Abstract
Major epidemics of measles are again in the news across the UK because of our failure to maintain population herd immunity. This situation has occurred primarily because of a loss of public confidence in the measles, mumps and rubella (MMR) vaccine, which was never restored following the Wakefield debacle, and a lack of awareness of the potential morbidity and mortality associated with measles. This article provides healthcare professionals with a succinct overview of important clinical aspects of measles and also describes the history of measles vaccination in the UK. Restoration of herd immunity will require higher public acceptance of the MMR vaccine in the context of recognition that measles remains an important infection. While achievement of this appears to be challenging, recent UK-based research suggests that it can be ascertained.
Keywords: measles, vaccine, vaccination
Introduction
Vaccination can be viewed in two different ways: one, as a supreme healthcare intervention that cost-effectively reduces morbidity and mortality, or, two, as an unusual pattern of exposure where the route, dose, age of exposure and strain of virus the person is exposed to, are all changed.1 Regardless of how individuals view vaccination, measles is one of the leading vaccine-preventable causes of morbidity and mortality among young children globally2 and is an important target for public health intervention. Recent, highly publicized outbreaks of measles in the UK have highlighted the need for all healthcare professionals working in primary and secondary care, and in public health, to be aware of this re-emerging infection. In this concise article, we review key clinical aspects of measles and place the current epidemiology of measles in the UK in the context of the turbulent history of measles vaccine.
Methodology
We performed a literature review of English-language studies by searching the Medline and Cochrane collaboration databases using the terms ‘Measles’, ‘Vaccine’, ‘Eradication’ and ‘History’. Information about measles was also ascertained from the World Health Organization (WHO), Health Protection Agency and the Medical Research Council (MRC) websites, and from general internet searches.
Important clinical aspects of measles
Measles is a disease caused by a single-stranded, negative-sense RNA Morbillivirus that is spread primarily via respiratory droplets with an incubation period of 8–14 days2; a high proportion of susceptible household contacts will develop infection. It is recognisable by the typical maculopapular rash associated with fever and the three ‘C’s’: cough, coryza and conjunctivitis, although not all of these may be present and the rash can sometimes look atypical. The rash lasts for at least 3 days and is first seen on the forehead and neck, followed by the trunk and finally the limbs. Patients are considered to be infectious until after the fourth day of rash. One of the significant sequelae of measles infection is immunosuppression, which persists for a few weeks and increases the risk of secondary complications. Complications of measles include otitis media (5%), respiratory tract infections (4%), convulsions (0.5%) and neurological complications (0.1%)3 with immunocompromised patients, pregnant women and children less than 1 year of age particularly at risk; susceptible individuals in these groups should be considered for human normal immunoglobulin following exposure to measles. Treatment is predominantly supportive, but antibiotics may be required in some cases for secondary bacterial infection and high-dose vitamin A should be prescribed in those at risk of deficiency.4
In the UK, cases should be reported to the local health protection unit and when admitted to hospital patients should be isolated, preferably in a negative pressure isolation room, and the infection control team informed; susceptible healthcare staff should not have contact with suspected cases. The potential impact of nosocomial transmission from a patient to a healthcare worker and onward to a second patient was recently reported; 110 contacts were identified for the healthcare worker with 61 advised to have vaccination and 5 given immunoglobulin.5 As with influenza and other vaccine-preventable infections, to avoid such occurrences, healthcare organizations and individual staff members have an ethical obligation to be aware of and ensure maintenance of their vaccination status.
