Abstract
Vascular smooth muscle cells (VSMCs) perform essential smooth muscle contractile and synthetic functions including migration, differentiation and proliferation under physiological and pathological conditions. In response to pathological stimuli, VMSCs undergo phenotypic change resulting in abnormal migration and proliferation, which may contribute to a “pathogenesis-like” atherosclerosis. Intracellular signaling mechanisms governing this phenotypic switch are of great significance not only for better understanding of atherosclerotic plaque formation but also for strategy for pertinent therapeutic remedies. Src Homology 2 Containing Protein Tyrosine Phosphatase 2 (SHP2) is a ubiquitous tyrosine phosphatase containing Src Homology 2 domains which plays major biological functions in response to various growth factors, hormones or cytokines. In particular, SHP2 is implicated in cell signaling pathways controlling cell cycle progression, growth and migration. In this review we will mainly discuss the recent literature demonstrating the role of SHP2 in VSMC migration and proliferation.
Keywords: Src homology 2 containing protein tyrosine phosphatase 2, vascular smooth muscle cells, migration, proliferation
Introduction
Under physiological condition, vascular smooth muscle cells (VSMCs) exist in an organized, differentiated and contractile phenotype to perform contractile and synthetic functions characterized by changes in morphology, proliferation and migration rates. However, in response to pathological stimuli these contractile cells may be switched to a proliferative and migratory phenotype. The ability to shuttle between phenotypes is necessary for wound healing and growth of new vessels in developing tissues. On the other hand, VSMCs may contribute to pathological changes in the vasculature such as atherosclerosis when they are inappropriately stimulated to proliferate and migrate1. A plethora of efforts have been made attempting to elucidate the governing of this phenotypic switching in VSMCs. In particular, a wide variety of growth factors have been identified to participate in the regulation of VSMC proliferation and migration. For instance, VSMCs may migrate and proliferate with a fair degree of predictability in response to platelet-derived growth factor (PDGF)2, 3. However, proliferation and migration can be bolstered or mitigated in VSMCs in the presence of other growth factors or stimuli. Thus the net outcome in proliferation and migration can be drastically different depending on the involvement of distinct signaling pathways4. Therefore a closer scrutiny of the cell signaling mechanisms seems essential in understanding the switch in phenotype for VSMC proliferation and migration. Among the many proteins and cell signaling molecules surfaced over the last decades, Src homology 2 (SH2) containing protein tyrosine phosphatase (PTP) 2 (SH-PTP2) has drawn some heavy attention recently in the regulation of multiple signaling pathways associated with growth and proliferation in a variety of cell types. SH-PTP2 is a member of the non receptor protein tyrosine phosphatase family and will be referred to as SHP2 in this review. SHP2, a 597 amino acid (AA) monomer first identified in human cells in 1992 as a homolog to the Drosophila Corkscrew protein5, acts by targeted dephosphorylation of substrate phosphotyrosine. The gene encoding this protein is found on chromosome 12 band q24.13. Mutations in this gene have been associated with several human genetic diseases such as Noonan syndrome, Leopard syndrome and Juvenile Myelo monocytic Leukemia6. Missense point mutations may result in increased phosphatase activity leading to short stature, facial dysmorphia, skeletal malformation and congenital heart disease in Noonan syndrome7. SHP2 also plays a significant role in intracellular signaling associated with growth factors, receptor tyrosine kinases, integrins, and immunoglobulin receptors in cell cycle, migration, proliferation and apoptosis regulation5, 8.
Structure and function
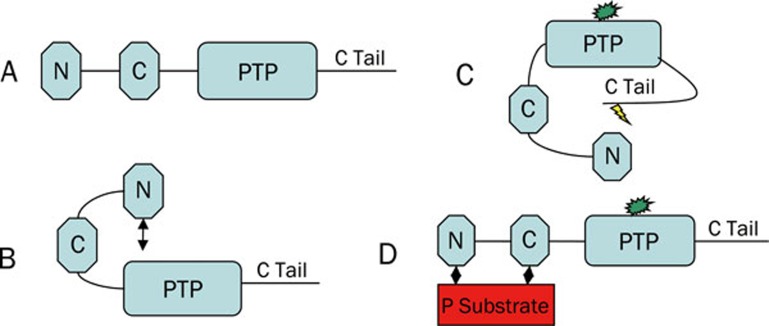
Structurally, SHP2 is characterized by two tandem N terminal SH2 domains, a catalytic PTP domain and a C terminal tail. The two SH2 domains are named N and C, with N being the SH2 domain closer to N terminal. These domains are about 100 AAs in sequence and are found between AAs 6-101 (N-SH2) and 112-211 (C-SH2). The business end of the SHP2 stick, the PTP domain lies between AAs 276-523 and is followed by the C-terminal tail which extends up to AA 5979. To-date, several different clones are available from NCBI ranging from 460 AA in length to the most prevalent 597 AA clone.
