Abstract
The PREDIMED (Prevención con Dieta Mediterránea) study was designed to assess the long-term effects of the Mediterranean diet (MeDiet) without any energy restriction on incident cardiovascular disease (CVD) as a multicenter, randomized, primary prevention trial in individuals at high risk. Participants were randomly assigned to 3 diet groups: 1) MeDiet supplemented with extra-virgin olive oil (EVOO); 2) MeDiet supplemented with nuts; and 3) control diet (advice on a low-fat diet). After 4.8 y, 288 major CVD events occurred in 7447 participants; crude hazard ratios were 0.70 (95% CI: 0.53, 0.91) for the MeDiet + EVOO and 0.70 (95% CI: 0.53, 0.94) for the MeDiet + nuts compared with the control group. Respective hazard ratios for incident diabetes (273 cases) among 3541 participants without diabetes were 0.60 (95% CI: 0.43, 0.85) and 0.82 (95% CI: 0.61, 1.10) compared with the control group. After 1-y follow-up, participants in the MeDiet + nuts group showed a significant 13.7% reduction in prevalence of metabolic syndrome compared with reductions of 6.7% and 2.0% in the MeDiet + EVOO and control groups, respectively. Analyses of intermediate markers of cardiovascular risk demonstrated beneficial effects of the MeDiets on blood pressure, lipid profiles, lipoprotein particles, inflammation, oxidative stress, and carotid atherosclerosis, as well as on the expression of proatherogenic genes involved in vascular events and thrombosis. Nutritional genomics studies demonstrated interactions between a MeDiet and cyclooxygenase-2 (COX-2), interleukin-6 (IL-6), apolipoprotein A2 (APOA2), cholesteryl ester transfer protein plasma (CETP), and transcription factor 7-like 2 (TCF7L2) gene polymorphisms. The PREDIMED study results demonstrate that a high-unsaturated fat and antioxidant-rich dietary pattern such as the MeDiet is a useful tool in the prevention of CVD.
Introduction
Cardiovascular diseases (CVDs) are the most important threat for population health in the 21st century (1). Healthy lifestyles and diets at younger and middle ages are key factors for a life free of chronic diseases at later ages. It follows that CVD prevention through diet and lifestyle is a public health priority. Because diet appears to be particularly relevant in CVD prevention, assessment of the “diet-heart hypothesis” was actively investigated in nutritional epidemiology during the past 50 y (2). In this context, analysis of food patterns, rather than single nutrients and foods, is the ideal approach to examine the effects of the overall diet with the synergistic interaction of its food and nutrient components (3).
Many nutritional epidemiology studies assessing the diet-heart hypothesis used intermediate biomarkers (reductions in blood pressure, cholesterol, inflammatory molecules, or other biomarkers) as a proxy for CVD risk. This approach could be flawed for several reasons. First, multiple pathways lead from diet to CVD, thus negating a high value of changes in single biomarkers. Second, the induction period can be variable for the different pathways, limiting the possibility of assessing multiple biomarker combinations at any time point. Third, unknown pathways might account for a substantial proportion of CVD. Consequently, the best approach to investigate the diet-heart hypothesis is to use hard clinical endpoints. A number of epidemiologic studies showed that overall dietary patterns can improve health and prevent CVD to a greater extent than isolated foods or nutrients (3, 4). However, most studies have been observational, and thus causal inference is problematic because of residual confounding and other sources of bias. Thus, large randomized trials using food patterns and assessing clinical endpoints are needed.
One food pattern reputed for its beneficial health effects is the Mediterranean diet (MeDiet)12; the traditional dietary pattern followed by Mediterranean populations in the early 1960s) (2–8). It is characterized by the following: 1) abundant use of olive oil; 2) high consumption of plant foods (fruits, vegetables, legumes, cereals, nuts, and seeds); 3) frequent but moderate intake of wine (especially red wine) with meals; 4) moderate consumption of fish, seafood, fermented dairy products (yogurt and cheese), poultry, and eggs; and 5) low consumption of red and processed meat and sweets.
The epidemiologic evidence on the CVD protection afforded by adherence to the MeDiet is strong. A systematic review of 32 candidate dietary factors associated with coronary heart disease ranked the MeDiet first as the most likely dietary model to provide causal protection (6), and there is sound biologic plausibility for this effect (7). A meta-analysis of observational studies (8) found strong evidence to support a beneficial effect of the MeDiet on CVD. In relation to incidence of fatal and nonfatal CVD, the analysis of 8 cohorts totaling 534,064 individuals showed a 10% reduction associated with a 2-point increase in a 9-point score of adherence to the MeDiet. After this meta-analysis, the results of 7 additional prospective studies were published up to October 2013 (9–15). These new studies are shown in Table 1. We updated this meta-analysis by using the same selection criteria and methods of Sofi et al. (8). When the 7 new studies were added to the previous meta-analysis and overlapping data were excluded, a new random-effect meta-analysis with 16 estimates showed that each 2-point increment in a 0- to 9-point score of adherence to the MeDiet was associated with a 10% relative reduction in CVD (risk ratio: 0.90; 95% CI: 0.86, 0.94). After removing studies that only assessed fatal CVD (10, 14, 16), the inverse association became stronger (risk ratio: 0.87; 95% CI: 0.85, 0.90), with no evidence of heterogeneity (17).
TABLE 1.
