Abstract
Purpose
Conducting research in a rural area can be challenging for nurses for a variety of different reasons. The task at hand can be especially difficult when it involves discussing a sensitive topic, such as Human Papillomavirus (HPV) vaccination. This study was conducted to describe parental perceptions of the HPV vaccine in rural areas, while simultaneously describing a method for engaging in successful nursing research in rural areas.
Methods
A team of nurse researchers completed a planned process to first understand rural culture in southeastern Georgia, and then more specifically, the families living in these three separate counties. This process initially involved developing a connection and working relationship with key community leaders, such as school principals. Following this, researchers worked on establishing rapport and trust with local parents and research participants themselves. Qualitative methods were then used to collect focus group and interview data on parental views of HPV, HPV vaccination, and HPV-related cancers.
Findings
Results indicated that parents had little knowledge of the HPV vaccine in rural Georgia, including misconceptions that the vaccine is for females only. In addition, many parents continually voiced the concern that the HPV vaccine would promote promiscuity in their children.
Conclusions
Providing consistent, timely, and open communication with the community members was crucial throughout the entire research process. This focused approach with respect to total community, culture, and religious value is essential in conducting research. Future studies conducted in rural areas should focus on specific intervention points that improve Parental HPV knowledge.
Keywords: Research Challenges in Isolated Communities, Cultural Competence, Educating Researchers, Parental Knowledge of HPV in Rural Georgia
Researching and Respecting the Intricacies of Isolated Communities
Conducting research in rural areas poses a number of challenges related to the person, such as a lack of trust in researchers or lack of interest in research topics; to the community, including a lack of connection to the rural population; and diminished access to the rural population due to physical distance. However, overcoming these challenges is essential because of the fact that these groups of individuals continue to suffer higher than normal rates of various morbidities, including cervical cancer. In order to begin to address this concern, a research study was implemented to speak with rural parents about their thoughts on the Human Papillomavirus (HPV) Vaccine. Study implementation required educating a research team, and then initiating a working relationship with rural community leaders, school officials, and parents. This paper was then developed to share successful strategies for research implementation in rural areas, while also describing results from a qualitative research project focusing on a sensitive topic: prevention of HPV infection in Rural Georgia.
Background
Working in Rural Areas
Rural communities in southern Georgia suffer both from health and geographic disparities that are unlike other rural populations in the United States (Hart, Larson, & Lishner, 2005). The rural poor are defined as those often living in isolated communities depending upon the help of the government, such as through welfare services like Medicaid or Medicare. These groups frequently live longer distances from healthcare services, and have higher costs associated with these services than their larger urban or larger rural counterparts (Hart et al., 2005; Ryan-Nicholls & Racher, 2004). However, many rural Georgians are living in extreme poverty, also termed the “extreme poverty experience”, which has been described by researchers as higher unemployment rates, declining or stalled industrial growth, slow or no job growth, and higher populations of children and the elderly (Brown & Hirschl, 1995). Unfortunately, in southern Georgia, extreme poverty has been perpetuated by stratified political and economic systems that foster dependency and increase health disparities (Tickamyer & Duncan, 1990).
A life of extreme poverty, which is one result of a state of persistent poverty, is associated with the inability to find employment, limited opportunities to improve and maintain financial independence, and persistent marginalization. Consequently, these factors have continually kept African Americans, one of the largest groups enduring the extreme poverty experience, in jobs with lower wages, as well as further increasing the overall number of those families living in extreme poverty (Williams, 2007; Zimmerman & Whetten, 1938). In addition, persistent poverty and the extreme poverty experience in rural southern communities have brought unique challenges to rural adolescents and their healthcare providers.
The extreme poverty experienced by many adolescents living in rural areas puts them at an increased risk for a variety of negative lifestyle choices, such as dropping out of school and participating in high-risk sexual behavior. This lifestyle thus increases their overall risk for contracting the Human Papillomavirus (HPV) and other asymptomatic sexually transmitted infections (Gottvall, Waldenström, Tingstig, & Grunewald, 2011; "New data show heavy impact of chlamydia on U.S. men and women, particularly young people.," 2005).
General Challenges for Nurse Researchers in Isolated Communities
Challenges for nurse researchers in isolated, rural communities include understanding the unique culture of rural communities and identifying health care challenges in these individual areas. Rural southern culture can vary from county to county, as each one has a social history that may include poverty, segregation, and marginalization. The variation from one county to another might best be viewed or described as a neighborhood effect. A neighborhood effect is the aggregate effect of social determinants of health, such as income, education, employment, and residence (Hartley, 2004). When challenged with research in rural communities, it is essential that each specific county be assessed individually and the uniqueness of each neighborhood examined to determine neighborhood effects and specific rural culture for that county.