SH2 domains are thought to localize SHP2 to phosphorylated tyrosine residues on substrate proteins. Based on chromatography affinity and peptide sequencing findings, Sweeney and colleagues predicted that there are 22 sequences the N-SH2 domain and 11 sequences that C-SH2 domain bind with high affinity10. Lesser binding was observed in 150 and 77 sequences for N and C-SH2s, respectively. While C-SH2 exhibits affinity for (T/V/I)XpY(A/s/t/v)X(I/v/l) sequences, the N-SH2 domain shows affinity for 4 consensus sequences as the following: (i): (I/L/V/m)XpY(T/V/A)X(I/V/L/f); (ii): W(M/T/v)pY(y/r)(I/L)X; (iii): (I/V)XpY(L/M/T)Y(A/P/T/S/g) and (iv): (I/V/L)XpY(F/M)XP. Note that items in parentheses indicate multiple AAs occurring with similar frequency at that location with lowercase letters representing less frequent AAs. In addition, X represents no specificity at that location and pY is phosphorylated tyrosine10. Sequences iii and iv are conserved sequences (commonly observed N-SH2 domain substrates). Actually, binding of sequences i and ii has not been shown to occur naturally.
The PTP domain of SHP2 acts to dephosphorylate the tyrosine residues. PTP activity in SHP2 is negatively regulated primarily by a close association with the N-SH2 domain in the inactive form. Reversible oxidation may also serve as an additional negative regulator of the PTP domain at active serines11. The family of classical PTPs is characterized by the presence of 10 highly conserved motifs in their catalytic domains for structural conformation, substrate interaction and phosphates action. Differences in other AA sequences add another layer of variation thus allowing for more targeted PTP activity. It is believed that SHP2 dephosphorylates substrates in a manner distinctly from other PTPs due to its SH2 localization/targeting domains, and variation from other PTPs in the catalytic domain6. Several studies have examined the SHP2 catalytic domain substrate specificity using capture techniques although little information is available on the precise target sequences of the PTP domain of SHP2.
The C-terminal tail extending from AA 524 through the end is by far the most interesting and functionally elusive aspect of SHP-2. SHP2 possesses a generally positive effect on its substrate as opposed to its sister phosphatase SHP-1 which generally displays a negative effect on its substrate. While this statement may be somewhat too general, it does highlight the power of the C-tail as this is where most of the variations occur between SHP-1 and SHP2 to allow alternate function. For more detailed information regarding possible function of this domain, please see the review by Poole and Jones12. Within the SHP2 C-terminal, there are tyrosine and serine phosphorylation sites, membrane lipid interaction and lipid raft localization sites and proline rich domains (possible SH3 interaction sites)12. When SHP2 is inactive the N-SH2 domain folds back to binds with the PTP sequence sequestering both domains although leaving the C-SH2 domain available for substrate interaction (Figure 1). This is thought to be the primary model of phosphatase regulation. When a phosphorylated substrate contacts the C-SH2 domain, the PTP/N-SH2 interaction is lost and N-SH2 also binds the phosphorylated substrate or another in close proximity13, 14. This allows the PTP domain to execute its phosphatase activity. Another more recent proposed method of activation is that the SHP2 tyrosine phosphorylation sites on the C terminal tail become phosphorylated and bind one or both SH-2 domains thus freeing the PTP domain for activity9. Interestingly, the C terminal 543 tyrosine phosphorylation site is flanked by AAs that match an SH2 conserved affinity sequence. There has been much speculation with regards to how SHP2 activity is regulated and how C terminal phosphorylation affects localization and phosphatase activity of SHP2. SHP2 phosphorylation of tyrosine 542 and 580 has been shown as required for Grb 2 recruitment via its SH2 domain12.
Figure 1.
Possible structural conformations of SHP2. (A) Basic structure; (B) inactive form with N-SH2 and PTP domain interaction; (C) active form after C tail phosphorylation and N-SH2 domain interaction; (D) active form after phosphorylated substrate binding of N and C-SH2 domains.
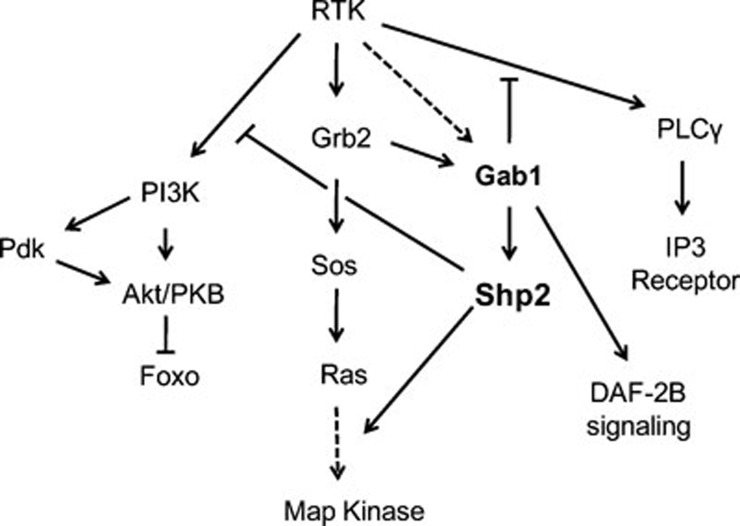
Dephosphorylation of target molecules have potentially stimulatory or inhibitory affects on the overall signal transduction. For instance, phosphorylation at tyrosine 416 on Src kinase increases the kinase activity while phosphorylation at tyrosine 527 decreases the kinase activity. Dephosphorylation at these sites is expected to result in alternate outcomes7. Hence increased SHP2 phosphorylation may either increase or decrease the target signal molecules depending on microenvironment. Furthermore, if the role of SHP2 is to dephosphorylate a protein that inhibits the pathway then the net effect should be stimulatory. On the other hand, dephosphorylation might directly stimulate a substrate by creating a conformational change that opens a hidden binding site upon phosphorylation. The same relationship holds for possible negative regulation. Also, dephosphorylation of ubiquitination sites can positively reinforce expression of proteins that would otherwise be destroyed15. Receptor tyrosine kinases (the class of receptor that insulin growth factor receptor (IGFR), fibroblast growth factor receptor (FGFR), epidermal growth factor receptor (EGFR), and PDGF receptor belong to) have been shown to conduct signal transduction through activation of RAS/MAPK, PI3K/AKT, and PLCγ (Figure 2).