Recent observational studies on adherence to the Mediterranean diet and cardiovascular disease1
| Study | Country | Sample size | Outcome | Events | Comment |
| Dilis et al., 2012 (12) | Greece | 23,929 | CHD incidence and death from CHD | 636 CHD events and 240 CHD deaths | There was a stronger inverse association for mortality than for incidence. |
| Tognon et al., 2012 (13) | Sweden | 77,151 | CVD death | 680 deaths | The inverse association was only significant among women. Effect of the dietary pattern (only present among women) was smaller than in studies conducted in Mediterranean countries. |
| Gardener et al., 2011 (14) | United States | 2568 | Stroke, myocardial infarction, and CVD death | 518 events | In a multiethnic population, a dietary pattern resembling the Mediterranean diet was protective against the combined outcome of ischemic stroke, myocardial infarction, and vascular death. |
| Misirli et al., 2012 (15) | Greece | 23,601 | Stroke | 395 incident cases and 196 stroke deaths | Inverse trends were stronger with respect to ischemic rather than hemorrhagic stroke. |
| Hoevenaar-Blom et al., 2012 (16) | The Netherlands | 40,011 | Fatal and nonfatal CVD events | 4881 events, including 487 CVD deaths | There were significant inverse linear associations for fatal CVD, total CVD, myocardial infarction, and stroke. |
| Menotti et al., 2012 (17) | Italy | 1139 | CHD death | 162 CHD deaths | There was an inverse association between an index of adequacy to the Mediterranean diet and total mortality in a male cohort. |
| Tognon et al., 2013 (18) | Denmark | 1849 | Fatal and nonfatal CVD events | 755 CVD events and 223 CVD deaths | Higher adherence to a Mediterranean dietary score was inversely associated with CVD and myocardial infarction but not with stroke. |
Description of observational studies recently published but not included in the 2010 meta-analysis by Sofi et al. (8). CHD, coronary heart disease; CVD, cardiovascular disease.
The Lyon Diet Heart study, a landmark trial conducted in survivors of a previous myocardial infarction (i.e., a secondary prevention trial), tested a MeDiet enriched with α-linolenic acid but not olive oil vs. a control diet and observed a strong protection against recurrent coronary heart disease (18).
We designed a large-scale primary prevention feeding trial, the PREDIMED (Prevención con Dieta Mediterránea) study, with the hypothesis that the MeDiet would be superior to a low-fat diet for CVD protection (19). In this review, we succinctly describe the design of the PREDIMED study and present its main published results relating to CVD up to 30 October 2013.
Current Status of Knowledge: The PREDIMED Study
Design and implementation.
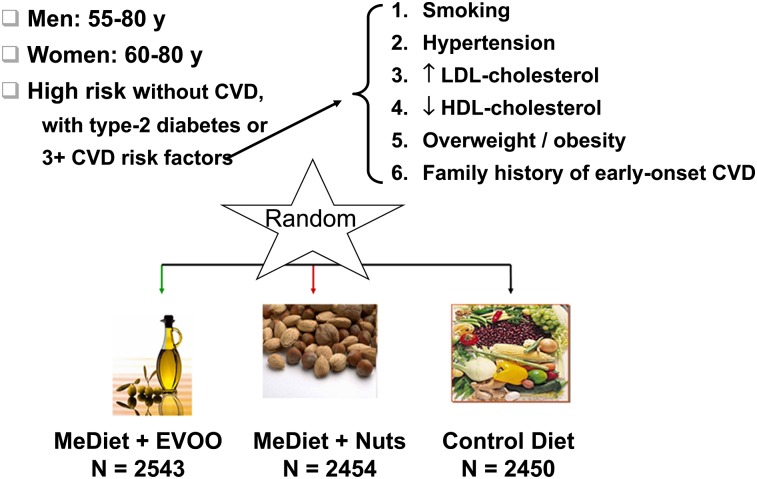
The PREDIMED study was designed to assess the long-term effects of the MeDiet on incident CVD in men and women at high cardiovascular risk. PREDIMED is a multicenter, randomized, nutritional intervention trial for the primary prevention of CVD performed in Spain from 2003 to 2011. The study was funded by the official Spanish agency for scientific research, Instituto de Salud Carlos III, and food industries donated the key foods used in the study. Full details of the study protocol have been described previously (19). Candidates were selected from primary care facilities affiliated with 11 recruiting sites and were at high risk of CVD but had no clinical disease at enrollment. Criteria for recruitment were age of 55–80 y and the presence of diabetes or ≥3 risk factors (smoking, overweight or obesity, hypertension, dyslipidemia, and family history of early-onset CVD )(Fig. 1). Participants were randomly assigned into 1 of 3 interventions: 1) MeDiet supplemented with extra-virgin olive oil (EVOO); 2) MeDiet supplemented with nuts; and 3) control diet (advice on a low-fat diet). Thus, the 2 MeDiet interventions were high vegetable–fat dietary patterns.
FIGURE 1.
Design of the PREDIMED (Prevención con Dieta Mediterránea) study. CVD, cardiovascular disease; EVOO, extra-virgin olive oil; MeDiet, Mediterranean diet.