Rural culture is also closely linked with family structures, and a common misconception is that all rural families are extended and live in close proximity. However, rural culture also includes teens raised in single parent homes. These teens have demonstrated greater health and geographic disparities than their counterparts raised in traditional nuclear or extended families (McLaughlin & Sach, 1988). Further evidence of the gap in health and geographic disparities for teens living in persistent rural poverty is seen in research that indicates rural women are less likely to be counseled about STIs during pregnancy and to lack a preferred method for STI prevention. Furthermore, these women believe that their partners do not carry any STIs (Crosby, Yarber, DiClemente, Wingood, & Meyerson, 2002). This makes transmission of HPV and rates of HPV infection a harsh reality for many women living in rural, isolated communities with limited financial and health resources.
The challenge of limited health care resources is also important to address when studying rural communities. When this study was initially being considered in 2008, Georgia ranked 41st out of 50 states in overall health rankings, demonstrating a decrease in public health funding by 22%, a decline in immunization coverage by 3%, high rates of infectious disease, and an increasing number of uninsured ("America's health rankings: a call to action for individuals & their communities," 2008). These rankings underline the effects of persistent rural poverty on health issues and define the health and geographic disparities prevalent for the rural poor, including teens. The rural counties selected for study suffered from the economic, public health, and educational challenges that are consistent with the overall, larger healthcare and geographic disparities.
Finally, geographic disparities compound the problems associated with poor access to care, disinterest in academic achievement, and poverty. Percentages of teens, women, and parents living in rural areas below the poverty level continue to increase in southern Georgia. The documented rates of poverty for girls and boys 14 to 17 years of age are greater than 26 %, compared to 17% of their urban counterparts (Rogers, 2001; Rogers & Dagata, 2000). African American girls ages 14 to 17 living in rural areas are at an even greater risk, as poverty rates here exceed 22%, which does not include those living in the “near poverty” category, or family incomes only marginally above the poverty line (Rogers, 2001). In addition, poverty rates for children under the age of 18 represent a disproportionate percentage of the poor − 35.7%, whereas children under the age of 18 represent only 25% of the total US population (Proctor & Dalaker, 2002). Given these challenges, the Principal Investigator (PI) of this study recognized the need to examine the culture, the health care environment, and the geographic disparities of each selected county to better educate the research team.
HPV: A Hidden Disease in Isolated Communities
HPV is the most commonly occurring sexually transmitted infection in the United States, infecting approximately twenty million people annually (Gottvall et al., 2011). Half of these infections occur in adolescents and young adults between the ages of 15 to 24 years, with actual rates for this age group projected to be much higher in rural areas due to the asymptomatic nature of the infection in many people (Gerund & Barley, 2009)
HPV infections are transmitted through direct contact during sexual intercourse, including genital-to-genital, manual, and oral sex practices. Winer et al. (2006) provide strong evidence that HPV is usually transmitted through penetrative sex; however, transmission rates of 9.7% suggest that skin-to-skin or genital-to-genital contact transmission does occur. It is estimated that in addition to the twenty million people currently infected with HPV through all modes of transmission, another six million infections are newly diagnosed each year (Centers for Disease Control and Prevention [CDC], 2012). Increasing rates of diagnosed HPV infection in rural communities is a growing concern, as the incidence of HPV-related cervical cancer in these rural communities continues to rise (Dempsey, Cohn, Dalton, & Ruffin, 2011; Jain et al., 2009).
This concerning rise in HPV and HPV-related cancers is the motivation for research in these rural communities. Because HPV infection can be a sensitive topic, an extensive review of literature, discussion of culture in rural communities, and a plan to contact and determine the feasibility of research in these isolated, rural South Georgia communities were conducted and completed. The Principal Investigator’s (PI) research proposal was submitted for a descriptive study with a theoretical framework based on the Health Belief Model to examine parental knowledge, attitudes, beliefs, and intent to vaccinate their children, ages 9 to 13, against HPV. After funding was received, a variety of challenges arose for the nurse researchers.
Community Engagement Methods
Pre-proposal Planning
Initially, pre-proposal planning and research team education was essential to build the foundation for successful data collection in new, rural sites. The strategies used during the pre-proposal phase included: informal phone conversations with community leaders, spontaneous interviews, planned meetings, presentations to school boards and parents, informal windshield surveys, and simple observational field notes.
Team Education
When the PI began to strategize on how to best educate the research team, many materials and frameworks were considered. This specific research project required a theoretical framework that would challenge team members, including nursing students and others with health science degrees, and include concepts of cultural competence. Campinha-Bacote’s model of Nursing Cultural Competence was eventually selected, due to its progressive viewpoint that cultural competence is a working process consisting of five constructs: cultural awareness, cultural knowledge, cultural skill, cultural encounters, and cultural desire (Camphinha-Bacote, 2002).
The research team was comprised of doctoral and bachelor nursing students. All nursing students had roles in data collection, interaction with community members and parents, and data entry. Initially, the research team and the PI reviewed and discussed current literature about persistent poverty and rural health. Using the information from the research and the topics from discussions, the research team hypothesized the possible correlations, if any, between HPV vaccine uptake, health disparities, and geographic barriers. In addition, formal and informal discussions occurred about each member’s own cultural awareness and cultural encounters. Along with this exercise, additional information about the rural counties, including demographics, unemployment rates, high school graduation rates, and economic impacts from the recession of 2008, increased the team members’ understanding of the culture in these rural communities. These discussions and exercises provided important contextual information needed to prepare for project implementation. The dramatic health and geographic disparities of the focal rural communities, in addition to the importance of consistent communication, were emphasized. Communication that was purposefully void of any condescension or bias was essential when working with the various parents, communities, and school leaders throughout the areas. Informal discussions among the team members prior to research clarified what the hypothesized concerns and disparities of the study should focus on. This was an additional strategy for educating the research team, and it assisted in dispelling any preconceived ideas or prejudices.
