examination results.15 The latter study, in agreement with a previous study,23 also demonstrated that the only advantage conferred by previous academic background was on specific module performance in the early part of the course.
The present data add to a growing body of knowledge research indicating a different profile for GE students in terms of timing and acquisition of clinical skills and biomedical sciences knowledge.11,12 Specifically, it shows that GE students also differ from undergraduates with respect to prior educational experience, learning style, and motivational factors.14,20 It remains to be clarified how these differences might relate to various assessments and other performance data during completion of their medical degree. Another avenue for investigation is whether differences between both groups will relate to subsequent postgraduate careers in medicine.
Conclusions
Research comparing graduates with different pre-medical school backgrounds is essential, given the increased number of students from both programmes who are now entering the workforce, and considering the number of medical schools considering changes to admission policies. The present data, collected from both UGE and GE students attending Irish medical schools, indicate that each cohort not only traverse different academic pathways to medicine but also differ with respect to motivational variables related to career choice. The majority of our GE and UGE students had wanted to study medicine from the outset, but it is interesting that our UGE students, who have less life experience, are more likely to indicate that professional independence and intellectual fulfilment are key motivating factors in their decision making. Such motivations have previously been more associated with older applicants.
Declarations
Competing interests
None declared
Funding
None declared
Ethical approval
This study was approved by the Clinical Research Ethics Committee of the Cork Teaching Hospitals (reference number ECM 4 (iii) 08/11/11) and the University of Limerick Faculty of Education and Health Sciences Research Ethics Committee (reference number EHSREC11-57).
Guarantor
CO’T
Contributorship
SS, CO’T, DMcG, SO’F, PF, and MH conceived of the study, participated in its design and coordination, and helped to draft the manuscript. SS also collected the data and performed the statistical analysis. All authors read and approved the final manuscript.
Acknowledgements
None
Provenance
Not commissioned; peer-reviewed by Olwyn Westwood
References
- 1. Blackman I, Darmawan IGN. Graduate-entry medical student variables that predict academic and clinical achievement. Int Educ J 2004; 4: 30–41 [Google Scholar]
- 2. Carter YH, Peile E. Graduate entry medicine: high aspirations at birth. Clin Med 2007; 7: 143–147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Working Group on Undergraduate Medical Education. Medical education in Ireland: a new direction, Dublin: Department of Health & Children, 2006 [Google Scholar]
- 4. Finucane P, Arnett R, Johnson A, Waters M. Graduate medical education in Ireland: a profile of the first cohort of students. Ir J Med Sci 2008; 177: 19–22 [DOI] [PubMed] [Google Scholar]
- 5. James D, Ferguson E, Powis D, Bore M, Munro D, Symonds I. Graduate entry to medicine: widening psychological diversity. BMC Med Educ 2009; 9: 67–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Garrud P. Who applies and who gets admitted to UK graduate entry medicine? – an analysis of UK admission statistics. BMC Med Educ 2011; 11: 71–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lambert TW, Goladacre MJ, Parkhouse J. Graduate status and age at entry to medical school as predictors of doctors’ choice of longterm career. Med Educ 2001; 35: 450–454 [DOI] [PubMed] [Google Scholar]
- 8. Rolfe IE, Ringland C, Pearson SA. Graduate entry to medical school? Testing some assumptions. Med Educ 2004; 38: 778–786 [DOI] [PubMed] [Google Scholar]
- 9. Wilkinson TJ, Wells JE, Bushnell J. Are differences between graduates and undergraduates in a medical course due to age or prior degree? Med Educ 2004; 38: 1141–1146 [DOI] [PubMed] [Google Scholar]
- 10. Mathers J, Sitch A, Marsh JL, Parry J. Widening access to medical education for under-represented socioeconomic groups: population based cross sectional analysis of UK data, 2002–6. BMJ 2011; 341: d918–d918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Calvert MJ, Ross NM, Freemantle N, Xu Y, Zvauya R, Parle JV. Examination performance of graduate entry medical students compared with mainstream students. J Royal Soc Med 2009; 102: 425–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Manning G, Garrud P. Comparative attainment of 5-year undergraduate and 4-year graduate entry medical students moving into foundation training. BMC Med Educ 2009; 9: 76–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dodds AE, Reid KJ, Conn JJ, Elliott SL, McColl GJ. Comparing the academic performance of graduate- and undergraduate-entry medical students. Med Educ 2010; 44: 197–204 [DOI] [PubMed] [Google Scholar]
- 14. Shehmar M, Haldane T, Price-Forbes A, Macdougall C, Fraser I, Peterson S. Comparing the performance of graduate-entry and school-leaver medical students. Med Educ 2010; 44: 699–705 [DOI] [PubMed] [Google Scholar]
- 15. Bodger O, Byrne A, Evans PA, Rees S, Jones G, Cowell C, et al. Graduate entry medicine: selection criteria and student performance. PloS One 2011; 6: 11–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kronqvist P, Makinen J, Ranne S, Kappa P, Vainio O. Study orientations of graduate entry medical students. Med Teach 2007; 29: 836–838 [DOI] [PubMed] [Google Scholar]
- 17. Goldacre MJ, Davidson JM, Lambert TW. The first house officer year: views of graduate and non-graduate entrants to medical school. Med Educ 2008; 42: 286–293 [DOI] [PubMed] [Google Scholar]
- 18. Kusurkar R, Kruitwagen C, Cate O, Croiset G. Effects of age, gender and educational background on strength of motivation for medical school. Adv Health Sci Educ 2010; 15: 303–313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mathers J, Parry J. Older mature students’ experiences of applying to study medicine in England: an interview study. Med Educ 2010; 44: 1084–1094 [DOI] [PubMed] [Google Scholar]
- 20. O’Tuathaigh CMP, Duggan E, Khashan AS, Boylan GB, O’Flynn S. Selection of student selected component (SSCs) modules across the medical undergraduate curriculum: relationship with motivational factors. Med Teach 2012; 34: 813–820 [DOI] [PubMed] [Google Scholar]
- 21. Dean SJ, Barratt AL, Hendry GP, Lyon PM. Preparedness for hospital practice amongst graduates of a problem-based, graduate-entry medical programme. Med J Aust 2003; 178: 163–167 [DOI] [PubMed] [Google Scholar]
- 22. Nedjat S, Majdzadeh R, Rashidian A. Graduate entry to medicine in Iran. BMC Med Educ 2008; 8: 47–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Craig P, Gordon JJ, Clark RM, Langendyk V. Prior academic background and student performance in assessment in a graduate entry programme. Med Educ 2004; 38: 1164–1168 [DOI] [PubMed] [Google Scholar]
- 24. Groves M, O’Rourke P, Alexander H. The association between student characteristics and the development of clinical reasoning in a graduate-entry, PBL medical programme. Med Teach 2007; 25: 626–631 [DOI] [PubMed] [Google Scholar]