Figure 2.
SHP2 in overall RTK receptor signaling. Adapted from Hopper 200616.
SHP2 and VSMCs
Up-to-date, very few reports can be found on PubMed focusing on SHP2 in VSMCs. The majority of efforts have been engaged towards activation of immune system, control of migration and proliferation associated with cancers and insulin signaling. While all worthwhile endeavors, SHP2 is highly expressed in vasculature that the volume of research in other tissue types seems disproportionate. Here we will highlight signaling pathways where SHP2 has been implicated in VSMCs. In cases when little data are available in VSMCs, the analysis will be augmented with information of SHP2 in that specific pathway observed in other tissues or species.
General expression profiles of SHP2 in VSMCs
SHP2 is expressed widely throughout mammalian tissues although expression levels vary significantly among different tissues, with livers and kidneys displaying the least expression. Using immunohistochemical staining and in situ hybridization techniques, Adachi and coworkers have shown ubiquitous expression of SHP2 in VSMCs17. Seki and colleagues also reported elevated SHP2 expression in thickened intima in balloon-induced tissue remodeling18. Chang and coworkers observed a transient increase in SHP2 levels in medial VSMCs after vascular injury. In addition they also reported that PDGF, basic fibroblast growth factor (bFGF) and nitric oxide (NO) but not Ang II, EGF and IGF-1 increase the SHP2 expression in cultured primary rat VSMC18, 19, 20. Recently, SHP2 expression and phosphorylation were found elevated in older VSMCs compared to the young ones21, indicating a possible role of SHP2 in vascular aging.
SHP2 activity and signal transduction
Growth factors and SHP2
Growth factors such as platelet-derived growth factor (PDGF), epidermal growth factor (EGF), and insulin like growth factor-1 (IGF-1), were involved in smooth muscle cell migration and proliferation by stimulating various signaling mechanisms under physiological and pathological conditions.
PDGF induces SHP2 tyrosine phosphorylation. Tyrosine phosphorylation of SHP2 stimulates catalytic activity. The activated SHP2 binds directly to the activated PDGF receptor at phoshpotyrosine-1009 pY1009 via its N terminal domain and thereby dephosphorylates the receptor or its associated substrates22, 23. On the other hand, SHP2 is also implicated in positive regulation, since tyrosine phosphorylation of SHP2 presents a binding site for the adaptor protein Grb2. Grb2 then mediates Ras activation through complex formation with the nucleotide exchange factor Sos23. In addition SHP2 activity is also involved in phosphatidylinositol 3-kinase independent regulation of cell migration24.
IGF-1 induced smooth muscle cell migration or proliferation is mediated through αVβ3 integrin. IGF-1 stimulates αVβ3 integrin ligand occupancy and phosphorylation, which results in SHP2 recruitment to the plasma membrane. This membrane associated SHP2 is subsequently recruited to Src homology 2 domain-containing protein tyrosine phosphatase substrate-1 resulting in PTP-1 tyrosine phosphorylation25, 26.
SHP-2 is a positive mediator of the mitogenic signal transduction induced by EGF. Tyrosine phosphorylation of the EGFR is followed by the recruitment of various SH2 domain-containing intracellular proteins to the cytoplasmic domain of EGFR. Formation of a Shc-Grb2-sos sevenless complex and the activation of Ras are key events in the initiation of signals through activated EGFR27.
SHP2 and focal adhesion kinase
Focal adhesion kinase (FAK) is prototype for a family of non-receptor protein tyrosine kinase highly expressed in VSMCs28. FAK is strongly activated by integrin, growth factor receptors and G-protein receptor engagement and serves to integrate downstream signals in response to a variety of ligands and agonists29. In particular, FAK is an intermediate signal in VSMC migration and proliferation30. Fibroblast SHP2 is required for cell spreading, migration and focal adhesion. FAK and SHP2-deficient cells exhibited similar phenotypes, suggesting that the turnover of focal adhesion sites required in migration is dependent on SHP2 action through cyclic activation and deactivation of FAK. In human VSMCs, SHP2 directly interacts with FAK by dephosphorylating FAK at Y397 and thereby regulating VSMC's focal adhesion and migration31, 32.