Each strategy for educating the research team focused on respecting every individual, rural southern community for its own intrinsic value and attributes, whether it was the town’s historic value, community pride, beautiful countryside, or hospitality of the residents. As the research team continued to discuss these issues across the period of data collection, it was clear that framing this project in terms of education and an attention to cultural competence was essential. Research team members quickly became aware that the problem of increased HPV transmission and decreased HPV vaccine uptake could be solved only by building a partnership with the residents in these rural southern communities. This process required an unwavering respect for these isolated communities, and the establishment of trust that began with appreciation for everyone involved.
Strategies for Contact
Efforts were initiated to engage and encourage community members, especially school principals and administrators, to participate in the research process. Support from these key community leaders was essential to successful implementation of data collection. Once school officials and community leaders agreed upon the aims of the project, these key, influential leaders assisted in developing communication venues with other school officials, parents, and school nurses. A reciprocal wheel of communication among the team members, PI, and community leaders was emphasized, with a focus on communication initiation and follow-through. The methods most commonly used to initiate and maintain contact between the community leaders and the PI included informal phone conversations, spontaneous interviews, planned meetings, and eventually presentations to school boards and parents to ascertain their level of interest in participating in the research process. Throughout the entire process, communication was purposefully kept open, honest, and consistent, as well as attentive to community leaders’ and parents’ suggestions and insights.
Research Procedures
Preliminary Participant Introduction
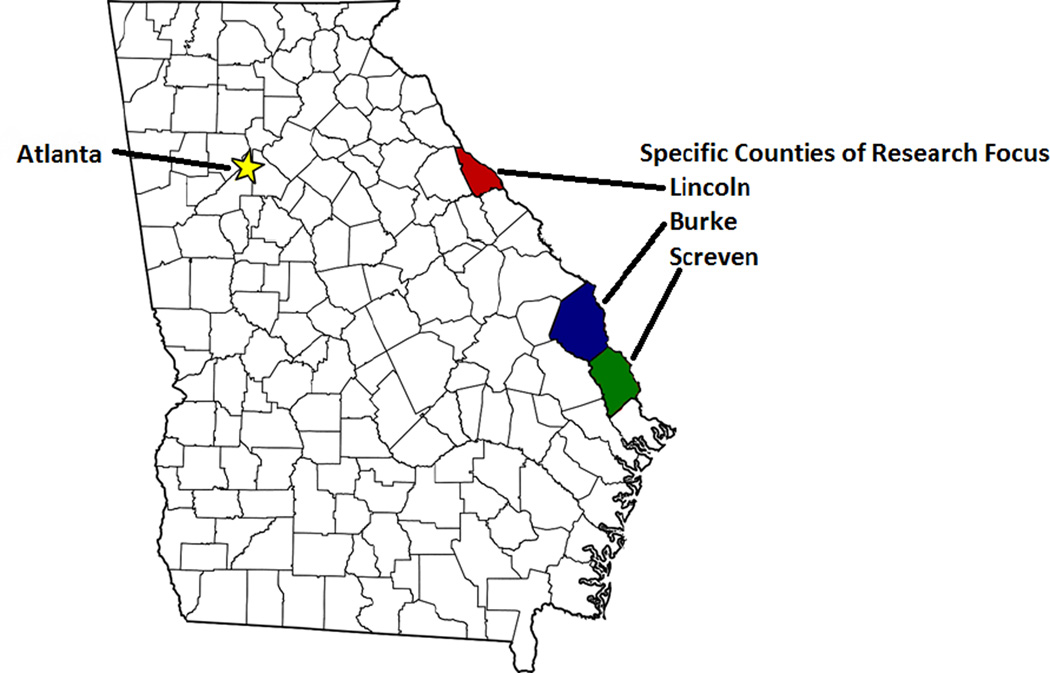
After community engagement and approval by the University’s Institutional Review Board (IRB) and the county School Superintendents, parents were recruited through IRB approved flyers and word of mouth recruitment by community leaders in the chosen counties of research focus: Burke, Lincoln, and Screven Counties, as shown in Figure 1. Parents were greeted by either the PI or trained research assistant (RA), and screened for eligibility (age 18 or older, had a child between the ages of 9 – 13, and signed and read the informed consent letter). Eligible parents were invited to attend a focus group discussion about sexual health and other health issues in their community through their Middle School Principals, whom the community views as well-respected and influential leaders. This community organization leader explained that the purpose of the study was to elicit information to inform the development of HPV Intervention Tools targeting rural areas. Parents were also informed that focus groups would last approximately 30 – 45 minutes, and that they would be reimbursed $50 total for their time spent completing a brief survey and the focus group discussions. Contact information was obtained from parents that agreed to participate, and reminder calls were made to participants in the two days before the focus group.