The PREDIMED intervention was delivered by registered dietitians. Throughout the study, participants attended quarterly individual visits and group sessions in which they were instructed to follow the allocated diet. In the group sessions, participants received written material with information on key Mediterranean foods and seasonal shopping lists, menus, and recipes for 1 wk. Those allocated into the corresponding MeDiet groups were given free allocations of EVOO (1 L/wk, including a minimum of 50 mL/d for participants and the rest for family needs) or mixed nuts (30 g/d: 15 g of walnuts, 7.5 g of almonds, and 7.5 g of hazelnuts plus extra allocations for the family), whereas participants in the control diet group received nonfood gifts. The diets were energy unrestricted, and no increase in physical activity was promoted.
Dietitians used a specific tool to both assess actual adherence to the MeDiet and enhance future adherence: a validated 14-point MeDiet score (20) (Table 2). Additional information was collected yearly on lifestyle, habitual food consumption with a validated FFQ covering 137 foods, physical activity, health status, and medication changes. Anthropometric and blood pressure measurements and an electrocardiogram were taken yearly. Fasting blood and spot urine samples were obtained, and serum, plasma, and DNA samples were saved. Objective biomarkers of adherence to the supplemental foods (urinary hydroxytirosol as a marker of EVOO consumption and plasma α-linolenic acid as a marker of walnut consumption) were determined in random subsamples.
TABLE 2.
Fourteen-point quantitative score of adherence to the Mediterranean diet
| Point | Foods and frequency of consumption | Criteria for 1 point1 |
| 1 | Do you use olive oil as main culinary fat? | Yes |
| 2 | How much olive oil do you consume in a given day (including oil used for frying, salads, out-of-house meals, etc.)? | ≥4 tablespoons |
| 3 | How many vegetable servings do you consume per day? (1 serving = 200 g; consider side dishes as half servings) | ≥2 (at least 1 portion raw or as salad) |
| 4 | How many fruit units (including natural fruit juices) do you consume per day? (1 unit = 150 g) | ≥3 |
| 5 | How many servings of red meat, hamburger, or meat products (ham, sausage, etc.) do you consume per day? (1 serving = 100–150 g) | <1 |
| 6 | How many servings of butter, margarine, or cream do you consume per day? (1 serving = 12 g) | <1 |
| 7 | How many sweet/carbonated beverages do you drink per day? | <1 |
| 8 | How much wine do you drink per week? | ≥7 glasses |
| 9 | How many servings of legumes do you consume per week? (1 serving = 150 g) | ≥3 |
| 10 | How many servings of fish or shellfish do you consume per week? (1 serving = 100–150 g of fish, or 4–5 units or 200 g of shellfish) | ≥3 |
| 11 | How many times per week do you consume commercial sweets or pastries (not homemade), such as cakes, cookies, biscuits, or custard? | <3 |
| 12 | How many servings of nuts (including peanuts) do you consume per week? (1 serving = 30 g) | ≥3 |
| 13 | Do you preferentially consume chicken, turkey, or rabbit meat instead of veal, pork, hamburger, or sausage? | Yes |
| 14 | How many times per week do you consume vegetables, pasta, rice, or other dishes seasoned with sofrito (sauce made with tomato and onion, leek, or garlic, simmered with olive oil)? | ≥2 |
0 points if these criteria are not met.
The primary endpoint was incident CVD (an aggregate of nonfatal myocardial infarction, nonfatal stroke, and CVD death) (19, 21). Secondary outcomes included total mortality, diabetes, metabolic syndrome (MetS), peripheral arterial disease, atrial fibrillation, neurodegenerative diseases, and major cancers. An event adjudication committee, whose members were blinded to group allocation, was responsible for event ascertainment. The PREDIMED protocol was approved by the Institutional Review Boards of all participating centers. The main results are described below.
Effects on the main outcome: CVD.
A total of 7447 candidates were randomly assigned into the 3 PREDIMED intervention groups (21). The groups were similar regarding baseline clinical characteristics and drug treatment regimes. The mean age of participants was 67 y, the mean BMI was 30 kg/m2, close to one-half had diabetes, two-thirds had dyslipidemia, and 4 of 5 had hypertension.
During follow-up, participants in the 2 MeDiet groups improved the 14-point score of adherence to the MeDiet, with statistically significant differences vs. the control group for 12 of the 14 points. Improved compliance with the MeDiet occurred early and was maintained throughout the duration of the trial. Compared with the control group, the main dietary changes were large increases in consumption of EVOO to 50 and 32 g/d and nuts to 0.9 and 6 servings (30 g/serving) per week in the MeDiet + EVOO and MeDiet + nuts groups, respectively. Changes in objective biomarkers indicated good compliance with the supplemental foods.
There were no between-group differences in physical activity during the study. No diet-related adverse effects occurred.