Because the symptoms of measles are non-specific, and patients with fever and rash commonly present to both primary and secondary care, cases are easily missed. However, in a population that is suboptimally vaccinated and suffering outbreaks, as is the case in the UK currently, to ultimately achieve eradication, the identification of cases is critically important to public health interventions, such as contact tracing and the immunization of susceptible individuals; ‘coalface’ healthcare professionals therefore need a low threshold to considering measles a possible diagnosis. The WHO defines a case as: ‘any person in whom a clinician suspects measles, or any person with fever and generalized maculopapular rash and cough, coryza or conjunctivitis’.4 The presence of measles-specific IgM antibodies, in the appropriate clinical context, provides laboratory confirmation of a measles case. Awareness of the clinical symptoms and signs of measles among health professionals in the UK is likely to be considerably lower than in previous decades, but is critical to reducing the number of missed cases and increasing intervention opportunities. Given that measles is an extremely contagious infectious disease with considerable morbidity, population vaccination is a critical part of prevention and control. The description of a case of measles in a young adult, with photographs of the rash, recently admitted to our unit is available via open access.6
The history of the measles vaccine
1950s–1980s
Before the first clinical use of measles vaccine in the UK, there were cycles of large epidemics every other year. The peak in 1955 saw 693,803 measles cases that contributed to 174 deaths (0.025%).7 The early use of measles vaccines in 1961 was based on a trial of three live attenuated vaccines derived from the Edmonston strain.8 Seventy-seven children took part in the research and although a protective antibody response was achieved, over half of the children experienced moderate to severe systemic reactions, including rash, pyrexia and tonsillitis.9 To reduce these side effects, a ‘weaker’ vaccine strain was developed and tested by the MRC in a series of four trials.10 The use of a single antigen measles vaccine was subsequently introduced in the UK for children between 1 and 2 years of age in 1968. In the 1970s, there was poor vaccination coverage with fewer than 60% of children vaccinated by the age of 2 years.11 It was not until the late 1970s that major national and international efforts developed routine immunization systems. As a result, by the mid-1980s measles vaccination coverage had increased to 80% with the number of cases decreasing to less than 100,000 per year with 13 deaths compared with peaks of over half a million cases and 100 deaths in previous decades.12 Between 1985 and 1988, however, vaccine failure remained common. The reasons for this were described by Krugman,13 and included: inadequate refrigeration of vaccine, early administration (before 12 months of age), excessive exposure of vaccine to light, simultaneous administration of gamma globulin and the use of killed measles vaccine.
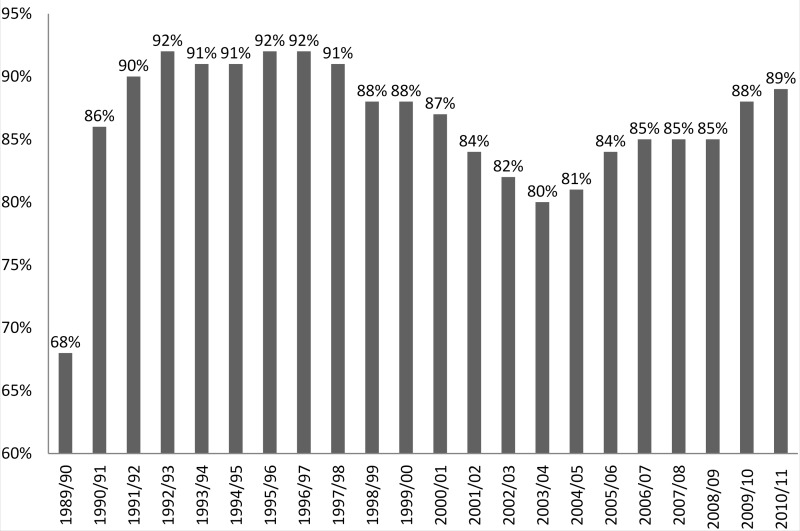
In 1988, a combined measles, mumps and rubella (MMR) vaccine replaced the single antigen vaccine and was given to children between 1 and 2 years of age. It was also offered to preschool children over the age of two in a ‘catch-up’ programme.11 As seen in Figure 1,14 following the introduction of MMR to several national vaccination campaigns and to the routine childhood immunization programme, coverage at 2 years of age reached a peak of around 92% in 1991 persisting until 1998.
Figure 1.
MMR vaccine coverage in England at 2 years of age, 1988–1989 to 2010–2011 (based on HPA information).14
1990s
Although notifications of measles fell annually from 1988 to 1991, an increase occurred in older children in 1992.11 A second dose of MMR at the age of 11 years was therefore introduced. Revaccination has been shown to increase clinical protection from 95% to 99.7%,11 which is important from the population perspective considering that 92–95% vaccination coverage15 is needed to achieve herd immunity and protect unvaccinated, susceptible individuals. During this period a failure in maintaining high vaccination coverage occurred leading to an epidemic in western Scotland and several outbreaks in England and Wales.11 A combined measles–rubella vaccine was, therefore, offered to all schoolchildren aged 5–16 years in a 6 week national campaign in 1994.11 In 1993, Wakefield et al.16 published an article suggesting a link between exposure to measles vaccines and Crohn’s disease in children.