Figure 1.
Specific Counties of Research Focus
Varying Demographics
Participants were recruited from September through November 2011, as part of a study to develop a culturally appropriate intervention addressing cancer prevention and HPV education. The counties selected for research included: Burke, Lincoln, and Screven counties of southeast, rural Georgia. Each county varies in demographic and geographic challenges.
Burke County has a population of 23,316 individuals, with a median household income of $33,155, and an unemployment rate of 8.9%. Forty-seven percent of the children in this county are living below the poverty line. In terms of race and culture, 43.3% of the individuals here are African American. The closest hospital to these residents is approximately 45 minutes away. Lincoln County’s population is smaller, at 7,966 individuals, with a median household income of $36,399. Despite this slight increase in household income compared to Burke County, the unemployment rate here is 11.2%. Thirty-two percent of the children in this county are living below the poverty line. Of all the county individuals, 32.1% are African American. A drive from Lincoln County to the closest hospital takes approximately 65 minutes. Finally, Screven County houses 14,593 individuals, with a median household income of $32,155. The unemployment in this area is at 14.8%. In this county, 33.5% of the children are living below the poverty line. In this area, 43.3% of the individuals are African American, as shown in Table 1. In addition, the closest hospital to Screven County is approximately 90 minutes away (US Census Bureau, 2011).
Table 1.
Summary of Demographic Data for Burke, Lincoln, and Screven Counties, GA
| Counties | Burke | Lincoln | Screven |
|---|---|---|---|
| Population | 23,316 | 7,996 | 14,593 |
| Population Density, per mile2 | 28.1 | 37. | 22. |
| Age Statistics | |||
| Median Age | 35.9 | 45.0 | 39.5 |
| Percent Female | 52.0% | 51.3% | 51.2% |
| Under 20 | 31.1% | 23.2% | 28.3% |
| Between 20 and 39 | 23.9% | 20.4% | 22.3% |
| Between 40 and 59 | 27.3% | 31.4% | 28.1% |
| 60 and older | 17.6% | 25.1% | 21.2% |
| Race and Culture | |||
| White | 54.6% | 65.7% | 54.6% |
| Black or African American | 43.3% | 32.1% | 43.3% |
| Asian | 0.4% | 0.4% | 0.4% |
| American Indian | 0.3% | 0.4% | 0.3% |
| Pacific Islander | 0.0% | 0.0% | 0.0% |
| Other Races | 0.3% | 0.4% | 0.3% |
| Two or more races | 1.1% | 0.9% | 1.1% |
| Hispanic or Latino culture | 1.2% | 1.2% | 1.2% |
| Households and Families | |||
| Housing Units | 9,865 | 4,786 | 6,739 |
| Housing Unit Density per mile2 | 11.9 | 22.7 | 10.4 |
| Households | 8,533 | 3,281 | 5,596 |
| Mean Household Size | 2.7 | 2.4 | 2.5 |
| Families | 6,110 | 2,252 | 3,854 |
| Mean Family Size | 3.2 | 2.9 | 3.1 |
| Households with children under 18 | 39.0% | 23.0% | 27.8% |
| Households with married couple living together | 42.4% | 50.3% | 45.1% |
| Households with no husband present | 24.1% | 14.2% | 18.6% |
| School | |||
| Public School Enrollment | |||
| Percent Female | 47.3% | * | 50.0% |
| Qualify for Free or Reduced Price Lunch | 83.7% | 97.9% | 78.1% |
| White | 30.5% | 58.3% | 46.2% |
| Black or African American | 66.7% | 38.5% | 51.9% |
| Elementary (Pre-K – grade 5) | 49.9% | 46.7% | 44.8% |
| Middle (Grades 6–8) | 21.5% | 20.4% | 23.2% |
| High (Grades 9–12) | 28.5% | 32.9% | 32.0% |
| Private School Enrollment | 582 | 4 | 64 |
Data was missing from US Census records.
One of the most challenging geographic barriers present to both the researchers and the participants was the distance required for both parties to travel in order to meet at a facility such as a school library, school administrative building, or public library that would be an environment conducive to conducting research. The PI and RAs traveled approximately 6–8 hours round trip to rural Southeastern Georgia for most focus groups, while many parent participants were required to travel upwards of an hour themselves.
Qualitative Methods
A total of four focus groups were conducted; the size of the groups ranged from three to five participants. Before the focus groups began, all participants read a letter of consent and acknowledged their agreement to participate in the study. Groups were audio taped using a digital recorder. Focus groups were conducted by one of three facilitators with training in qualitative research and issues facing rural and minority populations.