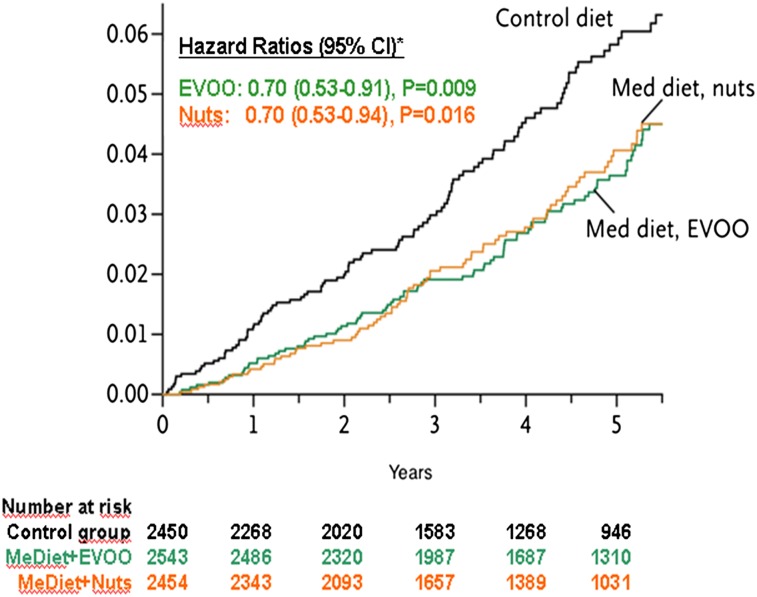
After 4.8 y, 288 major cardiovascular events occurred: 96 in the MeDiet + EVOO group (3.8%), 83 in the MeDiet + nuts group (3.4%), and 109 in the control group (4.5%) (21). The respective rates of the primary endpoint were 8.1, 8.0, and 11.2 per 1000 person-years. The unadjusted hazard ratios were 0.70 (95% CI: 0.53, 0.91) for the MeDiet + EVOO and 0.70 (95% CI: 0.53, 0.94) for the MeDiet + nuts (Fig. 2). Similar protection against CVD by the 2 MeDiets vs. the control diet was shown after multivariable adjustment for sex, age, adiposity variables, and baseline CVD risk factors. No effect on all-cause mortality was apparent. Disease risk reductions were similar across prespecified subgroups of sex, age, and cardiovascular risk factors. Hence, the PREDIMED study demonstrated for the first time with a randomized design that a MeDiet supplemented with either EVOO or nuts is useful in the primary prevention of CVD in individuals at high risk.
FIGURE 2.
Incidence of cardiovascular disease by intervention group in the PREDIMED (Prevención con Dieta Mediterránea) study. EVOO, extra-virgin olive oil; Med diet and MeDiet, Mediterranean diet. Reproduced from reference 21 with permission.
Regarding another CVD outcome, peripheral arterial disease, a strong relative risk reduction (>50%) was also apparent in both MeDiet groups compared with the control group (22).
Effects on MetS and diabetes.
As secondary endpoints of the PREDIMED study, we also assessed the effects of the interventions on diabetes incidence and MetS status. Based mostly on epidemiologic evidence, MeDiet adherence has been associated with a decreased risk of MetS (7) and diabetes (23). There is also consistent evidence that intensive lifestyle modification promoting weight loss through energy-restricted diets together with increased physical activity can reduce incident diabetes and is useful in managing MetS (7, 23). However, it was unknown whether dietary changes alone, without weight loss or exercise, might also prevent these conditions. Therefore, we hypothesized that the MeDiet interventions in the PREDIMED study could protect against diabetes in participants without diabetes and play a role in preventing or managing MetS, a cluster of metabolic abnormalities that predicts diabetes and cardiometabolic risk (24). MetS was defined by standard criteria as the presence of ≥3 of the following factors: 1) abdominal obesity; 2) hypertriglyceridemia; 3) low HDL cholesterol; 4) elevated fasting blood glucose; and 5) elevated blood pressure.
Preliminary data from the PREDIMED study showed that the MeDiets similarly decreased incident diabetes by 50% compared with the control diet after follow-up for 4.0 y (25). Of note, diabetes risk was reduced to a similar extent in participants of all treatment arms who reported higher scores of adherence to the MeDiet. However, that report was based on just 55 incident cases and dealt only with participants from 1 recruiting center. Recently, we reported the final results on diabetes in the whole PREDIMED cohort after follow-up for 4.1 y (26). Among 3541 participants without diabetes at baseline, 273 cases of new-onset diabetes occurred: 80 in the MeDiet + EVOO group, 92 in the MeDiet + nuts group, and 101 in the control group. After multivariable adjustment, hazard ratios for diabetes were 0.60 (95% CI: 0.43, 0.85) for MeDiet + EVOO and 0.82 (95% CI: 0.61, 1.10) for MeDiet + nuts compared with the control group. These results extend those of previous observational studies showing that lifestyle interventions, and specifically the MeDiet, can reduce the incidence of diabetes in persons at high risk (23), but here the beneficial effect was mainly attributable to diet alone, without other lifestyle changes.
We also evaluated the effect of intervention on MetS status in the first 1224 PREDIMED participants (27). At baseline, 61.4% of participants met the criteria for MetS. After 1 y, those allocated to MeDiet + nuts showed a significant reduction in the prevalence of MetS by 13.7% compared with reductions of 6.7% and 2.0% in the MeDiet + EVOO and control groups, respectively. Between-group incident MetS rates were similar, but reversion rates were significantly higher for the MeDiet + nuts.
Overall, these results show that a non-energy–restricted MeDiet, a dietary pattern high in unsaturated fats and antioxidants, could prevent diabetes and be useful in the management of MetS in high-risk individuals.
Mechanisms of protection: effects on intermediate markers of cardiovascular risk.