In 1996, a two-dose schedule of MMR was routinely offered to all children, the first dose given at 12–13 months with a booster between the age of 3 years and 4 months and 5 years.11 In 1998, the now infamous research article by Wakefield et al.17 was published in The Lancet. This erroneously suggested a link between the MMR vaccine, bowel disease and autism. The research included 12 children, 8 of whom appeared to have developed the condition very shortly after receiving MMR vaccine. The authors recommended the use of single vaccines instead of the combined MMR vaccine.15 This triggered immediate criticism and consequently a meeting of over 30 experts, convened by the MRC, concluded that the evidence did not support a causal link between MMR, autism and bowel disease. It has also been suggested18 that the research behind The Lancet article was a sophisticated fraud. The lead author, Andrew Wakefield, however, continues to defend his position, although he has now been struck off the General Medical Council medical register in the UK.1 Numerous studies have subsequently failed to show an association between MMR vaccine and autism.
In 1999, the public’s response to Wakefield’s paper resulted in a decline in vaccination coverage and an increase in parental demand for single MMR vaccines. The UK government subsequently banned the single-dose vaccine, which was the only alternative to MMR. This decision was based on a number of reasons, including a failure to pass UK safety testing, delay in the complete immunisation of children, reduction in the percentage of children vaccinated and an increase in the number of injections and potential for side effects.19
2000 onwards
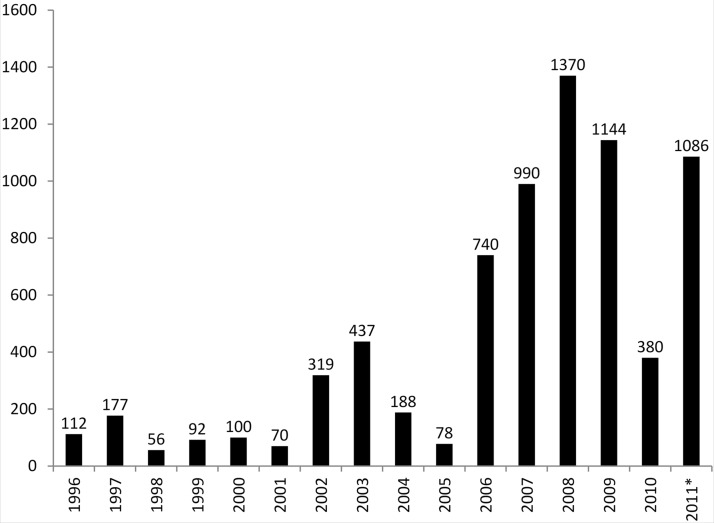
Given that the measles vaccine is as effective in the single formulation,2 it has been argued that keeping the options of both MMR and single-dose vaccines for parents might have maintained higher population coverage and reduced the subsequent increase in measles cases and outbreaks. It is likely, however, that government approved use of the single vaccine would have further undermined the MMR vaccine and made subsequent re-introduction to the childhood vaccination schedule more difficult for the public to accept. Although vaccination coverage in England was at its lowest in 2003–2004,14 the incidence of measles remained low. As Figure 2 shows, however, it began to rise sharply in 2008 and 2009, as population herd immunity decreased.20
Figure 2.
All laboratory confirmed cases of measles in England and Wales, 1996–2011* (based on HPA information).20
In early 2012, one of the largest outbreaks of measles since 1988 occurred in Liverpool with 301 confirmed and 148 probable cases21 resulting in an increase in MMR uptake rates. Between January and April 2012 there were 447 confirmed cases of measles in England and Wales.22 MMR coverage at this time remained lower than in the mid-1990s and considerably lower than the WHO target of 95% required for adequate population protection.11 Subsequently, large and highly reported outbreaks in, for example, northeast England and south Wales have occurred, the latter consisting of over 1000 cases with 7% requiring hospital attendance; over 75,000 vaccines were subsequently administered to unvaccinated individuals.23 Although targets set by the European region of the WHO for the elimination of measles from Europe could not be met in 2010, the target date was reset to 2015. However, as noted, there may be a considerable time lag between a decrease in vaccination coverage and a subsequent increase in the number of cases, so in light of recent UK and European outbreaks it seems unlikely that the 2015 target will be achieved.
What can we learn from the history of measles vaccination in the UK?