SHP2 and Rho
Rho functions as a molecular switch under the tight control of regulatory proteins that cycle between the active GTP-bound and inactive GDP-bound forms33, 34. In middle passage rat VSMCs, peroxisome proliferator-activated receptors (PPAR) ligands suppresses Rho activity by up-regulating cytoplasmic SHP2 where it binds and inactivates VAV, a GTP/GDP exchange factor for Rho kinase21, 35. In primary VSMCs, NO upregulates SHP2 expression (albeit not necessarily phosphorylation) and cell migration36, 37. When SHP2 was attenuated via an antisense oligonucleotide, the NO-induced motility was decreased, possibly due to Rho A-dependent change in cell motility37. It was also shown that the NO-induced cell motility is largely due to the Gab1/SHP2 interaction. This raises the question regarding the precise nature of the Gab1/VAV interaction in proliferation and migration. When VSMCs are dedifferentiated, NO is capable of reducing motility38 and blocking the increased motility in response to PDGF treatment. However, after an extended period of culture in dedifferentiated cells with insulin, a Gab1/SHP2 interaction may lead to a decrease in Rho A abundance en route to the increased motility39. Rho is thought to be responsible for SHPS-1 phosphorylation which leads to SHP2 recruitment40. Depending on environment, Rho can be either up- or down-stream of SHP2.
SHP2 and JAK/STAT
The JAK/STAT pathway plays a rather significant role in vascular smooth muscle cell proliferation and migration induced by angiotensin II. In response to angiotensin II the JAK/STAT signaling in VSMCs involves the tyrosine phosphorylation and subsequent activation of JAK tyrosine kinases, which in turn phosphorylates STATs. The phosphorylated STAT translocates to nucleus as dimers and binds to specific response elements in gene promoters and direct transcription41. In middle passage rat VSMCs, SHP2 phosphorylation and localization on AT1 receptor are necessary for the JAK2/AT1 interaction and modulation of JAK2 downstream signaling42. On contrary Doan and colleagues have reported SHP2 as a negative regulator of angiotensin II signaling, where phosphorylated SHP2 was found to inhibit c-Src catalytic activity by dephosphorylating a positive regulatory tyrosine 418 within the Src kinase domain43. High glucose conditions augment the Ang II-induced ROS production, VSMC proliferation and tyrosine phosphorylation of JAK2 via the polyol pathway. The polyol pathway may in turn activate PKCβ2 and NADPH oxidase to generate more ROS. ROS is known to regulate the activity of SHP2. The altered state of SHP2 hinders its ability to interact with JAK244. In hyperglycemic states, SHP2 levels and activity display a two-fold increase in VSMCs compared with the normal glucose environment45.
SHP2 and PI3K/AKT
PI3-K is composed of a catalytic p110 subunit and a regulatory p85 subunit. PI3-K phosphorylates membrane glycerophospholipid phosphatidylinositol 4,5 biphosphate resulting in production of phosphatidylinositol 3,4,5 trisphosphate (PIP3) and phosphatidylinositol 3,4 trisphosphate (PIP2). PI3-K is an upstream signaling molecule of Akt which is also important in the maintenance of VSMC differentiation. SHP2 interacts with the p85 subunit of PI3-K and is a required step for IGF-1-induced PI3-K activation en route to cell migration and phosphorylation of Akt in middle passage VSMCs25. In EGF- and Ang II-treated VSMCs, GAB 1 is rapidly phosphorylated and associates with the p85 subunit of PI3K and leads to Akt activation. When SHP2 is activated by resveratrol (compound from grape skin), it mitigates the GAB1/PI3K interaction and attenuates Akt activation46.
SHP2 and integrins
SHP2 recruitment to the plasma membrane is dependent on αVβ3 integrin occupancy and phosphorylation. This SHP2 recruitment is also dependent on an insulin receptor substrate (IRS) family protein DAK1 which serves as a docking protein between SHP2 and the β3 subunit of the integrin heterodimer47. Once at the plasma membrane, it can be recruited to the SHPS-1, IRS-1, or other substrates. Transforming growth factor (TGF)β stimulates the upregulation of αVβ3 integrins in 2-6 passage VSMCs. TGFβ is a positive proliferation effector of VSMC present following vascular injury48. αVβ3 integrins bind a non collagen substrate and are upregulated after oxidative damage in high passage proliferative cells20. Taken together, SHP2 recruitment to the plasma membrane by this specific integrin could be a primary mechanism priming VSMC migration and proliferation.
SHP2 and MAPK
SHP2 is tied to phenotype dependent response to IGF-1 in VSMCs. Upon IGF-1 stimulation, SHP2 dephosphorylated IRS-1 at Tyr-895 resulting in interrupted IRS-1/Grb 2/Sos signaling to Ras and subsequently ERK/p38 MAPK. Conversely after multiple passages in culture this negative regulation was silent and IGF-1 treatment led to IRS-1/Grb 2/Sos activation of Ras and subsequently of ERK/p38 MAPKs4. In middle passage VSMCs the GAB1 phosphorylation in response to PDGF was at least somewhat dependent on PKC and PLCγ49. IGF-1-dependent Shc phosphorylation is required for MAPK activation and cell proliferation. Recruitment of SHP2 and Shc to SHPS-1 in response to IGF-1 are both required for Shc phosphorylation and therefore necessary for mediating IGF-1 dependent mitogenic signaling in SMCs50. On a separate note, unsaturated lysophosphatidic acid (LPA) is capable of transforming the primary differentiated VSMCs into dedifferentiated VSMCs via ERK and p38 MAPKs51. How does this unsaturated LPA affect SHP2? In Rat-1 cells, LPA was shown to increase SHP2 association with SHPS-1, representing a possible mechanism for VSMC dedifferentiation. The SHP2/SHPS-1 interaction then appears to bring on MAPK activation at least in response to LPA and IGF-1. SHPS-1 is phosphorylated in the LPA and IGF-1 signaling40.