The PREDIMED study also reported a beneficial effect of the MeDiet on both classical and emergent risk factors. Results of the first 772 participants after intervention for 3 mo showed improved blood pressure, insulin sensitivity, lipid profile, and circulating inflammatory molecules with the 2 MeDiet interventions vs. the control diet (28). A PREDIMED substudy focusing on lipoprotein particles found that both MeDiets increased large HDL particles, whereas the MeDiet + nuts shifted LDL subfractions to a less atherogenic pattern (29). In a recent report of the whole PREDIMED cohort after a 4-y follow-up, diastolic but not systolic blood pressure values were lower after the 2 MeDiet interventions compared with the control diet (30). Of note, no significant body weight changes occurred with any diet in the 3-mo (28) and 1-y (27) assessments. Although traditional risk factors are critical for the development of atherosclerosis, the basis for CVD, other interrelated processes are at play, including endothelial dysfunction, inflammation, oxidative stress, and genetic factors among others. Increased LDL cholesterol is a potent atherogenic factor, but oxidatively modified LDL particles are critical in the onset of atherosclerosis and they were also reported to be decreased by the 2 MeDiets after 3 mo (31). Oxidation and inflammation are pathogenic in many chronic conditions when sustained over time. The reduction in inflammatory molecules demonstrated after the 2 MeDiets in the 3-mo pilot study (28) was confirmed by the decrease of monocyte expression of proinflammatory ligands after both MeDiets (32).
In a 1-y substudy, the 2 MeDiets reduced carotid intima-media thickness among participants with a high intima-media thickness at baseline (33). In a subsequent carotid ultrasound study at 2 y, the MeDiet + nuts was associated with plaque regression and the MeDiet + EVOO with delayed progression compared with progression in the control group (34). Although the underlying mechanisms of protection against CVD by the MeDiet are not fully understood, the richness of this dietary pattern in antioxidant and anti-inflammatory molecules is likely to be relevant (2, 5). One mechanism of action of nutrients relates to their capacity of modulating gene and protein expression and, subsequently, metabolite production. Previous nutrigenomic studies revealed that the MeDiet has a protective effect on the expression of several proatherogenic genes involved in vascular inflammation, foam cell formation, and thrombosis (35, 36). The MeDiet can also exert health benefits through changes in the overall transcriptomic response of genes related to cardiovascular risk (37). CVD protection by the MeDiet can be explained by a beneficial impact on classical and emergent cardiovascular risk factors, as well as nutrigenomic effects promoting antiatherogenic gene expression.
Nutritional genomics and the MeDiet within the PREDIMED study.
Nutritional genomic studies were included in the design of the PREDIMED study to achieve a better understanding of gene–diet interactions in determining disease phenotypes (38, 39). We sought to investigate whether the effects of the MeDiet as a whole or its components might differ depending on the genome. Gene expression studies further expanded our knowledge of genes and pathways influenced by the MeDiet. The PREDIMED study provides an exceptional framework for undertaking nutrigenetic studies because we can analyze the effect of different gene variants on intermediate phenotypes (lipids, blood pressure, etc.) and their interaction with diet, as well as effects of these interactions on final disease phenotypes (CVD, cancer, etc.).
Cyclooxygenase-2 (COX-2) and interleukin-6 (IL-6) are 2 important genes related to inflammation (40). At baseline, the COX-2 −765G > C polymorphism was associated with lower serum IL-6 and intercellular adhesion molecule-1 concentrations in carriers of the variant allele. The IL-6 −174G > C polymorphism (CC vs. G-carriers) was associated with higher serum intercellular adhesion molecule-1 concentrations, but no gene−diet interactions were found after dietary intervention. Thus, the MeDiet decreased inflammatory markers regardless of genotype. Because an increasing number of genetic variants are being discovered (41), we designed genetic analyses based on polymorphisms in new genes uncovered by our analyses at the whole-transcriptome level (37). Another strategy was to replicate gene–diet interactions described previously in other populations, such as those involving the apolipoprotein A2 (APOA2) gene (−265T > C) variant and saturated fat in determining BMI in 3 American populations (42). We also observed that the APOA2 saturated fat interaction was replicated in PREDIMED participants (43). Continuing with the classic polymorphisms, we analyzed the influence of the MeDiet and fat intake on the effects of CETP polymorphisms (−4502C > T and the TaqIB) on lipids (44). In another study, we focused on gene–diet interactions determining obesity (45). A genetic score, including the melanocortin 4 receptor (MC4R) rs17782313 and fat mass and obesity (FTO) rs9939609 variants, was strongly associated with BMI; although there was no statistically significant interaction with the MeDiet, greater adherence significantly reduced BMI in genetically susceptible individuals. Additional assessment of obesity-related variants focusing on the diabetes phenotype (46) showed significant interactions between them and the MeDiet in determining diabetes risk (greater adherence reduced risk in susceptible individuals).
Finally, we reported that intervention with MeDiet can reduce genetic risk (47). We assessed the transcription factor 7-like 2 (TCF7L2) gene, strongly associated with diabetes but controversially with plasma lipids and CVD, and found that the MeDiets reduced the adverse effect of the TCF7L2 rs7903146 (C > T) polymorphism on cardiovascular risk factors (fasting glucose and lipids) and stroke incidence.