Perhaps the clearest message from the history described is that when vaccine uptake is inadequate or falls, there is a predictable subsequent decline in herd immunity and an increase in the incidence of measles. This effect may be delayed; the consequences of Wakefield’s erroneous research, published in 1998, have only been realized in recent years. The underlying cause of this has been an ongoing undermining of the safety of MMR vaccine, particularly by some of the popular media, and a subsequent loss of public confidence. Although the reasons why people do not seek vaccination of themselves or their children are clearly complex, as demonstrated in a recent qualitative study,24 the high uptake of other childhood vaccines without controversy, however, such as conjugate pneumococcal vaccine introduced in 2006 after the problems with MMR, suggests that the public will accept vaccination. It appears that once a vaccine scare story, even if subsequently thoroughly discredited, however, enters the public’s mindset, it is a very challenging situation to reverse, the consequences of which can last for years and beyond a single generation. A recent UK-based cluster-randomized controlled trial, however, showed that web-based decision support can significantly reduce parental decision conflict and was associated with high vaccine uptake.25
Although the recent high profile local outbreaks of measles may start to reverse the public’s scepticism of the MMR vaccine, any such effect is likely to be temporary and cannot be relied on long term. A recent mathematical modelling study showed the dangers of doing so and suggested a potential important feedback loop between disease prevalence and vaccine uptake; when the infection is rare due to vaccination, public awareness of the consequence of infection is low, and the impact on vaccine uptake of any controversy is therefore disproportionately exaggerated; the public’s incentive to get themselves or their children vaccinated is low.26 Whether other interventions, implemented before these outbreaks, could have made a difference is open to debate, but a recent UK-based quality improvement study clearly demonstrates that improvement in vaccine uptake is achievable in a deprived and diverse inner-city population using a complex intervention with components including geographically based networks of general practices, small financial incentives, consistent coding, a systematic call/recall system, and surveillance and feedback of performance.27
Conclusion
All ‘coalface’ primary, secondary and public health healthcare professionals should have, at the very least, a basic understanding of measles infection and the historical and contemporary issues surrounding vaccination. High vaccine uptake remains the key critical control point in achieving herd immunity and eradicating measles in the longer term. Increasing vaccination coverage is likely to be primarily dependent on public acceptance of the vaccine; education and maintenance of public awareness of the importance of measles infection, in the context of innovative and established interventions, are likely to be important drivers of this. Healthcare providers should take every opportunity to reinforce the message that MMR vaccine is safe, highly effective and the main route to reducing cases of measles and associated morbidity and mortality.
Key points for healthcare professionals
Measles typically presents with a maculopapular rash, fever and the three C’s: cough, coryza and conjunctivitis
Patients with suspected measles admitted to hospital should be isolated with susceptible healthcare workers avoiding contact with such patients
Healthcare workers have a responsibility to be aware of their vaccination status and to seek vaccination if appropriate
Rapid response to measles cases with reporting to local health protection units is vital in the public health response to cases
Measles vaccine in the form of the MMR vaccine is safe and very effective; high uptake is the key to eliminating measles and healthcare professionals and organizations should try to educate and maintain public awareness of the importance of measles
Declarations
Competing interests
None declared
Funding
None declared
Guarantor
LKT
Ethical approval
Not required
Contributorship
All authors included in this paper fulfil the criteria of authorship and there is no one else who fulfils the criteria but has not been included as an author. In terms of contribution, LT is responsible for the overall content as guarantor. GB and NM were equally involved in the analysis and interpretation of data, revising the article critically for important intellectual content and the final approval of the version to be published.