Challenge in shp2 signaling in VSMCs
SHP2 exerts negative effects on Akt in the EGF and Ang II signaling pathways whereas it elicits positive effects on MAPK in the IGF-1 and LPA signaling cascades. GAB is capable of recruiting SHP2 in both instances. In response to EGF and Ang II, GAB works in concert with the p85 subunit of PI3K. On the other side of the coin, GAB also associates with Grb 2 and the RTK signaling complex upon IGF-1 stimulation. In addition, factors favoring VSMC proliferation and migration seem to contribute to SHP-2 localization at the plasma membrane and its association with SHPS-1 or other substrates, leading to subsequent MAPK activation. In increased migration due to SHP2 negative regulation of Rho, it is unclear where this takes place but again it looks as if there is SHP2-GAB interaction involved. Given that protein tyrosine phosphatase activity is often measured using dephosphorylation of p-nitrophenyl phosphate to offer an overall cellular phosphatase activity, it is often difficult to attribute the activity to a single phosphatase. Even with attempts being made to inhibit other phosphatases, the control is never adequate for all known dephosphorylation enzymes. Furthermore, it is not entirely clear if phosphorylation of C-terminal residues is a necessary step for phosphatase activity (possibly activated through SH2 domain interactions with substrate proteins). Further study with phospho residues in the C-tail of SHP2 as the marker for an active enzyme is warranted. It is difficult to sift through the seemingly contradictory evidence with regards to SHP2 activity and expression in VSMC action. Variables like cell type, cell age, growth factor employed, degree of confluence and time between treatment and assay must be considered in order to get a better picture of the vascular effect of SHP2. The complexity of SHP2 regulation and action further add to such technical difficulties.
With many possible catalytic, SH2 domain, and C tail substrates and regulators, SHP2 is clearly an important regulator of intracellular signaling. Co-precipitation assays and immunohistochemistry for cellular localization of molecules that alter phosphorylation states may also be used to determine possible interaction and site of action. Many further questions regarding the action of SHP2 remain. As a target for drug development, SHP2 is attractive because of its multiple sites and pathways for regulation. If the utility of the C terminal and SH2 domains can be better defined, possible antagonists or agonists for those specific regions may allow normal SHP2 action in a given pathway but “loss or gain of function” in another pathway. For instance if the section of the C tail responsible for phosphorylation and interaction with the SH2 domain is inactivated, one could limit SHP2 activity to targeted N and C-SH2 domain substrate interaction activation. Similarly, C terminal lipid raft localization motifs or the C-SH2 domain could be selectively inhibited to limit unique SHP2 action while preserving others. We should emphasize that any application will require a better understanding of the SH2/c-tail relationships.
In cases where SHP2 binding to a certain substrate is required for signal transduction, it is presumed that this signal is dependent on SHP2 phosphatase action on that substrate or one in the same complex. While some studies do connect SHP2 association with substrate protein and dephosphorylation of that or another substrate, most studies stop short. This may create a scenario that in cases where SHP2 is localized to its substrate proteins, it may actually be sequestered from other possible substrates.
Acknowledgments
We sincerely express our apology to those authors whose important work cannot be cited here due to space limitation.