Facilitators followed a semi-structured focus group guide that included open-ended questions related to HPV vaccine related beliefs and perceptions. Participants were asked their thoughts about general health, HPV knowledge, sources of HPV related information, and attitudes toward vaccinating their children against HPV, as seen in Table 2. These questions served as an initial stimulus for discussion; facilitators were encouraged to probe responses and ask follow-up questions based on participant responses to the initial questions. Throughout the data collection process, evidence for emerging ideas was sought. To do this, the research team listened to the audio recordings after each focus group, and facilitators and project staff discussed topics that merited additional follow-up in subsequent focus groups. Focus groups were conducted until content saturation was reached, i.e., until no new ideas or themes emerged during the focus groups. All procedures were approved by the IRBs of the participating institutions.
Table 2.
Sample HPV Focus Group Questioning Route
| Begin Focus Group |
| 1. PI or Group Leader Introduction |
2. Icebreaker/Parental Introduction
|
| 3. Identification of parents’ children’s ages |
4. First Question: “Have any of you ever known anyone who’s had cancer or died of cancer?”
|
5. Second Question: “Can you tell me what you think ‘good health’ is?”
|
| 6. Third Question: “What are some ways you think cancer is preventable?” |
7. Fourth Question: “Now I’d like to talk a little bit about HPV. Have you heard of it? What do you know about HPV?”
|
8. Fifth Question: “Did anyone know there’s a vaccine for HPV?”
|
| 9. Sixth Question: “Do you know anyone who’s had their kids vaccinated with the HPV vaccine?” |
10. Seventh Question: “Did they talk to you about the benefits? Do you think there are any benefits?”
|
11. Eighth Question: “Is there any reason you would choose not to get your child vaccinated with the HPV vaccine?”
|
12. Ninth Question: “Finally, I’d like to ask whether talking about the HPV vaccine here made you change your mind about getting your child vaccinated?”
|
Data Analysis
Thematic coding procedures were used to analyze the qualitative data. First, the digital audio recordings were transcribed and checked for accuracy. Transcripts were then preliminarily analyzed by an expert in qualitative analysis (EQA) using the principles of grounded theory (Cates, Brewer, Fazekas, Mitchell, & Smith, 2009; Glaser & Strauss, 1967). After familiarizing themselves with the recordings and transcripts, the EQA and an additional coder created broad categories, and each unit of the transcript was assigned to one or more categories. Within each broad category, similar data were grouped together, and subcategories were created based on these data groupings. Coders discussed categories and subcategories, which were then revised as new data were considered, or as researchers came to new understandings and generated new hypotheses. To optimize the trustworthiness of the results, regular meetings were held with the PI and EQA to discuss results and to develop new understandings and interpretations of the data.
Results
Demographics
Participants included 18 parents (2 men, 16 women) with ages ranging from 35 to 60 years, recruited from Burke, Lincoln, and Screven counties. The majority of participants were African American (n = 12; 67%); while 33% were White. The children of the parents’ being interviewed ranged in age from 3 to 30 years old, with all parents having at least one child 9–13 years old and/or in middle school, as per the study inclusionary criteria. The average number of children per participant was 2.5. The average age of the children was 12.5 years. Some parents did not list the gender of their child, but of those who did: male children represented a slight majority at 54% (n=21), while female children represented 46% (n=18) of the child population.
Qualitative Analysis
The results presented here are organized around three major themes identified in the analysis: 1) perception that the HPV vaccine is only for females, 2) concerns about the long-term implications of the vaccine, and 3) concerns that the vaccine encourages sexual promiscuity. In addition, many parents brought up the desire for more education on the vaccine, for both their children and themselves. They also felt that greater emphasis should be placed on community involvement and support in protecting children from sexual risks.
Perception that vaccine is for females
Many of the parents in the focus groups expressed that they had heard of the HPV vaccine, but the majority of them believed it was given exclusively to girls. As a result of their belief that the HPV vaccine is made solely for females, many of the parents only listed prevention of cervical cancer as the target for the vaccine. One parent specifically stated that:
It is transmitted predominantly through being sexually active…and I’ve always heard it just mostly for girls, as opposed to boys, but then again, I guess if you’re sexually active, anybody can get it… And that it’s very painful. That’s about all I know.
Concerns on long-term implications of HPV vaccine
Initially, parents were open to considering vaccination of their children, despite the fact that many of them voiced concerns regarding the risks associated with the vaccine. The general consensus was that there was a perceived lack of history of the vaccine’s use, and that they were unsure of the possible long-term side effects of the vaccine. Throughout the discussion, the parents’ willingness to vaccinate their children decreased. Many concerns were shared about the vaccine’s safety, including the comment by one parent:
My lack of knowledge about the benefits versus the side effects from vaccinations. What is the probability that it’s going to produce these results if I do expose my child to the vaccination? Because, you know, I like children. They can possibly suffer severe effects from the vaccination. So before I expose my child to those harmful side effects, I first need to know the benefits of him getting that vaccination.