Acknowledgements
None
Provenance
Not commissioned; peer-reviewed by Emmanuel Okpo
References
- 1. Wakefield A. New Evidence Refutes Fraud Findings in Dr. Wakefield Case. Interviewed by Mercola JM. See http://articles.mercola.com/sites/articles/archive/2012/01/24/new-evidence-refutes-fraud-findings-in-dr-wakefield-case.aspx (2012, last checked 14 October 2013)
- 2. World Health Organization. Measles. Fact sheet No 286. See http://www.who.int/mediacentre/factsheets/fs286/en/ (2012, last checked 14 October 2013)
- 3. Miller CL. Severity of notified measles. Br Med J 1978; 1: 1253–1255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization. Measles and Rubella Surveillance and Outbreak Investigation Guidelines. See http://www.searo.who.int/LinkFiles/Measles_and_MNT_SEA_Regional_Guidelines_M&R_Surveillance_and_Outbreak_Investigation.pdf (2009, last checked 14 October 2013)
- 5. Baxi R, Mytton OT, Abid M, et al. Outbreak report: nosocomial transmission of measles though an unvaccinated healthcare worker – implications for public health. J Public Health Epub ahead of print 6 October 2013. DOI: 10.1093/pubmed/fdt096. [DOI] [PubMed]
- 6. Bannaga AS, Wiles S, Rahama O, et al. Study in pink … rash!. BMJ Case Rep 2013. DOI: 10.1136/bcr-2013-201319. [DOI] [PMC free article] [PubMed]
- 7. Health Protection Agency. Measles Notifications and Deaths in England and Wales, 1940--2008. See http://www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1195733835814 (2013, last checked 14 October 2013)
- 8. Goffe AP, Laurence GD. Vaccination against measles: Part I. Preparation and testing of vaccines consisting of live attenuated virus. BMJ 1962; 2: 1244–1246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Aldous IR, Kirman H, Butler N, Goffe AP, Laurence GD, Pollock TM. Vaccination against measles: Part III. Clinical trial in British children. BMJ 1961; 2: 1250–1253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Benson PF, Butler NR, Goffe AP, et al. Vaccination of infants with living attenuated measles vaccine (Edmonston strain) with and without gamma-globulin. BMJ 1964; 2: 851–853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ramsay M, Gay N, Miller E, et al. The Epidemiology of Measles in England and Wales: Rationale for the 1994 National Vaccination Campaign. Health Protection Agency. Report number 12, 1994. [PubMed]
- 12. Medical Research Council. Measles. See http://www.mrc.ac.uk/Achievementsimpact/Storiesofimpact/Measles/index.htm (last checked October 2013)
- 13. Krugman S. Present status of measles and rubella immunization in the United States: a medical progress report. J Pediatr 1971; 78: 1–16 [DOI] [PubMed] [Google Scholar]
- 14. Health Protection Agency. Completed Primary Courses at Two Years of Age: England and Wales, 1966–1977, England only 1978 onwards. See http://www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1195733819251 (2011, last checked 14 October 2013)
- 15. Health Protection Agency. Herd Immunity – Concepts of Control. See www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1279889319696 (last checked 14 October 2013)
- 16. Wakefield AJ, Pittilo RM, Sim R, et al. Evidence of persistent measles virus infection in Crohn’s disease. J Med Virol 1993; 39: 345–353 [DOI] [PubMed] [Google Scholar]
- 17. Wakefield AJ, Murch SH, Anthony A, et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. The Lancet 1998; 351: 637–641 [DOI] [PubMed] [Google Scholar]
- 18. Deer B. How the vaccine crisis was meant to make money. BMJ 2011; 342: 136–142 [DOI] [PubMed] [Google Scholar]
- 19. British United Provident Association. Measles, Mumps and Rubella (MMR) Vaccine. See http://www.bupa.co.uk/individuals/health-information/directory/m/mmr-vaccine (2011, last checked 14 October 2013)
- 20. Health Protection Agency. Confirmed Cases of Measles, Mumps and Rubella 1996--2011. See http://www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1195733833790 (2013, last checked 14 October 2013)
- 21. Health Protection Agency. Vaccine Uptake at All Time High on Merseyside. See http://www.hpa.org.uk/ProductsServices/LocalServices/NorthWest/NorthWestPressReleases/nwest120613merseysidemeaslesvacc/ (last checked 14 October 2013)
- 22. Health Protection Agency. Number of Laboratory Confirmed Measles Cases in England and Wales. See http://www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1223019390211 (2013, last checked 14 October 2013)
- 23. BBC News. Swansea Measles Epidemic Officially Over. See http://www.bbc.co.uk/news/uk-wales-23168519 (2013, last checked 13 January 2014)
- 24. Brown KF, Long SJ, Ramsay M, et al. UK parents’ decision-making about measles-mumps-rubella (MMR) vaccine 10 years after the MMR-autism controversy: a qualitative analysis. J Vaccine 2012; 30: 1855–1864 [DOI] [PubMed] [Google Scholar]
- 25. Shourie S, Jackson C, Cheater FM, et al. A cluster randomized controlled trial of a web based decision aid to support parents’ decision about their child’s Measles Mumps and Rubella (MMR) vaccination. J Vaccine 2013; 31: 6003–6010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chris TB, Samit B. Evolutionary game theory and social learning can determine how vaccine scares unfold. PLoS Comput Biol 2012; 8: e1002452–e1002452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cockman P, Dawson L, Mathur R, et al. Improving MMR vaccination rates: herd immunity is a realistic goal. BMJ 2011; 343: d5703–d5703 [DOI] [PubMed] [Google Scholar]