References
- Lundberg MS, Crow MT. Age-related changes in the signaling and function of vascular smooth muscle cells. Exp Gerontol. 1999;34:549–57. doi: 10.1016/s0531-5565(99)00036-4. [DOI] [PubMed] [Google Scholar]
- Bornfeldt KE, Raines EW, Nakano T, Graves LM, Krebs EG, Ross R. Insulin-like growth factor-I and platelet-derived growth factor-BB induce directed migration of human arterial smooth muscle cells via signaling pathways that are distinct from those of proliferation. J Clin Invest. 1994;93:1266–74. doi: 10.1172/JCI117081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes AD, Clunn GF, Refson J, Demoliou-Mason C. Platelet-derived growth factor (PDGF): actions and mechanisms in vascular smooth muscle. Gen Pharmacol. 1996;27:1079–89. doi: 10.1016/s0306-3623(96)00060-2. [DOI] [PubMed] [Google Scholar]
- Hayashi K, Shibata K, Morita T, Iwasaki K, Watanabe M, Sobue K. Insulin receptor substrate-1/SHP-2 interaction, a phenotype-dependent switching machinery of insulin-like growth factor-I signaling in vascular smooth muscle cells. J Biol Chem. 2004;279:40807–18. doi: 10.1074/jbc.M405100200. [DOI] [PubMed] [Google Scholar]
- Freeman RM Jr, Plutzky J, Neel BG. Identification of a human src homology 2-containing protein-tyrosine-phosphatase: a putative homolog of Drosophila corkscrew. Proc Natl Acad Sci USA. 1992;89:11239–43. doi: 10.1073/pnas.89.23.11239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen JN, Mortensen OH, Peters GH, Drake PG, Iversen LF, Olsen OH, et al. Structural and evolutionary relationships among protein tyrosine phosphatase domains. Mol Cell Biol. 2001;21:7117–36. doi: 10.1128/MCB.21.21.7117-7136.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roskoski R Jr. Src kinase regulation by phosphorylation and dephosphorylation. Biochem Biophys Res Commun. 2005;331:1–14. doi: 10.1016/j.bbrc.2005.03.012. [DOI] [PubMed] [Google Scholar]
- Bennett AM, Tang TL, Sugimoto S, Walsh CT, Neel BG. Protein-tyrosine-phosphatase SHPTP2 couples platelet-derived growth factor receptor beta to Ras. Proc Natl Acad Sci USA. 1994;91:7335–9. doi: 10.1073/pnas.91.15.7335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neel BG, Gu H, Pao L. The 'Shp'ing news: SH2 domain-containing tyrosine phosphatases in cell signaling. Trends Biochem Sci. 2003;28:284–93. doi: 10.1016/S0968-0004(03)00091-4. [DOI] [PubMed] [Google Scholar]
- Sweeney MC, Wavreille AS, Park J, Butchar JP, Tridandapani S, Pei D. Decoding protein-protein interactions through combinatorial chemistry: sequence specificity of SHP-1, SHP-2, and SHIP SH2 domains. Biochemistry. 2005;44:14932–47. doi: 10.1021/bi051408h. [DOI] [PubMed] [Google Scholar]
- Kwon J, Qu CK, Maeng JS, Falahati R, Lee C, Williams MS. Receptor-stimulated oxidation of SHP-2 promotes T-cell adhesion through SLP-76-ADAP. Embo J. 2005;24:2331–41. doi: 10.1038/sj.emboj.7600706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poole AW, Jones ML. A SHPing tale: perspectives on the regulation of SHP-1 and SHP-2 tyrosine phosphatases by the C-terminal tail. Cell Signal. 2005;17:1323–32. doi: 10.1016/j.cellsig.2005.05.016. [DOI] [PubMed] [Google Scholar]
- Pluskey S, Wandless TJ, Walsh CT, Shoelson SE. Potent stimulation of SH-PTP2 phosphatase activity by simultaneous occupancy of both SH2 domains. J Biol Chem. 1995;270:2897–900. doi: 10.1074/jbc.270.7.2897. [DOI] [PubMed] [Google Scholar]
- Maheshwari M, Belmont J, Fernbach S, Ho T, Molinari L, Yakub I, et al. PTPN11 mutations in Noonan syndrome type I: detection of recurrent mutations in exons 3 and 13. Hum Mutat. 2002;20:298–304. doi: 10.1002/humu.10129. [DOI] [PubMed] [Google Scholar]
- Ali S, Nouhi Z, Chughtai N, Ali S. SHP-2 regulates SOCS-1-mediated Janus kinase-2 ubiquitination/degradation downstream of the prolactin receptor. J Biol Chem. 2003;278:52021–31. doi: 10.1074/jbc.M306758200. [DOI] [PubMed] [Google Scholar]
- Hopper NA. The adaptor protein soc-1/Gab1 modifies growth factor receptor output in Caenorhabditis elegans. Genetics. 2006;173:163–75. doi: 10.1534/genetics.106.055822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adachi M, Iwaki H, Shindoh M, Akao Y, Hachiya T, Ikeda M, et al. Predominant expression of the src homology 2-containing tyrosine phosphatase protein SHP2 in vascular smooth muscle cells. Virchows Arch. 1997;430:321–5. doi: 10.1007/BF01092755. [DOI] [PubMed] [Google Scholar]