Concerns on giving permission to have sex
Parents were also concerned that by having their children vaccinated, it would seem to the child as if the parents were giving them permission to have sex. Many parents expressed their beliefs that their children did not need the vaccine because they were raised to not engage in pre-marital sex. One parent explained her rationale by implying that the majority of HPV vaccine implications are directly related to sexual activity:
I think if it were strictly for cancer, that’s a different story. But the fact that you get the HPV virus through sexual transmission…That’s when you kind of have to stop and think. It’s almost like…‘Ok, son, here’s this to prevent this, here’s this to prevent that’…Excuse me, if you didn’t do it, you wouldn’t have to worry about it.
Discussion
Implications of Thematic Analysis
Data collection identified 3 key themes common throughout the focus groups, including a misconception on who should receive the vaccine, concerns about the safety and history of the vaccine, and a concern that giving the HPV vaccine to children will encourage sexual promiscuity. These findings imply that there is a need for more education about the HPV vaccine, and that the education should be targeted towards parents residing in rural areas, especially African American families who suffer disproportional rates of cervical cancer and deaths related to cervical cancer. In addition to providing basic education on what HPV and the HPV Vaccine are, the misconception that the vaccine is explicitly for females needs to be addressed. It is also imperative to discuss parental concerns relating to vaccination in order to increase vaccine uptake. Specifically, the history of the vaccine development and the relatively low-risk should be emphasized. Finally, it will also be necessary to openly discuss and explore parental concerns about a link between vaccination and sexual promiscuity. If parents see the benefits of the vaccine as outweighing the risks, vaccine uptake rates will likely increase. This is especially crucial in rural areas, where cervical cancer rates are exceptionally high and access to primary care is limited.
Assessment of Knowledge
Families living in rural areas are known to have less access to healthcare facilities, and consequently the services, such as HPV vaccination, that these facilities provide. In addition to this disparity, cervical cancer mortality is twice as high among African American women than in White women living in rural areas (Cates, et. al, 2009). Despite this, studies show that African American women are less likely to have heard of HPV than their White counterparts (Cates, et. al, 2009) This research conducted in rural Georgia supported these findings by discovering that between parents who have not/do not intend to vaccinate their children with the HPV vaccine, and those that do, African Americans accounted for over 83% of the former category. However, one distinct difference found in this current research was the overwhelmingly positive support by African Americans for vaccines in general. Despite some studies implying that African Americans are less likely to think that vaccines in general are beneficial and necessary than their White counterparts (Cates, et. al, 2009), this study in rural Georgia found the opposite results. Throughout focus groups, parents were specifically asked whether they approved of vaccines in general, and the vast majority, including mostly African American parents, stated that unless there was some type of allergy or medical contraindication, they were wholly supportive of vaccination. The issue seen with lack of HPV vaccine uptake, therefore, seems to stem from the fact that few of the African American parents interviewed had previously heard of either HPV or the HPV vaccine. Despite the majority of the African American parents not having heard of the HPV or the HPV vaccine, there was a general lack of knowledge on the vaccine implications and safety among parents of all races and ethnicities.
These findings imply that there is a need for more education about the HPV vaccine, and that the education should be targeted towards parents residing in rural areas, especially African American families who suffer disproportional rates of cervical cancer and deaths related to cervical cancer. In addition to providing basic education on what HPV and the HPV Vaccine are, the misconception that the vaccine is explicitly for females needs to be addressed. It is also imperative to discuss parental concerns relating to vaccination in order to increase vaccine uptake. Specifically, the history of the vaccine development and the relatively low-risk should be emphasized. Finally, it will also be necessary to openly discuss and explore parental concerns about a link between vaccination and sexual promiscuity. If parents see the benefits of the vaccine as outweighing the risks, vaccine uptake rates will likely increase. This is especially crucial in rural areas, where cervical cancer rates are exceptionally high and access to primary care is limited.
Role of Community Gate-keepers
Despite a variety of initial obstacles and challenges, research and community engagement were successfully initiated in multiple rural areas. One of the main reasons that this was possible was due to the support and guidance of key community leaders, or “gate-keepers” into the community. Key informers, including school superintendents, principals, and teachers, in the rural counties were fairly agreeable to the idea of conducting research there, and eventually became key proponents of the research project. However, they initially informed the PI that they had experienced some negative interactions with researchers previously, such as a lack of follow-up when data collection was completed. Despite any initial hesitancy or mistrust, the community gatekeepers were willing to organize and promote the research in the community. The PI and research assistants made a point to not only keep the community leaders informed throughout the entire research process, but also to seek their input on what topics should be addressed and how best to reach the parents. In addition, the PI regularly provided the counties with any and all preliminary data collected and plans for implementing interventions in the future. As this rapport and trust were built up, these individuals became indispensible consultants and collaborators for successful research study implementation and data collection. In addition to forming these necessary relationships to allow thorough data collection, the community gate-keepers paved the way to reach a multitude of parents throughout the communities who otherwise might not have been interested or trusting of nurse researchers from outside of town. Over the years spent collecting data and focus group information, the PI and research assistants gradually transitioned from the roles of nurse researchers interested in rural health, to identifiable community advocates interested in specifically improving the lives of children in Burke, Lincoln, and Screven counties of Georgia.