Conclusions
To the best of the authors’ knowledge, PREDIMED demonstrated for the first time in a randomized clinical trial that the traditional MeDiet protects against CVD and confirmed that it beneficially influences classical and emergent cardiovascular risk factors. Important teachings from this landmark study deserve to be discussed. First, the results clearly show that a high-unsaturated fat dietary pattern is better for cardiovascular health than a lower-fat diet. Second, the PREDIMED MeDiets were successful in older persons at high risk of CVD, most of whom were being treated with antidiabetic, hypolipidemic, and/or antihypertensive drugs; hence, it can be said that the MeDiet was effective in controlling part of the residual risk observed after standard treatment of cardiovascular risk factors. Third, given the age of PREDIMED participants, the results tell us that it is never too late to change dietary habits to improve cardiovascular health. Fourth, the supplemented foods given to participants at no cost in the 2 MeDiet groups were instrumental in promoting good adherence to the overall dietary pattern. Thus, part of the success of the study might be attributed to EVOO and nuts, unsaturated FA-rich and antioxidant-rich foods that, despite their high fat content, did not promote weight gain. Finally, nutritional genomic studies show that adherence to the MeDiet blunts the development of cardiometabolic phenotypes in genetically susceptible individuals, a finding that concurs with previous evidence obtained from alternate healthy dietary patterns. The PREDIMED study was conducted in Spain, a Mediterranean population. Except for the customary use of olive oil and regular intake of wine with meals, the MeDiet does not differ from vegetable-based dietary patterns recommended for health in other countries, so the findings are likely to be translatable to non-Mediterranean populations, albeit with the quandary of whether preferences, access, cost, and taste will permit using olive oil and wine to a similar extent as in Mediterranean Southern Europe.
Importantly, the 30% CVD risk reduction shown with the MeDiet in the PREDIMED study is of similar magnitude to that reported in the statin trials, although it is obtained at no cost for the health system. To better define which diet is the best for overall health, more randomized clinical trials of nutrition intervention with outcomes of clinical events are warranted.
Acknowledgments
All authors read and approved the final manuscript.
Footnotes
Abbreviations used: CHD, coronary heart disease; CVD, cardiovascular disease; EVOO, extra-virgin olive oil; IL-6, interleukin-6; MeDiet, Mediterranean diet; MetS, metabolic syndrome; PREDIMED, Prevención con Dieta Mediterránea.
Literature Cited
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, et al. Heart disease and stroke statistics-2013 update: A report from the American Heart Association. Circulation. 2013;127:e6–245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Appel LJ, Van Horn L. Components of a cardioprotective diet: New insights. Circulation. 2011;123:2870–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hu FB. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13:3–9 [DOI] [PubMed] [Google Scholar]
- 4.Appel LJ. Dietary patterns and longevity: Expanding the blue zones. Circulation. 2008;118:214–5 [DOI] [PubMed] [Google Scholar]
- 5.Willett WC, Sacks F, Trichopoulou A, Drescher G, Ferro-Luzzi A, Helsing E, Trichopoulos D. Mediterranean diet pyramid: A cultural model for healthy eating. Am J Clin Nutr. 1995;61(Suppl. 6):1402S–6S [DOI] [PubMed] [Google Scholar]
- 6.Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169:659–69 [DOI] [PubMed] [Google Scholar]
- 7.Kastorini CM, Milionis HJ, Esposito K, Giugliano D, Goudevenos JA, Panagiotakos DB. The effect of Mediterranean diet on metabolic syndrome and its components: A meta-analysis of 50 studies and 534,906 individuals. J Am Coll Cardiol. 2011;57:1299–313 [DOI] [PubMed] [Google Scholar]
- 8.Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. Am J Clin Nutr. 2010;92:1189–96 [DOI] [PubMed] [Google Scholar]
- 9.Dilis V, Katsoulis M, Lagiou P, Trichopoulos D, Naska A, Trichopoulou A. Mediterranean diet and CHD: The Greek European Prospective Investigation into Cancer and Nutrition cohort. Br J Nutr. 2012;108:699–709 [DOI] [PubMed] [Google Scholar]
- 10.Tognon G, Nilsson LM, Lissner L, Johansson I, Hallmans G, Lindahl B, Winkvist A. The Mediterranean diet score and mortality are inversely associated in adults living in the Subartic region. J Nutr. 2012;142:1547–53 [DOI] [PubMed] [Google Scholar]
- 11.Gardener H, Wright CB, Gu Y, Boden-Albala B, Elkind MS, Sacco RL, Scarmeas N. Mediterranean diet and risk of ischemic stroke, myocardial infarction, and vascular death: The Northern Manhattan Study. Am J Clin Nutr. 2011;94:1458–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Misirli G, Benetou V, Lagiou P, Bamia C, Trichopoulos D, Trichopoulou A. Relation of the traditional Mediterranean diet to cerebrovascular disease in a Mediterranean population. Am J Epidemiol. 2012;176:1185–92 [DOI] [PubMed] [Google Scholar]
- 13.Hoevenaar-Blom MP, Nooyens ACJ, Kromhout D, Spijkerman AM, Beulens JW, van der Schouw YT, Bueno-de-Mesquita B, Verschuren WM. Mediterranean style diet and 12-year incidence of cardiovascular diseases: The EPIC-NL cohort study. PLoS One. 2012;7:e45458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Menotti A, Alberti-Fidanza A, Fidanza F. The association of the Mediterranean Adequacy Index with fatal coronary events in an Italian middle-aged male population followed for 40 years. Nutr Metab Cardiovasc Dis. 2012;22:369–75 [DOI] [PubMed] [Google Scholar]
- 15.Tognon G, Lissner L, Sæbye D, Walker KZ, Heitmann BL. The Mediterranean diet in relation to mortality and CVD: A Danish cohort study. Br J Nutr. 2014;111:151–9 [DOI] [PubMed] [Google Scholar]
- 16.Mitrou PN, Kipnis V, Thiébaut AC, Flood A, Mouw T, Hollenbeck AR, Leitzmann MF, Schatzkin A. Mediterranean dietary pattern and prediction of all-cause mortality in a US population: Results from the NIH-AARP Diet and Health Study. Arch Intern Med. 2007;167:2461–8 [DOI] [PubMed] [Google Scholar]
- 17.Martinez-Gonzalez MA, Bes-Rastrollo M. Dietary patterns, Mediterranean diet, and cardiovascular disease. Curr Opin Lipidol. 2014;25:20–6 [DOI] [PubMed] [Google Scholar]
- 18.de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: Final report of the Lyon Diet Heart Study. Circulation. 1999;99:779–85 [DOI] [PubMed] [Google Scholar]
- 19. PREDIMED. Prevención con dieta Mediterránea. Available from: http://www.predimed.es. Accessed 2013 Oct 20.