- Seki N, Hashimoto N, Suzuki Y, Mori S, Amano K, Saito Y. Role of SRC homology 2-containing tyrosine phosphatase 2 on proliferation of rat smooth muscle cells. Arterioscler Thromb Vasc Biol. 2002;22:1081–5. doi: 10.1161/01.atv.0000022878.37277.ec. [DOI] [PubMed] [Google Scholar]
- Chang Y, Zhuang D, Zhang C, Hassid A. Increase of PTP levels in vascular injury and in cultured aortic smooth muscle cells treated with specific growth factors. Am J Physiol Heart Circ Physiol. 2004;287:H2201–8. doi: 10.1152/ajpheart.00520.2004. [DOI] [PubMed] [Google Scholar]
- Wilson E, Parrish AR, Bral CM, Williams ES, Ramos KS. Collagen suppresses the proliferative phenotype of allylamine-injured vascular smooth muscle cells. Atherosclerosis. 2002;162:289–97. doi: 10.1016/s0021-9150(01)00718-3. [DOI] [PubMed] [Google Scholar]
- Rice KM, Kinnard RS, Wright GL, Blough ER. Aging alters vascular mechanotransduction: pressure-induced regulation of p70S6k in the rat aorta. Mech Ageing Dev. 2005;126:1213–22. doi: 10.1016/j.mad.2005.07.001. [DOI] [PubMed] [Google Scholar]
- Klinghoffer RA, Kazlauskas A. Identification of a putative Syp substrate, the PDGF beta receptor. J Biol Chem. 1995;270:22208–17. doi: 10.1074/jbc.270.38.22208. [DOI] [PubMed] [Google Scholar]
- Li W, Nishimura R, Kashishian A, Batzer AG, Kim WJ, Cooper JA, et al. A new function for a phosphotyrosine phosphatase: linking GRB2-Sos to a receptor tyrosine kinase. Mol Cell Biol. 1994;14:509–17. doi: 10.1128/mcb.14.1.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi JH, Ito N, Claesson-Welsh L. Tyrosine phosphatase SHP-2 is involved in regulation of platelet-derived growth factor-induced migration. J Biol Chem. 1999;274:14455–63. doi: 10.1074/jbc.274.20.14455. [DOI] [PubMed] [Google Scholar]
- Kwon M, Ling Y, Maile LA, Badley-Clark J, Clemmons DR. Recruitment of the tyrosine phosphatase Src homology 2 domain tyrosine phosphatase-2 to the p85 subunit of phosphatidylinositol-3 (PI-3) kinase is required for insulin-like growth factor-I-dependent PI-3 kinase activation in smooth muscle cells. Endocrinology. 2006;147:1458–65. doi: 10.1210/en.2005-1115. [DOI] [PubMed] [Google Scholar]
- Ling Y, Maile LA, Clemmons DR. Tyrosine phosphorylation of the beta3-subunit of the alphaVbeta3 integrin is required for embrane association of the tyrosine phosphatase SHP-2 and its further recruitment to the insulin-like growth factor I receptor. Mol Endocrinol. 2003;17:1824–33. doi: 10.1210/me.2003-0143. [DOI] [PubMed] [Google Scholar]
- Montagner A, Yart A, Dance M, Perret B, Salles JP, Raynal P. A novel role for Gab1 and SHP2 in epidermal growth factor-induced Ras activation. J Biol Chem. 2005;280:5350–60. doi: 10.1074/jbc.M410012200. [DOI] [PubMed] [Google Scholar]
- Polte TR, Naftilan AJ, Hanks SK. Focal adhesion kinase is abundant in developing blood vessels and elevation of its phosphotyrosine content in vascular smooth muscle cells is a rapid response to angiotensin II. J Cell Biochem. 1994;55:106–19. doi: 10.1002/jcb.240550113. [DOI] [PubMed] [Google Scholar]
- Mitra SK, Hanson DA, Schlaepfer DD. Focal adhesion kinase: in command and control of cell motility. Nat Rev Mol Cell Biol. 2005;6:56–68. doi: 10.1038/nrm1549. [DOI] [PubMed] [Google Scholar]
- Keffel S, Alexandrov A, Goepel M, Michel MC. alpha(1)-adrenoceptor subtypes differentially couple to growth promotion and inhibition in Chinese hamster ovary cells. Biochem Biophys Res Commun. 2000;272:906–11. doi: 10.1006/bbrc.2000.2850. [DOI] [PubMed] [Google Scholar]
- Yu DH, Qu CK, Henegariu O, Lu X, Feng GS. Protein-tyrosine phosphatase Shp-2 regulates cell spreading, migration, and focal adhesion. J Biol Chem. 1998;273:21125–31. doi: 10.1074/jbc.273.33.21125. [DOI] [PubMed] [Google Scholar]
- von Wichert G, Haimovich B, Feng GS, Sheetz MP. Force-dependent integrin-cytoskeleton linkage formation requires downregulation of focal complex dynamics by Shp2. Embo J. 2003;22:5023–35. doi: 10.1093/emboj/cdg492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burridge K, Wennerberg K. Rho and Rac take center stage. Cell. 2004;116:167–79. doi: 10.1016/s0092-8674(04)00003-0. [DOI] [PubMed] [Google Scholar]
- Etienne-Manneville S, Hall A. Rho GTPases in cell biology. Nature. 2002;420:629–35. doi: 10.1038/nature01148. [DOI] [PubMed] [Google Scholar]
- Wakino S, Hayashi K, Kanda T, Tatematsu S, Homma K, Yoshioka K, et al. Peroxisome proliferator-activated receptor gamma ligands inhibit Rho/Rho kinase pathway by inducing protein tyrosine phosphatase SHP-2. Circ Res. 2004;95:e45–55. doi: 10.1161/01.RES.0000142313.68389.92. [DOI] [PubMed] [Google Scholar]