Specific Challenges for Rural Nursing Research
Overall, the main challenges encountered by the nurse researchers while working in a rural area centered on establishing rapport and trust with the community leaders and participants, encouraging parent participation, and the physical distances between survey/focus group collection sites. Working consistently and honestly with the community gatekeepers was an integral part in not only gaining trust and support among the leaders of the community, but also in gaining interest and participation from various parents. It is nearly impossible to enter into a secluded, rural community and start asking questions about parents’ children and their views on the HPV vaccine without having any sort of rapport established beforehand. Building a relationship with community leaders first, who could then reach out to their own community members, was a key component of the successful data collection. Not only did having the support from the community leaders give the parents trust in the researchers, it also enabled them to be honest and open in discussing their thoughts on various health topics relating to their children. An additional component of this was the manner in which the PI and research assistants framed their interest in the communities: not just as a scientific matter, but as a personal commitment to enhancing the health and lives of all children living in rural areas, who often lack access to primary care and experience a variety of health disparities.
Finally, the physical distance between the researchers (Atlanta-based) and the counties of interest (Southeastern Georgia) was also a barrier to overcome each time research was conducted. The PI and research team traveled an average of 3 – 4 hours, each way, to the communities in rural Georgia. In addition, the parents also had to travel upwards of an hour in order to reach a spot conducive to research and data collection. Many of the parents who participated in the research came from areas that required over an hour’s drive, which illustrates the geographical vastness in rural communities. This distance from any sort of school or town center in the communities is not only an issue when conducting research in the areas, but it is even more of a concern when the same expanse forces families to travel hours in order to reach the nearest pediatric hospital or healthcare facility.
Conclusions
Respect, Trust, and Communication
Educating a research team that is charged with work in rural communities must focus on the specific, individual rural culture for study success and community engagement. In addition, consistent communication, respect, and cultural competence are essential to build a foundation of relationships that support the entire research process. The initial pre-planning phase was imperative to understand the varying differences, community concerns, and possible barriers in each individual county. This research team found that this was best accomplished framing the cultural concerns in a specific model of cultural competency. With this information, the research team was then able to begin the process of establishing trust with the community members. One of the key methods to first establishing this respect and trust with the larger community body was building rapport with the specific, individual community gatekeepers, such as school principals or school officials, over a period of time. In addition to providing an avenue for reaching out to other possible parent participants, these types of community leaders can be invaluable resources for assessing the values and needs of the local community. Without the support of a key, influential community member, it would have been very unlikely that members of secluded, rural areas would have been willing to participate in nursing research where sensitive topics, such as adolescent sexual health, would be discussed. Once it was made clear that the research would be conducted with respect to specific concerns of each community, it was much easier for research participants to feel comfortable and trusting to discuss the topics associated with adolescent HPV infection.
In addition to the initial steps of building trust and ensuring respect, it was also essential to incorporate consistent, honest communication with all community members involved. One of the most common complaints and concerns that participants voiced was the lack of continued involvement after data collection was complete. Community gatekeepers expressed hesitancy in participating with the research because of past experiences when research was conducted with other groups, but no follow-up was provided with the parents to inform them of results and future actions to address the results found. To avoid this problem, the nursing research team made a point to consistently provide open, honest communication and to return to the communities once results were analyzed. In addition, at the completion of the initial parent surveys and focus groups, the researchers began collaborating with the parents on specific interventions to address the results and improve the overall health and well-being for adolescents living in areas.
Quick Steps to Researching in Rural Communities
Although any attempt to reach out to a rural community in order to conduct scientific research of them is a unique situation, and should be treated as such, the PI and researchers believe that the following “quick steps” are essential for those fellow researchers interested in accessing rural communities: (a) Research and identify the needs of a rural community; (b) Discuss these observations with a key community member, and potential liaison, such as a principal or church leader; (c) Assess willingness of key community member, or “gatekeeper”, to assess local willingness to participate; (d) Throughout this process of building trust and rapport, keep an open line of communication with the community gatekeepers and any parents willing to become involved in the research process; (e) Collect data at a time and in an environment that is convenient for the participants; (f) Follow up with community leaders and participants to let them know what data analysis shows, and what the implications are for further steps.
Implications for Future Rural Nursing Research
This focus on educating the research team and respecting the community has implications far beyond rural, isolated communities in southern Georgia. Research conducted in isolated areas in other parts of the world similarly requires educating a research team and respecting the community. While this may initially seem like common sense, there are few step-by-step explanations similar to those expressed in this article. This brief guide, or quick reference, can be highly valuable to students who wish to fully understand the intricacies of conducting rural health research. The strategies previously mentioned led to successful data collection, with greater than expected response rates. In addition, the relationships built during the pre-planning phase are ongoing, and have provided the framework for continued research.
Acknowledgments
Supporting Agencies
Funding from Robert Wood Johnson Foundation Nurse Faculty Scholar Program to Tami L. Thomas, ID # 67983
Contributor Information
Amy A. Blumling, Email: ablumli@emory.edu.
Tami L. Thomas, Email: tami.thomas@emory.edu.
Dionne P. Stephens, Email: Dionne.Stephens@fiu.edu.