- 20.Schröder H, Fitó M, Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Lamuela-Raventós R, Ros E, Salaverría I, Fiol M, et al. A short screener is valid for assessing Mediterranean Diet adherence among older Spanish men and women. J Nutr. 2011;141:1140–5 [DOI] [PubMed] [Google Scholar]
- 21.Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279–90 [DOI] [PubMed] [Google Scholar]
- 22.Ruiz-Canela M, Estruch R, Corella D, Salas-Salvadó J, Martinez-Gonzalez MA. Mediterranean diet inversely associated with peripheral artery disease: The PREDIMED randomized trial. JAMA. 2014;311:415–7 [DOI] [PubMed] [Google Scholar]
- 23.Salas-Salvadó J, Martinez-González MA, Bulló M, Ros E. The role of diet in the prevention of type 2 diabetes. Nutr Metab Cardiovasc Dis. 2011;21:B32–48 [DOI] [PubMed] [Google Scholar]
- 24.Després JP, Lemieux I, Bergeron J, Pibarot P, Mathieu P, Larose E, Rodés-Cabau J, Bertrand OF, Poirier P. Abdominal obesity and the metabolic syndrome: Contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol. 2008;28:1039–49 [DOI] [PubMed] [Google Scholar]
- 25.Salas-Salvadó J, Bulló M, Babio N, Martínez-González MÁ, Ibarrola-Jurado N, Basora J, Estruch R, Covas MI, Corella D, Arós F, et al. Reduction in the incidence of type 2 diabetes with the Mediterranean diet: Results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care. 2011;34:14–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salas-Salvadó J, Bulló M, Estruch R, Ros E, Covas MI, Ibarrola-Jurado N, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, et al. Prevention of diabetes with Mediterranean diets: A subgroup analysis of a randomized trial. Ann Intern Med. 2014;160:1–10 [DOI] [PubMed] [Google Scholar]
- 27.Salas-Salvadó J, Fernández-Ballart J, Ros E, Martínez-González MA, Fitó M, Estruch R, Corella D, Fiol M, Gómez-Gracia E, Arós F, et al. ; PREDIMED Study Investigators. Effect of a Mediterranean diet supplemented with nuts on metabolic syndrome status: One-year results of the PREDIMED randomized trial. Arch Intern Med. 2008;168:2449–58 [DOI] [PubMed] [Google Scholar]
- 28.Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez V, Covas MI, Fiol M, Gómez-Gracia E, López-Sabater MC, Vinyoles E, et al. Effects of a Mediterranean-style diet on cardiovascular risk factors. Ann Intern Med. 2006;145:1–11 [DOI] [PubMed] [Google Scholar]
- 29.Damasceno NR, Sala-Vila A, Cofán M, Pérez-Heras AM, Fitó M, Ruiz-Gutiérrez V, Martínez-González MA, Corella D, Arós F, Estruch R, et al. Mediterranean diet supplemented with nuts reduces waist circumference and shifts lipoprotein subfractions to a less atherogenic pattern in subjects at high cardiovascular risk. Atherosclerosis. 2013;230:347–53 [DOI] [PubMed] [Google Scholar]
- 30.Toledo E, Hu FB, Estruch R, Buil-Cosiales P, Corella D, Salas-Salvadó J, Covas MI, Arós F, Gómez-Gracia E, Fiol M, et al. Effect of the Mediterranean diet on blood pressure in the PREDIMED trial: Results from a randomized controlled trial. BMC Med. 2013;11:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fitó M, Guxens M, Corella D, Sáez G, Estruch R, de la Torre R, Francés F, Cabezas C, López-Sabater MC, Marrugat J, et al. Effect of a traditional Mediterranean diet on lipoprotein oxidation: A randomized controlled trial. Arch Intern Med. 2007;167:1195–203 [DOI] [PubMed] [Google Scholar]
- 32.Mena MP, Sacanella E, Vazquez-Agell M, Morales M, Fitó M, Escoda R, Serrano-Martínez M, Serra M, Salas-Salvadó J, Benages N, et al. Inhibition of circulating immune cell activation: A molecular antiinflammatory effect of the Mediterranean diet. Am J Clin Nutr. 2009;89:248–56 [DOI] [PubMed] [Google Scholar]
- 33.Murie-Fernández M, Irimia P, Toledo E, Martínez-Vila E, Buil-Cosiales P, Serrano-Martínez M, Ruiz-Gutiérrez V, Ros E, Estruch R, Martínez-González MA. Carotid intima-media thickness changes with Mediterranean diet: A randomizedtrial (PREDIMED-Navarra). Atherosclerosis. 2011;219:158–62 [DOI] [PubMed] [Google Scholar]
- 34.Sala-Vila A, Romero-Mamani ES, Gilabert R, Núñez I, de la Torre R, Corella D, Ruiz-Gutiérrez V, López-Sabater MC, Pintó X, Rekondo J, et al. Changes in ultrasound-assessed carotid intima-media thickness and plaque with a Mediterranean diet. A sub-study of the PREDIMED trial. Arterioscler Thromb Vasc Biol. 2014;34:439–45 [DOI] [PubMed] [Google Scholar]