- Brown C, Pan X, Hassid A. Nitric oxide and C-type atrial natriuretic peptide stimulate primary aortic smooth muscle cell migration via a cGMP-dependent mechanism: relationship to microfilament dissociation and altered cell morphology. Circ Res. 1999;84:655–67. doi: 10.1161/01.res.84.6.655. [DOI] [PubMed] [Google Scholar]
- Chang Y, Ceacareanu B, Dixit M, Sreejayan N, Hassid A. Nitric oxide-induced motility in aortic smooth muscle cells: role of protein tyrosine phosphatase SHP-2 and GTP-binding protein Rho. Circ Res. 2002;91:390–7. doi: 10.1161/01.res.0000033524.92083.64. [DOI] [PubMed] [Google Scholar]
- Sarkar R, Meinberg EG, Stanley JC, Gordon D, Webb RC. Nitric oxide reversibly inhibits the migration of cultured vascular smooth muscle cells. Circ Res. 1996;78:225–30. doi: 10.1161/01.res.78.2.225. [DOI] [PubMed] [Google Scholar]
- Dixit M, Zhuang D, Ceacareanu B, Hassid A. Treatment with insulin uncovers the motogenic capacity of nitric oxide in aortic smooth muscle cells: dependence on Gab1 and Gab1-SHP2 association. Circ Res. 2003;93:e113–23. doi: 10.1161/01.RES.0000100391.98425.BB. [DOI] [PubMed] [Google Scholar]
- Takeda H, Matozaki T, Fujioka Y, Takada T, Noguchi T, Yamao T, et al. Lysophosphatidic acid-induced association of SHP-2 with SHPS-1: roles of RHO, FAK, and a SRC family kinase. Oncogene. 1998;16:3019–27. doi: 10.1038/sj.onc.1201839. [DOI] [PubMed] [Google Scholar]
- Schindler C, Darnell JE., Jr Transcriptional responses to polypeptide ligands: the JAK-STAT pathway. Annu Rev Biochem. 1995;64:621–51. doi: 10.1146/annurev.bi.64.070195.003201. [DOI] [PubMed] [Google Scholar]
- Marrero MB, Venema VJ, Ju H, Eaton DC, Venema RC. Regulation of angiotensin II-induced JAK2 tyrosine phosphorylation: roles of SHP-1 and SHP-2. Am J Physiol. 1998;275:C1216–23. doi: 10.1152/ajpcell.1998.275.5.C1216. [DOI] [PubMed] [Google Scholar]
- Doan T, Farmer P, Cooney T, Ali MS. Selective down-regulation of angiotensin II receptor type 1A signaling by protein tyrosine phosphatase SHP-2 in vascular smooth muscle cells. Cell Signal. 2004;16:301–11. doi: 10.1016/j.cellsig.2003.08.001. [DOI] [PubMed] [Google Scholar]
- Shaw S, Wang X, Redd H, Alexander GD, Isales CM, Marrero MB. High glucose augments the angiotensin II-induced activation of JAK2 in vascular smooth muscle cells via the polyol pathway. J Biol Chem. 2003;278:30634–41. doi: 10.1074/jbc.M305008200. [DOI] [PubMed] [Google Scholar]
- Amiri F, Venema VJ, Wang X, Ju H, Venema RC, Marrero MB. Hyperglycemia enhances angiotensin II-induced janus-activated kinase/STAT signaling in vascular smooth muscle cells. J Biol Chem. 1999;274:32382–6. doi: 10.1074/jbc.274.45.32382. [DOI] [PubMed] [Google Scholar]
- Haider UG, Roos TU, Kontaridis MI, Neel BG, Sorescu D, Griendling KK, et al. Resveratrol inhibits angiotensin II- and epidermal growth factor-mediated Akt activation: role of Gab1 and Shp2. Mol Pharmacol. 2005;68:41–8. doi: 10.1124/mol.104.005421. [DOI] [PubMed] [Google Scholar]
- Ling Y, Maile LA, Badley-Clarke J, Clemmons DR. DOK1 mediates SHP-2 binding to the alphaVbeta3 integrin and thereby regulates insulin-like growth factor I signaling in cultured vascular smooth muscle cells. J Biol Chem. 2005;280:3151–8. doi: 10.1074/jbc.M411035200. [DOI] [PubMed] [Google Scholar]
- Li JM, Fan LM, Shah A, Brooks G. Targeting alphavbeta3 and alpha5beta1 for gene delivery to proliferating VSMCs: synergistic effect of TGF-beta1. Am J Physiol Heart Circ Physiol. 2003;285:H1123–31. doi: 10.1152/ajpheart.00103.2003. [DOI] [PubMed] [Google Scholar]
- Saito Y, Hojo Y, Tanimoto T, Abe J, Berk BC. Protein kinase C-alpha and protein kinase C-epsilon are required for Grb2-associated binder-1 tyrosine phosphorylation in response to platelet-derived growth factor. J Biol Chem. 2002;277:23216–22. doi: 10.1074/jbc.M200605200. [DOI] [PubMed] [Google Scholar]
- Ling Y, Maile LA, Lieskovska J, Badley-Clarke J, Clemmons DR. Role of SHPS-1 in the regulation of insulin-like growth factor I-stimulated Shc and mitogen-activated protein kinase activation in vascular smooth muscle cells. Mol Biol Cell. 2005;16:3353–64. doi: 10.1091/mbc.E04-10-0918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi K, Takahashi M, Nishida W, Yoshida K, Ohkawa Y, Kitabatake A, et al. Phenotypic modulation of vascular smooth muscle cells induced by unsaturated lysophosphatidic acids. Circ Res. 2001;89:251–8. doi: 10.1161/hh1501.094265. [DOI] [PubMed] [Google Scholar]