References
- America's health rankings: A call to action for individuals & their communities. 2008 Retrieved from http://cdnfiles.americashealthrankings.org/SiteFiles/Reports/2008.pdf. [Google Scholar]
- Brown DL, Hirschl TA. Household poverty in rural and metropolitan-core areas of the United States. Rural Sociology. 1995;60(1):44–66. [Google Scholar]
- Camphinha-Bacote J. The process of cultural competence in the delivery of healthcare services: A model of care. Journal of Transcultural Nursing. 2002;13(3):181–184. doi: 10.1177/10459602013003003. [ MEDLINE] [DOI] [PubMed] [Google Scholar]
- Cates JR, Brewer NT, Fazekas KI, Mitchell CE, Smith JS. Racial differences in HPV knowledge, HPV vaccine acceptability, and related beliefs among rural, southern women. Journal of Rural Health. 2009;25(1):93–97. doi: 10.1111/j.1748-0361.2009.00204.x. [ MEDLINE] [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC] Genital HPV Infection - Fact Sheet. 2012 Retrieved from http://www.cdc.gov/std/HPV/STDFact-HPV.htm#common.
- Crosby RA, Yarber WL, DiClemente RJ, Wingood GM, Meyerson B. HIV-associated histories, perceptions, and practices among low-income African American women: Does rural residence matter? American Journal of Public Health. 2002;92:655–659. doi: 10.2105/ajph.92.4.655. [ MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dempsey A, Cohn L, Dalton V, Ruffin M. Worsening disparities in HPV vaccine utilization among 19–26 year old women. Vaccine. 2011;29:528–534. doi: 10.1016/j.vaccine.2010.10.051. [ MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaser BG, Strauss A. The Discovery of grounded theory. Chicago: Adline, Atherton; 1967. [Google Scholar]
- Gottvall Karin, Waldenström Ulla, Tingstig Charlotta, Grunewald Charlotta. In-hospital birth center with the same medical guidelines as standard care: A comparative study of obstetric interventions and outcomes. Birth. 2011;38(2):120–128. doi: 10.1111/j.1523-536X.2010.00461.x. [ MEDLINE] [DOI] [PubMed] [Google Scholar]
- Hart GL, Larson EH, Lishner DM. Rural definitions for health policy and research. American Journal of Public Health. 2005;95:1149–1155. doi: 10.2105/AJPH.2004.042432. [ MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley David. Rural health disparities, population health, and rural culture. American Journal of Public Health. 2004;94:1675–1678. doi: 10.2105/ajph.94.10.1675. [ MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain N, Euler GL, Shefer A, Lu P, Yankey D, Markowitz L. Human papillomavirus (HPV) awareness and vaccination initiation among women in the United States, National Immunization Survey - Adult 2007. Preventive Medicine. 2009;48:426–431. doi: 10.1016/j.ypmed.2008.11.010. [ MEDLINE] [DOI] [PubMed] [Google Scholar]
- McLaughlin DK, Sach C. Poverty in female-headed households: Residential differences. Rural sociology (USA) 1988;53(3):287–306. [Google Scholar]
- New data show heavy impact of chlamydia on U.S. men and women, particularly young people. Centers for Disease Control and Prevention. 2005 http://www.cdc.gov/od/oc/media/pressrel/r050712.htm.
- Proctor BD, Dalaker J. Current population reports: Poverty in the United States: 2001. Washington, DC: U.S. Census Bureau, Current Population Reports, U.S. Government Printing Office; 2002. pp. 60–219. [Google Scholar]
- Rogers CC. Factors affecting high child poverty in the rural south. Rural America. 2001;15(4):50–58. [Google Scholar]
- Rogers CC, Dagata E. Child poverty in nonmetro areas in the 1990's. Rural America. 2000;15(1):28–37. [Google Scholar]
- Ryan-Nicholls KD, Racher FE. Investigating the health of rural communities toward framework development. Rural and Remote Health. 2004;4(1):224. [ MEDLINE] [PubMed] [Google Scholar]
- Tickamyer AR, Duncan CM. Poverty and opportunity structure in rural America. Annual Review of Sociology. 1990;16(1):67–86. [Google Scholar]
- US Census Bureau. Small area income and poverty estimates. 2011 Retrieved from: http://www.census.gov/did/www/saipe/
- Williams RA. Cultural diversity, health care disparities, and cultural competency in American medicine. Journal of the American Academy of Orthopaedic Surgeons. 2007;15(Suppl 1):S52–S58. doi: 10.5435/00124635-200700001-00013. [DOI] [PubMed] [Google Scholar]
- Winer RL, Hughes JP, Feng Q, O'Reilly S, Kiviat NB, Holmes KK, Koutsky LA. Condom use and the risk of genital Human Papillomavirus Infection in young women. New England Journal of Medicine. 2006;354:2645–2654. doi: 10.1056/NEJMoa053284. [ MEDLINE] [DOI] [PubMed] [Google Scholar]
- Zimmerman CC, Whetten NL. Rural families on relief. US Government. Prining Office; 1938. [Google Scholar]