- 35.Konstantinidou V, Covas MI, Muñoz-Aguayo D, Khymenets O, de la Torre R, Sáez G, Tormos Mdel C, Toledo E, Marti A, Ruiz-Gutiérrez V, et al. In vivo nutrigenomic effects of virgin olive oil polyphenols within the frame of the Mediterranean diet: A randomized controlled trial. FASEB J. 2010;24:2546–57 [DOI] [PubMed] [Google Scholar]
- 36.Llorente-Cortés V, Estruch R, Mena MP, Ros E, Martínez-González MA, Fitó M, Lamuela-Raventós RM, Badimon L. Effect of Mediterranean diet on the expression of pro-atherogenic genes in a population at high cardiovascular risk. Atherosclerosis. 2010;208:442–50 [DOI] [PubMed] [Google Scholar]
- 37.Castañer O, Corella D, Covas MI, Sorlí JV, Subirana I, Flores-Mateo G, Nonell L, Bulló M, de la Torre R, Portolés O, et al. In vivo transcriptomic profile after a Mediterranean diet in high-cardiovascular risk patients: A randomized controlled trial. Am J Clin Nutr. 2013;98:845–53 [DOI] [PubMed] [Google Scholar]
- 38.Ordovas JM, Corella D. Nutritional genomics. Annu Rev Genomics Hum Genet. 2004;5:71–118 [DOI] [PubMed] [Google Scholar]
- 39.Corella D, Ordovas JM. Single nucleotide polymorphisms that influence lipid metabolism: Interaction with dietary factors. Annu Rev Nutr. 2005;25:341–90 [DOI] [PubMed] [Google Scholar]
- 40.Corella D, González JI, Bulló M, Carrasco P, Portolés O, Díez-Espino J, Covas MI, Ruíz-Gutiérrez V, Gómez-Gracia E, Arós F, et al. Polymorphisms cyclooxygenase-2–765G>C and interleukin-6–174G>C are associated with serum inflammation markers in a high cardiovascular risk population and do not modify the response to a Mediterranean diet supplemented with virgin olive oil or nuts. J Nutr. 2009;139:128–34 [DOI] [PubMed] [Google Scholar]
- 41.Corella D, Ordovas JM. Nutrigenomics in cardiovascular medicine. Circ Cardiovasc Genet. 2009;2:637–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Corella D, Peloso G, Arnett DK, Demissie S, Cupples LA, Tucker K, Lai CQ, Parnell LD, Coltell O, Lee YC, et al. APOA2, dietary fat, and body mass index: Replication of a gene-diet interaction in 3 independent populations. Arch Intern Med. 2009;169:1897–906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Corella D, Tai ES, Sorlí JV, Chew SK, Coltell O, Sotos-Prieto M, García-Rios A, Estruch R, Ordovas JM. Association between the APOA2 promoter polymorphism and body weight in Mediterranean and Asian populations: Replication of agene-saturated fat interaction. Int J Obes (Lond). 2011;35:666–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Corella D, Carrasco P, Fitó M, Martínez-González MA, Salas-Salvadó J, Arós F, Lapetra J, Guillen M, Ortega-Azorin C, Warnberg J, et al. Gene-environment interactions of CETP gene variation in a high cardiovascular risk Mediterranean population. J Lipid Res. 2010;51:2798–807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Corella D, Ortega-Azorín C, Sorlí JV, Covas MI, Carrasco P, Salas-Salvadó J, Martínez-González MÁ, Arós F, Lapetra J, Serra-Majem L, et al. Statistical and biological gene-lifestyle interactions of MC4R and FTO with diet and physical activity on obesity: New effects on alcohol consumption. PLoS ONE. 2012;7:e52344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ortega-Azorín C, Sorlí JV, Asensio EM, Coltell O, Martínez-González MA, Salas-Salvadó J, Covas MI, Arós F, Lapetra J, Serra-Majem L, et al. Associations of the FTO rs9939609 and the MC4R rs17782313 polymorphisms with type 2 diabetes are modulated by diet, being higher when adherence to the Mediterranean diet pattern is low. Cardiovasc Diabetol. 2012;11:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Corella D, Carrasco P, Sorlí JV, Estruch R, Rico-Sanz J, Martínez-González MA, Salas-Salvadó J, Covas MI, Coltell O, Arós F, et al. Mediterranean diet reduces the adverse effect of the TCF7L2-rs7903146 polymorphism on cardiovascular risk factors and stroke incidence: A randomized controlled trial in a high-cardiovascular-risk population. Diabetes Care. 2013;36:3803–11 [DOI] [PMC free article] [PubMed] [Google Scholar]